Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Care Needs of Community-Residing Male Patients with Vascular Cognitive Impairment
Authors Jhang KM, Wang WF, Chang HF, Liu YH, Chang MC, Wu HH
Received 23 August 2020
Accepted for publication 8 October 2020
Published 3 November 2020 Volume 2020:16 Pages 2613—2621
DOI https://doi.org/10.2147/NDT.S277303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Kai-Ming Jhang,1,* Wen-Fu Wang,1,2,* Hao-Fang Chang,3,* Yu-Huei Liu,4– 6,* Ming-Che Chang,7 Hsin-Hung Wu3,8,9
1Department of Neurology, Changhua Christian Hospital, Changhua, Taiwan; 2Department of Holistic Wellness, Ming Dao University, Changhua, Taiwan; 3Department of Business Administration, National Changhua University of Education, Changhua, Taiwan; 4Graduate Institute of Integrated Medicine, China Medical University, Taichung City, Taiwan; 5Drug Development Center, China Medical University, Taichung City, Taiwan; 6Department of Medical Genetics and Medical Research, China Medical University Hospital, Taichung City, Taiwan; 7Department of Nuclear Medicine, Changhua Christian Hospital, Changhua, Taiwan; 8Department of M-Commerce and Multimedia Applications, Asia University, Taichung City, Taiwan; 9Faculty of Education, State University of Malang, Malang, East Java, Indonesia
*These authors contributed equally to this work
Correspondence: Hsin-Hung Wu No. 2 Shida Road, Changhua City 500, Taiwan
Tel +886 4 7232105 ext. 7412
Fax +886 4-7211292
Email [email protected]
Purpose: The aim of this study was to identify the care needs of male patients with vascular cognitive impairment (VCI) and their caregivers.
Patients and Methods: This cross-sectional study enrolled 389 male patients with VCI and their caregivers who were cared for by the dementia collaborative care team at Changhua Christian Hospital, Taiwan. Fifteen care needs consisting of most of quality measures for people living with dementia and their caregivers were developed by the care team. Through face-to-face evaluations, individualized care needs were collected. The Apriori algorithm was used to identify care bundles for the patients and their caregivers.
Results: Six basic care needs for patients and their caregivers were identified, including appropriate schedule of activities, regular outpatient follow-up treatment, introduction and referral of social resources, referral to family support groups and care skills training, care for the mood of the caregiver, and health education for dementia and behavioral and psychological symptoms of dementia. Compared to subjects with all dementia subtypes from the previous studies, care for the mood of the caregiver was an important and frequent care need for the male patients with VCI and their caregivers. A comparison among the study and similar studies was made to highlight the strength of this study concentrating on the precise selection of care needs.
Conclusion: Collaborative dementia care teams should monitor for caregivers’ depression and include this care need into the care bundle when assessing male subjects with VCI.
Keywords: male patients with vascular cognitive impairment, people living with dementia, behavioral and psychological symptoms of dementia, dementia collaborative care model, care need, Apriori algorithm
Introduction
The global population is aging, and Asia is expected to have up to 60% of the world’s older adults aged 60 years or above and 50% of the world’s oldest old by 2030.1 Dementia is a neurodegenerative illness which is strongly associated with aging, and is one of the greatest global challenges for health and social care.2 The percentage of the population over the age of 65 years in Taiwan has grown rapidly from 6.8% in 1992 to 14.1% in 2018.3 A nationwide cross-sectional survey showed that the prevalence of all-cause dementia in older Taiwanese in 2014 was 8.04%,4 indicating an estimated 320,000 people living with dementia (PLWD) by 2030.5
Vascular cognitive impairment (VCI) refers to all forms of cognitive disorders associated with cerebrovascular disease, encompassing the full range of cognitive deficits from mild cognitive impairment to dementia.6 Vascular dementia is now recognized to be the second most common form of dementia after Alzheimer’s disease (AD). In a systematic review targeting the Chinese general population, the average percentages of AD and vascular dementia were 63.3% and 28.5%, respectively.5 The incidence of vascular dementia is higher in males than in females in all age groups.7 Patients with VCI tend to have gait disturbance, focal neurological deficits, executive dysfunction, and more apathy than patients with AD.8,9
To provide better clinical outcomes for PLWD and caregivers, care models involving interprofessional teams and multicomponent interventions have been published.10–12 Past studies have provided comprehensive individualized assessments including the patients’ function, behavior and psychological status, caregivers willingness, and their unmet needs.10,11 After systematic assessments between medical teams and PLWD and their caregivers, a person-centered care plan was proposed to reach the goal of reducing safety risks, optimize the quality of life, and identify opportunities to support personhood.11 Consequently, a collaborative approach that improves the quality of care for patients with dementia, increases adherence to dementia guidelines, and decreases behavioral problems is recommended.13–15
In October 2014, a dementia collaborative care model was established at Changhua Christian Hospital, a medical center in Changhua, Taiwan. Team members include physicians (including neurologists, psychiatrists, gerontologists, and primary care physicians), psychologists, social workers, dieticians, occupational therapists, pharmacists, and nursing case managers. When a diagnosis of dementia or mild cognitive impairment has been made, a face-to-face interview is arranged between collaborative care team members and patients residing in the community as well as their caregivers. Assessments include the patient’s cognitive, functional, and living status, home environment, and behavior and psychological symptoms, as well as the caregivers’ burden, mood, and their preferences of care. After assessments by the team, an individualized care plan is formed. The care team addresses 15 different care needs (Table 1) containing mostly quality measures and the needs of the patients and their caregivers.10,11,16 Details of the content of the assessment for each care need have been published in our previous study.17 When assessments are abnormal (e.g. if there is a high Zarit's caregiver burden or risk of falls score), the care team addresses the care need and introduces corresponding education and resources.
 |
Table 1 Fifteen Care Needs Addressed by Changhua Christian Hospital |
Most previous studies have focused on the prevalence of various care needs of patients with dementia.18–22 In our previous study, we tried to group care needs as a basic care bundle for PLWD and their caregivers using the Apriori algorithm, a data mining method which reveals statistical correlations among attributes by establishing threshold values of support and confidence.17,23 The basic care bundle consisted of five care needs: appropriate schedule of activities, regular outpatient follow-up treatment, introduction and referral of social resources, referral to family support groups and care skills training, and health education for dementia and behavioral and psychological symptoms of dementia.17
Because the clinical presentations of different etiologies of dementia are distinct, it is reasonable to postulate that their care needs are also different. Gender differences may also affect the care needs. A previous study found that males were associated with more unmet needs in both activities of daily living (ADL) and instrumental ADL.24 However, fewer studies have focused on the care needs for a specific etiological or gender group of PLWD. A previous study reported that patients with AD required more care to prevent traffic accidents and getting lost, while patients with vascular dementia required more care to prevent falls when a diagnosis had been made.17 Another study focusing on female patients with AD concluded that 75–84 year-old patients with very mild dementia (clinical dementia rating of 0.5) should be helped to establish a safe home environment.25
At our hospital, the prevalence of young-onset dementia is higher in patients with VCI than in those with general dementia, especially male subjects, who are usually taken care of by their younger spouses. The study team speculated that the care needs of male subjects with VCI may be different to those with general dementia. Therefore, the aim of the study was to elucidate specific care bundles for male patients with VCI and their caregivers by using the Apriori algorithm and then to compare the results with similar studies in order to further clarify the care needs in specific dementia subgroups.
Patients and Methods
Patients diagnosed with mild cognitive impairment or dementia at the memory clinic of Changhua Christian Hospital from November 2015 to June 2019 were enrolled. A total of 389 male patients with VCI were identified. International Society for Vascular Behavioral and Cognitive disorders (VASCOG) criteria were used to diagnose VCI.26 Patients who met the criteria for both possible AD according to the National Institute on Aging-Alzheimer’s Association (NIA-AA)27,28 and possible major vascular cognitive disorders according to the VASCOG were classified as having mixed dementia, and were excluded from the study. The clinical trial was approved by the Institutional Review Board of Changhua Christian Hospital (CCH IRB 160165). The need for informed consent was waived by the Institutional Review Board of Changhua Christian Hospital because the design of the study was a retrospective data analysis. All data including assessment results (such as ADL score for Care 2, Zarit’s caregiver burden score for Care 13), and team-selected care need numbers (as listed in Table 1) were recorded in electronic medical charts with the highest confidentiality and in compliance with the Declaration of Helsinki. All data needed in the present study were extracted by our information technology department after deleting any personalized information. The demographic information of the male patients with VCI including age and clinical dementia rating (CDR) score were recorded (Table 2). A majority of the included patients were aged 75 years and older (75.3%) and had mild dementia (CDR=1, 39.3%). Subjects with a CDR score of 3 were further classified as having severe dementia and extremely severe dementia. In this study, extremely severe dementia indicated nonresponsive to external stimuli and unable to communicate, and these patients met the criteria for hospice care provided by the Taiwan National Health Insurance program.
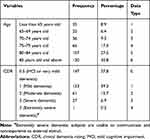 |
Table 2 Information of the Male Patients with VCI |
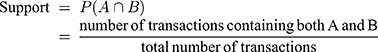
The aim of this study was to identify care need combinations for male patients with VCI and their caregivers in order to provide holistic care since patients with different ages and dementia severity may need different combinations of care needs. The Apriori algorithm was used to identify statistical correlations among attributes by setting up support, confidence, and lift.17,25 Jhang et al17 and Lin et al25 previously reported that the Apriori algorithm was a very effective approach to identify care bundles for patients with dementia and their caregivers. Therefore, we used the Apriori algorithm in this study. The descriptions of support, confidence, and lift are as follows.17,25,29 The support of A ⇒ B is calculated by the percentage of transactions consisting of both A and B in the database expressed by Equation (1):
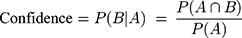
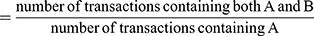
The confidence of A ⇒ B is to compute the accuracy of the rule based on the proportion of transactions in the database containing A and also containing B simultaneously depicted in Equation (2):
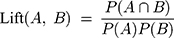
Lift in Equation (3) is to measure the correlation between A and B. If a lift is one, A and B are statistically independent indicating no rule will be generated containing either event. In contrast, if a lift is larger than one, A and B are dependent and positive correlated. In practice, analysts tend to prefer rules with either high support or high confidence, and usually both.30
The Apriori algorithm in IBM SPSS Modeler 14.1 was used, and the notations of data type in age and CDR are depicted in Table 2. The input variables for antecedents were age and CDR. The 15 care needs described in Table 1 and developed by the dementia collaborative care team at Changhua Christian Hospital were classified as both antecedents and consequents. In doing so, the analyst could identify whether there was any association between the care need combinations and age and CDR of the male patients with VCI. The notations for each care need adopted a binary data set, i.e., 0 and 1. If a particular care need was applied to a patient, a value of 1 was assigned. If not, a value of 0 was used. Minimum support, minimum confidence, and lift were set to 10%, 90%, and greater than one, respectively. The rules with higher support values were care bundles that could fulfill the majority of the patients’ needs. On the other hand, the rules with relatively lower support values were the care bundles that may only be applicable to a small portion of the patients, i.e., special needs.17,25
Results
A total of 22 rules summarized in Appendix were generated by the Apriori algorithm with support of 10%, confidence of 90%, and lift greater than 1. The meanings of the care combinations are explained below. For instance, there were 47 cases for Rule 1 out of the 389 male patients with VCI with support of 12.05%, confidence of 95.75%, and lift of 1.32. Rule 1 indicated that a male patient with mild vascular dementia required appropriate schedule of activities (Care 3), introduction and referral of social resources (Care 12), and education for dementia and behavioral and psychological symptoms of dementia (Care 15) along with regular outpatient follow-up treatment (Care 9). In Rule 2, Care 3, Care 12, referral to family support groups and care skills training (Care 13), care for the mood of the caregiver (Care 14), and Care 9 could be viewed as a care bundle.
The support values ranged from 10% to 26.41% in these 22 rules. In order to categorize the rules effectively, rules were divided into two categories according to a support of 20% and above and 10% but less than 20%. The general philosophy was that rules that had both high support and confidence values could be considered as the basic requirements for the male patients with VCI. Tables 3 and 4 provide two and seven generalized rules for the rules with support of 20% and above and 10% but less than 20%, respectively. That is, nine generalized rules were found in this study.
 |
Table 3 Two Generalized Rules with Support of 20% and Above |
 |
Table 4 Seven Generalized Rules with Support of 10% but Less Than 20% |
The first generalized rule showed that Care 9, Care 12, Care 13, and Care 15 could be viewed as a care bundle (Table 3). In the second generalized rule, Care 3, Care 9, and Care 15 were associated with either Care 12 or Care 13. In order to provide more comprehensive care, Care 3, Care 9, Care 12, Care 13, and Care 15 could take into account the five basic care needs for a larger portion of the male patients with VCI.
The first generalized rule with three similar rules indicated that Care 3, Care 9, Care 13, Care 14, and Care 15 along with Care 12 could be viewed as a care bundle (Table 4). There were four similar rules in the second generalized rule, and Care 9, Care 12, Care 13, and Care 15 were linked with Care 3 or Care 14. Only one rule was summarized in the third generalized rule, indicating that Care 9, Care 12, Care 13, and Care 14 could be considered to be a care combination. Three similar rules were summarized in the fourth generalized rule showing that male patients with mild vascular dementia required Care 9 and Care 15 along with either Care 3 or Care 12. The fifth generalized rule indicated that male patients with mild vascular dementia needed Care 9, Care 12, Care 13, and Care 15. The sixth generalized rule showed that Care 9, Care 12, and Care 13 were associated with Care 3 for male patients with mild vascular dementia. The seventh rule indicated that Care 6 and Care 12 were related to Care 9, Care 13, or Care 15. It is worth noting that three generalized rules (fourth, fifth, and sixth) identified the care needs for male patients with mild vascular dementia. Therefore, Care 3, Care 9, Care 12, Care 13, and Care 15 could be considered to be a care bundle for male patients with mild vascular dementia.
In summary, Care 3, Care 9, Care 12, Care 13, and Care 15 were the five basic care needs for all of the male patients with VCI including those with mild vascular dementia based on the findings in Tables 3 and 4. Moreover, Care 14 could be implemented via all five basic care bundles since this care need was sometimes associated with the five basic care needs in Table 4. That is, the case hospital might take these six care needs for male patients with VCI into consideration in order to provide more comprehensive care.
Discussion
The present study identified a care bundle consisting of six care needs for male VCI patients and their caregivers. The six care needs were appropriate schedule of activities (Care 3), regular outpatient follow-up treatment (Care 9), introduction and referral of social resources (Care 12), referral to family support groups and care skills training (Care 13), care for the mood of the caregiver (Care 14), and health education for dementia and behavioral and psychological symptoms of dementia (Care 15). These care needs are consistent with previous studies. Black et al reported that the most common unmet needs of community-living PLWD were home and personal safety, general health care, ADL, and management of behavioral and psychological symptoms of dementia.22 For the caregivers, resource referral and education was the most common unmet need followed by caregiver mental health care.18 The European Actifcare study reported that arranging daytime activities, company and psychological distress were the most common unmet needs for caregivers.21 Eichler et al reported that the most frequent unmet needs of patients with primary care dementia were nursing treatment and care, social counseling and legal support, and pharmaceutical treatment and care.19 The value of this research is to combine the care needs through a scientific-based method. Through the proposed care bundle, a collaborative care team can provide more efficient care for male VCI patients.
Table 5 summarizes the results of the present study with past similar articles. Except for the five basic care needs for PLWD and their caregivers,17 the present study highlights that more attention should be paid to the mood of the caregiver caring for male patients with VCI. Nearly 20% of the caregivers in this study had depressive mood as assessed by the Center for Epidemiologic Studies-Depression (CES-D) scale. Depression in caregivers caring for people with dementia can cause severe problems for both the caregiver and the person with dementia, as it has been reported to compromise the caregivers’ physical health31 and increase the risk of the caregiver contemplating suicide.32 Depression in caregivers can also have a direct effect on the persons with dementia, resulting in a more rapid cognitive decline33 and a higher risk of premature nursing home placement.34 Therefore, the mood of caregivers caring for males with VCI should be carefully assessed. Appropriate and prompt interventions should be implemented if depression is detected. There are several reasons to explain why care for the mood of the caregiver was addressed in this specific population. First, more than 65% of caregivers are female, and about 30% of caregivers are spouses in Taiwan.35,36 Since the present study targeted male subjects, more than 75% of the caregivers were predicted to be female. Several studies have reported that female caregivers of people with dementia have a higher risk of depressive mood and excessive care burden.36,37 Moreover, patients with VCI have been reported to have a lower neuropsychiatric inventory caregiver distress scale and lower emotional burden than patients with AD.8,38 In our previous study of 93 male and female patients with VCI, we found care that for fall prevention, but not the mood of the caregiver, should be incorporate into five basic care needs.17 Second, the functional status seemed to be worse in very mild dementia patients with VCI than AD due to focal neurological deficits. Because the team-approached assessment was conducted when the patient was first diagnosed, the majority of our study population had very mild to mild dementia. AD patients have relative preserved functions at these stages. ADL and instrumental activities of daily living dependency have been reported to be significant predictors for caregiver burden and depression.39
 |
Table 5 Frequent Combinations of Care Needs for Different Etiology of Dementia |
The care need of fall prevention was identified in VCI subjects in our previous study17 but it was not identified in the present study. The most likely reason is that elderly female Chinese have been reported to have a high risk of falls.40 That is, when assessing female VCI subjects, fall prevention should be evaluated carefully. A comparison of the care bundles in the patients with AD or VCI is listed in Table 5.
Although not constantly combined with all five basic care needs, preventing traffic accidents and getting lost is also frequently addressed in male patients with VCI. A previous study found that people with VCI had a higher frequency of wandering than those with AD,41 and that is led to getting lost outside in those with preserved walking ability. Gender differences have been also observed in spatial memory and efficiency in navigation.42 A previous study reminded care teams to pay attention to the problem of getting lost not only in patients with AD but also in male patients with VCI.17 In addition, the authors did not find specific care needs in relation to the severity of VCI because most of the study participants (77.1%) had a CDR score of 0.5 and 1.
The strength of present study is the relatively large number of case and that we only included male patients with pure VCI (excluding those with a mixed etiology). In addition, the care bundles were formed by combining the care needs in this specific population using a scientific method. Most previous studies have only shown the percentage of each unmet need for PLWD and their caregivers.17–21 Another strength is the precise selection of care needs. Through shared decision making between care teams, PLWD, and caregivers, the care needs were addressed by experienced collaborative team members. Elementary dementia case managers may be able to better understand the care focus by using the results of the present study.
There are also some study limitations. First, there is no universal approach to set up support and confidence values for the Apriori algorithm. Generally, a higher confidence value, for example 90% or above, is recommended to study the associations of attributes. Setting a support value is also essential because a higher support value reduces the number of rules that might result in missing some essential rules with low frequencies. However, a lower support value results in a large number of rules that might make it more difficult to determine whether the rules are meaningful. Therefore, there is a trade-off between higher or lower support values. In this study, we obtained the results using different support value intervals to balance this condition. Second, some important care needs, including early dementia evaluation and diagnosis and advanced care planning reported in previous reviews,10,16 were not included in our care need list. Because of the convenience and accessibility to medical care in Taiwan, PLWD and their caregivers usually receive a final etiological diagnosis within 1 month after completing evaluations. Since 2016, advanced care planning has been implemented for every PLWD who can name a surrogate decision maker at our hospital. Third, we did not include the characteristics of the caregivers, which may also have influenced the choice of care needs.
Conclusion
The basic care combinations for male VCI patients and their caregivers are composed of six care needs, including appropriate schedule of activities, regular outpatient follow-up treatment, introduction and referral of social resources, referral to family support groups and care skills training, care for the mood of the caregiver, and health education for dementia and behavioral and psychological symptoms of dementia. Preventing traffic accidents and getting lost is also a common care need in male patients with VCI. Collaborative care teams should pay more attention to these care needs when assessing this specific population.
Acknowledgment
This work is supported partially by China Medical University (CMU109-MF-91), Ministry of Science and Technology, Taiwan (MOST 107-2320-B-039-032-MY3), the peak project and thematic project of Academia Sinica, Taiwan, the higher education sprout project by the Ministry of Education, Taiwan via “Drug Development Center of China Medical University” from The Featured Areas Research Center Program, and short-term visiting program for domestic scholars of Academia Sinica, Taiwan.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. Kai-Ming Jhang, Wen-Fu Wang, Hao-Fang Chang, and Yu-Huei Liu contributed equally to this work as first authors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. United Nations. World Population Ageing. New York: Department of Economic and Social Affairs, Population Division; 2015.
2. Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–2734. doi:10.1016/S0140-6736(17)31363-6
3. Statistical Yearbook of Interior 2018. Available from: https://www.moi.gov.tw/stat/news_detail.aspx?sn=13742.
4. Sun Y, Lee H-J, Yang S-C, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PLoS One. 2014;9(6):e100303. doi:10.1371/journal.pone.0100303
5. Wu Y-T, Lee H-Y, Norton S, et al. Prevalence studies of dementia in mainland china, Hong Kong and Taiwan: a systematic review and meta-analysis. PLoS One. 2013;8(6):e66252. doi:10.1371/journal.pone.0066252
6. Dichgans M, Leys D. Vascular cognitive impairment. Circ Res. 2017;120(3):573–591. doi:10.1161/CIRCRESAHA.116.308426
7. Ruitenberg A, Ott A, van Swieten JC, et al. Incidence of dementia: does gender make a difference? Neurobiol Aging. 2001;22(4):575–580. doi:10.1016/S0197-4580(01)00231-7
8. D’Onofrio G, Sancarlo D, Panza F, et al. Neuropsychiatric symptoms and functional status in alzheimer’s disease and vascular dementia patients. Curr Alzheimer Res. 2012;9(6):759–771. doi:10.2174/156720512801322582
9. Graff-Radford J. Vascular cognitive impairment. Continuum. 2019;25(1):147–164.
10. Khanassov V, Vedel I. Family physician-case manager collaboration and needs of patients with dementia and their caregivers: a systematic mixed studies review. Ann Fam Med. 2016;14(2):166–177.
11. Molony SL, Kolanowski A, Van Haitsma K, Rooney KE. Person-centered assessment and care planning. Gerontologist. 2018;58(suppl_1):S32–S47. doi:10.1093/geront/gnx173
12. Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;5(1):CD008345.
13. Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148–2157.
14. Ganz DA, Koretz BK, Bail JK, et al. Nurse practitioner comanagement for patients in an academic geriatric practice. Am J Manag Care. 2010;16(12):e343–e355.
15. Vickrey BG, Mittman BS, Connor KI, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145(10):713. doi:10.7326/0003-4819-145-10-200611210-00004
16. Sanders AE, Nininger J, Absher J, Bennett A, Shugarman S, Roca R. Quality improvement in neurology: dementia management quality measurement set update. Neurology. 2017;88(20):1951–1957. doi:10.1212/WNL.0000000000003917
17. Jhang K-M, Chang M-C, Lo T-Y, et al. Using the apriori algorithm to classify the care needs of patients with different types of dementia. Patient Prefer Adherence. 2019;13:1899–1912. doi:10.2147/PPA.S223816
18. Black BS, Johnston D, Rabins PV, Morrison A, Lyketsos C, Samus QM. Unmet needs of community-residing persons with dementia and their informal caregivers: findings from the maximizing independence at home study. J Am Geriatr Soc. 2013;61(12):2087–2095. doi:10.1111/jgs.12549
19. Eichler T, Thyrian JR, Hertel J, et al. Unmet needs of community-dwelling primary care patients with dementia in Germany: prevalence and correlates. J Alzheimers Dis. 2016;51(3):847–855. doi:10.3233/JAD-150935
20. Johnston D, Samus QM, Morrison A, et al. Identification of community-residing individuals with dementia and their unmet needs for care. Int J Geriatr Psychiatry. 2011;26(3):292–298. doi:10.1002/gps.2527
21. Kerpershoek L, de Vugt M, Wolfs C, et al. Needs and quality of life of people with middle-stage dementia and their family carers from the European actifcare study. When informal care alone may not suffice. Aging Ment Health. 2018;22(7):897–902. doi:10.1080/13607863.2017.1390732
22. Black BS, Johnston D, Leoutsakos J, et al. Unmet needs in community-living persons with dementia are common, often non-medical and related to patient and caregiver characteristics. Int Psychogeriatr. 2019;31(11):1643–1654. doi:10.1017/S1041610218002296
23. Han J, Kamber M. Data Mining: Concepts and Techniques.
24. Zhou Y, Slachevasky A, Calvo E. Health conditions and unmet needs for assistance to perform activities of daily living among older adults with dementia in Chile. Int J Geriatr Psychiatry. 2018;33(7):964–971. doi:10.1002/gps.4879
25. Lin YS, Wang WF, Liu YH, et al. The study of care targets combination in women with alzheimer’s disease: a case study in a medical center in central Taiwan. J Qual. 2020;27(1):1–25. doi:10.6220/joq.202002_27(1).0001
26. Sachdev P, Kalaria R, O’Brien J, et al. Diagnostic criteria for vascular cognitive disorders: a VASCOG statement. Alzheimer Dis Assoc Disord. 2014;28(3):206–218. doi:10.1097/WAD.0000000000000034
27. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to alzheimer’s disease: recommendations from the National Institute on aging-alzheimer’s Association workgroups on diagnostic guidelines for alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–279. doi:10.1016/j.jalz.2011.03.008
28. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–269. doi:10.1016/j.jalz.2011.03.005
29. Chen WJ, Wang WF, Liu YH, et al. Using apriori algorithm to explore the influence of pressure from patients with dementia on caregivers from a medical center in Taiwan. J Qual. 2019;26(6):395–418. doi:10.6220/joq.201912_26(6).0004
30. Larose DT. Discovering Knowledge in Data: An Introduction to Data Mining. Hoboken, NJ: John Wiley & Sons; 2005.
31. Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62:126–137.
32. O’Dwyer ST, Moyle W, Zimmer-Gembeck M, De Leo D. Suicidal ideation in family carers of people with dementia. Aging Ment Health. 2016;20(2):222–230. doi:10.1080/13607863.2015.1063109
33. Norton MC, Clark C, Fauth EB, et al. Caregiver personality predicts rate of cognitive decline in a community sample of persons with alzheimer’s disease. The Cache County Dementia Progression Study. Int Psychogeriatr. 2013;25(10):1629–1637. doi:10.1017/S1041610213001105
34. Coehlo DP, Hooker K, Bowman S. Institutional placement of persons with dementia: what predicts occurrence and timing? J Fam Nurs. 2007;13(2):253–277. doi:10.1177/1074840707300947
35. Ku L-JE, Chang S-M, Pai M-C, et al. Predictors of caregiver burden and care costs for older persons with dementia in Taiwan. Int Psychogeriatr. 2019;31(6):885–894. doi:10.1017/S1041610218001382
36. Yan G-J, Wang W-F, Jhang K-M, Lin C-W, Wu -H-H. Association between patients with dementia and high caregiving burden for caregivers from a medical center in Taiwan. Psychol Res Behav Manag. 2019;12:55–65. doi:10.2147/PRBM.S187676
37. Pillemer S, Davis J, Tremont G. Gender effects on components of burden and depression among dementia caregivers. Aging Ment Health. 2018;22(9):1156–1161. doi:10.1080/13607863.2017.1337718
38. D’Onofrio G, Sancarlo D, Addante F, et al. Caregiver burden characterization in patients with alzheimer’s disease or vascular dementia. Int J Geriatr Psychiatry. 2015;30(9):891–899. doi:10.1002/gps.4232
39. Springate BA, Tremont G. Dimensions of caregiver burden in dementia: impact of demographic, mood, and care recipient variables. Am J Geriatr Psychiatry. 2014;22(3):294–300. doi:10.1016/j.jagp.2012.09.006
40. Peng K, Tian M, Andersen M, et al. Incidence, risk factors and economic burden of fall-related injuries in older Chinese people: a systematic review. Inj Prev. 2019;25(1):4–12. doi:10.1136/injuryprev-2018-042982
41. Bathgate D, Snowden JS, Varma A, et al. Behaviour in frontotemporal dementia, alzheimer’s disease and vascular dementia. Acta Neurol Scand. 2001;103(6):367–378. doi:10.1034/j.1600-0404.2001.2000236.x
42. Gagnon KT, Thomas BJ, Munion A, et al. Not all those who wander are lost: spatial exploration patterns and their relationship to gender and spatial memory. Cognition. 2018;180:108–117. doi:10.1016/j.cognition.2018.06.020
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.