Back to Journals » Infection and Drug Resistance » Volume 16
C-Reactive Protein-to-Albumin Ratio (CAR) and C-Reactive Protein-to-Lymphocyte Ratio (CLR) are Valuable Inflammatory Biomarker Combination for the Accurate Prediction of Periprosthetic Joint Infection
Authors Shi W, Jiang Y, Tian H, Wang Y, Zhang Y, Yu T, Li T
Received 24 November 2022
Accepted for publication 19 January 2023
Published 25 January 2023 Volume 2023:16 Pages 477—486
DOI https://doi.org/10.2147/IDR.S398958
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Weipeng Shi,1,2 Yaping Jiang,3 Hua Tian,4 Yingzhen Wang,1 Yingze Zhang,5 Tengbo Yu,1 Tao Li1
1Department of Orthopaedic Surgery, The Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 2Medical Department of Qingdao University, Qingdao, Shandong, People’s Republic of China; 3Department of Oral Implantology, The Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 4Department of Neurological Rehabilitation, Qingdao Special Servicemen Recuperation Center of PLA Navy, Qingdao, People’s Republic of China; 5Key Laboratory of Biomechanics of Hebei Province, Department of Trauma Emergency Center, The Third Hospital of Hebei Medical University, Orthopaedics Research Institution of Hebei Province, Shijiazhuang, People’s Republic of China
Correspondence: Tao Li; Tengbo Yu, Department of Orthopaedic Surgery, The Affiliated Hospital of Qingdao University, No. 59, Haier Road, Qingdao, Shandong Province, People’s Republic of China, Email [email protected]; [email protected]
Background: Periprosthetic joint infection (PJI) is a catastrophic complication after total joint arthroplasty (TJA). Timely and accurate diagnosis is important for the management of PJI. Currently, many biomarkers are available for the diagnosis of PJI, but which inflammatory biomarker combination has the best diagnostic value has not been reported.
Materials and Methods: We retrospectively analyzed 244 patients who underwent revision knee or hip arthroplasty in our institution. They were divided into two groups: 87 in the PJI group and 157 in the aseptic failure (AF) group. The preoperative C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), CRP-to-albumin ratio (CAR), CRP-to-lymphocyte ratio (CLR), neutrophil-to-albumin ratio (NAR) and platelet-to-albumin ratio (PAR) were determined and compared between the two groups. Receiver operating characteristic curve (ROC) and area under the curve (AUC) were used to assess the diagnostic value of all biomarkers, and the optimal cut-off value, positive predictive value (PPV) and negative predictive value (NPV) were further calculated by the Youden index.
Results: The NLR, PLR, CAR, CLR, NAR and PAR of the PJI group were significantly higher than those of the AF group (P< 0.001). According to the ROC and AUC results, the diagnostic value of CAR and CLR was considered excellent with AUCs of 0.931 and 0.935, respectively. The diagnostic value of NAR (0.739) and PAR (0.785) were fair, the diagnostic value of NLR (0.694) was poor, and PLR (0.535) had no diagnostic ability. Subgroup analysis showed no significant differences in combined inflammatory biomarkers between the two groups.
Conclusion: CAR and CLR are valuable combined inflammatory biomarkers for diagnosing PJI, while other markers were of limited value for the diagnosis of PJI.
Keywords: C-reactive protein-to-albumin ratio, C-reactive protein-to-lymphocyte ratio, biomarkers, periprosthetic joint infection
Introduction
Periprosthetic joint infection (PJI) is the most serious postoperative complication of total joint replacement (TJA) and one of the most challenging problems in joint surgery. Studies have found that the rate of PJI after hip replacement is about 0.5–1.2%,1,2 and the PJI following primary knee replacement is about 2%.3 The one-year mortality rates after total hip and total knee PJI are 4.22% and 4.33%, respectively, and the five-year mortality rates are 21.12% and 21.64%, respectively.13,14 The estimated total annual hospital costs associated with PJI in the US will be $1.85 billion by 2030.15 Therefore, PJI has become a serious public problem and the key to manage PJI is the early accurate diagnosis. It is well known that both PJI and aseptic failure (AF) patients may have the same symptoms such as joint pain and swelling at the early stage. However, the treatment regimens for PJI and AF are significantly different. Thus, early diagnosis is important for optimizing the treatment of PJI.
Diagnostic criteria developed by the Musculoskeletal Infection Society (MSIS) and the Infectious Diseases Society (IDSA) have helped surgeons improve the accuracy of PJI diagnosis.4,5 The new scoring system proposed in 2018 on this basis further enhanced the sensitivity and specificity of PJI diagnosis, and thus the new definition is widely accepted.6 In recent years, an increasing number of new methods or biomarkers have been shown to be beneficial in diagnosing PJI. For example, alpha-defensins are more stable and accurate than traditional inflammatory biomarkers (CRP and ESR) in PJI diagnosis.7 One study reported that synovial fluid alpha-defensins had lower sensitivity but higher specificity for the diagnosis of PJI compared with frozen sections.8 In addition, synovial calprotectin showed a good ability to diagnose PJI even in the presence of other local inflammatory diseases.9 The application of new technologies such as shotgun metagenomic sequencing (sNGS), electrical bioimpedance spectroscopy, and Ga-citrate PET also provides a more comprehensive and accurate diagnosis of PJI.10–12 However, these methods are difficult to popularize in primary hospitals because of high technical and economic requirements.
Serum biomarkers such as CRP, ESR, fibrinogen, and
In this single-center retrospective study, we aimed to evaluate the potential diagnostic value of each biomarker combination for PJI by comparing NLR, PLR, CAR, CLR, NAR and PAR with traditional inflammatory biomarkers (CRP and ESR).
Materials and Methods
Patient Selection
This single-center retrospective study was approved by the Institutional Review Board (IRB) of The Affiliated Hospital of Qingdao University (QYFY WZLL 27361) and complied with the ethical guidelines of the Declaration of Helsinki. From the electronic medical record system, we obtained the data of 303 patients who underwent knee or hip revision surgery in our hospital from June 2013 to July 2022. In order to improve the accuracy of this study, we excluded the cases that met the following exclusion criteria: (1) periprosthetic fractures; (2) prosthetic dislocations; (3) complicated with diseases that may affect biomarkers levels (malignancy, other joint trauma or infection, and hematological diseases) (4) complicated with autoimmune system diseases (rheumatoid arthritis, and ankylosing spondylitis); (5) recent use of anticoagulant drugs; (6) missing data. After careful review, a total of 244 patients were included in the final study, including 87 patients in the PJI group and 157 patients in the AF group. All PJI patients met the latest revised diagnostic criteria of PJI for MSIS in 2018.6
Data Extraction
Baseline data of all included patients including age, gender, height, weight, time and joint of infection were obtained from the medical record system. The fasting venous blood was drawn by the nurse on the day of admission or the next day and sent to the laboratory for analysis within 1 hour. We were responsible for recording CRP, ESR, neutrophils, lymphocytes, platelets, albumin levels and calculating NLR, PLR, CAR, CLR, NAR and PAR. In addition, synovial fluid or pus was collected at the time of surgery and sent to the laboratory for aerobic and anaerobic culture, while histopathological examination of periprosthetic tissue or bone was performed.
Statistical Analyses
All statistical analyses were performed using SPSS software version 26.0 (IBM Inc., Armonk, NY, USA) and figures were drawn using GraphPad Prism 8.0.2 (GraphPad Software Inc., San Diego, CA, USA). Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables as frequencies or percentages. The Mann–Whitney U-test was used to compare continuous variables between the two groups, and the chi-square test was adopted to analyze categorical variables. A P value <0.05 was considered statistically significant. Areas under the curves (AUCs), 95% confidence intervals (CI), sensitivity and specificity were calculated from receiver operating characteristic (ROC) curves of various combined inflammatory biomarkers. The optimal cut-off value of the biomarker was determined by the Youden index, and the negative predictive value (NPV) and positive predictive value (PPV) were further calculated according to the optimal cut-off value. The diagnostic value was divided into five grades based on the AUCs: excellent (0.900–1.000), good (0.800–0.899), fair (0.700–0.799), poor (0.600–0.699), and no diagnostic ability (0.500–0.599).
Results
The body mass index (BMI) of PJI patients was remarkably higher than that of the AF group (26.04±4.02 kg/m2 vs 24.79±3.47 kg/m2, P=0.005) and the number of infected knees was significantly higher than those of the AF group (P<0.001). Other basic data including age and gender did not show significant differences between the two groups. Details are presented in Table 1.
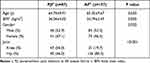 |
Table 1 Basic Characteristics of All Patents in the PJI and AF Groups |
Table 2 and Figure 1 show that patients in PJI group had significantly higher levels of NLR (3.36±2.93 vs 2.07±1.87), PLR (160.52±112.59 vs 135.64±82.63), CAR (1.20±1.54 vs 0.09±0.14), CLR (30.34±46.28 vs 2.25±5.17), NAR (0.14±0.11 vs 0.09±0.03) and PAR (8.21±3.04 vs 5.80±1.70) than AF group (P<0.001). ROC curve indicated that the diagnostic value of CAR (AUC=0.931, 95% [CI] 0.894, 0.969) and CLR (AUC=0.935, 95% [CI] 0.901, 0.967) was as “excellent” as CRP (AUC=0.941, 95% [CI] 0.909,0.973) and ESR (AUC=0.916,95% [CI] 0.881, 0.951). For CAR, the optimal cut-off value was 0.28 with a sensitivity of 80.2% and a specificity of 95.2%. At the optimal cut-off value (5.46), the sensitivity and specificity of CLR were 86.0% and 90.5%, respectively. As for NAR (AUC=0.739, 95% [CI] 0.672, 0.805, sensitivity: 65.1%, specificity: 74.1%) and PAR (AUC=0.785, 95% [CI] 0.725, 0.845, sensitivity: 72.1%, specificity: 76.0%), the diagnostic value was fair, with a cut-off value of 0.10 and 6.63, respectively. The diagnostic value of NLR was poor, with an AUC of 0.694 (95% [CI] 0.621, 0.767, sensitivity: 59.3%, specificity: 75.5%). The AUC of PLR was 0.535, which means that PLR has no diagnostic ability. According to the Youden index, the PPV of six biomarkers were 57.14%, 56.52%, 88.61%, 83.33%, 56.67% and 62.38%, and the NPV were 77.12%, 69.19%, 89.70%, 92.21%, 76.62% and 83.22%, respectively (Figure 2, Table 3).
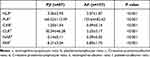 |
Table 2 Comparison of the Levels of All Inflammatory Biomarker Combination |
 |
Table 3 Diagnostic Value of CRP, ESR, NLR, PLR, CAR, CLR, NAR and PAR |
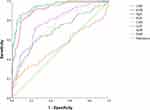 |
Figure 2 The ROC curves of CRP, ESR, NLR, PLR, CAR, CLR, NAR and PAR. |
Our subgroup analysis demonstrated that there was no significant difference in biomarker levels between the two groups, whether grouped by culture results, joint of infection, or time of infection, except that the patients with knee infection had lower PAR than the hip (P<0.001) (Table 4). In order to further improve the sensitivity and specificity of PJI diagnosis, we combined CAR, CLR and traditional inflammatory biomarkers (CRP and ESR) to conduct a combined test. Result of test showed significant improvement in sensitivity, specificity, PPV, and NPV in diagnosing PJI (Table 5). Notably, when ESR was connected in series with CAR and in parallel with CLR, the diagnostic specificity and sensitivity achieved the highest values, which suggests the diagnostic potential of ESR in the combined test.
 |
Table 4 Comparison of All Inflammatory Biomarker Combination in the Different PJI Subgroups |
 |
Table 5 Combinational Diagnostic Value of the CAR and CLR Combined with CRP and ESR for PJI |
Among the 87 PJI patients, 60 were culture-positive and 27 were culture-negative, with a positive rate of about 68.97% (60/87). The culture results showed that the most common pathogen was Staphylococcus epidermidis (19/60, 31.67%), followed by Staphylococcus aureus (11/60, 18.33%). Two patients (3.33%) were histopathologically found to be infected with two types of bacteria simultaneously: one with Staphylococcus epidermidis/Staphylococcus xylosus infection and the other with Staphylococcus epidermidis/Escherichia coli infection (Table 6).
 |
Table 6 Culture Results of Patients in the PJI Group |
Discussion
In the present study, we compared the value of multiple combined inflammatory biomarkers for the diagnosis of PJI for the first time and demonstrated that CAR and CLR have excellent diagnostic value. Compared with CRP and ESR, these two novel biomarkers have higher sensitivity or specificity, and the combination of CAR and CLR with CRP and ESR could further improve the sensitivity, specificity, NPV and PPV. These results suggest that these markers could be widely used in the future. In addition, the diagnostic value of NLR, NAR and PAR is limited and significantly lower than traditional inflammatory biomarkers. Surprisingly, PLR has no ability to diagnose PJI.
CRP is an acute-phase protein produced by the liver, which is increased in response to inflammation or infection. Albumin (ALB) is another protein produced by the liver, and serum albumin is often used as an indicator of malnutrition.21 Recent studies have shown that there is a close relationship between ALB and inflammation, and low ALB levels are associated with more severe inflammation.22,23 CRP level increases during infection while serum ALB level decreases when the immune system is activated.24 This opposite response in infection may account for the high diagnostic value of CAR. Therefore, as an emerging inflammatory biomarker, CAR has attracted extensive attention in various infectious diseases.25,26 Our previous studies confirmed that CAR, like traditional inflammatory biomarkers (CRP and ESR), had a high diagnostic value for PJI (AUC=0.941), with the highest specificity (94.9%) and the second highest sensitivity (83.8%) following CRP.27 In this study, we included more patients with PJI and AF to further validate the results of the previous study. It turns out that CAR does have high diagnostic value and performs the best among multiple combinations of inflammatory biomarkers. The AUC of CAR was 0.931, the sensitivity was 80.2%, and the specificity was 95.2%. When CAR combined with ESR and CRP, the sensitivity and specificity were further improved. Therefore, we considered that CAR is an excellent diagnostic indicator for PJI. Our results have also been confirmed by a recent study.28 In the study of Choe et al, CAR was highly accurate for PJI diagnosis, with an AUC of 0.97.28 Although the AUC of CAR was decreased in patients with low-grade PJI, CAR can be routinely used as a diagnostic biomarker for PJI. Another study conducted by Yiğit et al used CAR to predict PJI after TJA. They analyzed 12 risk factors including CRP, albumin, CAR and reported that CAR is more powerful than other risk factors in predicting PJI.29 Two-stage revision is the gold standard for the treatment of PJI, but there are still 4–33% failure cases.30,31 The timely determination of the risk factors for the failure of two-stage revision surgery is crucial to optimize clinical results and maximize patient satisfaction. Unfortunately, the only study at present shows that CAR is not suitable for predicting the prognosis of PJI two-stage revision.32 Considering that the data of all patients come from one year before the revision rather than during hospitalization, the CAR used in the calculation cannot accurately indicate the preoperative situation of patients. Therefore, the ability of CAR for predicting the failure after the second revision warrants further investigation.
Lymphocytes mainly mediate the specific immune response, which are activated when pathogens enter the human body. The same as albumin, the number of lymphocytes in sepsis patients also decreased significantly, which is related to the marginalization of lymphocytes, increase in apoptosis and redistribution of cells.33 Therefore, CLR, as a novel inflammatory biomarker, may have a similar function to CAR. For a long time, the studies on CLR mainly focused on the prognosis of various cancers and the disease severity of COVID-19.34,35 Taniai et al found that preoperative CLR can effectively predict the survival rate of colorectal liver metastases patients after hepatic resection.34 Another study confirmed that CLR is an important biomarker for differentiating patients with acute appendicitis and perforated appendicitis.36 However, no research has reported the relationship between CLR and PJI so far. In the present study, we found that the level of CLR was significantly elevated in the PJI group compared with that in the AF group. According to the AUC, the diagnostic value of CLR for PJI was considered excellent (AUC=0.935), which outperformed CAR and ESR (AUC: 0.931 and 0.916, respectively). By calculating the Youden-index, our results show that CLR has better sensitivity (86.0%), PPV (83.33%) and NPV (92.21%) than CRP and ESR. When the CLR was combined with either CRP or ESR, the sensitivity and specificity of the combined diagnosis reached more than 90%. We evaluated the accuracy of CLR in diagnosing PJI for the first time, and the results demonstrated that it can be a valuable referable tool for PJI diagnosis.
Neutrophils, as the most abundant white blood cells (50% to 70%) in the human body, are the main component in response to infection or tissue damage.37 When inflammation occurs, a large number of neutrophils are released into the blood, and the level of anti-apoptotic myeloid cell leukemia-1 (Mcl-1) increases. The apoptosis of neutrophils exposed to inflammatory mediators is delayed, leading to an increase in the number of peripheral blood neutrophils.38,39 This whole process plays an indispensable role in the emergence and prognosis of sepsis. In recent years, studies have shown that platelets not only have a physiological hemostatic effect but also play an important role in immune and inflammatory reactions.40 During the immune inflammatory reaction, the crosstalk between platelets and bacteria leads to platelet activation. Activated platelets interact with other cells through surface receptors, and release many functional proteins such as cytokines and chemokines through degranulation to maintain the balance of the immune system.41,42 To the best of our knowledge, this study is the first to explore the relationship between NAR, PAR and PJI. In our study, we found that the average levels of NAR and PAR increased significantly in PJI patients, but the diagnostic value of these two inflammatory biomarkers for PJI was considered fair (0.739 and 0.785, respectively), which were significantly lower than CRP and ESR. In addition, the sensitivity, specificity, NPV and PPV of NAR and PAR were also lower than those of CRP and ESR. These results indicate that the value of these two ratios in diagnosing PJI is limited. Notably, the level of PAR in knee PJI is significantly lower than that of hip PJI. Thus, the value of PAR in the diagnosis of different joint PJI deserves more investigation. At present, the diagnostic value of NLR in PJI remains controversial. The diagnostic value of NLR was considered good in two studies (AUC: 0.80 and 0.80, respectively).43,44 However, most studies have shown that AUCs of NLR range from 0.656 to 0.740, which indicates that NLR is of limited diagnostic value and cannot be used as a reliable biomarker to assist the diagnosis of PJI.18,45–50 In the present study, NLR could only obtain poor result (AUC: 0.694) when diagnosing PJI, with the sensitivity of 59.3% and the specificity of 75.5%. The conclusions obtained in our studies were supported by a latest meta-analysis.51
There are several limitations of our study. The inherent bias of the present study is unavoidable because of its single-center and retrospective design. Therefore, the conclusion needs to be verified by a prospective study with larger sample size. In addition, cirrhosis and malnutrition may lead to hypoalbuminemia in non-PJI patients, but our study did not exclude these patients, which may reduce the accuracy of CAR, NAR and PAR.
Conclusion
Our study revealed that compared with CRP and ESR, CAR and CLR have the equivalent excellent diagnostic value for PJI. Their diagnostic value can be further improved when combined with CRP and ESR, which is helpful for the screening of PJI patients. We believe that these two combinations of inflammatory biomarkers should be widely used in clinical practice.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
This single-center retrospective study was approved by the Institutional Review Board (IRB) of The Affiliated Hospital of Qingdao University (QYFY WZLL 27361). All data are anonymous and collected based on the ethics approval, so the requirement of informed consent was waived.
Consent for Publication
All authors agree to the publication of the article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Qingdao Traditional Chinese Medicine Science and Technology Project; Grant number: 2021-zyym28; Science and technology Development Project of Shandong Geriatric Society; Grant number: LKJGG2021W082; Youth Research Foundation of Affiliated Hospital of Qingdao University; Grant number: QDFYQN202001012.
Disclosure
The authors declare no competing interests.
References
1. Whitehouse MR, Parry MC, Konan S, et al. Deep infection after Hip arthroplasty: staying current with change. Bone Joint J. 2016;98-B:27–30. doi:10.1302/0301-620X.98B1.36294
2. Hviid GP, Becic PA, Claus V, et al. Increased mortality after prosthetic joint infection in primary THA. Clin Orthop Relat Res. 2017;475:2623–2631. doi:10.1007/s11999-017-5289-6
3. Kong KC, Irene Z, Saiprassad R, et al. Periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res. 2017;475:2194–2201. doi:10.1007/s11999-017-5396-4
4. Javad P, Benjamin Z, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469:2992–2994. doi:10.1007/s11999-011-2102-9
5. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1–e25. doi:10.1093/cid/cis803
6. Javad P, Tan TL, Karan G, et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018;33:1309–1314.e2. doi:10.1016/j.arth.2018.02.078
7. Giovanni R, Luca C, Wassim A, et al. Qualitative alpha-defensin versus the main available tests for the diagnosis of periprosthetic joint infection: best predictor test? J Bone Jt Infect. 2018;3:156–164. doi:10.7150/jbji.26401
8. Sigmund IK, Johannes H, Susanna L, et al. A comparative study of intraoperative frozen section and alpha defensin lateral flow test in the diagnosis of periprosthetic joint infection. Acta Orthop. 2019;90:105–110. doi:10.1080/17453674.2019.1567153
9. Igor L, Peter P, Maximilian S, et al. Synovial calprotectin is a reliable biomarker for periprosthetic joint infections in acute-phase inflammation - a prospective cohort study. Int Orthop. 2022;46:1473–1479. doi:10.1007/s00264-022-05421-1
10. Lim HH, Laure F, Thoendel MJ, et al. Targeted versus shotgun metagenomic sequencing-based detection of microorganisms in sonicate fluid for periprosthetic joint infection diagnosis. Clin Infect Dis. 2022. doi:10.1093/cid/ciac646
11. Marco B, Carlo P, Pasquale A, et al. Detecting and monitoring periprosthetic joint infection by using electrical bioimpedance spectroscopy: a preliminary case study. Diagnostics. 2022;12. doi:10.3390/diagnostics12071680
12. Tingting X, Yalan Z, Xiao Y, et al. Application of Ga-citrate PET/CT for differentiating periprosthetic joint infection from aseptic loosening after joint replacement surgery. Bone Joint Res. 2022;11:398–408. doi:10.1302/2046-3758.116.BJR-2021-0464.R1
13. Natsuhara KM, Shelton TJ, Meehan JP, et al. Mortality during total hip periprosthetic joint infection. J Arthroplasty. 2019;34:S337–S342. doi:10.1016/j.arth.2018.12.024
14. Lum ZC, Natsuhara KM, Shelton TJ, et al. Mortality during total knee periprosthetic joint infection. J Arthroplasty. 2018;33:3783–3788. doi:10.1016/j.arth.2018.08.021
15. Ajay P, Kolin DA, Farley KX, et al. Projected economic burden of periprosthetic joint infection of the hip and knee in the United States. J Arthroplasty. 2021;36:1484–1489.e3. doi:10.1016/j.arth.2020.12.005
16. Bao-Zhan Y, Jun F, Wei C, et al. Neutrophil to lymphocyte ratio as a predictor for diagnosis of early Periprosthetic joint infection. BMC Musculoskelet Disord. 2020;21:706. doi:10.1186/s12891-020-03704-5
17. Guanglei Z, Jie C, Jin W, et al. Predictive values of the postoperative neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and lymphocyte-to-monocyte ratio for the diagnosis of early periprosthetic joint infections: a preliminary study. J Orthop Surg Res. 2020;15:571. doi:10.1186/s13018-020-02107-5
18. Katharina SI, Johannes H, Kevin S, et al. Inferior performance of established and novel serum inflammatory markers in diagnosing periprosthetic joint infections. Int Orthop. 2021;45:837–846. doi:10.1007/s00264-020-04889-z
19. Hanyang L, Zhaohui B, Qiong W, et al. Inflammatory indexes for assessing the severity and disease progression of ulcerative colitis: a single-center retrospective study. Front Public Health. 2022;10:851295. doi:10.3389/fpubh.2022.851295
20. Awatef BJ, Noura S, Meriam BO, et al. Evaluation of individual and combined NLR, LMR and CLR ratio for prognosis disease severity and outcomes in patients with COVID-19. Int Immunopharmacol. 2022;109:108781. doi:10.1016/j.intimp.2022.108781
21. Don BR, George K. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17:432–437. doi:10.1111/j.0894-0959.2004.17603.x
22. Andreas E, Tristan S, Alexander K, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med. 2020;133:713–722.e7. doi:10.1016/j.amjmed.2019.10.031
23. Soeters PB, Wolfe RR, Alan S. Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr. 2019;43:181–193. doi:10.1002/jpen.1451
24. Toshio T, Masashi N, Tadamitsu K. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014;6:a016295. doi:10.1101/cshperspect.a016295
25. Yaohua Y, Weiwei W, Yanyan D, et al. C-reactive protein-to-albumin ratio predicts sepsis and prognosis in patients with severe burn injury. Mediators Inflamm. 2021;2021:6621101. doi:10.1155/2021/6621101
26. Ping K, Wen K, Yi L, et al. C-reactive protein-to-albumin ratio as an early biomarker to identify sepsis in neonates with pneumonia. Mediators Inflamm. 2022;2022:4711018. doi:10.1155/2022/4711018
27. Weipeng S, Yingzhen W, Xuan Z, et al. CRP/albumin has a promising prospect as a new biomarker for the diagnosis of periprosthetic joint infection. Infect Drug Resist. 2021;14:5145–5151. doi:10.2147/IDR.S342652
28. Hyonmin C, Naomi K, Koki A, et al. Evaluation of serum albumin and globulin in combination with C-reactive protein improves serum diagnostic accuracy for low-grade periprosthetic joint infection. J Arthroplasty. 2022. doi:10.1016/j.arth.2022.09.011
29. Şeyhmus Y, Sait AM, Akif ŞM, et al. Periprosthetic infection risks and predictive value of C-reactive protein / albumin ratio for total joint arthroplasty. Acta Biomed. 2021;92:e2021324. doi:10.23750/abm.v92i4.10995
30. Youssef SF, Leonard B, Sarim A, et al. Preoperative prediction of failure following two-stage revision for knee prosthetic joint infections. J Arthroplasty. 2014;29:115–121. doi:10.1016/j.arth.2013.04.016
31. Petis SM, Perry KI, Mabry TM, et al. Two-stage exchange protocol for periprosthetic joint infection following total knee arthroplasty in 245 knees without prior treatment for infection. J Bone Joint Surg Am. 2019;101:239–249. doi:10.2106/JBJS.18.00356
32. Hong CS, Ryan SP, Gabor JA, et al. Predicting success of two-stage exchange for prosthetic joint infection using c-reactive protein/albumin ratio. Adv Orthop. 2019;2019:6521941. doi:10.1155/2019/6521941
33. Felmet KA, Hall MW, Clark RSB, et al. Prolonged lymphopenia, lymphoid depletion, and hypoprolactinemia in children with nosocomial sepsis and multiple organ failure. J Immunol. 2005;174:3765–3772. doi:10.4049/jimmunol.174.6.3765
34. Tomohiko T, Koichiro H, Ryoga H, et al. The prognostic significance of C-reactive protein-to-lymphocyte ratio in colorectal liver metastases. J Surg Res. 2021;258:414–421. doi:10.1016/j.jss.2020.08.059
35. Miao Y, Xiaoping C, Yancheng X. A retrospective study of the C-reactive protein to lymphocyte ratio and disease severity in 108 patients with early covid-19 pneumonia from January to march 2020 in Wuhan. China Med Sci Monit. 2020;26:e926393.
36. Serhat K, Okan I. The role of C-reactive protein to lymphocyte ratio in the differentiation of acute and perforated appendicitis. Ulus Travma Acil Cerrahi Derg. 2020;26:760–764. doi:10.14744/tjtes.2020.47973
37. Peter H, Dinsdale RJ, Wearn CM, et al. Neutrophil dysfunction, immature granulocytes, and cell-free DNA are early biomarkers of sepsis in burn-injured patients: a prospective observational cohort study. Ann Surg. 2017;265:1241–1249. doi:10.1097/SLA.0000000000001807
38. Tie-Shan T, Ai-Ling J, Xin-Ying J, et al. Neutrophils and Immunity: from Bactericidal Action to Being Conquered. J Immunol Res. 2017;2017:9671604. doi:10.1155/2017/9671604
39. Hui-Bing Z, Juan C, Qiao-Fen L, et al. Diagnostic values of red cell distribution width, platelet distribution width and neutrophil-lymphocyte count ratio for sepsis. Exp Ther Med. 2016;12:2215–2219. doi:10.3892/etm.2016.3583
40. Leo N, Florian G, Steffen M. Platelets in host defense: experimental and clinical insights. Trends Immunol. 2019;40:922–938. doi:10.1016/j.it.2019.08.004
41. Xiaoyan L, Hongyun L, Xianming L, et al. Strains of Group B streptococci from septic patients induce platelet activation via Toll-like Receptor 2. Clin Exp Pharmacol Physiol. 2017;44:335–343. doi:10.1111/1440-1681.12707
42. Thomas MR, Storey RF. The role of platelets in inflammation. Thromb Haemost. 2015;114:449–458. doi:10.1160/TH14-12-1067
43. Christian K, Venkatsaiakhil T, Smith EJ, et al. Complete blood platelet and lymphocyte ratios increase diagnostic accuracy of periprosthetic joint infection following total Hip arthroplasty. Arch Orthop Trauma Surg. 2022;31:1–9.
44. Venkatsaiakhil T, Christian K, Liang X, et al. Diagnostic utility of platelet count/lymphocyte count ratio and platelet count/mean platelet volume ratio in periprosthetic joint infection following total knee arthroplasty. J Arthroplasty. 2021;36:291–297. doi:10.1016/j.arth.2020.07.038
45. Hao W, Liping P, Zhichao M, et al. C-reactive protein (CRP)/albumin-to-globulin ratio (AGR) is a valuable test for diagnosing periprosthetic joint infection: a single-center retrospective study. J Orthop Traumatol. 2022;23:36. doi:10.1186/s10195-022-00657-4
46. Yongyu Y, Weishen C, Minghui G, et al. Limited value of serum neutrophil-to-lymphocyte ratio in the diagnosis of chronic periprosthetic joint infection. J Orthop Traumatol. 2021;22:37. doi:10.1186/s10195-021-00599-3
47. Jing-Bo J, Jin-Cheng H, Xiao C, et al. Albumin to Globulin ratio, Neutrophil to Lymphocyte ratio, and Globulin levels do not outperform ESR or CRP when diagnosing periprosthetic joint infection. BMC Musculoskelet Disord. 2022;23:404. doi:10.1186/s12891-022-05357-y
48. Hong X, Jinwei X, Shaoyun Z, et al. Potential blood biomarkers for diagnosing periprosthetic joint infection: a single-center, retrospective study. Antibiotics. 2022;11. doi:10.3390/antibiotics11040505
49. Hong X, Jinwei X, Xufeng W, et al. Combination of C-reactive protein and fibrinogen is useful for diagnosing periprosthetic joint infection in patients with inflammatory diseases. Chin Med J. 2022;135:1986–1992. doi:10.1097/CM9.0000000000002215
50. Zulipikaer M, Chi X, Jun F, et al. The potential value of monocyte to lymphocyte ratio, platelet to mean platelet volume ratio in the diagnosis of periprosthetic joint infections. Orthop Surg. 2022;14:306–314. doi:10.1111/os.12992
51. Enrico F, Tiziana A, Alessio B, et al. Diagnostic performance of neutrophil to lymphocyte ratio, monocyte to lymphocyte ratio, platelet to lymphocyte ratio, and platelet to mean platelet volume ratio in periprosthetic hip and knee infections: a systematic review and meta-analysis. Diagnostics. 2022;12:2033.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

