Back to Journals » International Journal of General Medicine » Volume 11
Can patient safety be improved by reducing the volume of “inappropriate prescribing tasks” handed over to out-of-hours junior doctors?
Authors Amis SM, Osicki THE
Received 4 October 2017
Accepted for publication 3 January 2018
Published 20 March 2018 Volume 2018:11 Pages 105—112
DOI https://doi.org/10.2147/IJGM.S153227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Samuel Martin Amis, Tobin Henry Edgar Osicki
Department of Acute Internal Medicine, South Warwickshire Foundation Trust, Warwick, UK
Background: First-year doctors found that during out-of-hours shifts they were being delayed and distracted from reviewing potentially sick/deteriorating patients by a high volume of prescribing tasks. This predominately consisted of oral anticoagulation prescribing and rewrites of drug charts. We hoped that if we could reduce this burden of “inappropriate prescribing tasks”, we could not only improve junior doctors’ job satisfaction and opportunities for training but also give them more time for patient reviews.
Methods: Three weekends were initially audited to quantify the number of “inappropriate prescribing tasks” using data from the hospital’s computerized task assigning system. On three subsequent weekends, a checklist was handed out to the ward teams on Friday mornings. This checklist was designed to encourage the day teams to check that drug charts would not need oral anticoagulation or rewriting over the weekend.
Results: An overall reduction in “inappropriate prescribing tasks” of 46% with a specific reduction in inappropriate oral anticoagulation prescribing of 65% was observed. Inappropriate drug chart rewrites were reduced by 30%. The reduction in the mean number of pre-intervention inappropriate prescribing tasks (as a percentage of total prescribing tasks) and the post-intervention mean was 6.94% (95% confidence interval −0.54 to 14.42, p-value=0.062).
Conclusion: Improved job satisfaction and a perceived reduced workload were noted from post-intervention qualitative surveys. While improved patient safety directly resulting from this intervention is more difficult to establish, and the observed reduction in inappropriate prescribing was only approaching statistical significance, our colleagues commented in post-intervention feedback that they felt they had more time, and felt less pressured, while attending patients. The workload of junior doctors can exert a significant effect on patient care, and simple measures can alleviate this burden. Furthermore, computerized hospital task management systems are an underutilized source of data for audit and quality improvement.
Keywords: checklist, on-call, anticoagulation, drug-chart, workload
Introduction
On-call junior doctors covering the wards out-of-hours (OOH) can have considerable workloads. Tasks typically include plain film and blood result interpretation, drug and IV fluid prescription, discharge summaries and the urgent reviews of potentially deteriorating patients. Prescribing tasks, in particular, can comprise a considerable proportion of this workload. Specifically, tasks such as warfarin and therapeutic Tinzaparin prescribing and the rewriting of drug charts, with no further space for nursing signatures, were identified as being those that should ideally have been completed by the ward day teams. If the volume of these “inappropriate prescribing tasks” being handed over to the OOH junior doctors could be reduced, they would have greater time to spend on reviewing sick patients and patient safety, and quality of care would likely benefit as a result. There is considerable evidence in the literature that patient safety, due to a reduced rate of prescribing error, can be improved if workload is reduced.1,2 Similarly, the rate of task completion has been shown to be adversely affected by high frequency of interruptions.4,5 The level of strain experienced by doctors due to high workloads has also been shown to adversely affect their general performance.3
Some prescribing tasks are, of course, unforeseeable such as prescribing analgesia for a patient who has just started complaining of pain or antiemetics for a patient feeling nauseated, and these would not be classed as “inappropriate prescribing tasks” and so are not included in this study.
From our own first-hand experience and discussion with other first-year junior doctor (FY1) colleagues on the medical rota, it became clear that a high volume of inappropriate prescribing tasks was an issue that was impacting on the amount of time available for patient reviews as well as their overall job satisfaction and opportunities for learning. A further issue that was noted was a lack of documentation of patient summaries, ceilings of care and management plans, which could occasionally hinder patient reviews.
A questionnaire was handed out to the FY1s at one of the weekly teaching sessions to try and establish the presence of, and if so quantify the extent of, the issue. Thirteen of the 16 medical FY1s responded. The feedback from the questionnaires is displayed in Table 1.
  | Table 1 Questionnaire responses from pre-intervention survey of FY1s Abbreviation: FY1s, first-year junior doctors. |
In summary, our colleagues felt that the volume of “inappropriate prescribing tasks” was an issue in need of addressing, and our planned intervention had sufficient support to have a reasonable chance of being implemented. We also discussed this with the foundation program lead who confirmed that this has been an issue raised by previous cohorts of junior doctors at the trust.
Methodology
This project primarily aimed to assess whether a checklist, handed out on Friday mornings to the ward day teams, could reduce the volume of “inappropriate tasks” handed over to OOH junior doctors over the weekend. The checklist would aim to encourage the junior doctors to check warfarin/Tinzaparin prescriptions are filled out, and the drug charts have sufficient space for administration signatures and so will not need rewriting over the weekend. The checklist would double as the “jobs list” for the day, to make it more likely that it will be utilized. There would also be a checklist to remind juniors to check the notes of patients who could conceivably deteriorate over the weekend to ensure a plan, ceiling of care and summary of admission were documented. This was a secondary aim of the project (as a pilot scheme to assess if further work may be useful) and would only be assessed qualitatively during the post-intervention feedback session with FY1s (Supplementary materials).
Warwick Hospital employs a computerized system for distributing tasks to OOH junior doctors known as clinical task management system (CTMS). Staff nurses can submit jobs via the hospital intranet as they come up during OOH. Tasks can also be submitted toward the end of weekdays by the in-hours ward teams as a way of handing over jobs that need chasing up. As with any computerized system, the usage of the system is logged in a database. Access to the data was provided for us by the audit department. Initially, three weekends would be audited prior to starting the intervention and then compared to three weekends in which the checklist would be handed out on the Friday morning prior to the weekend. For the purposes of the project, the weekend was defined as 12:00 Friday till 12:00 Monday (72-hour period). The three pre-intervention weekends that were initially audited were the weekends in the period from December 16, 2016, to January 9, 2017, (excluding the Christmas weekend). The three weekends for which the checklist was handed out were in the period from January 13, 2017, to January 30, 2017.
The data from CTMS consisted of a list of all the jobs inputted into the system during the time periods specified above. Searches of the data using the “Ctrl+F” function were then carried out looking for the following keywords: warfarin, Tinzaparin, therapeutic, anticoagulation, drug chart, kardex, rewrite, prescribe, prescription, medication and drug. Each task was then reviewed individually to categorize it as a nonprescribing task (therefore excluded from the audit), an “anticoagulation prescribing task” (requesting warfarin dosing or continuing a therapeutic Tinzaparin prescription), a “drug chart rewrite task”, “other inappropriate prescribing task” or an appropriate prescribing task (also excluded from the audit). Appropriate prescribing tasks were defined as prescribing tasks that could not have reasonably been foreseen and completed by the ward day team. These included, most commonly, tasks such as analgesia, laxative or antiemetic prescriptions. “Other inappropriate prescribing tasks” included, most commonly, tasks such as prescribing a recently admitted patient’s routine medications, but could comprise any prescribing task that could conceivably have been completed during normal working hours.
Following the auditing of the initial three weekends, a presentation was made to the FY1s during one of the weekly teaching sessions. This sought to raise awareness of the project and explain its purpose prior to the handing out of the checklists. This also facilitated feedback that allowed modification to the checklist prior to its implementation. For example, the space at the bottom of the checklist for other important handover notes was added following this feedback. One of our colleagues also suggested that each checklist be designed with the specific bed layout for each ward; as this varied considerably between the medical wards, this was, again, enacted.
Ethical approval
Approval was not deemed to be required by an institutional review board or ethics committee by the Trust’s audit and quality improvement department.
Results
Table 2 displays the total number of inappropriate prescribing tasks broken down by class of task and for each of the six weekends that were audited. The total number of tasks distributed by the CTMS averaged 316 per weekend. The average number of anticoagulation prescriptions per weekend pre-intervention was 25.7, which fell to an average of nine anticoagulation tasks over the three post-intervention weekends. The number of drug chart rewrites over a pre-intervention weekend was an average of 6.7 compared to 4.7 over the post-intervention weekends. Similarly, the “other inappropriate prescribing tasks” saw a decrease in average number of tasks submitted via CTMS from 13.7 to 11.0. Overall, the total inappropriate prescribing tasks decreased from an average of 46 pre-intervention to 24.7 with the checklist being used. For every weekend that the checklist was in place, the proportion of the total jobs that the “inappropriate prescribing jobs” comprised was significantly lower than for the pre-intervention weekends.
  | Table 2 Comparison of “inappropriate” prescribing tasks submitted during individual pre-intervention weekends with the post-intervention weekends |
Figure 1 shows a breakdown of the results in terms of the individual types of inappropriate prescribing tasks but with the pre- and post-intervention weekend data grouped together. All three classes of “inappropriate prescribing task” saw a reduction in the number of tasks sent out over the CTMS. The greatest reduction was seen in anticoagulation prescription (ie, prescribing tasks sent out over the CTMS which involved warfarin prescription or therapeutic dose Tinzaparin prescription). This class of inappropriate prescribing task saw a decrease of 65%. The most modest reduction was in “other inappropriate tasks” which saw a fall of 19.5% despite the checklist not being designed to decrease these specifically. Tasks requesting a drug chart rewrite (due to the chart being full and therefore there being further space for nursing signatures for dose administration) were reduced by 30%. Combined, the reduction in total inappropriate jobs was by 46%.
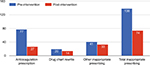  | Figure 1 Bar graph comparing the number of inappropriate prescribing tasks handed over in pre-intervention weekends with post-intervention weekends. |
Statistical significance testing
The null hypothesis was that the introduction of the checklist would result in no observable reduction in inappropriate prescribing tasks handed over to OOH junior doctors (ie, the difference between average pre-intervention inappropriate prescribing tasks and average post-intervention inappropriate prescribing, as a percentage of total prescribing, would be equal to 0) (Table 3).
Pre-intervention – mean: 14.97%, standard deviation (SD): 4.50, n=3 weekends.
Post-intervention – mean: 8.03%, SD: 1.23, n=3 weekends.
The difference between the mean number of pre-intervention inappropriate prescribing tasks as a percentage of total prescribing tasks and the post-intervention mean equals 6.94%.
The unpaired t-test was used to assess statistical significance. The two-tailed p-value equals 0.0615.
As a result, the 95% confidence interval (CI) of this difference is from −0.54 to 14.42. As this range includes 0 and the p-value is >0.05%, the null hypothesis cannot be rejected and the observed decrease in prescribing tasks can only be said to be approaching statistical significance.
Discussion
The checklist had been designed, not only to reduce inappropriate prescribing tasks but also to encourage day team junior doctors to ensure a summary, management plan and ceiling of care were documented in the notes of patients who were at risk of deteriorating over the weekend. This was included as a pilot study to assess if this could be the focus of a further quality improvement project. Unfortunately, the FY1s’ qualitative feedback from the post-intervention debrief was that on attending patients for reviews during OOH shifts, there was no observed improvement in documented summaries, plans and ceilings of care in the notes. An alternative methodology may be more appropriate to address this particular issue going forward.
There are a number of limitations that need to be acknowledged and taken into account when drawing conclusions from this data. First, the three pre-intervention weekends that were used to determine the baseline volume of inappropriate prescribing tasks were not selected at random. Instead, the three weekends (the Christmas weekend was excluded) were the weekends directly preceding the three post-intervention weekends that were used, which may have introduced a selection bias. Furthermore, the data from the six weekends were not blinded to ensure that the individual analyzing the data would be unaware that he/she was looking at a pre- or post-intervention weekend, so observer bias may also influence the data.
Also, only three weekends were used as the sample to determine the pre-intervention level of inappropriate prescribing tasks. This meant the p-value for the observed reduction in total inappropriate tasks equaled 0.0615 (>0.05), and the 95% CI of this difference, in inappropriate prescribing as a percentage of total prescribing tasks, ranged from −0.54 to 14.42%. As the CIs included the null hypothesis (that the difference in the number of inappropriate prescribing tasks as a percentage of total prescribing, pre- and post-intervention, would be zero), we were unable to reject the null hypothesis. On the other hand, there were a number of factors that would likely have worked against the observed reduction in inappropriate prescriptions that was observed. One issue was that a number of the medical wards did not have regular FY1s. This meant that the checklist was handed over to the more senior junior doctors who were not aware of the project as they had not been in attendance at the pre-intervention presentation which took place during weekly FY1 teaching. Another issue we identified was that not all prescribing tasks were assigned using the computerized CTMS; a number of nurses, who were unfamiliar with the system, would have bleeped the on-call junior doctor and assigned the task over the phone. Quantifying what proportion of the prescribing tasks were not assigned using the CTMS is difficult to establish, but subjectively, at least, this was not considered to be a significant proportion based on the feedback from the FY1s’ experiences.
Although drug chart rewrites were not reduced as greatly as we had hoped, this result could have been caused by confounding factor. Three drug chart rewrites on a particular ward were observed during one of the post-intervention weekends. This indicated that there may have been some unforeseen events that complicated the implementation of the checklist, for example, the junior being called away to deal with a sick patient for the remainder of the afternoon or staffing pressures that day. We later investigated this particular anomaly, and the ward had been short-staffed on that particular Friday resulting in the checklist not being used.
Conclusion
This project demonstrates that a significant change in staff behavior can be instigated with a simple quality improvement measure. Demonstrable improvements in workload, job satisfaction and patient safety are within the scope and capabilities of FY1s as demonstrated by this project as well as other work looking into the role of junior doctors in quality improvement.7 We also found that computerized hospital task management systems are a rich and accessible source of data for audit and quality improvement purposes.
The introduction of the checklist caused a reduction in the number of “inappropriate prescribing tasks” by almost a half. The number of inappropriate prescribing tasks in all three categories also fell individually. Reducing the number of drug chart rewrites by almost a third, in particular, was considered to be of significant value to the junior doctors we spoke to prior to the intervention, as it is perceived to be the most time-intensive of the prescribing tasks. While improved patient safety directly resulting from our intervention is more difficult to establish, our colleagues commented in post-study feedback that they had more time for patient reviews and felt less pressured. There is also, as mentioned previously, much literature to support the assumption that reducing workload and distractions can reduce the rate of error and so improve patient safety,1–5 particularly with regard to prescribing error.2
It is difficult to assess to what extent the success of the project was down to the checklist itself and what proportion of the reduction in “inappropriate prescribing tasks” can be attributed to the Hawthorne effect. This is the observed phenomenon whereby improvements in people’s behavior can result from the awareness that they are being observed.6 The fact that one of the classes of inappropriate prescribing tasks “other inappropriate tasks” was reduced by almost 20% despite the checklist only being designed to deal with anticoagulation and drug chart rewrites does lend credence to the Hawthorne effect contributing, at least to some extent, to the success of this project. Similarly, increased general awareness of the issue and the purpose of the project may have also contributed to the observed results. This may have resulted from the pre-intervention presentation to the FY1s but also the act of handing over checklists in person which would have acted as a further reminder for the junior doctors on the wards.
Further work
The structure of this quality improvement study allows for a straightforward reauditing with the next rotation of FY1s which occurs every 4 months. This would allow feedback to be implemented, including any improvements or additions to the checklist or ways of raising awareness. It would also be straightforward to audit a further 10 weekends, selected at random, from the 12 months prior to the intervention. This would ensure that the sample of pre-intervention weekends would be more likely to be representative of the number of inappropriate prescribing tasks on an average weekend. This would likely improve the statistical significance of any observed reduction in inappropriate prescribing tasks to the point where the null hypothesis could be rejected.
At the feedback session post-intervention, and also after the raising awareness presentation before the intervention, other tasks were suggested that could be added to the checklist in the future. One suggestion was IV fluids which is another common prescribing task for OOH junior doctors. This could only be applicable for Friday night however, as IV fluid should only be prescribed following assessment of patient’s hydration status as well as checking latest kidney function and electrolyte levels. It is therefore unreasonable and unsafe to expect a patient’s fluid to be prescribed for a whole weekend in advance.
The project could potentially be expanded to include all the OOH shifts on the medical rota, that is, the weekday evening and night shifts, with the checklists available every morning on the wards instead of just Friday. Discussion with nursing teams on each ward to involve them in the use of the list (eg, so they could highlight on the checklist patients who require their chart to be rewritten) might further improve the utilization and efficacy of the list. Similarly, this project could be expanded to include the surgical wards. During the feedback session, the surgical FY1s informed us that a much higher proportion of their prescribing tasks are not put on the CTMS but are instead given to them over the phone after being bleeped. As a result, if the project were to be repeated with the surgical FY1s, there would need to be considerable work to encourage nurses who work on surgical wards to send more jobs via the intranet instead of the phone. We would also need to encourage the surgical FY1s and more senior junior doctors to put any jobs that they get asked to do over the phone on CTMS themselves to ensure there is an auditable data trail.
Finally, given the relative ease of auditing prescribing tasks using the CTMS data, we would also propose that the volume of inappropriate jobs could be fed back to the FY1s at their weekly teaching sessions on a regular basis, for example, twice a rotation (ie, every 2 months). To avoid any “blame culture” among the FY1s, the individual wards need not be mentioned in the presentation. However, a comparison between their ward and other wards (eg, percentage of jobs that are inappropriate on a particular FY1’s ward vs the average percentage of jobs that are inappropriate from all wards) could later be emailed out to the respective junior doctor teams in order to commend the wards that are doing better than average and encourage those that are performing less well. This would facilitate continuous feedback for the juniors that could lead to a sustained reduction in inappropriate prescribing tasks.
Acknowledgments
The authors to thank the audit and quality improvement department at South Warwickshire Foundation Trust as well as their FY1 colleagues on general medicine. They also thank Mr Richard Morrell, consultant in emergency medicine, for championing the project.
Disclosure
The authors report no conflicts of interest in this work.
References
Li SY, Magrabi F, Coiera E. A systematic review of the psychological literature on interruption and its patient safety implications. J Am Med Inform Assoc. 2012;19(1):6–12. | ||
Raban MZ, Walter SR, Douglas HE, Strumpman D, Mackenzie J, Westbrook JI. Measuring the relationship between interruptions, multitasking and prescribing errors in an emergency department: a study protocol. BMJ Open. 2015;5(10):e009076. | ||
Weigl M, Muller A, Sevdalis N, Angerer P. Relationships of multitasking, physicians’ strain, and performance: an observational study in ward physicians. J Patient Saf. 2013;9(1):18–23. | ||
Westbrook JI, Coiera E, Dunsmuir WT, et al. The impact of interruptions on clinical task completion. Qual Saf Health Care. 2010;19(4):284–289. | ||
Weigl M, Müller A, Angerer P, Hoffmann F. Workflow interruptions and mental workload in hospital pediatricians: an observational study. BMC Health Serv Res. 2014;14:433. | ||
McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. Accessed September 28, 2017. | ||
Evidence scan: involving junior doctors in quality improvement. Health Foundation; 2011. Available from: http://www.health.org.uk/sites/health/files/InvolvingJuniorDoctorsInQualityImprovement.pdf. |
Supplementary materials
Instructions on the use of the checklist printed on its reverse
How to use this checklist
This checklist is designed to help minimize inappropriate prescribing jobs for the on-call teams over the weekend. We appreciate that Friday afternoons are usually hectic, but this checklist is designed to prompt you to do a quick round of the drug charts on the ward to check that no warfarin/Tinzaparin will need prescribing and no drug charts will need rewriting over the weekend. This chart should include your specific ward’s bed layout, and there is space for the checklist to double up as your Friday jobs list with space for any important jobs to be handed over as well. We are also trying to ensure that the patient notes, which will be used by the on-call team when they attend a potentially sick patient over the weekend, have a clearly documented ceiling of care, management plan and clinical summary.
Jobs
The ‘Jobs list’ column is to allow junior doctors space to note down tasks generated from the ward round. As a result, the checklist can act as an aide-memoire for these tasks throughout the working day on Friday and the checklist is more likely to be utilised.
Chart checklist
This box is to be ticked once it is confirmed that this patient’s chart has adequate space for nurse administration signatures over the weekend (and will therefore not need rewriting).
Anticoagulation checklist
This can be ticked once it is confirmed that this patient’s drug chart has had warfarin or therapeutic Tinzaparin prescribed (if applicable) for over the weekend.
Note summary checklist
This checklist is to serve as a reminder to check the notes of any patient, who you feel has the potential to deteriorate over the weekend. Please ensure that the last entry includes a brief clinical summary with overall management plan and a ceiling of care to aid the on-call doctors over the weekend.
Jobs to hand over
This space is for any tasks that come up during Fridays that will require handing over to on-call juniors.
  | Figure S1 Checklist designed to decrease inappropriate prescribing handed over to junior doctors during out-of-hours. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

