Back to Journals » Infection and Drug Resistance » Volume 15
Carbapenems versus Cephalosporin or Piperacillin-Tazobactam as Perioperative Antibiotic Prophylaxis in Liver Transplant Recipients with Model for End-Stage Liver Disease Scores of ≥30: A Retrospective Study in a Chinese Population
Authors Zhang W, Chen Y , Zhang Y, Wang R, Wang W, Bai X, Liang T
Received 7 May 2022
Accepted for publication 1 August 2022
Published 12 August 2022 Volume 2022:15 Pages 4487—4494
DOI https://doi.org/10.2147/IDR.S373773
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Wei Zhang,1,2,* Ying Chen,1,2,* Yuntao Zhang,1,2 Rongrong Wang,3 Weili Wang,1,2 Xueli Bai,1,2 Tingbo Liang1,2,4,5
1Department of Hepatobiliary and Pancreatic Surgery, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 2Liver Transplant Center, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 3Department of Clinical Pharmacy, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 4Zhejiang Provincial Key Laboratory of Pancreatic Disease, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 5Key Lab of Combined Multi-organ Transplantation of the Ministry of Health, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tingbo Liang, Department of Hepatobiliary and Pancreatic Surgery, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China, Tel +86-571-87236688, Fax +86-571-87236739, Email [email protected]
Objective: Perioperative prophylaxis, commonly with a third-generation cephalosporin plus ampicillin or piperacillin-tazobactam, is usually employed to prevent infections in liver transplantation (LT) recipients. Patients with a high Model for End-Stage Liver Disease (MELD) score have an increased infection risk after LT. However, whether carbapenems could be used as surgical prophylaxis in these high-risk patients remains unclear. Therefore, this study aimed at comparing the effectiveness of carbapenems with that of cephalosporin or piperacillin-tazobactam for surgical prophylaxis in high-risk LT recipients with a MELD score ≥ 30.
Design or Methods: This retrospective study included adult patients with a MELD score ≥ 30 who underwent LT between May 2018 and September 2020. We comparatively analyzed the infection rate and outcome between patients using cefoperazone-sulbactam or piperacillin-tazobactam and those using carbapenems as surgical prophylaxis.
Results: This study included 105 LT recipients. Seventy-eight and 27 patients used non-carbapenem and carbapenem antibiotics, respectively, as surgical prophylaxis. The corresponding infection incidence rates within 30 days were 38.5% and 66.7% (p = 0.011). Multivariate analysis revealed that reoperation and the Child–Pugh score were independent risk factors for infections within 30 days after LT. The following four risk factors were associated with the 180-day post-LT survival: MELD score, vascular complication, intra-abdominal bleeding, and infection with carbapenem-resistant organisms (CROs). There was no significant difference in CRO infection incidence between the carbapenem and non-carbapenem groups (18.5% vs 11.5%; p = 0.345).
Conclusion: Carbapenem use as surgical prophylaxis was not associated with infection incidence within 30 days after LT, 180-day post-LT survival or CRO infection. Therefore, carbapenems are not superior to cephalosporin or piperacillin-tazobactam for perioperative antibiotic prophylaxis in LT recipients with a MELD score ≥ 30.
Keywords: perioperative prophylaxis, liver transplantation, infection, carbapenems, carbapenem-resistant organisms
Introduction
Infectious complications are major causes of morbidity and mortality after liver transplantation (LT). Because of the high rate of surgical-site infections (SSIs) in LT patients, perioperative prophylaxis is usually employed.1–4 Clinical studies have suggested that perioperative antibiotic prophylaxis is beneficial in reducing postoperative SSIs in patients who undergo solid-organ transplantation.5–7 The Infectious Diseases Society of America (IDSA)/American Society of Health-System Pharmacists (ASHP)/Surgical Infection Society (SIS)/Society for Healthcare Epidemiology of America (SHEA) guidelines recommend a third-generation cephalosporin plus ampicillin or piperacillin-tazobactam alone for perioperative antibiotic prophylaxis in LT recipients.8
Liver transplant recipients, particularly those with high-risk factors such as high Model for End-Stage Liver Disease (MELD) scores, are vulnerable to developing infections with multidrug-resistant (MDR) gram-negative bacilli because of the prolonged exposure to broad-spectrum antibiotics and frequent invasive procedures.9–11 The increasing prevalence of multidrug resistance, such as that by extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, has driven the increased use of carbapenems in clinical practice. However, clinicians must balance the risk of severe MDR infection with the risk of the development of carbapenem resistance. It remains inconclusive whether carbapenems can be used as surgical prophylaxis for high-risk patients who undergo LT.
The aim of this study was to compare the effectiveness of carbapenems with that of cephalosporin or piperacillin-tazobactam for perioperative antibiotic prophylaxis in high-risk LT recipients with a MELD score ≥30.
Patients and Methods
Study Design and Participants
Between May 2018 and September 2020, 585 adult patients (age > 18 years) underwent their first liver-only transplantation at the First Affiliated Hospital of Zhejiang University, School of Medicine, China. Of these patients, 117 had a MELD score of ≥30. From among these patients, six were excluded because they passed away within 7 days after LT and another six were excluded because they had pre-LT infections within one week before transplantation (2 patients had blood stream infections; 2 patients had peritonitis; 3 patients had chest infections and 1 patient had leg abscess). In the end, 105 LT patients had a MELD ≥30 and were without pre-LT infections. Perioperative antibiotic prophylaxis was administered for at least 72 h after LT. The induction immunosuppression regimen comprised basiliximab and corticosteroids and the maintenance regimen consisted of tacrolimus and mycophenolate mofetil with or without corticosteroids in the early stage after LT. Since Jan 1, 2015, organ procurement from executed prisoners had been completely ceased in China. No organs from executed prisoners were used in any case involved in this study.
Setting
The First Affiliated Hospital of Zhejiang University, School of Medicine is a 2200-bed tertiary care university hospital in Hangzhou, China. Over 3000 LTs have been performed until December 2020 at the LT center.
Data Collection and Definitions
The patients’ electronic case reports were reviewed, and the following variables were evaluated: recipients’ characteristics (age, sex, body mass index [BMI], MELD score, Child–Pugh score, underlying liver diseases, and pre-LT intensive care unit [ICU] stay), graft information (graft type, cold ischemia time, and warm ischemia time), procedure-related information (intraoperative blood loss, vascular complications, biliary complications, post-LT intra-abdominal bleeding, and reoperation), perioperative antibiotic prophylaxis regimens, post-LT conditions (vasopressor support, mechanical ventilation, and renal replacement therapy [RRT]), infection variables (time, location, and pathogen), and outcomes (180-day post-LT survival rate).
Infection was defined per the Centers for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN) 2019 criteria.5 However, because this was a retrospective study, only culture-positive infections were included in this study. Patients with positive blood cultures and peritoneal fluid, biliary juice, sputum, endotracheal aspiration, urine, and other samples according to the CDC/NHSN criteria were retrospectively evaluated by two experts to assess whether they had infections.
CRE is defined as Enterobacteriaceae that is resistant to at least one of the carbapenem antibiotics (ertapenem, meropenem, doripenem, or imipenem) or produce a carbapenemase according to the Centers for Disease Control and Prevention.12 Detection of carbapenem resistance is based Clinical and Laboratory Standards Institute (CLSI) breakpoints.13
Vascular complications included hepatic artery thrombosis, hepatic vein thrombosis, and portal vein thrombosis. Biliary complications included bile duct stenosis and bile leakage.
Statistical Analysis
Patients who received carbapenems as antibiotic prophylaxis were compared to those who received cephalosporin or piperacillin-tazobactam. Continuous variables were compared using Student’s t-test or Mann–Whitney U-test. Categorical variables were compared using Pearson’s chi-square or Fisher’s exact test when appropriate. All variables with a p-value ≤ 0.05 in the univariate analysis were included in the logistic regression and/or Cox regression for multivariable analysis. A p-value ≤ 0.05 was considered significant. All statistical calculations were performed with SPSS 25.
Results
This study population consisted of 105 patients who underwent their first liver-only transplantation. Among them, 78 patients (74.3%) received non-carbapenem antibiotics for surgical prophylaxis (piperacillin-tazobactam, 21 patients; cefoperazone-sulbactam, 57 patients), while 27 patients (25.7%) received carbapenems for surgical prophylaxis (meropenem, 24 patients; imipenem-cilastatin, 3 patients). The basic characteristics of the patients in the carbapenem and non-carbapenem groups are shown in Table 1. Patients in the carbapenem group had a worse perioperative condition: higher MELD score (35.2 ± 3.9 vs 33.4 ± 3.5; p = 0.030) and higher chances of pre-transplant ICU stay (44.4% vs 21.8%; p = 0.023) and vasopressor support within 24 h after transplantation (29.6% vs 3.8%; p = 0.001). In addition, a greater percentage of patients in the carbapenem group required mechanical ventilation for more than 72 h (55.6% vs 17.9%; p = 0.000). The two groups showed no significant differences in the rates of surgical complications, such as intra-abdominal hemorrhage, vascular complications, biliary complications, and reoperation.
 |
Table 1 Comparison of Patients Who Did and Did Not Receive Carbapenems as Antibiotic Prophylaxis |
Overall, 48 (45.7%) of the 105 patients developed infections within 30 days after LT, and 24 of these 48 patients (50.0%) had polymicrobial infections. In the carbapenem group, 18 patients (66.7%) had infections within a median of 7.5 (interquartile range [IQR] 1.0–17.25) days after LT. The most common pathogen was Enterococcus (25.9%), followed by Enterobacteriaceae (18.5%) (Table 2). And it was common for patients to have more than one site of infection after LT: 10 patients (37.0%) had intra-abdominal infections, 7 patients (25.9%) developed bacteremia and 11 patients (40.7%) had pneumonia. In the non-carbapenem group, 30 patients (38.5%) had infections within a median of 3.0 (IQR 1.0–7.25) days after LT. Enterobacteriaceae (18.0%) was the most common pathogen, followed by Enterococcus (14.1%). Eighteen patients (23.1%) had intra-abdominal infections, 17 patients (21.8%) developed bacteremia and 17 patients (21.8%) had pneumonia.
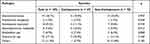 |
Table 2 Bacterial Pathogens of Infections |
Overall, 14 patients (13.3%) had CRO infections (carbapenem‐resistant Enterobacteriaceae and carbapenem‐resistant Acinetobacter baumannii, 6 patients each; carbapenem‐resistant Pseudomonas aeruginosa and carbapenem‐resistant Cupriavidus, 1 patient each). The two groups showed no significant difference in the proportion of CRO infections (18.5% vs 11.5%; p = 0.345) (Table 1).
A greater percentage of patients in the carbapenem group had infections within 30 days after LT (66.7% vs 38.5%; p = 0.011) (Table 1). In order to analyze whether prophylactic antibiotics was an independent risk factor of post-LT infections, the risk factors for infections were assessed by univariate and multivariate analyses (Table 3). Univariate analysis suggested that the following risk factors were associated with infection within 30 days after LT: prophylaxis with carbapenems, vasopressor support within 24 h after transplantation, ventilation for >72 h, reoperation, RRT > 3 days, and a high Child–Pugh score. Multivariate analysis showed that only reoperation (OR, 3.942; 95% CI, 1.004–15.468; p = 0.049) and a high Child–Pugh score (OR, 1.726; 95% CI, 1.183–2.519; p = 0.005) were independent risk factors for infections. Prophylaxis with or without carbapenems was not an independent risk factor for infections within 30 days after LT (OR, 1.940, 95% CI, 0.638–5.898, p = 0.243).
 |
Table 3 Univariate and Multivariate Analyses of Risk Factors for Infections After Liver Transplantation |
The 180-day survival rate of patients who underwent LT with MELD ≥30 was 81.9% in this study. The 180-day survival rates of patients in the carbapenem and non-carbapenem groups were 74.1% and 84.6%, respectively (p = 0.238) (Figure 1). We further analyzed the risk factors for 180-day survival after LT by Cox regression, and the results of this analysis are shown in Table 4. Univariate analysis suggested that five risk factors were associated with 180-day survival after LT, including the MELD score, vascular complications, RRT > 3 days, intra-abdominal bleeding, and CRO infection. Multivariate analysis identified four independent risk factors associated with 180-day survival post-LT, namely, MELD score (HR, 1.216; 95% CI, 1.040–1.422; p = 0.014), vascular complications (HR, 9.302; 95% CI, 1.769–48.914; p = 0.008), intra-abdominal bleeding (HR, 9.056; 95% CI, 2.185–37.541; p = 0.002), and CRO infection (HR, 6.669; 95% CI, 2.248–19.788; p = 0.001). Prophylaxis with or without carbapenems was not associated with the 180-day survival after LT. Regarding the cause of death, 9 patients (47.4%) died of infection. And 4 of the 9 patients had CRO infections.
 |
Table 4 Factors Associated with 180 Days of Survival in Patients After Liver Transplantation in the Cox Model |
 |
Figure 1 The 180-day post-transplant survival rate in patients who received carbapenems and those who received non-carbapenems for surgical prophylaxis (74.1% and 84.6%, log-rank p = 0.238). |
Discussion
Postoperative infections occur in up to 8–38% of LT patients, and are related to the patients’ poor nutritional status, comorbidities, the complexity of the surgical procedure, which requires penetration of the hepatobiliary system, and the use of immunosuppression.2,14,15 Antibiotic prophylaxis in solid organ transplantation has been described in a few studies.16–18 However, the benefits and disadvantages of prophylactic regimens in LT patients remain unclear because of inadequate evidence from current clinical trials.14 The optimal prophylactic antibiotic regimens should account for the risk factors of patients and local antibiotic resistance patterns. Transplant recipients with a high MELD score have additional risk factors such as poor underlying conditions, invasive procedures and use of catheters, exposure to broad-spectrum antibiotics, and colonization with MDR organisms. Moreover, according to the China Antimicrobial Surveillance Network (CHINET) 2018 report, the resistance rate of E. coli to piperacillin-tazobactam was 3.8–10.3%, and the resistance rate of K. pneumoniae to piperacillin-tazobactam was 28.7%-62%.19 On the basis of this background, we designed this study to determine whether carbapenems could be used for surgical prophylaxis to decrease the infection rate in LT recipients with a MELD score ≥30.
Our study included patients with a MELD score ≥30 who had undergone first-time liver-only transplantation, and we found that the overall incidence of infection was 45.7% within 30 days after LT. The incidence of infections was 66.7% in the carbapenem group and 38.5% in the non-carbapenem group. However, this difference may not be directly associated with antibiotic prophylaxis regimens because clinicians tend to prescribe carbapenems to patients with worse clinical conditions. And this was an important bias that might affect results. Therefore, we performed multivariate analyses and found out that only reoperation and the Child–Pugh score were independent risk factors for infections within 30 days after LT. Other studies have demonstrated that a prolonged ICU or hospital stay, high MELD scores, requirement of >4 units of red blood cells in the surgery, anastomotic leakage, donor infection, and post-transplant RRT were also risk factors for infections in LT.15,20 Some studies have suggested that prophylactic antibiotics may affect the incidence of SSIs in transplant recipients.16,17 However, none of these studies evaluated carbapenems as surgical prophylaxis in LT patients.
Liver transplant recipients are particularly vulnerable to developing CRO infection. The incidence of post-LT CRE infection varies among different centers, from 3% to 23%.21–23 In our previous study, the incidence of CRE infection was 6.7% within 30 days after LT, and patients with CRE infections had significantly lower 180-day survival rates (51.5% vs 92.4%, p < 0.001).24 Since the use of carbapenems is associated with an increased risk of CRO infection, we analyzed the incidence of CRO infection in this study.25 We found that 13.3% of patients developed CRO infections within 30 days after LT. And, the CRO infection rate did not differ significantly between the carbapenem and non-carbapenem groups. However, in our study, the number of CRO infection was relatively small to draw firm conclusions.
Finally, we found that the MELD score, vascular complications, intra-abdominal bleeding, and CRO infection were independent risk factors associated with the 180-day post-LT survival. Prophylaxis with carbapenems was not one of these factors, probably because cephalosporin or piperacillin-tazobactam was adequate to cover most pathogens and carbapenems would not further decrease the incidence of infection. Moreover, in this study, we did not observe an association between the use of carbapenems and CRO infection, which was one risk factor of post-LT survival.
Our study had some limitations. First, it was a monocentric retrospective study. Thus, our data may vary from the findings obtained at other centers. Moreover, we focused on culture-positive infection, which may have underestimated the overall incidence of infections. Second, the size of this study is relatively small; therefore, we were unable to perform subgroup analysis to determine whether highly selected patients may benefit from carbapenems. Third, this study did not include variable about MDR colonization prior to LT, which is a known risk factor of post-LT infections and could affect the prophylaxis selection, because we did not routinely screen LT candidates before LT.
Conclusion
We found that reoperation and the Child–Pugh score were independent risk factors for infections within 30 days after LT. Moreover, the MELD score, vascular complications, intra-abdominal bleeding, and CRO infection were independent risk factors for survival 180 days post-LT. The use of carbapenems for surgical prophylaxis was not associated with post-LT infection or survival. In this study, the use of carbapenems was not associated with CRO infection as well. Therefore, carbapenems are not superior to cephalosporin or piperacillin-tazobactam as perioperative antibiotic prophylaxis in liver transplantation recipients with a MELD score ≥30. The complexities of the clinical situation of individual LT patients will necessitate thoughtful prophylactic regimens. High-quality studies are needed to build a proper risk-stratification system to help guide the choice of prophylactic antibiotics.
Ethics Approval
This study complied with the guidelines of the Chinese Ethics Committee and the Declaration of Helsinki and was approved by the research ethics committee of the First Affiliated Hospital, Zhejiang University School of Medicine (IIT20220045A). All organs were donated voluntarily with written informed consent, and the organ donations were conducted in accordance with the Declaration of Istanbul. The data were anonymous, and the requirement for informed consent was waived for our retrospective study. Since Jan 1, 2015, organ procurement from executed prisoners had been completely ceased in China. No organs from executed prisoners were used in any case involved in this study.
Acknowledgments
We gratefully acknowledge our colleagues for their contribution to the transplant center and their comments on this study.
Funding
This project was supported by the Research Foundation of the First Affiliated Hospital of Zhejiang University, School of Medicine (IIT20200048C).
Disclosure
The authors report no conflicts of interest for this work and declare that there is no competing interest regarding the publication of this paper.
References
1. Blair JE, Kusne S. Bacterial, mycobacterial, and protozoal infections after liver transplantation–part I. Liver Transplant. 2005;11(12):1452–1459.
2. Kawecki D, Chmura A, Pacholczyk M, et al. Bacterial infections in the early period after liver transplantation: etiological agents and their susceptibility. Med Sci Monit. 2009;15(12):Cr628–637.
3. Paya CV, Hermans PE. Bacterial infections after liver transplantation. Eur J Clin Microbiol Infect Dis. 1989;8(6):499–504.
4. Romero FA, Razonable RR. Infections in liver transplant recipients. World J Hepatol. 2011;3(4):83–92.
5. Bartlett ST. Pancreatic transplantation after thirty years: still room for improvement. J Am Coll Surg. 1996;183(4):408–410.
6. Novick AC. The value of intraoperative antibiotics in preventing renal transplant wound infections. J Urol. 1981;125(2):151–152.
7. Ramos E, Karmi S, Alongi SV, Dagher FJ. Infectious complications in renal transplant recipients. South Med J. 1980;73(6):751–754.
8. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195–283.
9. Santoro-Lopes G, de Gouvêa EF. Multidrug-resistant bacterial infections after liver transplantation: an ever-growing challenge. World J Gastroenterol. 2014;20(20):6201–6210.
10. Herati RS, Blumberg EA. Losing ground: multidrug-resistant bacteria in solid-organ transplantation. Curr Opin Infect Dis. 2012;25(4):445–449.
11. van Duin D, van Delden C. Multidrug-resistant gram-negative bacteria infections in solid organ transplantation. Am J Transplant. 2013;13(Suppl 4):31–41.
12. Centers for Disease Control and Prevention. FAQs about choosing and implementing a CRE definition. Available from: https://www.cdc.gov/hai/organisms/cre/technical-info.html#Definition.
13. CDC/NHSN. CDC/NHSN surveillance definitions for specific types of infections. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf.
14. Almeida RA, Hasimoto CN, Kim A, Hasimoto EN, El Dib R. Antibiotic prophylaxis for surgical site infection in people undergoing liver transplantation. Cochrane Database Syst Rev. 2015;2015(12):Cd010164.
15. Kim SI. Bacterial infection after liver transplantation. World J Gastroenterol. 2014;20(20):6211–6220.
16. García Prado ME, Matia EC, Ciuro FP, et al. Surgical site infection in liver transplant recipients: impact of the type of perioperative prophylaxis. Transplantation. 2008;85(12):1849–1854.
17. Asensio A, Ramos A, Cuervas-Mons V, et al. Effect of antibiotic prophylaxis on the risk of surgical site infection in orthotopic liver transplant. Liver Transplant. 2008;14(6):799–805.
18. Berry PS, Rosenberger LH, Guidry CA, Agarwal A, Pelletier S, Sawyer RG. Intraoperative versus extended antibiotic prophylaxis in liver transplant surgery: a randomized controlled pilot trial. Liver Transplant. 2019;25(7):1043–1053.
19. Hu F, Guo Y, Yang Y, et al. Resistance reported from China antimicrobial surveillance network (CHINET) in 2018. Eur J Clin Microbiol Infect Dis. 2019;38(12):2275–2281.
20. Anesi JA, Blumberg EA, Abbo LM. Perioperative antibiotic prophylaxis to prevent surgical site infections in solid organ transplantation. Transplantation. 2018;102(1):21–34.
21. Giannella M, Bartoletti M, Morelli MC, et al. Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae after liver transplantation: the importance of pre- and posttransplant colonization. Am J Transplant. 2015;15(6):1708–1715.
22. Satlin MJ, Jenkins SG, Walsh TJ. The global challenge of carbapenem-resistant Enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis. 2014;58(9):1274–1283.
23. Pereira MR, Scully BF, Pouch SM, et al. Risk factors and outcomes of carbapenem-resistant Klebsiella pneumoniae infections in liver transplant recipients. Liver Transplant. 2015;21(12):1511–1519.
24. Chen Y, Wang WL, Zhang W, et al. Risk factors and outcomes of carbapenem-resistant Enterobacteriaceae infection after liver transplantation: a retrospective study in a Chinese population. Infect Drug Resist. 2020;13:4039–4045.
25. Kalpoe JS, Sonnenberg E, Factor SH, et al. Mortality associated with carbapenem-resistant Klebsiella pneumoniae infections in liver transplant recipients. Liver Transplant. 2012;18(4):468–474.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
