Back to Journals » International Journal of Women's Health » Volume 9
Can mHealth improve access to safe blood for transfusion during obstetric emergency?
Authors Rahman A , Akhter S , Nisha MK, Islam SS, Ashraf F, Rahman M, Begum N, Chowdhury ME, Austin A , Anwar I
Received 19 August 2016
Accepted for publication 2 December 2016
Published 20 April 2017 Volume 2017:9 Pages 235—243
DOI https://doi.org/10.2147/IJWH.S120157
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Aminur Rahman,1,2 Sadika Akhter,1 Monjura Khatun Nisha,3 Syed Shariful Islam,4 Fatema Ashraf,5 Monjur Rahman,1 Nazneen Begum,6 Mahbub Elahi Chowdhury,1 Anne Austin,7 Iqbal Anwar1
1International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), Dhaka, Bangladesh; 2College of Public Health Sciences, Chulalongkorn University, Bangkok, Thailand; 3Sydney School of Public Health, Sydney Medical School, The University of Sydney, Sydney, NSW, Australia; 4Department of Public Health and Informatics, Bangabandhu Sheikh Mujib Medical University, 5Department of Gyenaecology and Obstetric, Shaheed Suhrawardi Medical College and Hospital, 6Department of Gyenaecology and Obstetric, Dhaka Medical College and Hospital, Dhaka, Bangladesh; 7JSI Research & Training Institute, Inc., Boston, MA, USA
Purpose: Of the 99% maternal deaths that take place in developing countries, one-fourth is due to postpartum hemorrhage (PPH). PPH accounts for one-third of all blood transfusions in Bangladesh where the transfusion process is lengthy as most facilities do not have in-house blood bank facilities. In this context, the location where blood is obtained and the processes of obtaining blood products are not standardized, leading to preventable delays in collecting blood, when it is needed. This study evaluated the effectiveness of an online Blood Information Management Application (BIMA) system for reducing lag time in the blood transfusion process.
Patients and methods: The study was conducted in a public medical college hospital in Dhaka, Bangladesh, and in two proximate, licensed blood banks between January 2014 and March 2015, using a before after design. A total of 310 women (143 before and 177 after), who needed emergency blood transfusion during their perinatal period, as determined by a medical professional, were included in the study. A median linear regression model was employed to assess the adjusted effect of BIMA on transfusion time.
Results: After the introduction of BIMA, the median duration between the identified need for blood and blood transfusion reduced from 152 to 122 minutes (P<0.05). For PPH specifically, the reduction was from 175 to 113 minutes (P<0.05). After introducing BIMA and after adjusting for criteria such as maternal age, education, parity, duty roster of providers, and reasons for blood transfusion, a 24 minute reduction in the time was observed between the identified need for blood and transfusion (P<0.001).
Conclusion: BIMA was effective in reducing delays in blood transfusion for emergency obstetric patients. This pilot study suggests that implementing BIMA is one mechanism that has the potential to streamline blood transfusion systems in Bangladesh.
Keywords: blood transfusion, online application, postpartum hemorrhage, mhealth, Bangladesh
Introduction
Globally, postpartum hemorrhage (PPH) accounts for one-quarter of maternal deaths, and the related morbidity and mortality burden is found to be the highest in developing countries.1 A systematic review examining the geographic distribution of PPH found that PPH accounts for 30%–34% of all maternal deaths in Asia and Africa.2 In Bangladesh, 31% of maternal deaths are due to PPH.3 Development of PPH is unpredictable, and if untreated PPH can kill the mother within 2 hours.4 The extent of morbidity and mortality associated with PPH is dependent on quick diagnosis and prompt administration of effective treatment. Management of PPH includes administration of non-pharmacological and/or pharmacological agents, (uterotonic drugs), uterine tamponade or a range of surgical techniques to control bleeding, and blood transfusion (BT) if blood loss becomes excessive.5 To prevent a significant number of preventable maternal deaths and morbidities due to obstetric hemorrhage, access to adequate and safe blood for transfusion, during and after delivery, is critical.6 Evidence has shown that, globally, up to 150,000 pregnancy-related deaths could be avoided each year if women had access to safe and sufficient blood.7 BT is one of the eight signal functions that should be available in a designated comprehensive emergency obstetric and new-born care facility.8
Accessing blood for medical emergencies in the Bangladeshi context
BT services have been identified as an integral and indispensable part of the health care system in Bangladesh, although there remain significant gaps between policy and practice.9 In 2002, Bangladesh enacted a safe BT law, aimed at ensuring the safety, adequacy, accessibility, and efficiency of the national blood supply.10 Ensuring a safe blood supply demands that there are willing donors and an existence of mechanisms and oversight to ensure safe preparation and storage of blood products. For blood to be safe, staff must be trained to follow health and safety procedures, and blood storage facilities must have the equipment and supplies to ensure that blood is adequately tested and safely stored. For both government and non-government transfusion centers, the Bangladesh Gazette (2008)11 published rules to ensure standard laboratory practices in blood grouping, compatibility testing, component preparation, storage, and transportation of blood and blood products. As of 2012, there were 203 government-approved (licensed) BT centers in the country, while the number of unauthorized BT centers is unknown.12 According to the Bangladesh Safe Blood Transfusion Program report in 2010, only 72% of the licensed BT centers were functional, and most BT centers were located outside of health facilities.13 Many BT centers, due to inadequate funding and a lack of oversight, face a shortage of reagents, apparatus, and skilled workers.14,15 It is estimated that approximately 600,000 units of blood are required, annually, in Bangladesh.12
When emergent blood is needed, on-site blood facilities are rare, and the onus of obtaining blood often falls upon attendants/relatives of patients. In many instances patient attendants/relatives are unaware of where and how to obtain lifesaving blood. This has resulted in a cadre of unregulated blood brokers, aware of blood services, who often wait outside the ward for attendants/relatives who need blood. For a fee, these brokers are often the only option from whom family members can obtain blood when it has been deemed medically necessary. Unfortunately, there is no way to ensure that these brokers provide services in a timely manner, nor is there any mechanism to ensure that these brokers provide safe blood.16
The World Health Organization (WHO) has declared that mobile-health (mHealth) has the potential to transform the face of health service delivery across the globe.17 Recently, worldwide efforts have been undertaken to utilize smart phone applications in health service delivery. Building on these efforts, our team endeavored to utilize innovations in mHealth to make quick access to BT a reality in Bangladesh. Our goal was to digitalize information about the location and availability of blood and make the blood acquisition process more convenient and accessible, particularly in emergency situations. In our vision, the digitalization of blood center data, and systematically linking health facilities with blood banks, would be an effective strategy in streamlining the transfusion process.
We performed an extensive review of existing published and gray literature on technology-based, blood-availability systems. Although India, Ireland, and three states in the USA have designed interventions using mobile technology to streamline the blood availability system18,19 no study has been undertaken in Bangladesh to explore this issue. The present study was undertaken to develop and implement a digitalized system called the “Blood Information Management Application” (BIMA) at a tertiary level public hospital of Bangladesh to streamline access to safe and adequate blood for emergency obstetric patients.
Developing BIMA
The BIMA system is an online blood information management application that provides access to different blood information databases (within and outside the hospital). It captures information regarding name and location of proximate, licensed blood centers, current stock of each type of blood available in each facility, and donor list (along with blood groups and Rh typing), and it has a booking information system to reserve specific quantities and types of blood.
Figure 1 depicts the BIMA flowchart. First, a provider determined a particular patient’s need for BT in the obstetrical ward. Then, a study team research assistant (RA), who was in obstetrical ward, operated BIMA through a mobile device (Figure 2). The application allowed the RA to access the blood information databases connected with the system (the blood bank of Dhaka Medical College Hospital [DMCH] and the Sandhani blood bank). Using the BIMA information database, the RA identified the facility to be stocked with the required blood (by matching with the group) and ensured that the facility had the requisite number of blood units needed. After sending the request for a particular blood type, a booking identification number (ID) was simultaneously generated at both the mobile end and at the blood center. If both centers had adequate supplies of the needed blood, then the ID was generated for the center that responded more rapidly. The booking ID was visible to the blood bank personnel through the web application at his/her computer (Figure 3). This booking number along with the name and address of the blood center was provided to the patient’s relative(s) so that they could purchase the blood from the licensed blood bank.
  | Figure 1 BIMA flowchart. |
  | Figure 2 Computer screenshot of blood requisition form from ward. |
  | Figure 3 Computer screenshot of BIMA form from blood bank. |
Implementing the BIMA system
Between August 2014 and mid-October, four orientation sessions were conducted on the BIMA system and the relevant technologists at the blood centers to train providers (doctors, study RAs, Sandhani medical students). These orientation sessions served to introduce providers to the BIMA system and to address any concerns that the providers had. There were mixed responses from the technologists, and later a few showed some resistance to BIMA implementation. Additionally, all providers of each center underwent a 1-day hands-on training on the BIMA system. Refresher trainings were conducted 1 month after the start of data collection.
Materials and methods
The study was conducted between January 2014 and March 2015 in the DMCH, a 2,300 bed, tertiary-level hospital situated at Dhaka, Bangladesh. A before and after design was used to assess changes in the lag time between doctor’s advice for BT and the actual time of transfusion in the respective ward. The DMCH Blood Bank and Sandhani are the only two DMCH-affiliated (licensed) blood centers proximate to the hospital.
The sample size was calculated to test a 40% reduction in mean lag time (between doctor’s advice for BT and the actual time of receiving blood) from 2.21 hours (standard deviation [SD]: 2.63). The 2.2 hours lag time was estimated from a pilot study conducted at similar tertiary hospital in Dhaka. Using 80% power and 95% confidence intervals, and an expected 5% refusal rate, the estimated minimum numbers were 178 subjects for each before and after the intervention. This study enrolled mothers from the obstetric ward of the DMCH before (March and mid-July 2014, n=143) and after BIMA was implemented (October 2014 and January 2015, n=177). Before the introduction of the BIMA application, there was no clear system for acquiring blood; blood used for transfusion was collected mainly through multiple sources, and mainly from informal blood brokers. After BIMA was introduced, all blood was collected using the BIMA system. As women were not in a position to participate in the interview, due to emergency situations, this study interviewed the relatives or the attendants of women participants after taking their consent. This study experienced no refusal cases.
We employed structured questionnaires before and after introducing BIMA in order to calculate the lag time. Study RAs were placed round-the-clock at the obstetrical ward of DMCH to collect the required information from the blood centers, patients, and patient attendants.
The outcome (between doctor’s advice for BT and the actual time of receiving blood in the respective ward) was compared between the two groups – before and after the intervention. Bivariate analyses were performed using chi-square test (X2) to find out the variations in the basic characteristics of the respondents selected before and after the intervention. Median time was computed instead of mean and non-parametric testing was used as the data were not normally distributed. We compared median time (minutes) in outcome variable through Wilcoxon rank-sum test (Mann–Whitney median test) with 95% confidence intervals (CI). As time data were not normally distributed, we used median regression, a non-parametric regression model/quintile regression model.20–22 This median regression model has been used to identify the implication of introducing BIMA. Median regression expresses the median of the conditional distribution of the dependent variable as a linear function of the independent variables. This method is similar to ordinary regression. Data were analyzed using SPSS v.20 and we performed median regression analysis using Stata 12 software.
Ethical approval
Ethical approval was obtained from both the institutional review board of International Centre for Diarrheal Disease Research, Bangladesh (icddr,b) and DMCH prior to the implementation of the study.
Results
Background characteristics of mothers
We considered 143 and 177 cases for the before and after phase of BIMA intervention, respectively. About 42% of women, in both the phases, had completed at least a secondary education. There were no statistical differences between the two populations, with both being predominantly Muslim, parity 1–2, gravida 3 or more, with at least a primary and secondary education. Unsurprisingly, O positive (+ve) blood group was found to be the most common both before (34.3%) and after (44.1%) the implementation of BIMA (Table 1).
  | Table 1 General characteristics of the participants |
Differences in blood availability time
We analyzed the median value of the time (in minutes) taken for transfusion. Time for blood collection was calculated as the difference between doctor’s advice for BT and the actual time of receiving blood in the respective ward. Figure 4 shows the overall total time of blood collection before and after the administration of BIMA. After implementing BIMA in the obstetrical ward of DMCH, the median duration for blood availability declined from 152 minutes to 122 minutes.
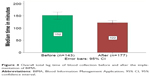  | Figure 4 Overall total lag time of blood collection before and after the implementation of BIMA. |
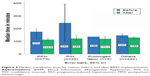
The major obstetric causes associated with the need for BT during the study period were PPH (n=73), pregnancy-induced hypertension (PIH) (n=20), prolonged labor (n=5), anemia (n=21), and cesarean section (n=47). For PPH, the median time of blood availability reduced from 175 minutes to 112 minutes after the introduction of BIMA. For PIH, the time declined from 245 minutes to 122 minutes (Figure 5).
Of all the reasons of BT, after the introduction of BIMA, the highest reduction in time was observed for women with PIH (before =245 minutes, after =122 minutes), followed by women with PPH (before =175 minutes, after =112.5 minutes). BIMA saved more than 2 hours (123 minutes) for PIH cases and more than 1 hour (62.5 minutes) for PPH cases.
It was possible to save about 62 minutes (more than 1 hour) for PPH patients after the introduction of BIMA in the obstetric ward of DMCH (before: 175 minutes and after 112.5 minutes) (P<0.05). For the women with prolonged labor, it took 136 minutes in the before phase, while it reduced to 120 minutes in the after phase. Also, in case of other causes that led women to BT, the time was 147 minutes in the before phase, whereas the time decreased to 130 minutes in the after phase. BIMA was also able to reduce blood availability time throughout the day (Figure 6).
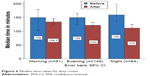  | Figure 6 Median time taken by duty roster. |
Table 2 shows how BIMA has reduced the time of blood collection after adjustment with age, education status, parity of women, duty roster periods, and reasons for BT. After introducing BIMA, on an average, the delay (between decision making and BT) reduced by 24 minutes.
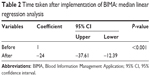  | Table 2 Time taken after implementation of BIMA: median linear regression analysis |
Discussion
This study assessed the impact of a digitalized blood bank information system on reducing the time between a doctor’s advice to collect blood and safe transfusion in a public medical college hospital in Bangladesh. The DMCH is the busiest hospital in Bangladesh, which serves a population that is predominantly poor, and many patients come from underprivileged socioeconomic groups. In this context, BIMA was successful in reducing the time to BT in obstetric emergencies. This study has demonstrated that with the help of BIMA, it is possible to streamline the BT process and ensure safe blood. This has clinical significance, particularly for PPH, where the BIMA system reduced the lag time for transfusion by 62 minutes.
Electronic blood donation systems have been tested in India and Bangladesh,23–25 but none of them have directly linked patients, blood banks, and hospitals. Other electronic information systems, tested in Thailand and the UK, have reduced the blood collection time significantly, but they did not follow conventional grouping and cross-matching process. Instead, they were programmed only to receive red blood cells, which is not realistic in Bangladeshi context.26–28
BIMA has documented that the highest lag time (48 minutes) was reduced during night roster, when most of the resources, and unofficial blood brokers, are usually not available or difficult to access. This is an important finding that could make hospital management optimize their resources, and BIMA could be a great help during such or similar situations (eg, during national holidays, festivals, and vacation).
Thirty-one percent of mothers still die due to PPH in Bangladesh; ensuring timely and safe BT can save their lives. This study was implemented in an urban setting, where blood banks are proximate to health facilities; this is not the case in rural areas. The proposed BIMA approach could be a solution for making access to safe BT a reality to all clients attending public hospitals in Bangladesh. However, implementing BIMA at scale will be a challenge in the existing Bangladeshi health system as most of the hospitals do not have the setup or incentive to introduce it.
Limitations
In some cases, the BIMA system was not as fast as the existing brokers (Dadu-informal blood brokers) in collecting blood for transfusion. It was observed in several occasions that these brokers were able to collect blood within 15–30 minutes after advice for transfusion by the doctors. This rapid collection of blood by the Dadus was far from the norm, and the head of blood transfusion department of DMCH mentioned that it usually took more than an hour for brokers to acquire blood. More alarmingly, blood provided by the Dadus does not undergo any formalized screening procedures. Any screening proof from outside the medical college hospital was questionable. In 34 cases, before the introduction of BIMA, we could not verify the blood type and screening status, and hence they were removed from the analyses. This could hamper the power of the study. After the implementation of the BIMA system, the broker group had no scope of collecting blood either from blood bank or from Sandhani. The broker system, that currently exists, needs further in-depth evaluation and mechanisms to ensure that it is providing safe blood. One possible way to do this would be to incorporate them into the BIMA system.
Data quality of the study was assured through rigorous routine field supervision and ongoing training in data collection. Broad inclusion criteria, similarity of the intervention groups at enrolment, separation of the recruitment from the evaluation team, and comprehensive follow-up helped to reduce bias in the study. The fact that our findings are internally consistent and biologically plausible with logical chronology suggests that they are reliable and representative of the target population.
Conclusion
Digitalization of the blood management system effectively reduced the delay in BT among the obstetric patients. BIMA was able to secure BT, for PPH patients, within a 2-hour period, which has clinical significance. Currently Bangladesh is moving toward electronic data collection and electronic record-keeping systems, and this study provides evidence that digitalizing blood information systems has the potential to reduce lags in transfusion time and ensures that safe blood is used. Findings of this study show that Bangladesh should take efforts to streamline all aspects of its health information systems.
Acknowledgments
This project was made possible with support from the Maternal Health Task Force at the Harvard TH Chan School of Public Health through Grant #01065000621 from the Bill & Melinda Gates Foundation. The authors would also like to acknowledge the contribution of the current donors who provided unrestricted support to icddr,b: Australian Agency for International Development (AusAID), Government of the People’s Republic of Bangladesh, Canadian International Development Agency (CIDA), Swedish International Development Cooperation Agency (Sida), and the Department for International Development, UK (DFID). We also kindly acknowledge the contribution made by Prof Ferdousi Islam, Head, Department of Gynaecology and Obstetrics, and Prof Hosne Ara Begum, Head, Department of Blood Transfusion from Dhaka Medical College Hospital for supporting this study.
Author contributions
AR has conceptualized the study and AR, SA, SSI, FA, MR, MEC, AA, and IA designed the methods. AR, SA, MKN, FA, and NB were involved with the implementation process. AR, MKN, SSI, IA, and AA led the data analysis, interpretation of results, and development of first draft. All the authors contributed toward drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Maternal Mortality in 2005: Estimates Developed by WHO, UNICEF, UNFPA, and the World Bank. Geneva: World Health Organization; 2007. | ||
Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–1074. | ||
National Institute of Population Research and Training. Bangladesh Maternal Mortality and Health Care Survey 2010. Dhaka: National Institute of Population Research and Training; 2012. | ||
Walraven G, Telfer M, Rowley J, Ronsmans C. Maternal mortality in rural Gambia: levels, causes and contributing factors. Bull World Health Organ. 2000;78(5):603–613. | ||
Balki M, Dhumne S, Kasodekar S, Seaward G, Carvalho JC. Blood transfusion for primary postpartum hemorrhage: a tertiary care hospital review. J Obstet Gynaecol Can. 2008;30(11):1002–1007. | ||
United Nations Children’s Fund. Guidelines for Monitoring the Availability and use of Obstetric Services. New York: United Nations Children’s Fund; 1997. | ||
World Health Organization. Blood Transfusion Safety. Geneva: World Health Organization; 2006. | ||
World Health Organization. Monitoring Emergency Obstetric Care: A Handbook. Geneva: World Health Organization; 2009. | ||
Nurunnabi ASM, Jahan M, Alam MA, Hoque MM. Safe blood transfusion and ethical issues in transfusion medicine. J Dhaka Med Coll. 2010;19(2):144–149. | ||
Bangladesh Health Watch. Bangladesh Health Watch Report 2009: How Healthy Is Health Sector Governance? Dhaka: University Press Limited; 2010. | ||
Ministry of Health and Family Welfare. Bangladesh Gazette, 2008: no. Extraordinary: 3639–3722. Dhaka, Bangladesh: Ministry of Health and Family Welfare; 2008. | ||
Ministry of Health and Family Welfare, Directorate General of Health Services. Situation Assessment of Public and Private Blood Centres in Bangladesh. Dhaka, Bangladesh: Directorate General of Health Services, Ministry of Health and Family Welfare; 2012. | ||
Ministry of Health and Family Welfare, Directorate General of Health Services. Home safe blood transfusion. 2010. Available from: http://hsmdghs-bd.org/Safe%20Blood%20Transfusion.htm. Accessed July 7, 2016. | ||
Hossain M. Importance of safe blood transfusion in prevention of blood borne diseases. Souvenir. In: 13th Sandhani Central Annual Conference, November 12, 1994. Rajshahi: Rajshahi Medical College; 1994. | ||
Bhuiya I, Hossain SMI, Streatfield K. Situation of Blood Testing/Screening in Relation to HIV/AIDS in Dhaka City. Dhaka: Population Council; 1995. | ||
Akhter S, Anwar I, Akter R, et al. Barriers to timely and safe blood transfusion for PPH patients: evidence from a qualitative study in Dhaka, Bangladesh. PLoS One. 2016;11(12):e0167399. | ||
World Health Organization. mHealth: new horizons for health through mobile technologies: based on the findings of the second global survey on eHealth; GLOBAL Observatory for eHealth series – volume 3. Geneva: World Health Organization; 2011. | ||
Mostafa AM, Youssef AE, Alshorbagy G. A framework for a smart social blood donation system based on mobile cloud computing. Available from: http://arxiv.org/pdf/1412.7276v1. Accessed July 7, 2016. | ||
Kulshreshtha V, Maheshwari S. Blood Bank Management Information System in India. Int J Eng Res Appl. 2011;1(2):260–263. | ||
Koenker R. Quantile regression: statistical theory and methods. In: Encyclopedia of Environmetrics. Hoboken, NJ: John Wiley & Sons, Inc.; 2013. | ||
Kottas A, Gelfand AE. Bayesian semiparametric median regression modeling. J Am Stat Assoc. 2001;96(456):1458–1468. | ||
Ying Z, Jung SH, Wei LJ. Survival analysis with median regression models. J Am Stat Assoc. 1995;90(429):178–184. | ||
Singh R, Bhargava P, Kain S. Smart phones to the rescue: the Virtual Blood Bank Project. IEEE Pervasive Comput. 2007;6(4):86–89. | ||
Rahman MS, Akter KA, Hossain S, Basak A, Ahmed SI. Smart blood query: a novel mobile phone based privacy-aware blood donor recruitment and management system for developing regions. In: Advanced Information Networking and Applications (WAINA), 2011 IEEE Workshops of International Conference, 22–25 March 2011. Singapore: IEEE; 2011:544–548. | ||
Islam AHMS, Ahmed N, Hasan K, Jubayer M. mHealth: blood donation service in Bangladesh. In: Informatics, Electronics & Vision (ICIEV), 2013 International Conference, 17–18 May 2013. Dhaka: IEEE; 2013:1–6. | ||
Turner CL, Casbard AC, Murphy MF. Barcode technology: its role in increasing the safety of blood transfusion. Transfusion. 2003;43(9):1200–1209. | ||
Davies A, Staves J, Kay J, Casbard A, Murphy MF. End-to-end electronic control of the hospital transfusion process to increase the safety of blood transfusion: strengths and weaknesses. Transfusion. 2006;46(3):352–364. | ||
Staves J, Davies A, Kay J, Pearson O, Johnson T, Murphy MF. Electronic remote blood issue: a combination of remote blood issue with a system for end-to-end electronic control of transfusion to provide a “total solution” for a safe and timely hospital blood transfusion service. Transfusion. 2008;48(3):415–424. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.