Back to Journals » International Journal of General Medicine » Volume 14
Butorphanol versus Propofol in Patients Undergoing Noninvasive Ventilation: A Prospective Observational Study
Received 14 December 2020
Accepted for publication 23 February 2021
Published 22 March 2021 Volume 2021:14 Pages 983—992
DOI https://doi.org/10.2147/IJGM.S297356
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xiaohong Wang,1 Jianbiao Meng2
1Intensive Care Unit, The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang Province, 310003, People’s Republic of China; 2Intensive Care Unit, Tongde Hospital of Zhejiang Province, Hangzhou, Zhejiang Province, 310012, People’s Republic of China
Correspondence: Jianbiao Meng
Intensive Care Unit, Tongde Hospital of Zhejiang Province, #234 Gucui Road, Hangzhou, Zhejiang Province, 310012, People’s Republic of China
Email [email protected]
Background: The present study aimed to explore sedation management in agitated patients who suffered from acute respiratory failure (ARF) and were treated with noninvasive ventilation (NIV).
Patients and Methods: We divided 118 patients undergoing NIV treatment with butorphanol or propofol into two groups: group B (n = 57, butorphanol was initiated at the rate of 0.12 μg/kg/min as a continuous intravenous infusion and then titrated by 0.06 μg/kg/min every half an hour, group P (n = 61, propofol was initiated at the rate of 5 μg/kg/min as a continuous intravenous infusion and then titrated by 1.5 μg/kg/min every half an hour). Score of Sedation Agitation Scale (SAS) in the two groups was maintained between 3 and 4. Medications including sedative, analgesic, and antipsychotic, NIV intolerance score, SAS score, visual analog scale (VAS), medication use and adverse events were recorded repeatedly.
Results: Patients receiving butorphanol required significantly less total amount of fentanyl than patients receiving propofol during NIV to maintain the target VAS [0 (0– 0) μg vs 150 (50– 200) μg, P< 0.005]. Hemodynamic stability during NIV showed it was better kept in patients treated with butorphanol.
Conclusion: Butorphanol not only decreased the requirements of fentanyl but also enhanced hemodynamic stability in agitated patients suffering from ARF receiving NIV.
Trial Registration: Registered at http://www.chictr.org.cn/ (ChiCTR1800015534).
Keywords: butorphanol, acute respiratory failure, noninvasive ventilation
Background
In recent decades, with the development of techniques of respiratory support and monitoring, noninvasive ventilation (NIV) was widely implemented in intensive care units (ICU) and obviates the need for invasive ventilation and mortality among patients undergoing acute exacerbations of chronic obstructive pulmonary disease1,2 or severe pulmonary edema induced by injuries of lung and heart,3 because these diseases are usually the main reasons for acute respiratory failure (ARF). In addition, NIV was also practiced in patients suffering from refractory hypoxemia and/or the compromise of immunity, and during the period of postextubation.
However, lots of uncomfortable experience of NIV, for example pain, anxiety, dysphoria, delirium, intolerance of NIV and asynchrony with the ventilator often exist and result in failure of NIV in critically ill patients treated with NIV.4 For the success of NIV, these uncomfortable aspects must be treated with sedative-hypnotic medications. Therefore, sedation management is a very critical consideration during the care of patients undergoing NIV. A desirable sedation should facilitate mechanical ventilation and sleep, allay anxiety, release pain and delirium, and alleviate physiologic responses to stress including tachycardia, shortness of breath and hypertension without depressing respiration or hypoxic drive and cough reflex.
The regimens of sedation and analgesic that clinicians prefer to use may improve patients’ comfort and tolerance and be quite varied during NIV. It is reported that benzodiazepines, propofol and opiates are the most often selected for NIV in patients with ARF,5,6 but clinicians are very cautious to administer these medications because these medications may compromise the respiratory and cough reflex.7 Furthermore, propofol and benzodiazepines are related to greater delirium.8 A synthetic opioid agonist-antagonist analgesic, butorphanol, can agonize the κ and σ opiate receptors principally, but antagonize µ opiate receptor or partially.9,10 Because of lower affinity between butorphanol and σ opiate receptors, little dysphoria could be induced by butorphanol.9 In addition to analgesia, butorphanol also exerts the effect of sedation through agonising κ opiate receptors without tolerance.10 There is not floaty euphoria and drug dependence during period of use butorphanol because it antagonize µ opiate receptor or partially.11 Butorphanol has been used widely for treatment of pain with moderate-to-severe degree, opioid-induced cough, as a supplement to balancing general anesthesia and reducing post-operative shivering.12,13 However, no studies have been reported on the use of butorphanol during NIV.
To date, it is still not known what the optimal strategy of sedation and analgesic for patients who suffer from ARF and are treated with NIV is. Hence, we explore the treatment with sedatives, analgesics, and antipsychotics, and describe tolerance of NIV, sedation depth, pain evaluation, and the incidence of delirium in the first 24-hours after NIV treatment in our study.
Patients and Methods
Ethics Statement
The research was approved by the Ethics Committee of Tongde Hospital of Zhejiang Province (approval no. 2018–018) and implemented according to the guidelines of the Declaration of Helsinki.14 All participants were recruited by Tongde Hospital of Zhejiang Province and they all (or their guardians) signed informed consents prior to enrollment.
Patients
The data of patients with ARF were collected prospectively, and they had been consecutively treated with NIV in the ICU of Tongde Hospital of Zhejiang Province, China, between January 2018 and June 2019.
The inclusion criteria of NIV were that 1) pulse oxygen saturation (SpO2) was less than 90% while inspiration of oxygen was more than 10 L/min through reservoir mask, 2) acute respiratory acidosis showed levels of partial pressure of carbon dioxide in artery (PaCO2) were more than 45 mmHg, or 3) respiratory distress, including both more than 24 breaths per minute of respiratory rate (RR) and enhanced use of accessory respiratory muscle.
The main exclusion criteria were severe dementia, less than or equal to 12 points of a Glasgow Coma Scale (GCS) score, and treatment with butorphanol or propofol during the past month. Endotracheal intubation in an urgent situation, a definite refusal decision of intubation, and an order not to participate.
Noninvasive Ventilation
NIV was conducted with a Philips ventilator (BiPAP Vision, Respironics Inc, USA). The ventilator operates in the following modes: 1) Continuous Positive Airway Pressure (CPAP), 2) Spontaneous (S) and 3) Spontaneous/Timed (S/T) through a nose mask or nose-mouth mask. The inclusion criteria mentioned above determined the setting of a ventilator and choice of ventilation modes including the CPAP and S/T. If a patient satisfied criterion 2) and/or 3), the S/T mode was chosen, yet we chose the CPAP mode if one satisfied criterion 1) and suffered from mere hypoxemia. The initial setting of the S/T mode included an inspiratory positive airway pressure (IPAP) of 14 cm H2O, an expiratory positive airway pressure (EPAP) of 6 cm H2O, a RR of 10 breaths per minute, and a pressure support of 8 cm H2O. In the CPAP mode, the ventilator delivered continuous pressure support at 6 cm H2O at the beginning. In order to maintain the SpO2 of more than 90%, the fraction of inspiratory oxygen (FiO2) was modulated based on the SpO2. The physicians proficiently adjusted the NIV settings during NIV treatment based on each patient’s condition followed by the beginning of NIV treatment.
We discontinued the treatment of NIV in the patients who satisfied all criteria as follows: 1) patients did not manifest signs of respiratory distress such as a RR of more than 24 breaths per minute and enhanced use of accessory respiratory muscle, 2) SpO2 was above 90% with the flow of inhaled oxygen of less than 10 L/min through the oxygen storage mask, and 3) the levels of PaCO2 were less than 45 mmHg or acute respiratory acidosis did not manifest in patients.
But invasive mechanical ventilation was performed after endotracheal intubation if patients met one of the criteria as follows: decrease in hemodynamic stability, a deterioration of consciousness status, or symptoms of respiratory failure, which was persisting or deteriorating and met no less than two of the criteria as follows: a RR of more than 45 breaths per minute, becoming no better in symptoms of severe overload on respiratory muscle, increased amount of secretions in trachea, acidosis manifesting a pH value of less than 7.25, and an SpO2of less than 90% persisting for no less than 5 minutes.
Sedation, Analgesia and Anti-Delirium
One hundred and eighteen patients were divided into two cohorts, those who received butorphanol (group B, 57 patients) or received propofol (group P, 61 patients). In group B, butorphanol (Jiangsu Xinchen Pharmaceutical Co. Ltd) treatment was begun at a rate of 0.12 µg/kg/min as a continuous intravenous infusion without a beginning bolus, then titrated by 0.06 µg/kg/min every half an hour (up until the highest rate of 0.24 µg/kg/min) to keep a Sedation-Agitation Scale (SAS) score of between 3 and 4.11 In group P, propofol (AstraZeneca S.p.A.) treatment was started at a rate of 5 µg/kg/min as a continuous intravenous infusion without a beginning bolus, then titrated by 1.5 µg/kg/min every half an hour (up until the highest rate of 10.0 µg/kg/min) to keep a SAS score of between 3 and 4.15 After ten minutes when any butorphanol tartrate or propofol dose was raised, the injection of midazolam (Jiangsu Nhwa Pharmaceutical Limited by Share Ltd) with a dose from 0.01 to 0.02 mg/kg would be infused as necessitated when the patient manifested a sign of agitation (SAS score of no less than 5), in addition, the injection of fentanyl (Yichang human well pharmaceutical limited liability company) with a dose from 0.5 to 1 µg/kg would be infused as necessitated when a patient exhibited pain (Visual Analog Scale, VAS score of no less than 5 of 10 cm) once the last dose of midazolam or fentanyl had been administered for three hours.16,17 The intramuscular injection of haloperidol (Hunan Dongting pharmaceutical Limited by Share Ltd) of 2.5 to 5 mg would be administered as necessitated if a patient developed delirium.18
Study Outcomes
In this study, the variable of main outcome was the tolerance of NIV, which was ranked by a NIV intolerance score.19 The NIV intolerance score included four points and was modified based on NIV tolerance scores with four-points and five-points which have been published previously.20,21 The level of sedation was evaluated using SAS score, with a SAS score of no less than 5 indicating agitation but a SAS score of no more than 2 indicating deep sedation.22 Pain was estimated using a VAS, with a length of 0 cm representing no pain but a length of 10 cm representing severe pain.23 When the patient could not finish the VAS, it would be recorded on the form by the bedside nurse based on patient’s self-reported pain score. The Intensive Care Delirium Screening Checklist was performed to screen patients with delirium.24 The bedside nurse, well educated regarding each assessment, conducted all assessments of sedation, pain and delirium and recorded in medical records repeatedly, every hour.
Vital signs, such as heart rate (HR), invasive blood pressure (IBP), and RR, were monitored every minute and recorded every 10 minutes during the first sixty minutes and every half an hour from one hour after the initiation to the finish of the study's medication infusion. Acute Physiology and Chronic Health Evaluation (APACHE)-IIand sequential organ failure assessment (SOFA) were performed at baseline. In addition, we repeated the analysis of blood gases and laboratory tests at NIV initiation and 1, 6, 12, and 24 hours after the drugs were administered. Clinical and laboratory data of all patients were recorded.
During our research, all patients were monitored for evidence of clinical or laboratory adverse events. Adverse events referred to any adverse events that occurred in patients such as symptoms, signs, laboratory findings or test results.
Statistical Analysis
The IBM SPSS Statistics 19 (IBM Corporation, Armonk, New York, USA) was used to conduct statistical analyses. Continuous variables were presented as the means ± standard deviation (SD). Comparisons of repeated measurements within groups was conducted using repeated measurement variance analysis. Comparisons between groups were performed with the independent-sample t test. Categorical variables were presented as the frequency (n) and percentage (%) and analyzed using Chi-squared tests or Fisher exact tests as appropriate. In all analyses, a P value of < 0.05 was deemed to be statistically significant.
Results
Baseline Characteristics
From January 2018 to June 2019, there were 201 patients undergoing treatment with NIV, but according to the inclusion criteria and exclusion criteria mentioned above, 83 patients were excluded and 118 were included in our study (Figure 1). Characteristics of the patients at baseline were similar in the two groups (Table 1). The mean age, proportion of men and body-mass index (BMI) were similar between the two groups (P = 0.211, 0.501 and 0.521 respectively). The APACHE-II, SOFA scores, duration of ICU stay, the proportion of reasons for ARF and the source of pain showed no significant difference between the two groups (P = 0.301, 0.512, 0.127, 0.469 and 0.916 respectively).
 |
Table 1 Demographic and Baseline Clinical Parameters Between the Two Groups |
 |
Figure 1 Patient enrolment flow diagram. |
Changes in NIV Intolerance Score, SAS Score and VAS Between the 2 Groups
In both groups, NIV intolerance score, SAS score and VAS were significantly decreased after the infusion of butorphanol or propofol (all P < 0.05). Between the groups, there was no significant difference in NIV intolerance score, SAS score and VAS at baseline, 1 hour, 6 hour, 12 hour and 24 hour during continuous intravenous infusion of butorphanol or propofol (all P > 0.05) (Figure 2).
 |
Figure 2 Comparison of NIV intolerance score (A), Sedation-Agitation Scale (SAS) score (B) and visual analog scale (VAS) (C) between the two groups. *P < 0.05 versus baseline. |
Changes in Respiratory and Hemodynamic Parameters Between the 2 Groups
RR reduced and pH level raised gradually during continuous intravenous infusion of butorphanol and propofol in group B and group P (P < 0.05). FiO2 and PaCO2declinedsignificantly in the two groups (P <0.05). As to the levels of partial pressure of oxygen (PaO2), the comparisons within group and between groups were similar (P > 0.05). PaO2/FiO2 increased in both group comparisons (P< 0.05), but had no significant difference between group comparisons (P > 0.05). While HR and mean arterial pressure (MAP) at baseline were similar between the two groups (P > 0.05), HR levels of patients were significantly lower in both groups during continuous intravenous infusion of butorphanol and propofol compared with baseline (P < 0.05), but the difference between-group comparisons was not significant (P > 0.05). Patients had lower MAP levels at 1 hour during continuous intravenous infusion of propofol in group P compared with group B administered with butorphanol (P = 0.002). In group P, MAP levels were lower at 1 hour, 6 hour and 12 hour checks during continuous intravenous infusion of propofol when compared with baseline measurements (P < 0.05). However, the difference in MAP at 1 hour, 6 hour, 12 hour and 24 hour in group B had no statistical significance (P > 0.05) (Table 2).
 |
Table 2 Comparison of Respiratory and Hemodynamic Parameters Between the Two Groups |
Administration of Midazolam, Fentanyl and Haloperidol as Needed
The difference in the need of infusion of midazolam was not significant between group B and group P (44 vs 48, patients administered ≥ 1 dose, P = 0.845; 1.95±0.20 vs 1.98±0.19, doses/24hr, P = 0.896; 1.67±0.17 vs 1.77±0.17 total amount, mg, P = 0.667). And the difference in the need of haloperidol infusion as needed was similar between group B and group P (3 vs 5, patients administered ≥1 dose, P = 0.526; 0 (0–0) vs 0 (0–0), doses/24hr, P = 0.512; 0(0–0) vs 0 (0–0) total amount, mg, P = 0.520). In group B, however, number of patients administered fentanyl, doses and total amount of fentanyl as needed in 24 hours were less for group P (4 vs 49, patients administered ≥1 dose, P < 0.001; 0 (0–0) vs 150 (50–200), doses/24hr, P < 0.001; 0 (0–0) vs 3 (1–4) total amount, mg, P < 0.001) (Table 3).
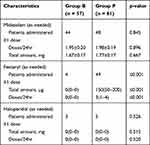 |
Table 3 Comparison of Medication Use During Period of the First 24h After Initiation of NIV Between the Two Groups |
Adverse Events
In this study, 15.8% (9 of 57) of patients in group B and 42.6% (26 of 61) of patients in group P suffered from one or more adverse events and, concerning the severity of these adverse events, most of them were mild or moderate (P = 0.001). The frequency of hypotension and hypovolemia has significant differences between group B and group P [2 (22.2%) vs 16 (61.6%), hypotension, P = 0.042; 1 (11.1%) vs 13 (50.0%), hypovolemia, P = 0.040]. But there were no significant differences in other adverse events between group B and group P [4 (44.4%) vs 6 (23.1%), vomiting, P = 0.211; 3 (33.3%) vs 9 (34.6%), tachycardia, P = 0.944; 2 (22.2%) vs 2 (7.7%), bradycardia, P = 0.238; 0 (0%) vs 1 (3.8%), shivering, P = 0.551]. Patients who were administered haloperidol in group B and group P did not manifest depression, extrapyramidal syndromes, rigidity and QT prolongation. No one developed withdrawal symptoms when butorphanol was discontinued in group B.
Discussion
This research compared the effects of butorphanol with propofol for treating agitated patients undergoing NIV. The main findings in our study are as follows. First, continuous intravenous infusion of butorphanol resulted in the same effect of sedation as propofol after NIV initiation. Second, compared with propofol, both sedation and analgesia were induced by butorphanol. Third, continuous intravenous infusion of butorphanol led to a stabler state of hemodynamics and less adverse events.
During NIV, patients’ intolerance, agitation or refusal could be considered frequent contributors to patient-ventilator asynchrony, which could also result in discontinuation of NIV and cause an increased rate in the unplanned requirement for endotracheal intubation. Research conducted by Carlucci et al indicated the withdrawal percentage of NIV for the refusal of patients was more than 20%.21 On average, about 100 patients with ARF suffered from NIV every year in the ICU of our hospital, NIV failure happened among some of them because of anxiety, agitation and delirium associated with intolerance of the mask and even claustrophobia. The patient`s ability to cooperate and synchronize to the ventilator during NIV determined the success of NIV.5 Hence, in order to improve the success of NIV, it is important for clinicians to assess the efficiency of NIV, and improve the comfort level and patient-ventilator harmonization in patients undergoing NIV.
Appropriate depth of sedation is necessary to eliminate anxiety and fear, increase compliance and tolerance of NIV, prevent patient-ventilator asynchrony and decrease work and oxygen consumption of respiratory muscles without respiratory depression. It is reported that benzodiazepines, propofol and opiates are the most often administered sedative agents in ICU.8 A short-acting medication, Propofol could lead to a lower level of consciousness and eliminate memory of events.25 The usage of propofol includes the inducing and maintenance for general anesthesia and procedural sedation in patients undergoing mechanical ventilation. A synthetic agonist-antagonist opioid analgesic, butorphanol exerts the effects of analgesia and sedation through agonising kappa opiate receptors without dependence.9,11 We compared butorphanol and propofol in the investigation.
It is recognized that excess sedation will result in lots of complications including delirium, hemodynamic instability and enhance the incidence of intubation and mortality in patients suffering from ARF. Therefore, excess sedation was avoided in our study and all patients in the study fulfilled the criteria including the NIV intolerance score of no more than 2, the SAS score of no more than 5 and the VAS score of no more than 5, experiencing adequate sedation with analgesia, it was interesting that we found patients in group B were administered fewer doses and amount of fentanyl than group P [0 (0–0) µg vs 150 (50–200) µg, P < 0.005], it was obvious that the analgesia of butorphanol was better than propofol. In addition, there was no significant difference in the need of infusion midazolam and haloperidol between group B and group P (all P > 0.05), so we inferred that butorphanol could cause the same effect of sedation as propofol in patients suffering from ARF with treatment of NIV. As was mentioned above, the sedative effect of butorphanol is related to agonising kappa opiate receptors.26 The same sedative effect of butorphanol in patients who underwent dental operations and laparoscopic surgery for ectopic pregnancy were reported.27,28
Compared with propofol, butorphanol did not exacerbate hemodynamic stability in patients with NIV. Patients in group P showed less MAP than group B at 1 hour after sedation, but there were no significant differences in MAP at 6 hour, 12 hour and 24 hour times between the two groups when patients in group P were administered fluid therapy during sedation. This indicated that patients in group P suffered from hypovolemia and even hypotension. Therefore, although a previous study showed that hypotension or hypertension was caused by butorphanol,29 we did not find this phenomenon in the study. It is concluded that butorphanol is better than propofol in maintaining hemodynamic stability in ARF patients undergoing NIV. Between-group comparisons, however, there were not significant differences in RR, PaCO2, and PaO2/FiO2, during continuous intravenous infusion of butorphanol and propofol (P > 0.05). Therefore, the results showed that both butorphanol and propofol could reduce oxygen consumption and improve oxygenation in ARF patients undergoing NIV. Previous studies found that sedative and opioid analgesic agents could release pain, anxiety and delirium, and improve intolerance of NIV and difficulty synchronizing with the ventilator,6,8 which could contribute to less oxygen consumption and improved oxygenation in ARF patients undergoing NIV.
Although sedative and opioid analgesic agents shave effects of sedation and play a necessary role during the wider treatment of agitation, pain and delirium,30,31 The adverse events of sedatives and opioid analgesic agents are common during the clinical practice, such as vomiting, hypotension, tachycardia, bradycardia and so on.32 In our study, the percentage of patients who suffered from one or more adverse events in group B was lower than in group P [15.8% (9 of 57) vs 42.6% (26 of 61)]. Concerning the severity of these adverse events, most of them were mild or moderate (P = 0.001). The frequency of hypotension and hypovolemia has significant differences between group B and group P (P = 0.042 and 0.040). Compared with benzodiazepine in fusions, the use of continuous propofol infusion was related to decreased mortality, and length of mechanical ventilation,33 however, the disadvantages of propofol were common during infusions.34,35 Some adverse events such as vomiting, shivering, tachycardia and bradycardia were observed in our study and might be related to NIV and reasons for ARF,36 and there were no serious adverse events which were regarded to be associated to the study medication in our study.
Our study, however, has several limitations. First, the sample size of this study is small, so it might not reflect the results of the general population completely. Second, because this is a prospective non-randomised comparative study, selection bias is unavoidable in this study. Third, the investigation was performed in a single-center, which was proficient in the administration of sedative and analgesia drugs and NIV treatment in patients undergoing ARF. Therefore, the indications for sedation and/or analgesia should be considered according to the proficiency in every center. In order to further understand the relationship between adverse events and sedative and analgesia drugs, a larger prospective randomised controlled study is needed.
Conclusions
In this prospective non-randomised comparative study, when comparing infusion of butorphanol to propofol infusion for sedation in patients with ARF undergoing noninvasive ventilation during the first 24 hours, both agents were found to cause the sedative effect and improve synchronization with the ventilator. Patients infused with butorphanol were administered markedly fewer analgesics to keep adequate sedation, analgesia and synchronization with the ventilator and experienced stabler hemodynamic stability.
Data Sharing Statement
We declare that all relevant raw data and materials described in the manuscript will be freely available through the corresponding author to any scientist, researcher and reader wishing to use them for non-commercial purposes, without breaching participant confidentiality. This study maintained patient data confidentiality in accordance with the ethical standers of the Helsinki Declaration.
Compliance with Ethical Standards
The study is conducted on already available data. Ethical approval was approved by the Ethics Committee of Tongde Hospital of Zhejiang Province (Approval No. 2018-018).
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Keenan SP, Sinuff T, Cook DJ, Hill NS. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive-pressure ventilation? A systematic review of the literature. Ann Intern Med. 2003;138(11):861–870. doi:10.7326/0003-4819-138-11-200306030-00007
2. Lightowler JV, Wedzicha JA, Elliott MW, Ram FSF. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: cochrane systematic review and meta-analysis. BMJ. 2003;326(7382):185. doi:10.1136/bmj.326.7382.185
3. Mariani J, Macchia A, Belziti C, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema: a meta-analysis of randomized controlled trials. J Card Fail. 2011;17(10):850–859. doi:10.1016/j.cardfail.2011.05.010
4. Nava S, Ceriana P. Patient-ventilator interaction during noninvasive positive pressure ventilation. Respir Care Clin N Am. 2005;11(2):281–293. doi:10.1016/j.rcc.2005.02.003
5. Rocco M, Conti G, Alessandri E, et al. Rescue treatment for noninvasive ventilation failure due to interface intolerance with remifentanil analgosedation: a pilot study. Intensive Care Med. 2010;36(12):2060–2065. doi:10.1007/s00134-010-2026-y
6. Hilbert G, Clouzeau B, Bui HN, Vargas F. Sedation during non-invasive ventilation. Minerva Anestesiol. 2012;78(7):842–846. doi:10.1016/j.annfar.2012.04.024
7. Devlin JW, Mallow-Corbett S, Riker RR. Adverse drug events associated with the use of analgesics, sedatives, and antipsychotics in the intensive care unit. Crit Care Med. 2010;38(6 Suppl):S231–S243. doi:10.1097/CCM.0b013e3181de125a
8. Devlin JW, Roberts RJ. Pharmacology of commonly used analgesics and sedatives in the ICU: benzodiazepines, propofol, and opioids. Anesthesiol Clin. 2011;29(4):567–585. doi:10.1016/j.anclin.2011.09.001
9. Heel RC, Brogden RN, Speight TM, Avery GS. Butorphanol: a review of its pharmacological properties and therapeutic efficacy. Drugs. 1978;16(6):473–505. doi:10.2165/00003495-197816060-00001
10. Ji J, Lin W, Vrudhula A, et al. Molecular Interaction Between Butorphanol and κ-Opioid Receptor. Anesth Analg. 2020;131(3):935–942. doi:10.1213/ane.0000000000005017
11. Vandam LD, Vandam LD. Drug therapy: butorphanol. N Engl J Med. 1980;302(7):381–384. doi:10.1056/NEJM198002143020705
12. Zhang J, Miao S, Tu Q, et al. Effect of butorphanol on opioid-induced cough: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2018;12:3263–3268. doi:10.2147/DDDT.S180533
13. Dobkin AB, Eamkaow S, Zak S, Caruso FK. Butorphanol: a double-blind evaluation in postoperative patients with moderate or severe pain. Canad Anaesthetists Soc j. 1974;21(6):600–610. doi:10.1007/bf03006021
14. Shephard DA. The 1975 Declaration of Helsinki and consent. Can Med Assoc J. 1976;115(12):1191–1192. doi:10.1021/cen-v029n032.p3161
15. Lundström S, Twycross R, Mihalyo M, Wilcock A. Propofol. J Pain Symptom Manage. 2010;40(3):466–470. doi:10.1016/j.jpainsymman.2010.07.001
16. Nordt SP, Clark RF. Midazolam: a review of therapeutic uses and toxicity. J Emerg Med. 1997;15(3):357–365. doi:10.1016/s0736-4679(97)00022-x
17. Stanley TH. Fentanyl. J Pain Symptom Manage. 2005;29(5 Suppl):S67–S71. doi:10.1016/j.jpainsymman.2005.01.009
18. Latronico N. Haloperidol and delirium in the ICU: the finger pointing to the moon. Intensive Care Med. 2018;44(8):1346–1348. doi:10.1007/s00134-018-5276-8
19. Devlin JW, Al-Qadheeb NS, Chi A, et al. Efficacy and safety of early dexmedetomidine during noninvasive ventilation for patients with acute respiratory failure: a randomized, double-blind, placebo-controlled pilot study. Chest. 2014;145(6):1204–1212. doi:10.1378/chest.13-1448
20. Nava S, Ambrosino N, Bruschi C, Confalonieri M, Rampulla C. Physiological effects of flow and pressure triggering during non-invasive mechanical ventilation in patients with chronic obstructive pulmonary disease. Thorax. 1997;52(3):249–254. doi:10.1136/thx.52.3.249
21. Carlucci A, Pisani L, Ceriana P, Malovini A, Nava S. Patient-ventilator asynchronies: may the respiratory mechanics play a role? Critical Care. 2013;17(2):R54. doi:10.1186/cc12580
22. Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med. 1999;27(7):1325–1329. doi:10.1097/00003246-199907000-00022
23. Ho K, Spence J, Murphy MF. Review of pain-measurement tools. Ann Emerg Med. 1996;27(4):427–432. doi:10.1016/s0196-0644(96)70223-8
24. Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27(5):859–864. doi:10.1007/s001340100909
25. Miller KA, Andolfatto G, Miner JR, Burton JH, Krauss BS. Clinical practice guideline for emergency department procedural sedation with propofol: 2018 update. Ann Emerg Med. 2019;73(5):470–480. doi:10.1016/j.annemergmed.2018.12.012
26. Lin L, Liu S, Chen Z, Lin S. Effect of ketamine combined with butorphanol on emergence agitation of postoperative patients with gastric cancer. Therapeutics Clin Risk Manag. 2016;12(5):713–717. doi:10.2147/tcrm.s103060
27. Jann MW, Fidone G, Gorday M, Rostedt RR. Butorphanol as a dental premedication in the mentally retarded. Oral Surg Oral Med Oral Pathol. 1987;63(4):403–407. doi:10.1016/0030-4220(87)90248-9
28. Chang WY, Li HY. Anesthetic efficacy of propofol combined butorphanol in laparoscopic surgery for ectopic pregnancy: a protocol of systematic review and meta-analysis. Medicine. 2020;99(20):e20289. doi:10.1097/MD.0000000000020289
29. Boulton DW, Duncan GF, Vachharajani NN. Validation and application of a high-performance liquid chromatography/tandem mass spectrometry assay for sumatriptan in human plasma. Biomed Chromatography. 2003;17(1):48–52. doi:10.1002/bmc.211
30. Devlin JW, Roberts RJ. Pharmacology of commonly used analgesics and sedatives in the ICU: benzodiazepines, propofol, and opioids. Crit Care Clin. 2009;25(3):431–449. doi:10.1016/j.ccc.2009.03.003
31. Pohlman AS, Simpson KP, Hall JB. Continuous intravenous infusions of lorazepam versus midazolam for sedation during mechanical ventilatory support: a prospective, randomized study. Crit Care Med. 1994;22(8):1241–1247. doi:10.1097/00003246-199408000-00007
32. Fierro MA, Bartz RR. Management of sedation and paralysis. Clin Chest Med. 2016;37(4):723–739. doi:10.1016/j.ccm.2016.07.012
33. Lonardo NW, Mone MC, Nirula R, et al. Propofol is associated with favorable outcomes compared with benzodiazepines in ventilated intensive care unit patients. Am J Respir Crit Care Med. 2014;189(11):1383–1394. doi:10.1164/rccm.201312-2291OC
34. Bray RJ. Propofol-infusion syndrome in children. Lancet. 1999;353(9169):2074–2075. doi:10.1016/s0140-6736(05)77896-x
35. Devaud JC, Berger MM, Pannatier A, et al. Hypertriglyceridemia: a potential side effect of propofol sedation in critical illness. Intensive Care Med. 2012;38(12):1990–1998. doi:10.1007/s00134-012-2688-8
36. Arnal J-M, Texereau J, Garnero A. Practical insight to monitor home NIV in COPD patients. Copd J Chronic Obstruct Pulmonary Dis. 2017;14(4):401–410. doi:10.1080/15412555.2017.1298583
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
