Back to Journals » Journal of Blood Medicine » Volume 12
Can Hematological Ratios Predict Outcome of COVID-19 Patients? A Multicentric Study
Authors Aly MM , Meshref TS, Abdelhameid MA, Ahmed SA, Shaltout AS, Abdel-Moniem AE , Hamad DA
Received 20 April 2021
Accepted for publication 25 May 2021
Published 29 June 2021 Volume 2021:12 Pages 505—515
DOI https://doi.org/10.2147/JBM.S316681
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Mai M Aly,1,* Taghreed S Meshref,2,* Marwa A Abdelhameid,3 Shimaa A Ahmed,4 Asmaa S Shaltout,5 Alaa Eldin Abdel-Moniem,2 Dina A Hamad2
1Clinical Hematology Unit, Department of Internal Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt; 2Critical Care Unit, Department of Internal Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt; 3Department of Internal Medicine, Faculty of Medicine, Aswan University, Aswan, Egypt; 4Department of Internal Medicine, Faculty of Medicine, Qena University, Qena, Egypt; 5Department of Medical Microbiology & Immunology, Faculty of Medicine, Assiut University, Assiut, Egypt
*These authors contributed equally to this work
Correspondence: Mai M Aly
Clinical Hematology Unit, Department of Internal Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt
Tel +201223971678
Email [email protected]
Introduction: Coronaviruses belong to a large family that leads to respiratory infection of various severity. Hematological ratios are indicators of inflammatory response widely used in viral pneumonia with affordability in developing countries.
Purpose: Study the role of the neutrophil lymphocyte ratio (NLR), derived NLR ratio (d-NLR), platelet lymphocyte ratio (PLR), and lymphocyte monocyte ratio (LMR) in predicting the outcome of COVID-19 Egyptian patients.
Methods: A retrospective study on 496 COVID-19 Egyptian patients, managed in four tertiary centers, grouped into non-severe, severe, and critical. Patients’ laboratory assessment including total leucocyte count (TLC), absolute neutrophil count (ANC), absolute lymphocyte count (ALC), absolute monocyte count (AMC), NLR, d-NLR, LMR and, PLR were reported as well as C reactive protein (CRP), D-dimer and serum ferritin.
Results: TLC, ANC, AMC, NLR, d-NLR and, PLR were highest in the critical group (p< 0.001 for all except AMC p=0.033), while this group had the least ALC and LMR (p=0.049 and < 0.001, respectively). Higher CRP and d-dimer levels were reported in the critical group (p< 0.001). At the same time, higher ferritin was found in the severe group more than the critical and non-severe groups (p< 0.001, p=0.005, respectively). We calculated the optimal cut-off values of the hematological ratio; NLR (3.5), d-NLR (2.86), PLR (192), and LMR (3). D-NLR had the highest specificity (89.19%), while NLR had the highest sensitivity (71.38%). By univariate logistic regression, age, DM, HTN, cardiovascular diseases, COPD, NLR, d-NLR, LMR and PLR, CRP, steroid, oxygen aids, and mechanical ventilation were associated with the severity of COVID-19. Still, only age, NLR, CRP, and oxygen aid were independent predictors in multivariate logistic regression.
Conclusion: NLR is a predictor for severity in COVID-19. LMR, d-NLR, and PLR may assist in risk stratification.
Keywords: COVID-19, NLR, d-NLR, LMR, PLR, Egypt
Introduction
COVID-19 virus, a single-chain enveloped RNA virus,1 causes multisystemic infections in animals and humans, mainly leads to respiratory tract infection.2 Classically patients exhibit mild symptoms such as fever, sore throat, and upper respiratory tract infections.3 Severe respiratory tract infection that contributes to the syndrome of adult respiratory distress, multiple organ failure, and even death is reported, especially in the elderly and in patients with comorbidities.4,5 Declaring COVID-19 as a pandemic, serious morbidity, and mortality; created an urgency to study diagnostics, treatment, and prognostic markers.4
Inflammatory biomarkers representing the immune status are possible predictors of prognosis for COVID-19.5 Hematological ratio such as neutrophil to lymphocyte ratio (NLR), derived NLR ratio (d-NLR) (calculated by neutrophil count divided by the result of WBC count minus neutrophil count), platelet to lymphocyte ratio (PLR), and lymphocyte to monocyte ratio (LMR) are systemic inflammatory markers that have already been extensively investigated as a potential predictor of viral pneumonia.6 Such ratios are useful, inexpensive prognostic indicators that can be widely tested in developing countries with respectable significance in viral pneumonia, including COVID-19.6–8
The diagnostic use of NLR in bacteria9 and viral pneumonia6 as well as in COVID-19 positive patients has been documented; the NLR is substantially greater in COVID-19 cases vs controls.8 NLR can be easily used as a rapid, inexpensive, available prognostic indicator.6,8 Both PLR and LMR are considered indicators of the systematic inflammatory response and useful predictors for the prognosis in viral pneumonia.10 More studies are demanded to decide the applicable threshold of d-NLR, PLR, and LMR and decide their predictive value.
This retrospective, multi-centric study was conducted to investigate the complete blood count parameters (NLR, d-NLR, PLR, and LMR) as inflammatory biomarkers and prognostic indicators in 496 COVID-19 positive cases.
Methods
Study Design
The study was a retrospective study, including 496 COVID 19 patients, diagnosed based on guidance from WHO with Positive SARS-CoV-2 RNA identification by real-time PCR methods in throat swab specimens.11 The study included patients admitted to four major tertiary centers in Upper Egypt (Assiut University Hospital, El Rajhi Hospital, Aswan University Hospital, South Valley University Hospital) through June 2020.
Data of the Patients
Data of the patients were gathered from the hospital reports following the authorization of the local research ethics committee (IRB number: 17300513) according to the Declaration of Helsinki. It included: age, sex, history of smoking, diabetes, hypertension, chronic chest disease and cardiovascular disease, duration of hospital admission and outcome, treatment included steroid and oxygen supply either by low flow oxygen supplementation (nasal cannula, facial masks, or non-rebreather facial masks) or high flow oxygen supplementation (high flow nasal cannula, continuous positive ventilation pressure (CPAP) or mechanical ventilation).
Investigations Included
Complete blood count; total leukocyte count (TLC), red blood cells, hemoglobin level, absolute lymphocyte count (ALC), absolute monocyte count (AMC), absolute neutrophil count (ANC), NLR (ANC/ALC), derived NLR ratio (d-NLR; calculated by ANC divided by the result of TLC count minus ANC), PLR (Platelet count/ALC) and LMR (ALC/AMC). Inflammatory markers; CRP (C-reactive protein) and serum ferritin and coagulation factor; D-dimer. All collected laboratory results are at the peak of the disease. Definition as the beginning of the symptoms that meet the categories of severity of illness as determined by WHO.12,13
Computed tomography (CT) of the chest of the patients was classified into specific findings suggestive to COVID19 infection as bilateral or unilateral multifocal ground-glass opacities that classically predominate in the peripheral, posterior, and basal part of the lungs or other less specific findings. CORADS classification was scored from very low or CO-RADS 1 to very high or CO-RADS 6 based on the CT findings.
Patients were classified into the following categories of severity of illness:14
1) Critical: patients with any of the following criteria: respiratory failure that requires artificial ventilation, shock, or other organ damage that requires intensive care unit monitoring and treatment.
2) Severe: patients with a ratio of arterial partial oxygen pressure to inspired oxygen fraction (PaO2/FiO2) <300 mmHg, respiratory rate >30 breaths per minute, lung infiltrates >50%, or patients with SpO2 <94% in room air.
3) Non-severe: patients who did not meet the criteria of critical or severe illness.
All patients were treated according to the World Health Organization’s provisional guidelines (WHO). All patients received steroids, and none of the patients received immunomodulatory drugs.2,11
Statistical Analysis
SPSS version 25.0 was used for data management and data analysis. Quantitative variables were first subjected to the normality test (Kolmogorov v Smirnov). Continuous variables were presented median (interquartile range), and the Kruskal–Wallis test assessed their differences. Categorical variables were described as numbers (percentage) and were compared by the chi-square test and fisher’s exact test. The optimal cut-off values of the continuous NLR, d-NLR, PLR, and LMR were calculated using the receiver operating curve (ROC) analysis. The Kaplan–Meier survival analysis and COX regression analysis were used to investigate the independent adverse factors that might check patients’ recovery and discharge with COVID-19. The demographics and laboratory data with significant differences between the three groups were assessed by univariate and multivariate logistic regression analysis to discover the independent early predictors and risk factors associated with the disease severity of COVID-19. A two-sided P<0.05 was considered statistically significant.
Results
Characteristics of the Studied Population
The studied population were divided into 3 groups, non-severe (n=185; 37.3%), severe (n= 165; 33.3%) and, critical (n=146; 29.4%); older patients were found in the critical group (median age =61) then the severe group (median age=55) while, the youngest were among the non-severe group (median age =33.5) with a significant difference between them (p <0.001). Most of the patients were males in all groups.
In comparing associated co-morbidities, the critical group was more associated with diabetes mellitus (DM), hypertension (HTN), cardiovascular diseases and, chronic obstructive pulmonary diseases (COPD) versus the non-severe and severe groups (p <0.001).
Regarding hematological parameters, the hemoglobin level was least in the severe group [median (IQR); 12(10–13)], and highest in the non-severe group [Median (IQR);12 (11–14) p =0.04]. Surprisingly, platelets were lowest in the non-severe group, with a significant difference between the three groups (p<0.001). TLC, ANC, AMC, NLR, d-NLR and, PLR were highest in the critical group, followed by the severe group and least in the non-severe group with a significant difference (p<0.001 for all except AMC p-value=0.033). ALC and LMR were inversely proportionate to severity (p = 0.049 and <0.001, respectively).
Higher CRP and d-dimer levels were reported in the critical group (p <0.001). At the same time, higher ferritin was found in the severe group more than the critical and non-severe groups (p <0.001, p=0.005 respectively).
The critical group patients had multi-slice computed tomography (MSCT) imaging, which showed more extensive lesions (either bilateral lesions or multiple unilateral lesions) than in the non-severe and severe groups (p <0.001). We used CORAD system to assess the probability of COVID-19 infection in our studied cohort; most of them were CORAD 6. CORAD 1, 2 were reported in the non-severe group, while only three patients were in the severe group.
In comparing the oxygen supplementation given to the patients, most of the severe group patients (83%) received oxygen aid, and only 10% were mechanically ventilated. In comparison, 92.5% received oxygen aids in the critical group, and 72.4% required mechanical ventilation.
Most of the non-severe group recovered (93%) and discharged home. The death was more in the critical (65.1%) and severe (15.2%) groups. Demographic and baseline data of the studied cohort are shown in (Table 1).
 |
Table 1 Characteristics of the Studied Population |
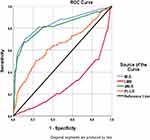
ROC Curve to Detect Optimal Cut-off Values of the Hematological Ratios
We analyzed the optimal cut-off values of NRL, d-NLR, LMR, and PLR calculated by the ROC analysis and presented in (Figure 1). Areas under the curve (AUC) of NLR, d-NLR, PLR and LMR were 0.838, 0.817, 0.643, and 0.285, respectively. LMR could not be used as a potential diagnostic biomarker for subsequent analysis because its AUC was less than 0.50. The optimal cut-off values were NLR (3.5), d-NLR (2.86), and PLR (192). D-NLR had the highest specificity (89.19%), followed by NLR (87%) then PLR (77.62%). The most heightened sensitivity was in favor of NLR (71.38%), then the d-NLR (67.2%), and the PLR (50%; Table 2).
 |
Table 2 ROC Curve Analysis of All Studied Population to Detect Optimal Cut-off Values, Sensitivity and Specificity of the Hematological Ratios |
Survival Analysis with Kaplan–Meier Curves
The estimated mean time until death was 21.3 days for non-severe vs 19.1 days for severe vs 16.2 days for critical patients (p<0.0001). The survival probability is lowest in critical patients at all-time points, so they are less likely to survive (Figure 2A).
We estimated the mean survival time according to NLR (estimated mean time until death is 20.5 days for NLR <3.5 and 17.7 days for NLR >3.5; p<0.001), d-NLR (The estimated mean time until death is 20.2 days for d-NLR <2.5 and 17.5 days for d-NLR >2.5; p<0.001), and PLR (the estimated mean time until death is 19.3 days for PLR <192 and 18.8 days for PLR>192; p=0.04). So, it is obvious that those patients with NLR >3.5, d-NLR >2.5, or PLR> 192 are less likely to survive (Figure 2B–D).
Identification of Possible Predictors of Severity in COVID-19 Patients
To determine the effect of hematological ratios on the prognosis of COVID-19 patients, we also performed Kaplan–Meier survival analysis and COX regression analysis to explore the possible independent predictors for severe COVID-19. Further univariate and multivariate analysis of COX regression showed that the estimated NLR (HR 1.056, 95% CI 1.0.37–1.075), d-NLR (HR 1.075, 95% CI 1.045–1.104), and PLR (HR 1.001, 95% CI 1–1.002) identified by univariate Cox regression but in multivariate Cox regression, only elevated NLR (HR 1.046, 95% CI 1.024–1.069) was the independent adverse factor affecting recovery and discharge of patients with COVID-19.
The univariate logistic regression analysis showed age, DM, HTN, cardiovascular diseases, COPD, NLR, d-NLR, LMR, PLR, CRP, d-dimer, steroid, oxygen aids, and mechanical ventilation were associated with increased severity of COVID-19. Subsequently, all the above univariate analysis parameters with statistical significance were integrated for in-depth analysis into the multivariate logistic regression model. In the multivariate logistic regression model, considering the likelihood of overfitting, we assumed a stepwise forward method for logistic regression analysis to decrease the number of independent variables entering the model to reduce the probability of overfitting the model.
The results showed that the early independent predictors for severe COVID-19 were age, NLR, CRP, d-dimer, and oxygen aid upon entry, while the role of d-NLR, LMR, and PLR is unclear (Table 3).
 |
Table 3 Identification of Possible Predictors of Severity in COVID-19 Patients |
Discussion
A cluster of cases of pneumonia of unknown etiology started to emerge in Wuhan, China, at the end of 2019, a striking event that terrifies the whole world. A rapid spread of that infection took place with a relatively low mortality rate.3 At the end date of the collection of data (2020-12-5), more than one and a half million deaths were reported to WHO. Mortality rates vary from one region to another; it was less than 2.5% in CDC, China, but in Egypt, the mortality rate was higher, reaching up to 6.7%. Lack of accurate recording and delayed diagnosis may play a significant role in explaining such a high mortality rate. This issue pushed us to investigate possible cheap, rapid, and simple predictors that may force attention to more risky victims.
Not enough data supporting increased liability of COVID-19 infection to patients with chronic diseases but, many previous researchers –in line with our results- confirmed the increased severity in older people, especially those suffering from diabetes mellitus (DM),15 hypertension (HTN)3 cardiovascular diseases;16 also, we reported increased severity in chronic obstructive pulmonary disease (COPD) patients which appears logic as the virus affects mainly the respiratory system and it is well known that serious adverse effects are associated with respiratory viral infections in those with COPD;17 chronic pulmonary diseases, however, are under-reported, according to the first epidemiological studies and detected only in 0.3–2.5% without a significant increase in risk as it was expected.18
C-reactive protein (CRP), d-dimer and ferritin, are markers that are extensively studied in COVID-19 infected victims;19–21 CRP levels correlate with the degree of inflammation. Interestingly, it was found to increase parallel to the increase in the diameter of the largest pneumonia lesion in COVID-19 patients;19 this supports our findings in which CRP is least in the non-severe group. D-dimer >2 was found in an early study to be the only factor associated with mortality in COVID-19 patients;20 this is also observed in our results, where it was highest in the critical group. Hyperferritinemia in a large meta‐analysis found to be associated with severe conditions and adult respiratory distress syndrome (ARDS).21 However, Wu et al found that ferritin was neither associated with ARDS nor severe cases of COVID-19.22 Surprisingly, in ours, mean ferritin levels favored the severe group, not the critical one.
The complete blood count is the test used to approach varieties of infections, with the advantages of being available and highly informative. In the Chinese population, leucopenia was reported in COVID-19 patients at the expense of lymphopenia without investigating its relation to disease severity.23 In our research, critical group patients suffered from the lowest lymphocyte count and the highest leukocyte count mostly due to neutrophilia, which could be explained by secondary bacterial infection occurred in most critical cases; this was also approved previously by a large meta-analysis;24 Recently, an autopsy report on a 50-year-old COVID-19 patient with ARDS revealed that although the peripheral blood lymphocyte count was dramatically decreased, there was inflammatory lymphocyte infiltration in both lungs and immune hyperactivation.25 Lymphopenia in COVID-19 patients can be explained by varieties of theories, as the ability of the virus to infect lymphocytes,26 to destroy lymphatic organs like the thymus and spleen, to disturb the levels of interleukin (IL)-6 and other inflammatory cytokines may result in lymphocyte apoptosis,27 and the inhibition of lymphocytes proliferation by metabolic molecules as the lactic acid.28 High monocyte count is another hematological parameter found more in critical population, representing the main generators of inflammation in COVID-19 and predisposing to serious outcomes mostly due to “a dysregulation syndrome”;29 in contrary, the difference in monocyte count between healthy and COVID-19 patients was not significant in another study.30
In the present study, we concentrated on the value of the hematological ratios as NLR, d-NLR, LMR and, PLR; our results supported a previous study that indicated that elevated NLR predicts poor outcome in COVID-19 patients so that those with high NLR attract more attention than those with low NLR.6,7,30 It is well established that NLR tends to increase with severe infection or systemic inflammation in line with the magnitude of clinical status and outcome.31 NLR, as well as, age were independent factors for poor clinical outcome of COVID-19 in Chinese cohort. NLR was one of the earliest studied markers that were correlated with severity.4,32,33 The following are potential explanations for these findings in COVID-19 patients; on the one hand, neutrophil releases large amounts of reactive oxygen species stimulates the antibody-dependent cell-mediated cell (ADCC) that can directly kill the virus, expose virus antigen, and activate cell-specific and humoral immunities.34 Besides, neutrophil produces numerous cytokines, such as circulating vascular endothelial growth factor (VEGF), which is profoundly expressed in COVID-19 patients.35 Moreover, several inflammatory factors, including interleukin-6, tumor necrosis factor-alpha, granulocyte colony-stimulating factor, and interferon-gamma factor, can trigger neutrophils.36–38 On the other hand, viral infections mostly affect lymphocytes,39 as systematic inflammation causes marked suppression of CD4+ T lymphocytes and increases CD8+ suppressor T lymphocyte.40 Thus, the critical group had higher NLR in comparison to severe and non-severe groups.
We studied a unique ratio derived from the NLR and named the d-NLR; this ratio was previously correlated with severity in chronic and neoplastic conditions.41 According to our knowledge, few studies had investigated its role in Covid-19 cases.4 Surprisingly, d-NLR carried the highest specificity among all studied factors with an optimal cut-off value of 2.86.
Another attractive ratio is LMR, which was signed in its lower values in critical patients of COVID-19. This finding was previously detected but concerning community-acquired pneumonia without identification of the causative pathogen.32,42,43 In another study, 190 COVID‐19 patients were enrolled, and LMR was significantly lower than the healthy group, with a significant negative correlation with body temperature.30
PLR is a new inflammatory index of interest, which is more valuable than the simple platelet or lymphocyte count. It mostly reflects changes in platelets, which are considered to have a unique role in inflammation and immune response,32,44 and higher in the critical group in our study. Previous investigators proved that peak PLR is more elevated in severe populations than in non-severe.45 In addition to a significant correlation with a poor prognosis on COVID-19,45 while others failed to detect any value to such index in COVID-19 patients.46
The optimal thresholds for NLR, d-NLR, PLR, and LMR were estimated using the ROC curve. The NLR yielded the highest AUC value than the other ratios, and its optimal cut-off value was 3.5, with 87.03% specificity and 71.38% sensitivity. In line with ours, a previous study showed that NLR had the highest AUC value with a relative cut-off value (3.3) with the highest specificity and sensitivity (63.6% and 88%, respectively).4 In a comparable study, the monocyte to lymphocyte ratio (MLR) had the highest AUC value with an optimal cut-off value of 0.23, with 90.00% specificity and 75.79% sensitivity (9). Some studies have shown that a surrogate predictor for influenza A is an LMR value <2.47
To predict severity in COVID-19 patients, regression analysis found that age, NLR, CRP, d-dimer, and oxygen aid on admission were reasonable predictors. In agreement with ours, previous research confirmed the prediction role of NLR in COVID-19 patients.4 Another one found that PLR value was an independent determining factor in severe patients.45
There are some limitations to this study. First, the research was retrospective. The data were recruited from hospital medical records after a set of criteria were met, which carry the risk of selection bias. Second, because of data limitation, we only used one measure in time rather than a longitudinal measure. Third, despite trials to exclude confounding factors, some confounders might affect the value of the hematological ratios.
In conclusion, NLR is a predictor for severity in COVID-19. LMR, d-NLR, and PLR may assist in risk stratification. According to our observations in this study, NLR can improve risk stratification of COVID-19 severity, LMR, d-NLR, and PLR can be quick, cost-effective, and interesting potential markers.
Ethical Approval
Authorization of the local research ethics committee of Assiut University.
Consent to Participate
Authors consented to participate in this research article.
Encrypted patients’ data was collected from hospital reports without a written consent; the reason for the written consent wavier was that the research presents no risk of harm to participants and involves no procedure for which written consent is normally required outside of the research context (retrospective survey) as well as participant verbally approved documentation and reporting of their medical and laboratory information. Approval of the local research ethics committee (IRB number: 17300513) according to the Declaration of Helsinki was provided. Patient data confidentiality was maintained.
Consent for Publication
Authors consented for publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Zhou Y, Yang Y, Huang J, Jiang S, Du L. Advances in MERS-CoV vaccines and therapeutics based on the receptor-binding domain. Viruses. 2019;11(1):60. doi:10.3390/v11010060
2. World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus ( nCoV) Infection is Suspected: Interim Guidance, 25 January 2020. World Health Organization; 2020.
3. Guan W-J, Liang W-H, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi:10.1183/13993003.00547-2020
4. Yang A-P, Liu J, Tao W, Li H-M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;106504.
5. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
6. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71(15):762–768. doi:10.1093/cid/ciaa248
7. Zahorec R, Hulin I, Zahorec P. Rationale use of neutrophil-to-lymphocyte ratio for early diagnosis and stratification of COVID-19. Bratisl Lek Listy. 2020;121(7):466–470. doi:10.4149/BLL_2020_077
8. Feng G, Zheng KI, Yan -Q-Q, et al. COVID-19 and liver dysfunction: current insights and emergent therapeutic strategies. J Clin Transl Hepatol. 2020;8(1):18. doi:10.14218/JCTH.2020.00018
9. Um S-J, Huh J-H, Choi IS, Lee S-K, Yoon N-B, Son C. Role of the neutrophil-lymphocyte count ratio in the differential diagnosis of pulmonary tuberculosis and bacterial community acquired pneumonia. In: C61. Immunodiagnostics for Latent Tuberculosis Infection and Tuberculosis. American Thoracic Society; 2012:A4737–A4737.
10. Ying H-Q, Deng Q-W, He B-S, et al. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol. 2014;31(12):305. doi:10.1007/s12032-014-0305-0
11. World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Middle East Respiratory Syndrome Coronavirus ( MERS-Cov) Infection is Suspected: Interim Guidance. World Health Organization; 2019.
12. Tian L, Li X, Qi F, et al. Harnessing peak transmission around symptom onset for non-pharmaceutical intervention and containment of the COVID-19 pandemic. Nat Commun. 2021;12(1):1–12. doi:10.1038/s41467-021-21385-z
13. Commission NH. Translation: diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7). Infect Microb Dis. 2020;2(2):48–54. doi:10.1097/IM9.0000000000000022
14. Wang M, Guo L, Chen Q, Xia G, Wang B. Typical radiological progression and clinical features of patients with coronavirus disease 2019. Aging (Albany NY). 2020;12(9):7652–7659. doi:10.18632/aging.103170
15. Ugwueze CV, Ezeokpo BC, Nnolim BI, Agim EA, Anikpo NC, Onyekachi KE. COVID-19 and diabetes mellitus: the link and clinical implications. Dubai Diabetes Endocrinol J. 2020;26(2):69–77. doi:10.1159/000511354
16. Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543–558. doi:10.1038/s41569-020-0413-9
17. Busse WW, Lemanske RF
18. Bernheim A, Mei X, Huang M, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):200463. doi:10.1148/radiol.2020200463
19. Wang L. C-reactive protein levels in the early stage of COVID-19. Med Mal Infect. 2020;50(4):332–334. doi:10.1016/j.medmal.2020.03.007
20. Yao Y, Cao J, Wang Q, et al. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a Case Control Study. J Intensive Care. 2020;8(1):49. doi:10.1186/s40560-020-00466-z
21. Cheng L, Li H, Li L, et al. Ferritin in the coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Lab Anal. 2020;34(10):e23618. doi:10.1002/jcla.23618
22. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934. doi:10.1001/jamainternmed.2020.0994
23. Gopaul C, Ventour D, Thomas D. Laboratory Predictors for COVID-19 ICU Admissions in a Caribbean Territory. 2020.
24. Xu X, Yu C, Qu J, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47(5):1275–1280. doi:10.1007/s00259-020-04735-9
25. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi:10.1016/S2213-2600(20)30076-X
26. Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):1–5. doi:10.1038/s41368-020-0074-x
27. Liao Y-C, Liang W-G, Chen F-W, Hsu J-H, Yang -J-J, Chang M-S. IL-19 induces production of IL-6 and TNF-α and results in cell apoptosis through TNF-α. J Immunol. 2002;169(8):4288–4297. doi:10.4049/jimmunol.169.8.4288
28. Fischer K, Hoffmann P, Voelkl S, et al. Inhibitory effect of tumor cell–derived lactic acid on human T cells. Blood. 2007;109(9):3812–3819. doi:10.1182/blood-2006-07-035972
29. Mangalmurti N, Hunter CA. Cytokine storms: understanding COVID-19. Immunity. 2020;53(1):19–25. doi:10.1016/j.immuni.2020.06.017
30. Peng J, Qi D, Yuan G, et al. Diagnostic value of peripheral hematologic markers for coronavirus disease 2019 (COVID-19): a Multicenter, Cross-Sectional Study. J Clin Lab Anal. 2020;34(10):e23475. doi:10.1002/jcla.23475
31. Curbelo J, Rajas O, Arnalich B, et al. Neutrophil count percentage and neutrophil–lymphocyte ratio as prognostic markers in patients hospitalized for community-acquired pneumonia. Arch Bronconeumol. 2019;55(9):472–477. doi:10.1016/j.arbr.2019.07.002
32. Asghar MS, Khan NA, Haider Kazmi SJ, et al. Hematological parameters predicting severity and mortality in COVID-19 patients of Pakistan: a retrospective comparative analysis. J Community Hosp Intern Med Perspect. 2020;10(6):514–520. doi:10.1080/20009666.2020.1816276
33. Asghar MS, Kazmi SJH, Khan NA, et al. Clinical profiles, characteristics, and outcomes of the first 100 admitted COVID-19 patients in Pakistan: a single-center retrospective study in a tertiary care hospital of Karachi. Cureus. 2020;12(6).
34. Kusumanto YH, Dam WA, Hospers GA, Meijer C, Mulder NH. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis. 2003;6(4):283–287. doi:10.1023/B:AGEN.0000029415.62384.ba
35. Kim S-L, Lee S-T, Trang KTT, et al. Parthenolide exerts inhibitory effects on angiogenesis through the downregulation of VEGF/VEGFRs in colorectal cancer. Int J Mol Med. 2014;33(5):1261–1267. doi:10.3892/ijmm.2014.1669
36. Blaser MJ, Chyou P, Nomura A. Age at establishment of Helicobacter pylori infection and gastric carcinoma, gastric ulcer, and duodenal ulcer risk. Cancer Res. 1995;55(3):562–565.
37. Scholl S, Pallud C, Beuvon F, et al. Anti-colony-stimulating factor-1 antibody staining in primary breast adenocarcinomas correlates with marked inflammatory cell infiltrates and prognosis. J Natl Cancer Inst. 1994;86(2):120–126. doi:10.1093/jnci/86.2.120
38. Gupta SC, Hevia D, Patchva S, Park B, Koh W, Aggarwal BB. Upsides and downsides of reactive oxygen species for cancer: the roles of reactive oxygen species in tumorigenesis, prevention, and therapy. Antioxid Redox Signal. 2012;16(11):1295–1322. doi:10.1089/ars.2011.4414
39. Rabinowich H, Cohen R, Bruderman I, Steiner Z, Klajman A. Functional analysis of mononuclear cells infiltrating into tumors: lysis of autologous human tumor cells by cultured infiltrating lymphocytes. Cancer Res. 1987;47(1):173–177.
40. Menges T, Engel J, Welters I, et al. Changes in blood lymphocyte populations after multiple trauma: association with posttraumatic complications. Crit Care Med. 1999;27(4):733–740. doi:10.1097/00003246-199904000-00026
41. Putzu C, Cortinovis DL, Colonese F, et al. Blood cell count indexes as predictors of outcomes in advanced non-small-cell lung cancer patients treated with Nivolumab. Cancer Immunol Immunother. 2018;67(9):1349–1353. doi:10.1007/s00262-018-2182-4
42. Huang Y, Liu A, Liang L, et al. Diagnostic value of blood parameters for community-acquired pneumonia. Int Immunopharmacol. 2018;64:10–15. doi:10.1016/j.intimp.2018.08.022
43. Lissoni P, Rovelli F, Monzon A, Privitera C, Messina G, Porro G. Evidence of abnormally low lymphocyte-to-monocyte ratio in covid-19-induced severe acute respiratory syndrome. J Immunol Allergy. 2020;1(2):1–6.
44. Nicolai L, Massberg S. Platelets as key players in inflammation and infection. Curr Opin Hematol. 2020;27(1):34–40. doi:10.1097/MOH.0000000000000551
45. Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi:10.1016/j.bbi.2020.07.037
46. Wang X, Li X, Shang Y, et al. Ratios of neutrophil-to-lymphocyte and platelet-to-lymphocyte predict all-cause mortality in inpatients with coronavirus disease 2019 (COVID-19): a Retrospective Cohort Study in a single medical centre. Epidemiol Infect. 2020;148.
47. Merekoulias G, Alexopoulos EC, Belezos T, Panagiotopoulou E, Jelastopulu E. Lymphocyte to monocyte ratio as a screening tool for influenza. PLoS Curr. 2010;2:RRN1154. doi:10.1371/currents.RRN1154
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.