Back to Journals » Clinical Ophthalmology » Volume 9
Brinzolamide 1%/timolol versus dorzolamide 2%/timolol in the treatment of open-angle glaucoma or ocular hypertension: prospective randomized patient-preference study
Authors Altafini R, Scherzer M, Hubatsch DA, Frezzotti P
Received 20 May 2015
Accepted for publication 27 August 2015
Published 1 December 2015 Volume 2015:9 Pages 2263—2270
DOI https://doi.org/10.2147/OPTH.S88891
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Romeo Altafini,1 Maria-Luise Scherzer,2 Douglas A Hubatsch,3 Paolo Frezzotti4
1Glaucoma Segment Unit, “San Bortolo” Hospital, Vicenza, Italy; 2Private Practice, Regenstauf, Germany; 3Alcon Laboratories, Inc., Fort Worth, TX, USA; 4Ophthalmic Unit, University of Siena, Siena, Italy
Purpose: The objective of this study was to assess preference for fixed-combination brinzolamide 1%/timolol 0.5% (BTFC) versus fixed-combination dorzolamide 2%/timolol 0.5% (DTFC) in patients with open-angle glaucoma or ocular hypertension.
Methods: In this prospective, single-masked crossover study, patients were randomized 1:1 to BTFC-DTFC or DTFC-BTFC treatment sequences. Patients self-administered each medication for 7 days, with a 48-hour washout period between treatments, and rated ocular discomfort after each treatment period. Medication preferences based on ocular comfort (primary endpoint) and anticipated adherence were assessed. Safety outcomes included adverse events and intraocular pressure. Between-group differences in treatment preference and ocular discomfort scores were analyzed using chi-square and Wilcoxon–Mann–Whitney tests, respectively. Adherence, intraocular pressure, and adverse events were summarized descriptively.
Results: In total, 112 patients were enrolled (mean ± SD age, 66±11 years), and 109 patients completed the study. Numerically, more patients in the intent-to-treat dataset preferred BTFC versus DTFC (59.3% versus 40.7%); however, this result was not statistically significant (treatment difference, 18.6%; P=0.0670). Mean ocular discomfort scores (range, 0–9) were statistically significantly lower with BTFC versus DTFC (2.6 versus 3.7; P=0.0002, Wilcoxon–Mann–Whitney test). More patients who preferred BTFC over DTFC were confident that they would adhere to their preferred medication. Treatment-related adverse events included blurred vision with BTFC and eye irritation or eye pain with DTFC.
Conclusion: BTFC and DTFC were preferred by approximately 60% and 40% of patients, respectively, and BTFC was associated with less patient-reported ocular discomfort. Greater ocular comfort of glaucoma medications may improve treatment adherence.
Keywords: brinzolamide, dorzolamide, fixed combination, ocular discomfort, patient preference
Introduction
Glaucoma and ocular hypertension are vision-threatening conditions that may be associated with elevated intraocular pressure (IOP). Of the estimated 60+ million people worldwide with glaucoma in the year 2010, open-angle glaucoma accounted for nearly 75% of cases,1 and it has been estimated that open-angle glaucoma was the cause of bilateral blindness in more than 4.4 million people.1 Reducing IOP to prevent or delay disease progression is the standard of care for ocular hypertension and glaucoma,2 and treatment with topical ocular hypotensive medication has been shown to slow the progression of visual field defects.3 Many patients require two or more glaucoma medications after the 1st year of treatment to maintain target IOP reductions.3 Fixed combinations of two ocular hypotensive medications have been shown to effectively reduce IOP, simplify treatment regimens, and decrease cumulative exposure to preservatives and may increase treatment adherence compared with concomitant therapy with individual medications.4,5
The carbonic anhydrase inhibitors brinzolamide 1% and dorzolamide 2% reduce IOP by clinically significant magnitudes.6 Combination therapies comprising brinzolamide 1% or dorzolamide 2% and the β-blocker timolol 0.5% have IOP-lowering efficacy significantly greater than monotherapy with the individual active components.7,8 Furthermore, IOP-lowering efficacy of unfixed brinzolamide 1%/timolol 0.5% and unfixed dorzolamide 2%/timolol 0.5% is similar.9 These medications are generally well tolerated; dorzolamide 2% has been associated with greater ocular discomfort (ie, burning or stinging) compared with brinzolamide 1%.6,9–11 Successful IOP management relies on patient adherence to treatment regimens, which can be decreased by discomfort of ophthalmic instillations.10,12 Previous 1-day preference studies evaluated patient-reported ocular discomfort and patient preference after acute exposure to fixed-combination brinzolamide 1%/timolol 0.5% (BTFC; Azarga®, Alcon Laboratories, Inc., Fort Worth, TX, USA) and fixed-combination dorzolamide 2%/timolol 0.5% (DTFC; Cosopt®, Merck & Co., Inc., Whitehouse Station, NJ, USA).13,14 In these studies, patient-perceived discomfort may have been influenced by limited exposure to study medications (ie, two doses).13,14 The objective of this study was to assess the comfort-based patient preference after 1 week of exposure to each study medication in patients with open-angle glaucoma or ocular hypertension.
Methods
Study design and treatment
This was a 15-day, Phase IV, prospective, patient-masked, randomized, interventional, crossover study (www.ClinicalTrials.gov identifier, NCT01340014) conducted at ten sites in Germany, the UK, and Italy to assess patient preference for BTFC compared with DTFC after 1 week of administration of each study medication to both eyes. The study consisted of three visits at approximately the same time of the day (9.30 am): screening (day 0), follow-up after 1 week of the first treatment (day 7), and follow-up after 1 week of the second treatment (day 15; Figure 1). At screening, patients received one drop of BTFC in one eye and one drop of DTFC in the other eye to provide baseline comfort information on the two study medications. Patients were randomized to one of two treatment sequence groups: BTFC (first medication)-DTFC (second medication) or DTFC (first medication)-BTFC (second medication), with treatment identities masked to patients. Study medications were administered twice daily (one drop in each eye at 9 am and 9 pm) from days 1 to 6 (first medication) and days 9 to 14 (second medication). The morning doses on days 7 and 15 were administered by study site personnel. The first medication was washed out after the morning dose on day 7 until before the morning dose on day 9.
This study was performed in compliance with the Declaration of Helsinki and Good Clinical Practice. Patients provided written informed consent before the screening visit was conducted; consent forms were reviewed and approved. Approval in the UK was from the National Research Ethics Service; approval in Germany was from the Ethikkommission der Fakultät für Medizin, Klinikum rechts der Isar der TU München; and approval in Italy was from the Fondazione centro San Raffaele del Monte Tabor.
Patients
Eligible participants were ≥18 years of age, diagnosed with ocular hypertension or open-angle glaucoma (with or without pseudoexfoliation or pigment dispersion), and on a stable regimen of IOP-lowering medication for ≥30 days before the screening visit. Additional inclusion criteria were a baseline IOP considered safe (in the opinion of the investigator) in both eyes to ensure clinical stability of vision and the optic nerve throughout the study, IOP between 19 and 35 mmHg in ≥1 eye, and discontinuation of all other prescribed and over-the-counter ocular drugs before screening and for the entire study period. Key exclusion criteria were hypersensitivity to any components of study treatments; best-corrected visual acuity (BCVA) worse than 20/80 Snellen in either eye; any abnormality or opacity preventing reliable applanation tonometry or examination of the ocular fundus or anterior chamber in either eye; corneal dystrophies; concurrent conjunctivitis, keratitis, or uveitis in either eye; intraocular eye surgery (conventional or laser) within 3 months before the screening visit; risk of visual field or visual acuity worsening as a consequence of participation in the study; progressive retinal or optic nerve disease from any cause; history of ocular herpes simplex or hyperchloremic acidosis; severe allergic rhinitis or cardiopulmonary conditions that precluded safe use of a topical β-blocker; severe renal impairment; use of any topical carbonic anhydrase inhibitor (single or fixed combination) within 1 year before screening; women who were pregnant or lactating or could become pregnant during the study; and participation in any other investigational study within 30 days before the screening visit.
Outcome measures
The primary outcome was patient preference based on perceived ocular comfort, assessed through a questionnaire consisting of a single preference question with the ratings “prefer the first medication” or “prefer the second medication”. Patients completed the preference questionnaire on day 15 after instillation of the morning dose of the assigned medication. The secondary outcome measure was ocular discomfort using a 10-point scale (0= no discomfort, 9= substantial discomfort). Patients completed the ocular discomfort scale on days 7 and 15, approximately 1 minute after instillation of the morning dose of the assigned medication and before completion of the preference questionnaire on day 15. Anticipated adherence to treatment was evaluated as an exploratory outcome. The adherence questionnaire was completed on day 15 after completion of the preference questionnaire.
Safety outcome measures were adverse events (AEs), IOP, BCVA, and ocular signs (cornea, eyelids/conjunctiva, iris/anterior chamber, lens). AEs were assessed at all study visits and coded using Medical Dictionary for Regulatory Activities version 15.1. IOP was measured by Goldmann applanation tonometry in both eyes at screening and at the day 7 and day 15 follow-up visits. Ocular signs and BCVA were assessed for each eye using slit-lamp biomicroscopy and a Snellen visual acuity chart, respectively, at screening and at day 15.
Statistical analysis
Statistical testing was performed on a two-sided basis, with P<0.05 considered significant, using SAS/STAT® (SAS Institute, Cary, NC, USA). Demographic and baseline characteristic information for the intent-to-treat (ITT) population (ie, patients who received ≥1 dose of study medication, completed both treatment periods, and completed the preference questionnaire) was summarized descriptively; potential between-group differences in age were assessed by analysis of variance with treatment sequence, study period, and center as factors, and differences in sex and primary diagnosis were evaluated with Cochran–Mantel–Haenszel tests stratified by center. Treatment preference was assessed in the ITT dataset using chi-square tests, and preference for BTFC was compared versus 50% (ie, random chance) using a two-sided binomial test. Because one patient received the incorrect treatment sequence, a post hoc analysis based on the actual treatment received was also performed; the post hoc analysis used the same method of statistical testing as the prespecified analysis. Ocular discomfort scores were summarized descriptively and were compared using exact Wilcoxon–Mann–Whitney tests. Adherence questionnaire data were summarized descriptively by preferred medication in the ITT dataset. IOP was assessed in the safety population (ie, patients who entered into the study and received ≥1 dose of study medication) using analysis of variance that included sequence, patient within sequence, period, and treatment as factors. Ocular signs, logMAR (logarithm of the minimum angle of resolution)-converted BCVA, and AEs were summarized descriptively in the safety population. All analyses based on the safety population were carried out using the actual treatment sequence received.
Based on an assumed noncompletion rate of 10%, a sample size of 112 subjects was determined to ensure ≥100 evaluable patients with a stated medication preference. A study population of 100 evaluable patients provided 80% power to detect a minimal difference of 15% between the preference rates for the two study medications, using a two-sided binomial test at a significance level of 0.05.
Results
Patients
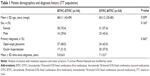
A total of 112 patients (mean ± SD age, 66±11 years) were randomized to treatment. Patients were mostly female (63.9%) and were diagnosed with open-angle glaucoma (65.7%). There were no significant between-group differences in patient characteristics (Table 1); 109 patients completed the study, and 108 patients completed the preference questionnaire and were included in the ITT dataset. One patient was randomized to the BTFC-DTFC sequence but received the DTFC-BTFC sequence; therefore, the reported treatment preference (ie, preference for the first or second medication) was attributed to the wrong study drug in the ITT dataset.
Efficacy outcomes
After exposure to both study treatments, 59.3% of patients (n=64/108) in the ITT dataset reported a preference for BTFC versus DTFC (95% exact CI, 49%–69%; P=0.0670; Figure 2A), a treatment difference of 18.6%. Analysis of patient preference data based on actual treatment received similarly demonstrated that more patients preferred BTFC over DTFC (60.2%; n=65/108; 95% exact CI, 51%–70%; P=0.0428). This post hoc analysis indicated that statistical significance of patient preference data was dependent on the correct versus incorrect allocation of one patient. Treatment preference was independent of the treatment sequence in both analyses (P≥0.695). Patients in the ITT dataset reported significantly less ocular discomfort with BTFC compared with DTFC (P=0.0002; least squares mean difference point estimate, −1.19; 95% CI, −1.80 to −0.58; Figure 2B); mean (median) level of discomfort was 2.6 (2.0) with BTFC and 3.7 (4.0) with DTFC. Ocular discomfort scores ≤3 were reported by 74.1% and 44.4% of patients with BTFC and DTFC, respectively.
On the adherence questionnaire, 57.1% of patients in the ITT population who preferred BTFC (n=56/98) reported being very confident or somewhat confident that they would use their preferred medication as prescribed, compared with 38.8% (n=38/98) who preferred DTFC (Table 2). In total, 27.6% of patients who preferred BTFC (n=27/98) and 13.3% of patients who preferred DTFC (n=13/98) were not at all confident that they would use a glaucoma medication that resulted in burning or stinging.
Safety outcomes
No serious AEs were reported with either treatment. A total of 16.1% of patients reported AEs during the study, including the screening period; 8.0% of patients (n=9/112) had AEs related to BTFC and 5.4% of patients (n=6/112) had AEs related to DTFC (Table 3). The most frequent treatment-related AEs were blurred vision (BTFC, n=4 patients; DTFC, n=1 patient), eye irritation (BTFC, n=2 patients; DTFC, n=3 patients), and eye pain (DTFC only, n=2 patients). Most treatment-related AEs were mild and of short duration, and all AEs resolved. Moderate AEs related to BTFC were abnormal sensation in the eye and dizziness (one patient each). Moderate AEs related to DTFC were eye irritation (two patients), blurred vision (one patient), and tachycardia (one patient). Two severe AEs (one event each of eye pain and nasopharyngitis) were reported as related to DTFC. Two patients discontinued the study because of AEs reported after instillation of BTFC (fatigue at screening lasting 3 days and blurred vision lasting 3 hours on day 10).
Mean ± SD IOP at screening was 21.02±2.08 mmHg in the left eye and 21.12±2.41 mmHg in the right eye. Mean IOP was not increased from baseline in either treatment group. No changes in BCVA from screening to day 15 were observed in either treatment sequence group; mean BCVA was 0.08 logMAR in the left and right eyes at screening and at day 15. A clinically significant change from screening to study end (eyelids/conjunctiva) was observed in both eyes of one patient in the BTFC-DTFC sequence group. No clinically significant changes were observed in assessments of cornea, iris/anterior chamber, or lens.
Discussion
Reducing IOP with one or more ocular hypotensive medications is the standard of care for minimizing glaucoma progression and preserving vision.2 Patient adherence to glaucoma treatment regimens is an important factor in long-term stability of IOP reduction, but adherence is typically poor for a variety of reasons, such as treatment complexity and poor treatment tolerability.15,16 Glaucoma medications that are better tolerated may lead to better patient adherence and therefore better treatment outcomes. Fixed-combination glaucoma therapies provide multiple ocular hypotensive agents in a single eye drop, which may improve adherence by simplifying treatment regimens.4 The objective of this crossover study was to assess preference for either BTFC or DTFC after 1 week of exposure to each study medication in patients with glaucoma or ocular hypertension.
Approximately 19% more patients reported a preference for BTFC compared with DTFC. This finding was not statistically significant (ie, P≥0.05) in the ITT dataset, wherein one patient received the incorrect treatment sequence; however, a post hoc analysis of preference data by actual treatment received yielded a P-value <0.05. Statistical significance of patient preference data was dependent on the correct versus incorrect allocation of one patient. Patients reported approximately 30% less ocular discomfort with BTFC compared with DTFC (discomfort scores, 2.6 versus 3.7). Additionally, compared with patients who preferred DTFC, greater percentages of patients who preferred BTFC reported being confident that they would use their preferred treatment as prescribed. No IOP increases from baseline were observed for either treatment group, and both study treatments were well tolerated; most treatment-related AEs were mild and of short duration, and no serious AEs occurred. A clinically significant change in eyelid/conjunctiva assessments was observed in both eyes of one patient in the BTFC-DTFC treatment sequence group at the exit visit; it is unclear whether this change was related to DTFC treatment or prior BTFC treatment because slit-lamp examination was performed only at baseline and at the end of the study. Ocular signs and BCVA were largely unchanged from screening to study completion.
In this study, 60.2% of patients reported a preference for BTFC and 39.8% of patients preferred DTFC. These results are consistent with previous double-masked crossover studies that demonstrated patient preference for BTFC over DTFC ranging from approximately 67% to 80%, and preference for DTFC over BTFC ranging from approximately 21% to 30%.13,14 Those studies assessed treatment preference after a single dose of BTFC or DTFC, in contrast with the 7 days of exposure to each treatment in the current study. In an open-label study of patients switched to BTFC from prior glaucoma therapies, patients preferred BTFC to DTFC at a ratio of more than 9 to 1; 89% of patients rated the tolerability of BTFC as good or very good compared with 29% for DTFC.17 The treatment difference in patient preference (approximately 19%) was smaller than in these previous reports.
In crossover studies, significantly higher ocular discomfort scores were reported with DTFC versus BTFC (2.9–3.5 versus 1.4–2.1);13,14 discomfort scores in this study were 3.7 and 2.6 with DTFC and BTFC, respectively. The modest difference in patient preference in favor of BTFC may be related to the increased severity of stinging or burning reported with DTFC. In previous studies, significantly more patients reported ocular pain and discomfort,13,18 more stinging for a longer duration, more eye redness,19 and more ocular irritation20 with DTFC compared with BTFC. Similar to this study, BTFC was associated with more temporary blurred vision.13,19
A potential limitation of this study is that data on screening failures were not collected, and it is possible that some patients may have decided not to participate in the study because of ocular discomfort associated with the doses of study medication administered at screening. Patient-reported ocular discomfort and treatment preference may have been influenced by differences in tear production and prior IOP-lowering medications. The short duration of the study is also a potential limitation. Further, the crossover design could have introduced a potential learning effect, particularly with regard to eye discomfort. However, patient preference for study medications was not associated with treatment sequence. Anticipated adherence with treatment based on patient comfort and preference was evaluated subjectively, but compliance with dosing was not objectively quantified. Finally, although treatment differences in ocular comfort and patient preference may influence compliance with topical glaucoma medications and therefore affect IOP outcomes, an effect size required for clinical significance was not determined. Hence, a conclusion cannot be made about whether or not the 18.6% difference in patient preference in favor of BTFC was clinically meaningful. Studies of longer duration that combine patient-reported ocular comfort and treatment preference with objective assessments of treatment adherence will provide valuable information.
Conclusion
In this crossover preference study, approximately 60% of patients preferred BTFC to DTFC after 7 days of treatment with each drug. This finding was statistically significant when analyzed based on actual drug received but not in the ITT dataset in which one patient received the incorrect treatment sequence. Both medications were well tolerated. Patients reported 30% less ocular discomfort with BTFC compared with DTFC. Greater ocular comfort of topical IOP-lowering medications may improve treatment adherence.
Acknowledgments
Medical writing assistance was provided by Heather D Starkey, PhD of Complete Healthcare Communications, Inc. (Chadds Ford, PA, USA), and was funded by Alcon.
Disclosure
This study was funded by Alcon Laboratories, Inc. (Fort Worth, TX, USA). RA, MLS, and PF have no financial, competing, or proprietary interests to disclose. DAH is an employee of Alcon Laboratories, Inc. The authors report no other conflicts of interest in this work.
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. | ||
Webers CA, Beckers HJ, Nuijts RM, Schouten JS. Pharmacological management of primary open-angle glaucoma: second-line options and beyond. Drugs Aging. 2008;25(9):729–759. | ||
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. | ||
Djafari F, Lesk MR, Harasymowycz PJ, Desjardins D, Lachaine J. Determinants of adherence to glaucoma medical therapy in a long-term patient population. J Glaucoma. 2009;18(3):238–243. | ||
Higginbotham EJ. Considerations in glaucoma therapy: fixed combinations versus their component medications. Clin Ophthalmol. 2010;4:1–9. | ||
Sall K. The efficacy and safety of brinzolamide 1% ophthalmic suspension (Azopt) as a primary therapy in patients with open-angle glaucoma or ocular hypertension. Brinzolamide Primary Therapy Study Group. Surv Ophthalmol. 2000;44(Suppl 2):S155–S162. | ||
Boyle JE, Ghosh K, Gieser DK, Adamsons IA. A randomized trial comparing the dorzolamide-timolol combination given twice daily to monotherapy with timolol and dorzolamide. Dorzolamide-Timolol Study Group. Ophthalmology. 1998;105(10):1945–1951. | ||
Kaback M, Scoper SV, Arzeno G, et al. Intraocular pressure-lowering efficacy of brinzolamide 1%/timolol 0.5% fixed combination compared with brinzolamide 1% and timolol 0.5%. Ophthalmology. 2008;115(10):1728–1734. | ||
Michaud JE, Friren B; International Brinzolamide Adjunctive Study Group. Comparison of topical brinzolamide 1% and dorzolamide 2% eye drops given twice daily in addition to timolol 0.5% in patients with primary open-angle glaucoma or ocular hypertension. Am J Ophthalmol. 2001;132(2):235–243. | ||
Barnebey H, Kwok SY. Patients’ acceptance of a switch from dorzolamide to brinzolamide for the treatment of glaucoma in a clinical practice setting. Clin Ther. 2000;22(10):1204–1212. | ||
Silver LH. Ocular comfort of brinzolamide 1.0% ophthalmic suspension compared with dorzolamide 2.0% ophthalmic solution: results from two multicenter comfort studies. Brinzolamide Comfort Study Group. Surv Ophthalmol. 2000;44(Suppl 2):S141–S145. | ||
Dreer LE, Girkin C, Mansberger SL. Determinants of medication adherence to topical glaucoma therapy. J Glaucoma. 2012;21(4):234–240. | ||
Mundorf TK, Rauchman SH, Williams RD, Notivol R; Brinzolamide/Timolol Preference Study Group. A patient preference comparison of Azarga (brinzolamide/timolol fixed combination) vs Cosopt (dorzolamide/timolol fixed combination) in patients with open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2008;2(3):623–628. | ||
Sanseau A, Sampaolesi J, Suzuki ER Jr, Lopes JF, Borel H. Preference for a fixed combination of brinzolamide/timolol versus dorzolamide/timolol among patients with open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2013;7:357–362. | ||
Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically: the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191–199. | ||
Sleath B, Robin AL, Covert D, et al. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113(3):431–436. | ||
Lanzl I, Raber T. Efficacy and tolerability of the fixed combination of brinzolamide 1% and timolol 0.5% in daily practice. Clin Ophthalmol. 2011;5:291–298. | ||
Vold SD, Evans RM, Stewart RH, Walters T, Mallick S. A one-week comfort study of BID-dosed brinzolamide 1%/timolol 0.5% ophthalmic suspension fixed combination compared to BID-dosed dorzolamide 2%/timolol 0.5% ophthalmic solution in patients with open-angle glaucoma or ocular hypertension. J Ocul Pharmacol Ther. 2008;24(6):601–605. | ||
Auger GA, Raynor M, Longstaff S. Patient perspectives when switching from Cosopt® (dorzolamide-timolol) to Azarga™ (brinzolamide-timolol) for glaucoma requiring multiple drug therapy. Clin Ophthalmol. 2012;6:2059–2062. | ||
Manni G, Denis P, Chew P, et al. The safety and efficacy of brinzolamide 1%/timolol 0.5% fixed combination versus dorzolamide 2%/timolol 0.5% in patients with open-angle glaucoma or ocular hypertension. J Glaucoma. 2009;18(4):293–300. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.