Back to Journals » Local and Regional Anesthesia » Volume 15
Bupivacaine for Root Canal Treatment – Practitioner Behaviors and Patient Perspectives: Survey Studies
Authors Erdogan O, Casey SM, Ruparel NB, Sigurdsson A
Received 20 September 2021
Accepted for publication 28 October 2021
Published 3 February 2022 Volume 2022:15 Pages 11—21
DOI https://doi.org/10.2147/LRA.S339238
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Stefan Wirz
Ozge Erdogan,1,2 Sharon M Casey,1,2 Nikita B Ruparel,3 Asgeir Sigurdsson1
1Department of Endodontics, New York University College of Dentistry, New York, NY, USA; 2Department of Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, Boston, MA, USA; 3Department of Endodontics, University of Texas Health Science Center at San Antonio, San Antonio, TX, USA
Correspondence: Ozge Erdogan
Department of Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, 188 Longwood Ave, Boston, MA, 02115, USA
, Email [email protected]
Introduction and Objectives: Local anesthesia is essential in dentistry in providing intraoperative analgesia and anesthesia. However, knowledge related to its use for management of post-operative pain is limited. Perioperative pain management is especially important for root canal treatment (ie, endodontic therapy), performed by endodontists. In this study, we sought to better understand endodontists’ attitudes regarding the use of long-lasting anesthetic, namely 0.5% bupivacaine HCl with 1:200,000 epinephrine, for the management of post-endodontic pain. Additionally, we aimed to understand the perspectives of dental patients about receiving longer lasting anesthesia for endodontic therapy and to determine factors that affect their anesthetic preferences within the orofacial region.
Methods: An email invitation to participate in an anonymous online survey was sent to members of the American Association of Endodontists. Also, 82 patients attending an in-person visit to an endodontic clinic were recruited to the study.
Results: Data from 474 endodontic practitioners and 82 patients included in analysis. Among practitioners, the majority reported to either never (33.31%) or rarely (34.84%) using bupivacaine. Most chose “I don’t think I need it” (47%) and “patient discomfort because of longer duration of soft tissue anesthesia” (30.81%) as reasons for not preferring the use of bupivacaine. Of the practitioners who reported at least rare use, most chose bupivacaine for post-operative pain management (78.02%). Conversely, 52% of patients reported that they were likely/most likely to request long-lasting anesthetics for post-operative pain control.
Conclusion: Bupivacaine is rarely used as a post-operative pain management strategy for endodontic therapy. Specifically, bupivacaine is not preferred not because of adverse events, toxicity, or slow onset concerns, but rather, because of longer duration of soft tissue anesthesia. However, our data suggest that patients may be willing to receive long-lasting anesthesia. Further patient-centered research should investigate the use of long-lasting anesthetic agents for management of post-endodontic pain.
Keywords: bupivacaine, long lasting local anesthesia, post-operative pain, root canal treatment, endodontics
Introduction
Toothache is one of the most prevalent orofacial pain types reported in the United States.1 Dental pain often occurs when bacteria reach the pulp tissue subsequent to hard tissue damage such as caries or fracture.2 When infection and inflammation of the tooth become severe, endodontic therapy (ie, root canal treatment) or tooth extraction are the most common treatment modalities. While endodontic treatment is highly successful in relieving pain,3 patients have been reported to suffer from moderate to severe pain after endodontic treatment for up to seven days, with pain being the most severe during the first two days.4 Therefore, post-operative pain management is a crucial component of endodontic practice. Various pharmacological modalities for the management of post-operative pain such as non-steroid anti-inflammatory drugs (NSAIDs), acetaminophen, and corticosteroids have been investigated and are often implemented in routine clinical practice.5,6 While these approaches are generally effective, contraindications for administration of these drugs limit their use.7 Importantly, multimodal analgesia is recommended to provide more potent pain relief, and to lower dosage of drug intake.8
Bupivacaine is a long-lasting anesthetic (LLA) which is used to manage post-operative pain either alone or when included in a multimodal analgesia regimen.9 Administration of bupivacaine can provide post-operative pain relief for 12 hours or more and works by blocking sensory afferent stimulation and inhibiting peripheral and central sensitization.9–12 The use of a long-lasting anesthetic, such as bupivacaine, as a post-surgical pain management strategy in medicine is widely accepted.13 Despite local anesthesia (LA) being an essential component of any dental treatment to provide intra-operative anesthesia and analgesia, knowledge regarding the use of local anesthesia by endodontic practitioners, specifically the use of long-lasting anesthetics, for post-endodontic pain management is limited.9,14,15
The purpose of this study was to investigate endodontic practitioners’ knowledge and attitudes regarding the use of long-lasting anesthetic, namely 0.5% bupivacaine HCl with 1:200,000 epinephrine, for the management of post-endodontic pain. Additionally, we sought to understand the perspective of dental patients about receiving longer lasting anesthesia and to determine factors that affect their anesthetic preferences.
Materials and Methods
Endodontic Practitioner Survey
This study was approved by the Institutional Review Board of New York University (IRB-FY2019-2718) and was conducted in accordance with the Declaration of Helsinki. An email invitation to participate in an anonymous online survey was distributed to 4190 American Association of Endodontists members. The survey was designed to determine the type of local anesthetic preferred by endodontic practitioners, the factors influencing their decision regarding the use of anesthetics, specifically the use of long-lasting anesthetics, as a post-endodontic pain management strategy. Potential explanatory variables included age of respondents, years of endodontic practice, and type of current endodontic practice setting. The survey was created using Qualtrics software (Provo, UT), evaluated by an epidemiologist, and pilot tested by a group of endodontic residents and faculty. At the beginning of the survey, participants first completed and signed the consent form. The consent was obtained anonymously, no identified data was asked during the consent procedure. The subject could either consent or reject to participate by clicking the appropriate box. If the subject did not consent, she/he was directed to the end of the survey. Potential participants were assured that no identifiers, including IP addresses, would be collected. The survey was sent to prospective participants in April 2019 and a reminder email was sent 2 weeks later.
Dental Patient Survey
This study was approved by the Institutional Review Board of New York University (IRB-FY2019-2499) was conducted in accordance with the Declaration of Helsinki. Patients attending the New York University College of Dentistry post-graduate endodontic clinic between January 2019 - May 2019 were invited to participate in this study. Participants were at least 18 years of age, and could independently complete the English language survey. Participants were introduced to the study by research personnel, informed that participation was voluntary and completing the survey would take 5–10 minutes. Participants who were interested in joining the study were then consented. The study survey data were collected and managed using REDCap (Research Electronic Data Capture). The survey questions asked about demographics, previous root canal treatment history, pain history and participants’ perspective on receiving long lasting anesthesia. A brief script explaining the purpose and use of long lasting anesthesia was provided within the questionnaire. An optional Pain Catastrophizing Scale (PCS) questionnaire was available to participants.
Statistical Analysis
Data were imported into Stata version 16 (StataCorp, College Station, TX) from Qualtrics and REDCap. Descriptive analyses of variables was performed to identify frequency, mean and standard deviation, and tabulation and ranking were performed when appropriate. Chi-square tests and univariate analyses were used for categorical and continuous variables. A p-value less than 0.05 was considered statistically significant. Figures were created using GraphPad Prism version 8.0 for MacBook (GraphPad Software, San Diego, California USA).
Results
Endodontic Practitioner Sample
Of the 4190 AAE members who were invited to participate in the study, 474 endodontic practitioners completed the online survey, representing a response rate of 11%. The mean number of years of practice was 16 years (SD ± 10.01, range 1–45 years). Distribution of age, years of practice, current practice setting, and geographic location of current practice is presented (Table 1).
 |
Table 1 Demographic Information of Practitioner Survey Respondents |
Local Anesthesia Selection Criteria
Local anesthetic agents chosen by participants for endodontic practice, reasons for their choice, local anesthesia available in current endodontic practice settings, and preferred local anesthesia for endodontic treatments are described in Table 2. Participants indicated the main criterion when choosing appropriate local anesthesia was efficacy (96%), while 51% reported safety. The most preferred local anesthesia by practitioners was Lidocaine HCI 2% and Epinephrine 1:100,000 (81%), and bupivacaine HCI 0.5% and Epinephrine 1:200,000 was preferred by 23% of participants.
 |
Table 2 Practitioner Survey – Local Anesthetic Preferences |
Post-Operative Endodontic Pain Management with Local Anesthesia
The majority of endodontic practitioners reported either never using bupivacaine (never as an infiltration injection (34%) and never as an inferior alveolar nerve block (IANB) (32%)) or rarely using bupivacaine (rarely as an infiltration injection (37%) and rarely as an IANB (33%)) (Table 2). Of those who at least reported rare use of bupivacaine, most reported to using bupivacaine for post-operative pain management (78%) (Figure 1). For the question “why don’t you prefer bupivacaine?”, when we excluded responses solely selecting “I use bupivacaine” for this question, the reminder most often chose “I don’t think I need it” (47%) and “patient discomfort because of longer duration of soft tissue anesthesia” (31%) as reasons for not using bupivacaine (Figure 1, Table 2).
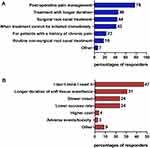 |
Figure 1 (A) What purposes do practitioners prefer Bupivacaine HCI 0.5% and Epinephrine 1:200,000 in their practice? (select all that apply, Percentages were calculated by excluding 100 subjects who said they never use bupivacaine either with infiltration or IANB in question 9 Table 2) (N=373)). (B) Why do not practitioners prefer Bupivacaine HCI 0.5% and Epinephrine 1:200,000? (select all that apply) (Percentages were calculated by excluding 90 subjects solely selected “I use bupivacaine” in question 10 Table 2) (N= 383)). |
Post-Operative Pain Management with Additional -Post Treatment- LA Injection
The use of local anesthetic agents as a post-operative pain management strategy with additional post-treatment local anesthetic injection was relatively low (rarely=59%). Of those who reported at least rare use of providing additional injection of local anesthetic for post-operative pain management, 61% chose bupivacaine (Table 2). Age, years of practice or practice setting were not associated with participants’ attitudes towards using bupivacaine or use of LA as a post-operative pain management strategy (Table 3).
 |
Table 3 Practitioner Survey – Subcategory Analysis for Bupivacaine Use |
Patient Survey
Study Sample
Eighty-two participants were included in this study. Patient demographics, history of previous root canal treatment, and type of appointment (treatment, dental emergency due to pain or swelling etc.) are listed in Table 4. Presence of pain in the tooth being treated, pain intensity using a Numerical Rating Scale (0–10), pain duration and frequency, pain medication use, and pain catastrophizing scale results are also reported (Table 4).
 |
Table 4 Patient Survey Characteristics |
Patients’ Attitudes Towards Longer Lasting Anesthesia
When asked how likely they were to request administration of LLA from their endodontist for their treatment, 52% reported they were likely/most likely to request long-lasting anesthesia. When asked how likely they were to request an extra injection of long-acting anesthesia at the end of their endodontic treatment for pain management, 41% of respondents reported “likely/most likely” (Figure 2). We performed univariate analysis and chi-square tests to determine associations between previous root canal therapy experience, presence and intensity of pain, pain medication use, and PCS scores, and patients’ request of LLA, these factors were not significantly associated with requesting long lasting anesthesia following treatment. When PCS was dichotomized as <30 and >30, there was a trend that patients with >30 PCS scores were tend to request LLA more frequently than patients who reported <30 PCS scores (p=0.07).
Discussion
A significant proportion of the endodontic patient population presents with pain, and obtaining profound anesthesia and analgesia before beginning root canal therapy is crucial. Moreover, patients have been reported to experience moderate to severe pain for up to seven days after endodontic treatment.4 However, the use of LA, more specifically LLA, for post-endodontic pain management is not well understood. The administration of LLA is widely accepted in medicine, including bupivacaine, as well as extended-release bupivacaine formulations which can last up to 4 days.16 A published guideline for the management of post-operative pain after general surgery strongly recommends the use of site-specific peripheral regional anesthesia with high quality level evidence for acute post-operative pain control.13 However, while LA is an essential component of any dental treatment to provide intra-operative anesthesia and analgesia, our study suggests that within endodontic practice bupivacaine is not widely used, where most practitioners reported never or rarely using bupivacaine. Our results also indicate that practitioners’ attitudes towards use of LA as a post-operative pain management strategy did not differ according to age, years of practice or practice setting. Although the use of bupivacaine was infrequent, 78% of those who reported at least rare use stated the primary purpose of use as “post-operative pain management”. These results reveal that LA selection is mostly based on intra-operative pain management needs and is rarely chosen for post-operative pain control following endodontic treatment.
Interestingly, only a small proportion of endodontic practitioners reported “slower onset time”, “lower success rate” and “adverse events/toxicity” as reasons for not using bupivacaine.17,18 The majority of respondents stated that “they don’t think they need it” (47%), despite the evidence that patients may suffer from moderate to severe pain following endodontic treatment4 and NSAIDs and/or acetaminophen are often prescribed.5 A study by Pak et al found that 81% of patients reported moderate pre-operative pain intensity when they attend a dental clinic.4 Moreover, pre-operative pain is a predictor of post-operative pain,19 highlighting the necessity of adequate post-operative pain management required for patients who present with ongoing pre-operative pain. Therefore, LLA is a pain management option for patients at risk of post-operative pain,9 that can be delivered before endodontic treatment initiation or as a supplemental injection at the end of the treatment.
Another significant finding of the study is that almost a third of practitioner respondents chose “patient discomfort because of longer duration of soft tissue anesthesia” as the reason for not using bupivacaine. It is possible that longer duration of soft tissue anesthesia around the orofacial region can pose discomfort and soft tissue injury, and some patients may dislike longer term soft tissue numbness as it may alter important orofacial function such as eating and speaking.9,10 Interestingly, our data suggest that approximately half of the patient respondents would very likely/likely consider requesting LLA as an anesthetic choice, knowing that LLA causes soft tissue numbness for an extended duration. Although our findings did not capture that patients with higher intensity or longer duration of pre-operative pain preferred LLA more often, there was a trend where patients with higher pain catastrophizing scale scores preferred LLA more often. Comprehensive, clinical studies are needed to investigate patients’ experience with LLA when applied within the orofacial region and which patient population might benefit more from LLA.
It is noteworthy to mention that in this study 23% of the practitioners who reported at least rare use of bupivacaine, stated the purpose of use as “for patients with a history of chronic/persistent pain”. Studies report the incidence of chronic pain after endodontic therapy as high as 3–12%.20–22 Given that pre-operative and post-operative pain are predictive of pain chronification after endodontic treatment,20,22,23 the use of bupivacaine can be considered as a preventive measure for persistent pain after treatment, especially for patients who are at increased risk.24 What is more, an additional post-treatment injection of LA could be indicated as a preventive measure for persistent pain after endodontic treatment for those patients who are at risk.13,24 An additional injection with bupivacaine can help blocking sensory afferent stimulation hence limiting peripheral and central sensitization and prevent chronification of post-operative pain.9–12 In this survey, the majority of practitioners (59%) reported rare use of an additional injection after endodontic therapy for management of post-operative pain. Of those who reported at least rare use, 61% preferred using bupivacaine. On the other hand, when we asked patients, about 40% said that they would most likely/likely want to receive an additional injection at the end of their treatment for managing post-treatment pain. These findings suggest that patients may be informed about bupivacaine as a post treatment pain management option and can be given the option of additional bupivacaine administration.
The primary limitation in this study is the low response rate (11%). However, as we sampled a professional homogenous group with similar distribution among age groups and years of endodontic practice, we believe that non-response bias likely does not significantly impact the results of this study.25 One barrier our group faced regarding distribution of the survey was the email address list limited use clause (maximum of two email communications), meaning we could not send additional survey invitations or reminders to prospective participants. An important point to highlight is the possibility that those who did not respond to the survey, may not have bupivacaine available to them in their endodontic practice setting. Further investigation to capture the perspectives of these individuals may be warranted. Finally, the survey was distributed only to AAE members, whose practice is focused on endodontics and the preferences and attitudes of general dental practitioners may be different, as seen from previous studies.14,26,27
Conclusion
Findings from this study suggest that bupivacaine is rarely used by endodontic practitioners as a post-operative pain management strategy following root canal treatment. However, endodontic patients might prefer receiving long lasting anesthesia for endodontic pain control. Based on the perspectives captured in this study, further patient-centered clinical studies should be conducted to investigate the use of LLA during or after procedures within the orofacial region.
Data Sharing Statement
The original data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
We would like to thank Dr. Ahn Chiyoon for his contribution to collect patient surveys. We also would like to thank Dr. Ryan R. Ruff, Dr. Lorel E. Burns and Dr. Austin A. Ramsey for their contributions during survey question preparations.
Funding
The authors received no financial support for the research.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124(10):115–121. doi:10.14219/jada.archive.1993.0200
2. Bergenholtz G. Pathogenic mechanisms in pulpal disease. J Endod. 1990;16(2):98–101. doi:10.1016/S0099-2399(06)81571-2
3. Law AS, Nixdorf DR, Rabinowitz I, et al. Root canal therapy reduces multiple dimensions of pain: a national dental practice-based research network study. J Endod. 2014;40(11):1738–1745. doi:10.1016/j.joen.2014.07.011
4. Pak JG, White SN. Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod. 2011;37(4):429–438. doi:10.1016/j.joen.2010.12.016
5. Aminoshariae A, Kulild JC, Donaldson M, Hersh EV. Evidence-based recommendations for analgesic efficacy to treat pain of endodontic origin: a systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147(10):826–839. doi:10.1016/j.adaj.2016.05.010
6. Shamszadeh S, Shirvani A, Eghbal MJ, Asgary S. Efficacy of corticosteroids on postoperative endodontic pain: a systematic review and meta-analysis. J Endod. 2018;44(7):1057–1065. doi:10.1016/j.joen.2018.03.010
7. Hargreaves KM, Berman LH. Cohen’s Pathways of the Pulp.
8. Derry CJ, Derry S, Moore RA. Single dose oral ibuprofen plus paracetamol (Acetaminophen) for acute postoperative pain. Cochrane Database Syst Rev. 2013;2013(6):CD010210. doi:10.1002/14651858.CD010210.pub2
9. Parirokh M, Yosefi MH, Nakhaee N, Manochehrifar H, Abbott PV, Reza Forghani F. Effect of bupivacaine on postoperative pain for inferior alveolar nerve block anesthesia after single-visit root canal treatment in teeth with irreversible pulpitis. J Endod. 2012;38(8):1035–1039. doi:10.1016/j.joen.2012.04.012
10. Moradi S, Naghavi N. Comparison of bupivacaine and lidocaine use for postoperative pain control in endodontics. Iran Endod J. 2010;5(1):31–35.
11. Su N, Wang H, Zhang S, Liao S, Yang S, Huang Y. Efficacy and safety of bupivacaine versus lidocaine in dental treatments: a meta-analysis of randomised controlled trials. Int Dent J. 2014;64(1):34–45. doi:10.1111/idj.12060
12. Gordon SM, Dionne RA, Brahim J, Jabir F, Dubner R. Blockade of peripheral neuronal barrage reduces postoperative pain. Pain. 1997;70(2–3):209–215. doi:10.1016/S0304-3959(96)03315-5
13. Chou R, Gordon DB, de Leon-casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17(2):131–157. doi:10.1016/j.jpain.2015.12.008
14. Gaffen AS, Haas DA. Survey of local anesthetic use by Ontario dentists. J Can Dent Assoc. 2009;75(9):649.
15. Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. Occurrence of paresthesia after dental local anesthetic administration in the United States. J Am Dent Assoc. 2010;141(7):836–844. doi:10.14219/jada.archive.2010.0281
16. Balocco AL, Van Zundert PGE, Gan SS, Gan TJ, Hadzic A. Extended release bupivacaine formulations for postoperative analgesia: an update. Curr Opin Anaesthesiol. 2018;31(5):636–642. doi:10.1097/ACO.0000000000000648
17. Gordon SM, Mischenko AV, Dionne RA. Long-acting local anesthetics and perioperative pain management. Dent Clin North Am. 2010;54(4):611–620. doi:10.1016/j.cden.2010.06.002
18. Fernandez C, Reader A, Beck M, Nusstein J. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31(7):499–503. doi:10.1097/01.don.0000167395.61075.38
19. Arias A, de la Macorra JC, Hidalgo JJ, Azabal M, Moradi S, Naghavi N. Predictive models of pain following root canal treatment: a prospective clinical study. Int Endod J. 2013;46(8):784–793. doi:10.1111/iej.12059
20. Polycarpou N, Ng YL, Canavan D, Moles DR, Gulabivala K. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int Endod J. 2005;38(3):169–178. doi:10.1111/j.1365-2591.2004.00923.x
21. Nixdorf DR, Moana-Filho EJ, Law AS, McGuire LA, Hodges JS, John MT. Frequency of nonodontogenic pain after endodontic therapy: a systematic review and meta-analysis. J Endod. 2010;36(9):1494–1498. doi:10.1016/j.joen.2010.06.020
22. Philpott R, Gulabivala K, Leeson R, Ng YL. Prevalence, predictive factors and clinical course of persistent pain associated with teeth displaying periapical healing following nonsurgical root canal treatment: a prospective study. Int Endod J. 2019;52(4):407–415. doi:10.1111/iej.13029
23. Nixdorf DR, Law AS, Lindquist K, et al. Frequency, impact, and predictors of persistent pain following root canal treatment: a National Dental PBRN Study. Pain. 2016;157(1):159.
24. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9(5):723–744. doi:10.1586/ern.09.20
25. Hovland EJ, Romberg E, Moreland EF. Nonresponse bias to mail survey questionnaires within a professional population. J Dent Educ. 1980;44(5):270–274. doi:10.1002/j.0022-0337.1980.44.5.tb01365.x
26. Yapp KE, Hopcraft MS, Parashos P. Dentists’ perceptions of a new local anaesthetic drug–articaine. Aust Dent J. 2012;57(1):
27. Corbett IP, Ramacciato JC, Groppo FC, Meechan JG. A survey of local anaesthetic use among general dental practitioners in the UK attending postgraduate courses on pain control. Br Dent J. 2005;199(12):
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

