Back to Journals » International Journal of General Medicine » Volume 13
Cardiovascular System Affection and Its Relation to First-Year Mortality in Patients Initiating Maintenance Hemodialysis
Authors Ali OM, Sayed AA , Mohammed WS, Mohammed RR
Received 17 January 2020
Accepted for publication 12 June 2020
Published 9 July 2020 Volume 2020:13 Pages 379—385
DOI https://doi.org/10.2147/IJGM.S242549
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Omaima Mohamed Ali,1 Aml Ahmed Sayed,1 Wafaa Salah Mohammed,2 Ragaa Ramadan Mohammed3
1Internal Medicine Department, Faculty of Medicine, Aswan University, Aswan, Egypt; 2Clinical Pathology Department, Faculty of Medicine, Aswan University, Aswan, Egypt; 3Internal Medicine Department, Faculty of Medicine, Al-Azhar University for Girls, Cairo, Egypt
Correspondence: Omaima Mohamed Ali
Department of Internal Medicine, Faculty of Medicine, Aswan University, Aswan 81528, Egypt
Tel +201005373193
Fax +20973480449
Email [email protected]
Background: The incidence of end-stage renal disease (ESRD) has increased by 30– 40% in the last decade. These patients have a higher mortality rate of 3– 8 times compared to the general population. In the present study, we aimed to detect cardiovascular complications and their relation to the first-year mortality rate in patients on hemodialysis in Aswan University Hospital, upper Egypt.
Patients and Methods: Our study was a cross-sectional study which was done at the hemodialysis unit in Aswan University Hospital from May 2016 to May 2018. The study included 100 patients with ESRD on regular hemodialysis (first year on programmed hemodialysis). All patients were subjected to full clinical examination and laboratory studies includngd complete blood count (CBC), kidney function tests, serum calcium and phosphorus level, parathormone (PTH) hormone, serum albumin level, C-reactive protein (CRP), echocardiography and electrocardiogram (ECG), and lateral abdominal x-ray for detection of aortic calcification.
Results: The present study included 47 males and 53 females, with a mean age of 50.6 ± 13.89 years. The main risk factors for patients with ESRD were hypertension (48%) followed by diabetic nephropathy (36%), glomerulonephritis (15%), idiopathic etiology (11%), obstructive uropathy (8%), lupus nephritis (6%), polycystic kidney disease (4%) and cardio renal syndrome (1%). Twenty-seven deaths have been noted during the first year of dialysis treatment. The leading causes of death were cardio-vascular events (66, 67%), infection (22, 22%) and malignancy (11, 11%), The most common cardiovascular events were myocardial infarction (27.8%), sudden cardiac death (SCD) (27.8%) and heart failure (22.2%).
Conclusion: In conclusion, our study showed that the main risk factors for ESRD patients in Aswan University Hospital are hypertensive nephrosclerosis, diabetic nephropathy, glomerulonephritis and idiopathic etiology, and the main causes of first-year mortality were cardiovascular events followed by infection and malignancy.
Keywords: end-stage renal disease, cardiovascular complication, mortality rate
Introduction
Chronic kidney disease (CKD) is one of the leading causes of mortality and morbidity worldwide. Recent epidemiological studies reported that CKD, especially stage 3, affects almost 11–13% of the global population.1 CKD is defined as a progressive loss of kidney function or glomerular filtration rate (GFR) <60 mL/min/1.73 m2, that persists for more than three months.2 According to a 2004 global consensus developed by Kidney Disease Improving Global Outcomes (KDIGO), CKD is classified into five stages based on the degree of kidney failure and albuminuria.3 End-stage renal disease (ESRD) is the final stage of CKD is characterized by irreversible loss of renal functions and the need for renal replacement therapy (RRT) or transplantation.4 ESRD represents an emerging healthcare challenge due to the exponential increase in its incidence rates over the past few decades owing to increased longevity of the population and the epidemic of diabetes.5 The incidence of ESRD was reported to be around 74 per million while the prevalence of patients on regular dialysis is 264 per million in Egypt.6 However, the prevalence of ESRD in Egypt has risen to 483 patients per million according to the 9th Annual Report of The Egyptian Renal Registry provided by Egyptian Society of Nephrology and Transplantation (ESNT).7
ESRD is a major cause of mortality and morbidity as well, previous reports showed that patients with ESRD had a very poor prognosis and higher mortality than general population.8 Moreover, ESRD is a major risk factor for various comorbidities including cardiovascular diseases (CVD), malnutrition, and diabetes.9 Therefore, early and good management of ESRD is the cornerstone to prevent its complications and improve the quality of life of the patients.10 RRT, whether hemodialysis or peritoneal dialysis, is the mainstay for the management of ESRD and to prevent its progression.
On the other hand, CVDs are the most commonly encountered comorbidities in CKD patients affecting up to 50% of patients undergoing dialysis.11 The patients with CKD are at relatively high risk of occurrence of ischemic heart diseases, hypertension, congestive heart failure, cardiac arrhythmias and valvular calcification.12 Although it is widely known that the occurrence of CVDs in ESRD patients is a consequence of the underlying hypertension and diabetes mellitus, recent reports suggested that ESRD is an independent risk factor by itself for the development of CVDs.13 Besides being a common comorbidity in ESRD, CVDs are a major cause of mortality in hemodialysis patients; ESRD patients were found to have a 20 times higher risk of death from CVD events than the general population.14 Several observational studies have shown that the first 3 to 4 months of dialysis are associated with an increased risk of mortality.15
In spite of the high prevalence of CKD and risk factor of CVDs in the Middle East, there is a lack in the published literature about the effect of CVD on the mortality of the patients with ESRD in this area. Therefore, we conducted the present cross-sectional study to detect cardiovascular complications and its relation to the rate of first-year mortality in patients on maintenance hemodialysis.
Patients and Methods
Study Design, Setting, and Patients
Our study was a cross-sectional study that recruited patients with ESRD from the hemodialysis unit of the Internal Medicine Department in Aswan University Hospital during the period from May 2016 till May 2018. We included patients who were diagnosed with ESRD and were scheduled to undergo maintenance hemodialysis.
Exclusion Criteria
Acute renal failure, patients on dialysis more than one year, CKD patients not on dialysis.
Data Collection
We collected the following data from every eligible patient: demographic characteristics, duration since the start of hemodialysis, clinical examination findings, and laboratory investigations findings. The laboratory investigation included complete blood count (CBC), kidney function tests, serum calcium and phosphorus (Ph) level, parathormone (PTH) hormone, serum albumin level, C-reactive protein (CRP), echocardiography and electrocardiogram (ECG), and lateral abdominal x-ray for detection of aortic calcification.
Study Outcomes
The main outcome in the present study was the one-year mortality rates for ESRD patients who were scheduled for maintenance hemodialysis and its association with CVD events. Also determination of the correlation and significance between vascular calcification and serum phosphorus, PTH and CRP level.
Ethical Statement
We confirm that this study is consistent with international ethical standards and the applicable local regulatory guidelines. The study has no physical, psychological, social, legal, economic or other expected risks to the study participants. Participants in the study were informed of the objectives, methods, risks and benefits. A written informed consent has been obtained from every qualifying patient in the study. Our study was conducted in accordance with the Declaration of Helsinki for studies on human subjects. It was approved by the institutional review board of The Faculty of Medicine, Aswan University.
Statistical Analysis
Data entry, processing, and statistical analysis were carried out using Microsoft Excel 2007 (Microsoft Corporation, NY, and the USA) and SPS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 22 for Microsoft Windows. Quantitative data were described in terms of mean ± standard deviation (±SD), while qualitative data were expressed as frequencies (number of cases) and relative frequencies (percentages). Comparisons between quantitative variables were done using unpaired Student’s t-test for parametric data or Mann–Whitney Rank Sum test for non-parametric data. Chi-square test (X2) was performed for categorical variables. Survival analysis was done using the Kaplan–Meier method. A probability value (p-value) less than 0.05 was considered statistically significant.
Results
Our study included 100 patients with ESRD on regular hemodialysis in the hemodialysis unit of Internal Medicine Department in Aswan University Hospital. The majority of patients were females (53%) with a mean age of 50.6 ±13.89 years. The average body mass index (BMI) of the included patients was 24.61 ± 5.37 kg/m2. The most common cause of ESRD was hypertension (48%), followed by diabetic nephropathy (36%), glomerulonephritis (15%), idiopathic etiology (11%), and obstructive uropathy (8%), lupus nephritis (6%), polycystic kidney disease (4%) and cardio renal syndrome (1%). Among hemodialysis patients the most common vascular access was arteriovenous fistulas (73%), the rest of these patients were treated using catheter (25%) or permacath (2%). Risk factors of CVD were diabetes (65.5%), hypertension (62.1%), dyslipidemia (75.9%), smoking (17.2%), peripheral vascular disease (65.5%) and history of stroke (37.9%), as shown in Table 1.
 |
Table 1 Baseline Characteristics of the Included Patients |
Notably, 22% of the patients had vascular calcification, which was detected by abdominal x-ray imaging. There were statistically significant differences between patients with and without calcification in terms of PTH (p < 0.001), phosphorus level (p < 0.001) and CRP (p < 0.001), and patients with vascular calcification had significantly higher PTH, Ph, and CRP levels as shown in Tables 2 and 3, respectively. our study also showed that there were statistically significant correlations between vascular calcification, PTH, phosphorus and CRP level in a multivariate analysis, as shown in Table 4.
 |
Table 2 Correlation Between PTH, Ph Levels and Vascular Calcification |
 |
Table 3 Correlation Between CRP and Vascular Calcification |
 |
Table 4 Multivariate Analysis of Vascular Calcification, CRP, PTH, and Ph Levels |
Our study noted that there was insignificant correlation between anemia (hemoglobin level <11 mg/dL) and left ventricular hypertrophy (LVH) (p > 0.05) (Figure 1).
 |
Figure 1 Correlation between anemia and left ventricular hypertrophy. Abbreviation: LVH, left ventricular hypertrophy. |
In terms of one-year morality, the one-year mortality was 27% in our study. The most common causes of death were CVD events (66.67%), followed by infection (22.22%) and malignancy (11.11%) (Figure 2). The most common infections were pneumonia, diabetic foot and catheter-related infection. The most common CVDs were myocardial infarction (27.8%), sudden cardiac death (SCD) (27.8%), heart failure (22.2%), pulmonary embolism (11.1%), stroke (5.55%) and intracranial hemorrhage (5.55%), as shown in Table 5.
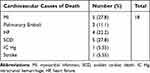 |
Table 5 Cardiovascular Causes of Death |
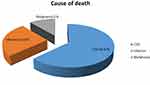 |
Figure 2 Causes of first-year mortality of all studied patients. Abbreviation: CVD, cardiovascular diseases. |
Analysis of ECHO and ECG findings of all studied patients reported that 23% of patients complained of left ventricular hypertrophy (LVH), 25% ischemic heart disease (IHD), 7% left bundle branch block (LBBB), 12% atrial fibrillation (AF), 10% suffered from ischemic dilated cardiomyopathy (IDCM), 3% heart failure (HF), 13% pericardial effusion (PE) and 2% rheumatic heart disease (RHD), as shown in Table 6.
 |
Table 6 ECHO and ECG Finding of All Studied Patients |
Survival analysis of the studied group using Kaplan–Meier reported that censored cases were 73.0%, mortality rate was 27%, mean survival time was 18.186 months, as shown in Figure 3A and B.
 |
Figure 3 (A and B) Survival analysis of the studied group using Kaplan–Meier, mean survival time is 18.186 months. |
Discussion
ESRD represents an economic burden for patients, healthcare providers, and the community. In addition, patients with ESRD had an increase in the risk of mortality compared to the normal population, especially from CVD causes.16 Our study showed that the first-year mortality of ESRD patients on hemodialysis was 27%, the CVD events followed by infection and malignancy. Our analysis also showed that ESRD patients with vascular calcification had significantly higher levels of CRP, phosphorus and PTH than patients without vascular calcification.
The currently published literature shows that more than half of patients on dialysis have at least one of the CVDs, while more than 30% present with evident ischemic events at the diagnosis of the CKD.13 The dramatic increase in the circulating uremic toxins, with subsequent oxidative stress and endothelial dysfunction, is thought to be the major contributor to the development of CVD in ESRD patients.17 Recently, it has been elaborated that CVDs are not only common comorbidities in ESRD patients, but they also have a negative impact on the patients’ survival; ESRD patients who had CVD events wres reported to have a higher rate of all-cause of mortality than patients without CVD.18 In our study, we found that ESRD patients had a high rate of one-year mortality (27%) which was attributed to CVD events in 66% of the cases. In agreement with our findings, a recent cohort study from China, which recruited 591 patients on dialysis, reported that CVD patients had higher mortality rates than non-CVD counterparts, while CVD was the most common cause of mortality in the included patients.19 Similarly, a previous meta-analysis study showed that the CVD significantly increases the hazards ratio of mortality among patients with ESRD. Another USRDS-based cohort study reported that acute myocardial infarction and other cardiac events were the most common causes of death in ESRD.20 Wang and colleagues21 also demonstrated that almost 25% of deaths in ESRD patients were attributed to sudden cardiac cause.
Vascular calcifications are mineral deposits on the wall of the vessels which are common complication in uremia due to impaired mineral metabolism; hyperphosphatemia and hyperparathyroidism were also found to be significantly associated with CVD mortality in hemodialysis patients, through vascular calcification, stiffening, increased pulse pressure, decreased coronary perfusion pressure, and LVH, aortic calcification was detected by x-ray which is a useful marker of vessel ossification.22 A strong relationship between elevated CRP levels and vascular calcification has also been documented in ESRD patients.23 Such findings can highlight that ESRD patients with CVDs have a higher degree of chronic inflammation than patients without CVDs. Previous reports showed that patients with ESRD had a higher level of chronic inflammation which is a strong predictor of mortality.24 We acknowledge that the present study has some limitations, as the study was conducted in one center only with small sample size.
Conclusion
Our study showed that the CVDs were the major contributor for one-year mortality in ESRD patients followed by infection. Moreover, patients with vascular calcification had a higher degree of inflammation which needed further investigations. Further multi-center studies with large sample size are still needed to assess the pathophysiology of higher mortality rate among dialysis patients with CVDs.
Disclosure
The authors reported no conflicts of interest in this work.
References
1. Hill NR, Fatoba ST, Oke JL, et al. Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-Analysis. PLoS One. 2016;11(7):e0158765. doi:10.1371/journal.pone.0158765
2. Inker LA, Astor BC, Fox CH, et al. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of CKD. Am J Kidney Dis. 2014;63(5):713–735. doi:10.1053/j.ajkd.2014.01.416
3. Levey AS, Eckardt K-U, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089–2100. doi:10.1111/j.1523-1755.2005.00365.x
4. Abbasi MA, Chertow GM, Hall YN. End-stage renal disease. BMJ Clin Evid. 2010;2010.
5. Bello AK, Nwankwo E, El Nahas AM. Prevention of chronic kidney disease: a global challenge. Kidney Int. 2005;68:S11–S17. doi:10.1111/j.1523-1755.2005.09802.x
6. Barsoum RS. Chronic kidney disease in the developing world. N Engl J Med. 2006;95:997–999. doi:10.1056/NEJMp058318
7. El-Ballat MA, El-Sayed MA, Emam HK. Epidemiology of end stage renal disease patients on regular hemodialysis in El-Beheira governorate, Egypt. Egypt J Hosp Med. 2019;76(3):3618–3625.
8. Tonelli M, Wiebe N, Culleton B, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17(7):2034–2047. doi:10.1681/ASN.2005101085
9. Eiam-Ong S, Sitprija V. Comorbidities in patients with end-stage renal disease in developing countries. Artif Organ. 2002;26(9):753–756. doi:10.1046/j.1525-1594.2002.07064.x
10. Perneger TV, Klag MJ, Whelton PK. Cause of death in patients with end-stage renal disease: death certificates vs registry reports. Am J Public Health. 1993;83(12):1735–1738. doi:10.2105/AJPH.83.12.1735
11. Schiffrin EL, Lipman ML, Mann JFE. Chronic kidney disease: effects on the cardiovascular system. Circulation. 2007;116(1):85–97. doi:10.1161/CIRCULATIONAHA.106.678342
12. Ronco C, McCullough P, Anker SD, et al. Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010;31(6):703–711. doi:10.1093/eurheartj/ehp507
13. Cozzolino M, Mangano M, Stucchi A, Ciceri P, Conte F, Galassi A. Cardiovascular disease in dialysis patients. Nephrol Dial Transplant. 2018;33(suppl_3):iii28–iii34. doi:10.1093/ndt/gfy174
14. Cozzolino M, Galassi A, Pivari F, Ciceri P, Conte F. The cardiovascular burden in end-stage renal disease. Contrib Nephrol. 2017;191:44–57.
15. Noordzij M, Jager KJ. Increased mortality early after dialysis initiation: a universal phenomenon. Kidney Int. 2014;85(1):12–14. doi:10.1038/ki.2013.316
16. Muntner P, He J, Hamm L, et al. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13(3):745–753.
17. Moradi H, Sica DA, Kalantar-Zadeh K. Cardiovascular burden associated with uremic toxins in patients with chronic kidney disease. Am J Nephrol. 2013;38(2):136–148. doi:10.1159/000351758
18. Ganesh SK, Hulbert-Shearon T, Port FK, Eagle K, Stack AG. Mortality differences by dialysis modality among incident ESRD patients with and without coronary artery disease. J Am Soc Nephrol. 2003;14(2):415–424. doi:10.1097/01.ASN.0000043140.23422.4F
19. Tong J, Liu M, Li H, et al. Mortality and associated risk factors in dialysis patients with cardiovascular disease. Kidney Blood Press Res. 2016;41(4):479–487. doi:10.1159/000443449
20. Bloembergen WE, Port FK, Mauger EA, Wolfe RA. Causes of death in dialysis patients: racial and gender differences. J Am Soc Nephrol. 1994;5(5):1231–1242.
21. Wang AY-M, Lam CW-K, Chan IH-S, Wang M, Lui S-F, Sanderson JE. Sudden cardiac death in end-stage renal disease patients. Hypertension. 2010;56(2):210–216. doi:10.1161/HYPERTENSIONAHA.110.151167
22. Palmer SC, Hayen A, Macaskill P, et al. Serum levels of phosphorus, parathyroid hormone,and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011;305:1119–1127. doi:10.1001/jama.2011.308
23. Kawaguchi T, Tong L, Robinson BM, et al. C-reactive protein and mortality in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephron Clin Pract. 2011;117(2):c167–c178. doi:10.1159/000320116
24. Endre ZH, Walker RJ. Biomarkers of cardiovascular risk in chronic kidney disease. Biomarkers Kid Dis. 2016.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
