Back to Journals » Clinical Epidemiology » Volume 14
Cancer Diagnosis and Prognosis After Guillain–Barré Syndrome: A Population-Based Cohort Study
Authors Girma B , Farkas DK, Laugesen K , Skajaa N , Henderson VW , Boffetta P, Sørensen HT
Received 8 April 2022
Accepted for publication 5 July 2022
Published 19 July 2022 Volume 2022:14 Pages 871—878
DOI https://doi.org/10.2147/CLEP.S369908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Blean Girma,1 Dóra Körmendiné Farkas,2 Kristina Laugesen,2 Nils Skajaa,2 Victor W Henderson,2,3 Paolo Boffetta,4,5 Henrik Toft Sørensen2
1Department of Environmental Medicine and Public Health, Icahn School of Medicine, New York, NY, USA; 2Department of Clinical Epidemiology, Aarhus University Hospital and Aarhus University, Aarhus, Denmark; 3Departments of Epidemiology & Population Health and of Neurology & Neurological Sciences, Stanford University, Stanford, CA, USA; 4Stony Brook Cancer Center, Stony Brook University, Stony Brook, NY, USA; 5Department of Medical and Surgical Sciences, University of Bologna, Bologna, Italy
Correspondence: Henrik Toft Sørensen, Department of Clinical Epidemiology, Aarhus University Hospital and Aarhus University, Olof Palmes Allé 43-45, Aarhus, 8200, Denmark, Tel +45 87 16 82 15, Email [email protected]
Introduction: It is unclear whether Guillain–Barré syndrome (GBS) can be a marker of a paraneoplastic syndrome. We examined whether GBS is associated with cancer and whether the prognosis of GBS patients with cancer differs from that of other cancer patients.
Materials and Methods: We conducted a population-based cohort study of patients diagnosed with GBS between 1978 and 2017 using Danish registry-data. Main outcome measures were cancer incidence and mortality after cancer diagnosis. We calculated absolute risks of a cancer diagnosis, treating death as competing risk, and standardized incidence ratios (SIRs) as measures of relative risk. We matched each GBS cancer patient with up to 10 cancer patients without a GBS diagnosis and examined the six-month survival after cancer diagnosis using Cox regression analysis.
Results: We identified 7897 patients (58% male, median age 57 years) with GBS. During a median follow-up of 9.5 years, the one-year risk of cancer was 2.7% (95% confidence interval (CI), 2.4– 3.1). The SIR was increased throughout follow-up, but most noticeably during the first year after diagnosis (SIR: 3.35, 2.92– 3.83). SIRs were particularly elevated for hematologic cancers (SIR: 8.67, 6.49– 11.34), smoking-related cancers (SIR: 3.57, 2.81– 4.47), and cancers of neurological origin (SIR: 8.60, 5.01– 13.77). Lung cancer was the main contributor to the overall excess risk, which persisted after 36 months of follow-up (SIR: 1.17, 1.09– 1.25). The mortality rate ratio comparing patients diagnosed with any cancer within one year of their GBS diagnosis and matched GBS-free cancer cohort members was 1.56 (95% CI, 1.27– 1.90).
Conclusion: GBS patients had a three-fold increased risk of cancer diagnosis in the first year of follow-up. The absolute cancer risk was almost 3.0%. A GBS diagnosis was an adverse prognostic marker for survival following cancer diagnosis. Clinicians should consider occult cancer in patients hospitalized with GBS.
Keywords: Guillain–Barré syndrome, cancer, paraneoplastic syndrome, survival, risk, cohort
Introduction
Guillain–Barré syndrome (GBS) is an acute inflammatory polyradiculoneuropathy in which peripheral nervous system damage causes rapid muscle weakness.1 The condition is often life-threatening and can lead to lasting disability. GBS affects 1.1–1.8 per 100,000 people annually.2 Incidence increases with age, and men are more often affected than women.2 The exact etiology is unknown, but the condition may result from an autoimmune response directed against components of the peripheral nervous system.1 Within four weeks prior to GBS onset, approximately 40–70% of GBS patients have an antecedent infection, mainly of the respiratory system or the digestive tract.2 A case-control study showed that cancer can be a risk factor for GBS with the strongest associations for hematological cancer.3
Cancers can present with paraneoplastic neurological syndromes involving the central or peripheral nervous system, mediated by an autoimmune response.4 However, whether GBS is a marker of occult cancer remains unclear. Available evidence is limited to case reports5–18 and two small regional, single-hospital cohort studies, which included 435 and 109 GBS patients, respectively.19,20 In both cohorts, a two-fold increased incidence of cancer was reported among GBS patients compared with the cancer incidence expected in the general population, based on nine and 10 cancer cases, respectively.19,20 Most cases were diagnosed in close temporal proximity to the onset of GBS. Thus, the current evidence remains suggestive but insufficient to draw conclusions regarding an association between GBS and cancer, its directionality, and possible underlying mechanisms. Moreover, the prognosis for cancer associated with GBS is poorly understood. Two small recent studies suggested that paraneoplastic neuropathic syndromes are associated with a poor prognosis.21,22
In this large population-based cohort study using Danish nationwide registry data, we aimed to provide precise epidemiological evidence concerning the association between GBS and subsequent the risk and prognosis of cancer, and to investigate whether GBS may be a marker of underlying occult cancer.
Methods
Design and Data Sources
This cohort study was based on registry data covering the entire Danish population between January 1, 1978, and December 31, 2017 (cumulative source population: 8.6 million residents). Denmark has a free tax-supported healthcare system.23 Data sources included the Danish Civil Registration System,24 the Danish National Patient Registry,25 and the Danish Cancer Registry.26 We linked these data sources at the individual level using the unique 10-digit identifier assigned to all Danish residents at birth or upon immigration. In Denmark, unrestricted access to tax-financed health care is available to all legal residents.23
Patients with Guillain–Barré Syndrome
We used the Patient Registry to identify all patients with a first-time diagnosis of GBS (ICD-8 code 354 and ICD-10 code G61.0) during the study period. To do so, we searched all available records, ie, primary or secondary discharge diagnoses given in either the inpatient, outpatient clinic, or emergency department setting. The admission date of the hospitalization yielding a GBS diagnosis was set as the “index date”. Diagnosis codes for GBS in the Patient Registry have been found to be valid.27 We excluded patients with a cancer diagnosis before the index date. The Patient Registry contains complete nationwide information on hospital inpatient admissions since 1977 and on hospital outpatient clinic and emergency room contacts since 1995. Each hospital or outpatient clinic visit is recorded in the Patient Registry with one primary discharge diagnosis and one or more secondary discharge diagnoses coded according to the International Classification of Diseases, Eighth Revision between 1977 and 1993, and Tenth Revision thereafter.24
Follow-Up for Cancer Incidence and Mortality
Incident cancers were identified from the Cancer Registry.25 We considered all cancer types (except non-melanoma skin cancer), as well as site-specific cancers, grouped according to the annual cancer report published by the Danish Health Data Authority.28 We divided cancers into subgroups, including sex hormone-related cancers, hematologic cancers, immune-related cancers, gastrointestinal cancers, smoking-related cancers, and cancers of neurological origin.28 The Cancer Registry has recorded all incident cases of malignant neoplasms in Denmark since 1943 (mandatory since 1987), including information on morphology, histology, and cancer stage at the time of diagnosis. In 2008, reporting to the Cancer Registry became electronic through integration with patient administrative systems, and manual coding was partly replaced by an automatic coding logic. Diagnoses in the Cancer Registry have high validity, with 95–98% completeness and accuracy of recorded diagnoses.26 Cancer cases are coded according to the International Classification of Diseases, Tenth Revision. The extent of tumor spread at the time of diagnosis is classified as localized, regional, metastatic to distant sites, or unknown.
Information on mortality was extracted from the Civil Registration System23 which is updated daily for changes in vital status and migration among the entire Danish population. All diagnostic codes used in the study are listed in eTable 1 in the Supplement.
Statistical Analyses
We followed patients with GBS from their index date until the occurrence of cancer, death, emigration, or December 31, 2018, whichever came first. In all analyses, we divided the follow-up period into two categories: first year, and second and subsequent years. Most cancers have long latency periods, and particularly for cancers diagnosed during the first follow-up year, we assumed that the cancer was present but undetected prior to hospital admission for GBS. To estimate the absolute risk of cancer, we calculated cumulative incidences, treating death as a competing risk. As a measure of the relative risk of cancer, we calculated standardized incidence ratios (SIRs), ie, the ratio of observed to expected numbers of cancers. Expected numbers of cancers were based on national incidence rates according to sex, age, and calendar period in five-year intervals, accessed from the Cancer Registry. Confidence intervals (CIs) for the estimated SIRs were computed based on the assumption that the observed number of cases in a specific category followed a Poisson distribution. Exact 95% CIs were used when the observed number was less than ten; otherwise Byar’s approximation was used. Data were not presented for cancer sites with fewer than five recorded diagnoses. We stratified the analyses by sex, age group (<40 years, 40–49 years, 50–59 years, 60–69 years, and ≥70 years), year of diagnosis (1978–1993, 1994–2017), hospital-diagnosed infection within six months before the index date (yes, no), and preexisting autoimmune disease at any time before the index date (yes, no). To examine a potential time-varying association, we further stratified the analyses according to follow-up time (0–<3 months, 3–<6 months, 6–<12 months, 12–<24 months, 24–<36 months, and ≥36 months).
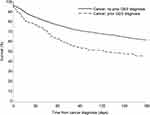
To examine the association between GBS and cancer mortality, we matched each GBS patient who was diagnosed with a subsequent cancer with up to ten cancer patients without a GBS diagnosis. Comparison cohort members were selected from the Cancer Registry. Matching factors were cancer site, sex, age at the time of cancer diagnosis (five-year intervals), and year of diagnosis (five-year intervals). Using the Kaplan–Meier estimator, we computed the six-month survival probability. Then, using Cox proportional hazards regression analysis, we calculated mortality rate ratios, ie, hazard ratios following cancer diagnosis, comparing cancer patients with a previous GBS diagnosis with cancer patients without this diagnosis. The analysis was restricted to patients with a subsequent cancer within one year of GBS diagnosis and their matched members of the GBS-free comparison cancer cohort. We adjusted the mortality rate ratios for cancer stage (localized, regional, metastatic spread, and unknown) and Charlson Comorbidity Index score (0, 1–2, and 3+) (eTable 2 in the Supplement), a validated scoring system aimed to categorize the severity of a patient’s burden of comorbidity.29
All statistical analyses were conducted using SAS software version 9.4 (SAS Institute Inc). The study was reported to the Danish Data Protection Agency (record no. KEA‐2017‐36/812). Approval from an ethics committee is not required for registry-based studies in Denmark.
Results
We identified 7897 patients, 58% male, with a diagnosis of GBS. Their median age was 57 years [interquartile range (IQR) 40–69 years]. The median length of hospital stay was 20 days (IQR 9–49 days), and the median follow-up time was 9.5 years (IQR 3.6–19.0 years). One-year cumulative incidence of any cancer was 2.7% (95% CI, 2.4–3.1%). In general, GBS patients were at increased risk of developing cancer compared with expected rates in the general population (Figure 1).
Based on 215 observed cancers within the first year of follow-up, the overall SIR was 3.35 (95% CI, 2.92–3.83). The SIR was particularly elevated among those aged <40 years (SIR: 7.04 [95% CI, 3.22–13.38]). No clear effect modification was otherwise observed, according to sex, year of diagnosis, hospital-diagnosed infections within six months prior to the index date, and preexisting autoimmune disease. Figure 2 displays SIRs according to follow-up time in months. We observed an inverse association with length of follow-up time. The SIR was markedly elevated within the first three months after hospitalization with GBS (SIR: 7.34 [95% CI, 6.10–8.76]) and steadily dropped thereafter. However, an elevated risk of cancer persisted even during 24–36 months of follow-up (SIR: 1.40 [95% CI, 1.11–1.74]) and after 36 months of follow-up (SIR: 1.17 [95% CI, 1.09–1.25]).
The elevated cancer risk during the first year of follow-up was driven by hematologic cancers (53 cancers; SIR: 8.67 [95% CI, 6.49–11.34]), smoking-related cancers (75 cancers; SIR: 3.57 [95% CI, 2.81–4.47]), and cancers of neurological origin (17 cancers; SIR: 8.60 [95% CI, 5.01–13.77]) (Figure 3). In particular, lung cancer (small cell lung cancer; SIR: 13.67 [95% CI, 8.76–20.35] and non-small cell lung cancer; SIR: 3.31 [95% CI, 2.18–4.81]) was the most common cancer in GBS patients and the main contributor to the excess cancer risk during the first year of follow-up.
Figure 4 shows six-month survival among patients diagnosed with any cancer within one year of GBS diagnosis and among members of the matched GBS-free comparison cancer cohort. Six months after cancer diagnosis, the overall survival probability for patients with a previous GBS diagnosis was 45% (95% CI, 38–52) compared to 61% (95% CI, 59–63) for cancer patients without GBS. The prevalence of metastatic spread was 32% in cancer patients with a previous GBS diagnosis and 28% in those without GBS. Among cancer patients with a previous GBS diagnosis, 40% had a Charlson Comorbidity Index score of 1–2, compared with 23% among those without a GBS diagnosis; for a score of 3+, the prevalences were 6% and 4%, respectively. The adjusted mortality rate ratio comparing patients diagnosed with any cancer within one year of GBS diagnosis with matched GBS-free cancer cohort members was 1.56 (95% CI, 1.27–1.90). When comparing patients diagnosed with any cancer more than one year after their GBS diagnosis with members of the GBS-free cancer cohort member, the adjusted mortality rate ratio was 1.18 (95% CI, 1.08–1.30).
Discussion
In this large nationwide population-based cohort study, patients with an inpatient or outpatient clinic hospital diagnosis of GBS had an increased risk of a subsequent cancer diagnosis compared with the general population. During the first year of follow-up, GBS patients had an approximately three-fold increased risk of cancer, particularly hematologic cancers, lung and other smoking-related cancers, and cancers of neurological origin. The absolute cancer risk was close to 3%. The elevated risk decreased over time, but an approximately 17% increased risk persisted 36 months after GBS diagnosis. An earlier GBS diagnosis was an adverse prognostic marker for survival following a cancer diagnosis; the all-cause mortality risk was 1.6-fold higher in cancer patients with a recent GBS diagnosis compared with GBS-free cancer cohort members, after controlling for cancer stage and burden of comorbidity.
Previous case-reports5–18 and small cohort studies,19,20 as well as the recent case-control study,3 have reported cancers before, concomitantly with, and shortly after the diagnosis of GBS. These diverse approaches complicate the interpretation of the association, in terms of directionality. Using a registry population-based cohort design limits our ability to investigate cancer diagnosed before GBS hospitalization and to determine appropriate cutoff times to observe the association in the opposite direction. Given the lack of understanding in literature regarding the underlying mechanism between GBS and occult cancer, we decided to use this study design to address the precise question of cancer diagnosis after GBS; allowing us to make inference regarding underlying latent cancer status. Therefore, we are able to conclude that there is increased cancer-risk in the peri-symptomatic period of hospitalization for moderate-to-severe GBS.
The association between GBS and cancer may have several explanations. Hospitalized GBS patients are acutely ill and therefore often closely monitored. Some cancers may be more likely to be detected and diagnosed during this time. Thus, heightened diagnostic, detection, and surveillance efforts associated with a GBS hospital admission could account for part of the association, particularly during the first year of follow-up. The diminished strength of the association over longer follow-up time is consistent with this explanation. Still, if surveillance bias were to fully explain the association, a compensatory deficit (ie, an increased short-term risk followed by a decreased long-term risk) would be expected; however, we did not see such a pattern. In fact, an excess risk of cancer persisted even 36 months after the index date. Another potential mechanism could be that development of GBS reflects an underlying paraneoplastic syndrome, as GBS shares characteristics with other paraneoplastic neuropathic syndromes. Although paraneoplastic syndromes, including “paraneoplastic GBS”,9 occur in fewer than 1% of cancer patients,6 they are especially prevalent among patients with small cell and non-small cell lung cancer.30
Paraneoplastic neurologic syndromes also are frequently associated with both small cell and non-small cell lung cancer.31 The magnitude of risk and prevalence of small cell and non-small cell lung cancer in our GBS cohort, as well as results from past case reports, align with this evidence.5–18 A potential mechanism underlying the association between GBS and cancer is based on the observation that the cross-immunoreaction involving the tumor and peripheral nerves is caused by the presence of high levels of anti-GM1 ganglioside IgG autoantibodies, anti-Hu, and onconeural antibodies targeting antigen-specific T-lymphocytes.9 However, evidence of the presence of these markers in GBS patients with malignancies is inconsistent. In a previous study, patients with malignancy and a GBS-like syndrome were not significantly different from controls with regard to the presence of anti-ganglioside antibodies.5
To our knowledge, this is the first report on survival in cancer patients with GBS compared with cancer patients without GBS. After adjustment for cancer stage and comorbidity burden, cancer patients with a previous GBS diagnosis had worse survival, particularly following a cancer diagnosis within one year of the GBS diagnosis. A full explanation of the worse prognosis of cancer patients with GBS requires a detailed understanding of the clinical characteristics of these neoplasms that goes beyond the information available in our study. One speculative interpretation is that GBS patients are more debilitated because of residual neurological deficits, which, in turn, could affect both mobility and pulmonary function. However, we cannot rule out the possibility of uncontrolled confounding from smoking, a risk factor for both infections and cancer. Although data on smoking habits among GBS patients were unavailable for this study, lung cancer was the cancer most commonly observed during follow-up.
This population-based study was conducted within a universal healthcare system, which diminished the risks of referral and selection biases. The large size of the study population enabled us to assess risks of specific cancers. Further, the Danish Cancer Registry holds complete and valid information on all incident cancers in Denmark. Our analyses were standardized according to sex, age, and calendar period, and these variables were therefore accounted for in the estimated associations between GBS and cancer. It must be noted that some mild cases of GBS may not have required acute hospitalization, and these patients were not included in our analyses. Findings from this population-based study generalize to patients in developed countries with moderate or severe GBS. This limitation does not allow us to observe if association patterns with occult malignancy differ between mild versus severe cases of GBS as well as different variants of GBS.
In conclusion, our study suggests that GBS may be a marker of underlying cancer. In particular, an excess of hematologic cancers, cancers of neurological origin, and lung and other smoking-related cancers was diagnosed in patients with GBS within one year after hospitalization for this disorder, and – to a lesser extent – in subsequent years. We cannot exclude the possibility that increased surveillance related to hospitalization for GBS contributed to the excess cancer risk observed during the early follow-up period, but this explanation does not account for increased risk after the first year of follow-up.
Acknowledgments
The Department of Clinical Epidemiology, Aarhus University, receives funding for other studies from companies in the form of research grants to (and administered by) Aarhus University. None of these studies have any relation to the present study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
BG was supported by NIEHS R01ES030717, National Heart, Lung and Blood Institute R25 HL 108857.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Dimachkie MM, Barohn RJ. Guillain-Barré syndrome and variants. Neurol Clin. 2013;31(2):491–510. doi:10.1016/j.ncl.2013.01.005
2. McGrogan A, Madle GC, Seaman HE, de Vries CS. The epidemiology of Guillain-Barré syndrome worldwide. A systematic literature review. Neuroepidemiology. 2009;32(2):150–163. doi:10.1159/000184748
3. Levison LS, Thomsen RW, Sindrup SH, Andersen H. Association between incident cancer and Guillain-Barré syndrome development: a nationwide case-control study. Neurology. 2022;2:
4. Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med. 2003;349(16):1543–1554. doi:10.1056/NEJMra023009
5. Naveed S, Okoli K, Hollingsworth J, Kasmani R. Guillain-Barré syndrome as a paraneoplastic manifestation of small-cell carcinoma of lung. South Med J. 2010;103(2):156–158. doi:10.1097/SMJ.0b013e3181bfd2c0
6. Eimil M, Benito-León J. Guillain-Barré-like syndrome heralding small-cell lung cancer. Eur J Neurol. 2007;14(11):e15–e16. doi:10.1111/j.1468-1331.2007.01957.x
7. Jung I, Gurzu S, Balasa R, et al. A coin-like peripheral small cell lung carcinoma associated with acute paraneoplastic axonal Guillain-Barre-like syndrome. Medicine. 2015;94(22):e910. doi:10.1097/MD.0000000000000910
8. Wu D, Liu A, Baldinger E, Frontera AT. A case of paraneoplastic Guillain-Barré syndrome associated with squamous cell carcinoma of the lung. Cureus. 2018;10(8):e3202. doi:10.7759/cureus.3202
9. Nokura K, Nagamatsu M, Inagaki T, et al. Acute motor and sensory neuronopathy associated with small-cell lung cancer: a clinicopathological study. Neuropathology. 2006;26(4):329–337. doi:10.1111/j.1440-1789.2006.00698.x
10. Lagrange E, Veran O, Besson G. Pure motor relapsing Guillain-Barré syndrome associated with anti-GM1 antibodies revealing urinary bladder cancer. Eur J Neurol. 2007;14(12):e7. doi:10.1111/j.1468-1331.2007.01990.x
11. Kim MH, Hwang MS, Park YK, et al. Paraneoplastic Guillain-Barré syndrome in small cell lung cancer. Case Rep Oncol. 2015;8(2):295–300. doi:10.1159/000437295
12. Ferrufino E, Camarasa A, Chiner E. Guillain-Barre syndrome as an initial manifestation of small cell lung carcinoma. Arch Bronconeumol. 2011;47(2):107–108. doi:10.1016/j.arbres.2010.08.006
13. Vallat JM, De Mascarel HA, Bordessoule D, et al. Non-Hodgkin malignant lymphomas and peripheral neuropathies–13 cases. Brain. 1995;118(Pt 5):1233–1245. doi:10.1093/brain/118.5.1233
14. Rodrigues A, Monteiro A, Viana J, Macedo A, Graca F, Sena A. Acute non-lymphoblast leukaemia presenting as a Guillain-Barré syndrome. J Neurol Neurosurg Psychiatry. 1993;56(8):936–937. doi:10.1136/jnnp.56.8.936-A
15. Christodoulou C, Anastasopoulos D, Visvikis A, et al. Guillain-Barré syndrome in a patient with metastatic colon cancer receiving oxaliplatin-based chemotherapy. Anticancer Drugs. 2004;15(10):997–999. doi:10.1097/00001813-200411000-00010
16. Zilli T, Allal AS. Guillain-Barré syndrome as an atypical manifestation of an esophageal carcinoma. Neurol Sci. 2011;32(1):151–153. doi:10.1007/s10072-010-0363-9
17. Lisak RP, Mitchell M, Zweiman B, Orrechio E, Asbury AK. Guillain-Barré syndrome and Hodgkin’s disease: three cases with immunological studies. Ann Neurol. 1977;1(1):72–78. doi:10.1002/ana.410010107
18. Re D, Schwenk A, Hegener P, Bamborschke S, Diehl V, Tesch H. Guillain-Barré syndrome in a patient with non-Hodgkin’s lymphoma. Ann Oncol. 2000;11(2):217–220. doi:10.1023/A:1008389607293
19. Vigliani MC, Magistrello M, Polo P, Mutani R, Chiò A. Risk of cancer in patients with Guillain-Barré syndrome (GBS). A population-based study. J Neurol. 2004;251(3):321–326. doi:10.1007/s00415-004-0317-3
20. Hiew FL, Rajabally YA. Malignancy in Guillain-Barré syndrome: a twelve-year single-center study. J Neurol Sci. 2017;375:275–278. doi:10.1016/j.jns.2017.02.024
21. Maddison P, Lang B, Thomsen S, et al. Prospective study of cancer survival in patients with HuD-antibody-associated paraneoplastic neurological disorders. J Neurol Neurosurg Psychiatry. 2021;92(12):1350–1351. doi:10.1136/jnnp-2021-326067
22. Shah S, Flanagan EP, Paul P, et al. Population-based epidemiology study of paraneoplastic neurologic syndromes. Neurol Neuroimmunol Neuroinflamm. 2022;9(2). doi:10.1212/NXI.0000000000001124
23. Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi:10.2147/CLEP.S179083
24. Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
25. Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/CLEP.S91125
26. Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39(7_suppl):42–45. doi:10.1177/1403494810393562
27. Levison LS, Thomsen RW, Christensen DH, Mellemkjær T, Sindrup SH, Andersen H. Guillain-Barré syndrome in Denmark: validation of diagnostic codes and a population-based nationwide study of the incidence in a 30-year period. Clin Epidemiol. 2019;11:275–283. doi:10.2147/CLEP.S199839
28. Danish Health Data Authority, Nye Kræfttilfælde i Danmark; 2017. Available from: file:///C:/Users/AU125348/Downloads/Kraefttilfaelde%202017.pdf.
29. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
30. Kanaji N, Watanabe N, Kita N, et al. Paraneoplastic syndromes associated with lung cancer. World J Clin Oncol. 2014;5(3):197–223. doi:10.5306/wjco.v5.i3.197
31. Giometto B, Grisold W, Vitaliani R, Graus F, Honnorat J, Bertolini G. Paraneoplastic neurologic syndrome in the PNS Euronetwork database: a European study from 20 centers. Arch Neurol. 2010;67(3):330–335. doi:10.1001/archneurol.2009.341
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.