Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 10
Bracing In The Treatment Of Adolescent Idiopathic Scoliosis: Evidence To Date
Authors Karavidas N
Received 29 June 2019
Accepted for publication 18 September 2019
Published 8 October 2019 Volume 2019:10 Pages 153—172
DOI https://doi.org/10.2147/AHMT.S190565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Alastair Sutcliffe
Nikos Karavidas
Schroth Scoliosis & Spine Clinic, Physiotherapy Department, Athens, Greece
Correspondence: Nikos Karavidas
Schroth Scoliosis & Spine Clinic, Physiotherapy Department, Kolokotroni 5, Athens 15451, Greece
Tel +306974801432
Email [email protected]
Abstract: Brace effectiveness for adolescent idiopathic scoliosis was controversial until recent studies provided high quality of evidence that bracing can decrease likelihood of progression and need for operative treatment. Very low evidence exists regarding bracing over 40º and adult degenerative scoliosis. Initial in-brace correction and compliance seem to be the most important predictive factors for successful treatment outcome. However, the amount of correction and adherence to wearing hours have not been established yet. Moderate evidence suggests that thoracic and double curves, and curves over 30º at an early growth stage have more risk for failure. High and low body mass index scores are also associated with low successful rates. CAD/CAM braces have shown better initial correction and are more comfortable than conventional plaster cast braces. For a curve at high risk of progression, rigid and day-time braces are significantly more effective than soft or night-time braces. No safe conclusion on effectiveness can be drawn while comparing symmetrical and asymmetrical brace designs. The addition of physiotherapeutic scoliosis-specific exercises in brace treatment can provide better outcomes and is recommended, when possible. Despite the growing evidence for brace effectiveness, there is still an imperative need for future high methodological quality studies to be conducted.
Keywords: scoliosis, brace, non-operative treatment, orthosis, evidence
Introduction
According to Scoliosis Research Society (SRS), scoliosis is radiologically defined as a lateral spinal curve exceeding 10 degrees in a radiograph, with vertebra rotation.1 Society on Scoliosis Orthopedic and Rehabilitation Treatment (SOSORT) defines scoliosis more detailed, as a complex three-dimensional deformity of the spine and trunk, which appears in apparently healthy children and can go into progression due to multiple factors, during any rapid period of growth or even later in life.2 Approximately 80% of the scoliosis cases are adolescent idiopathic scoliosis (AIS), in which the cause still remains unknown.2
Scoliosis treatment can be either conservative or surgical. Non-operative treatment consists of observation, physiotherapy and/or bracing. The current SRS guidelines report observation or physiotherapy for curves below 25 degrees, brace indication between 25ο and 40ο, at a growth stage Risser 0–3.1 For scoliosis between 20ο and 30ο, the Lonstein formula can estimate progression risk and brace is indicated when surpasses 80%.3
The aims of scoliosis conservative treatment are summarized below:2
- Three-dimensional treatment of the deformity
- Halt progression or even partial correction
- Improve clinical appearance
- Improve pain and quality of life
- Avoid surgical treatment
A wide variety of braces have been described, including Boston, Cheneau and its derivatives, Milwaukee, Wilmington, Osaka Medical College (OMC), soft braces (SpineCor/TriaC), night-time braces (Providence/Charleston), etc., but their treatment results are non-consistent.4 BrAIST (Bracing in Adolescent Idiopathic Scoliosis Trial) study was a “landmark” multi-center randomized control trial (RCT),5 proving brace efficacy. The study stopped early for ethical reasons, as the preliminary results significantly favored brace treatment against observation. Zhang and Li (2019) in a meta-analysis, including only RCTs that compared brace with observation, concluded that bracing is an efficient and safe treatment for AIS, providing significantly better results than natural history.6
However, to date, there is still no safe conclusion on brace type, dosage of treatment or predictive factors contributing to a successful result. The purpose of the present article is to highlight the existed evidence for brace treatment and to provide an updated review, including the most recently published studies.
Materials And Methods
We performed a literature review in electronic databases (Pubmed, EMBASE, CINHAL, Google Scholar and Scopus), to retrieve the most relevant research for scoliosis bracing. The keywords used for the search were “brace”, “adolescent idiopathic scoliosis”, “orthosis”, “scoliosis”, and “non-operative treatment”. All relevant articles until August 2019, including all level of evidence, were analyzed to make a synthesis. Non-English language articles were excluded.
Level of Evidence was estimated according to the Journal of Bone and Joint Surgery updated guidelines.7
We divided our analysis into different categories:
- Evidence for scoliosis bracing
- Predictive factors for successful treatment (Table 1)
- Brace weaning
- Brace and physiotherapeutic scoliosis-specific exercises (PSSE)
- Adult bracing
- Comparing different brace types
 |  |  |  |
Table 1 Level Of Evidence Of The Predictive Factors For Bracing |
Results
Evidence For Scoliosis Bracing
Evidence Until 2013
For many decades, brace effectiveness remained controversial. Lenssick et al (2005) in their systematic review included RCTs and controlled clinical trials for conservative treatment, but despite some promising results, the methodological quality was very low.8 Weiss and Goodall (2008) compared non-operative and operative treatment options, including only prospective studies with a control group of natural history.9 A prospective controlled study supported in-patient rehabilitation with Schroth exercises, two long-term studies supported bracing and no study existed for surgery. The authors recommended the composition of a future RCT and concluded that the evidence for conservative treatment was scarce.9
In 2010, a first Cochrane review about the efficacy of bracing was published, including only RCTs and prospective cohorts comparing braces with either natural history or other braces, exercises and surgery.10 Only two studies met the strict inclusion criteria.11,12 Wong et al (2008)11 compared a rigid brace with SpineCor. Forty-three patients were recruited with an average Cobb angle 24.3ο and 45-month follow-up. Curve progression occurred in 4.7% in rigid brace group, while 31.8% in soft brace group. The authors also reported quality of life (QoL) outcomes, based on patient’s satisfaction, showing that rigid brace caused problems with heat and elastic brace with toileting.
Nachemson and Peterson (1995)12 in a prospective multinational research included 240 girls with AIS and Cobb angle 20ο to 35ο, who were divided into 3 groups, first wore rigid orthosis, second received electrical stimulation and third just observation. Four years after treatment 74% of the rigid orthosis avoided progression >5ο, while 34% for observation and 33% for electrical stimulation groups. However, the Cochrane review10 found very low quality of evidence, due to methodological pitfalls and pinpointed the need for further research.
Another systematic review in 201113 evaluated whether brace treatment could lead to lower surgical rates, better quality of life or improved curve angle compared to observation. Eight studies were included for analysis, using GRADE criteria for research quality assessment. One study significantly favored brace treatment regarding surgical rate. For post-treatment quality of life, two studies reported better outcome for bracing and one for observation. For curve reduction, one study showed a non-statistically significant difference in favor of bracing. Their conclusion was that low evidence existed to support brace treatment and proposed conduction of an RCT. Maruyama et al (2011)14 reported that, based on current evidence, brace recommendation could be for Cobb angles between 25ο and 35ο.
Sanders et al (2012)15 estimated the Number Needed to Treat (NNT) in order to prevent surgery. NNT is an epidemiological measurement, presenting the average number of patients who should be treated to prevent a bad outcome. Bracing could halt curve progression over 6ο but not to prevent surgery. The NNT was 9 patients to prevent an operation, but only 4 for highly compliant patients. Sanders et al (2014)16 in a later study found that the NNT to avoid surgery was 3 for compliant patients.
Positive results for bracing provided by other studies, but convenient samples or retrospective designs were used; therefore, no good evidence can be derived by them. Rigo et al (2003)17 in a retrospective study with 106 subjects used Cheneau brace with Schroth exercises and achieved 94.4% of success rate in terms of avoiding surgery. Negrini et al (2008)18 combined brace with SEAS (Scientific Exercises Approach to Scoliosis) exercises getting a success rate of 95.5%, but mean Cobb angle was very low (23.4ο), so patients with low risk of progression were included. Zaborowska et al (2011)19 reported contradictive results, as the success rate was only 48.1%, using Cheneau orthosis and physiotherapy with SRS criteria.
Two studies showed high effectiveness of Progressive Action Short Brace (PASB) in the treatment of single lumbar or thoracolumbar curves.20,21 In 2009, 50 patients wore the PASB brace and followed up 2 years post-weaning. As high as 94% of the patients improved, 6% remained stable and nobody progressed. Similarly, in 2012, 82.5% improved and 17.5% remained stable.21 Coillard et al (2011)22 found that SpineCor brace was superior to observation, but Cobb angle ranged 15ο to 30ο, so not at high risk of progression.
SRS Inclusion Criteria For Bracing
SRS Committee on Bracing and Nonoperative Management in 2005 published their optimal inclusion criteria for AIS brace research to standardize the methodology of future research in order to make comparisons more compatible.23 The SRS criteria are described as:
- Age > 10 years at brace prescription
- Growth stage, Risser 0–2
- Cobb angle 25ο–40ο
- No prior treatment
- If female, less than 1-year postmenarchal
Furthermore, assessment of effectiveness should include:
- Percentage of curve progression or improvement, defined with a cut-off point of 5ο
- Percentage of patients exceeding 45ο, which is defined as the surgical threshold
- Minimum 2 years follow-up after skeletal maturity to clarify the percentage required operation
- Reporting of compliance
SRS and SOSORT in 2015, after a Consensus Delphi process, agreed to report patient-centered outcomes as primary measurements (esthetics, disability, pain, quality of life) and radiological parameters as secondary.1 They also emphasized the role of adherence to treatment for conservative treatment and decided to exclude menarche-related criteria for research, due to poor reliability in residual growth prediction.
Recent Evidence Using SRS Research Criteria For Bracing, After 2013
BrAIST study5 used the SRS inclusion criteria but finally separated into a randomized and a preference cohort (patients chose treatment), because of rejection to randomization of approximately 60% of the participants. Moreover, inclusion criteria were broadened by accepting subjects over 20ο. A total of 242 patients divided into 2 groups, bracing and observation. Treatment failure was determined as curve progression to 50ο or more. The trial stopped early for ethical reasons, as the results were significantly better for bracing. The success rate was 72% for the brace group and 48% for the observation group. A positive correlation of brace wear time and treatment success was reported.
Following the BrAIST study, many authors used SRS research criteria to validate brace effectiveness and some combined brace and PSSE. A first attempt for a complete conservative approach, with brace and exercises, was made in 2009 and reported only 4% of progression.24 All curve patterns improved, except from double major. De Giorgi et al (2013)25 treated AIS patients with Cheneau brace and exercises, having 100% success rate in avoiding surgery. Both studies used SRS criteria, but had retrospective analysis, so possible selection bias can influence their results and decrease the quality of evidence.
Negrini et al (2014)26 in a prospective study demonstrated the effectiveness of bracing along with PSSE, as only 9.6% experienced a curve progression, 52.3% improved and 30.8% remained unchanged. The intent-to-treat analysis (considering dropouts as failures) raised the percentage of progression to 15%, but significantly better compared to BrAIST study (28%).5 Maruyama et al (2015)27 retrospectively evaluated the effectiveness of Rigo-Cheneau type brace in 33 scoliotic patients. As high as 76% avoided progression, while just 12% passed 45ο at the end of follow-up and 3% had spinal fusion. Hump degrees and in-brace correction (IBC) were crucial factors for success or failure. The sample was small, but all curve types were included.
Kuroki et al (2015)28 performed a retrospective cohort to investigate the efficacy of Osaka Medical College (OMC) brace. Success rate was 67.7% regarding progression, but significantly higher (88.2%) for subjects with better adherence to treatment. Weiss et al (2015)29 found 66% IBC in 21 patients, with Cheneau-Gensingen brace produced by computer-aided design/computer-aided manufacturing (CAD/CAM), but no data on curve progression among participants were provided.
Aulisa et al (2015)30 evaluated the effectiveness of Lyon brace in 102 patients with single thoracic scoliosis. Two years post-weaning, 85.5% of the curves improved, 13% remained stable and only 1.5% progressed (98.5% success rate). Sixteen percent drop-out rate, retrospective selection, no worst-case scenario analysis (authors reported that 5% of the dropouts had progression at abandonment) and exclusion of double curves were some of the study limitations.
The aforementioned studies added some evidence (Level II or III), but their results should be interpreted by caution because of methodological pitfalls (lack of control group, retrospective design, inappropriate inclusion criteria, selection bias). The higher success rates compared to the BrAIST study5 can be partly explained by the development of brace manufacturing and the combination with PSSE.
Bracing For Curves Above 40ο
According to SRS, surgery is indicated for curves over 40ο.1 Natural history studies have shown greater potential for progression in adulthood for curves exceeding 50ο.31 The measurement error on X-rays (3ο–7ο), defining progression or surgical indication, should also be taken into account before decision-making for operative or non-operative treatment.2
The absence of strong scientific evidence for operative versus non-operative treatment and a considerable percentage of patients rejecting surgery created an interest to examine brace effectiveness for curves exceeding 40ο.32
Lusini et al (2014)33 in a prospective controlled study investigated the efficacy of brace treatment for curves above 45ο. The intent-to-treat analysis revealed 20.5% failures for Brace group (39 patients, Risser 0–4, refused surgery, brace and PSSE) and 55.6% for Control group (18 patients, no treatment). As high as 53.8% of the brace group even improved >5ο. Their findings were confirmed by Weiss et al (2017),34 who reported 92% success rate of 25 patients (mean Cobb 49ο, Risser 0.84), treated with Gensingen Cheneau brace (48% stable, 44% improved, 8% progressed).
Similarly, Aulisa et al (2019)35 recruited 160 patients (Cobb > 40ο, Risser 0–4, refused operation) and the success rate was 91% (78% improved, 13% stabilized, 9% progressed). No intent-to-treat-analysis was performed for the dropouts (28 patients). In contrast, Zhu et al (2017)36 found bracing less effective for curves 40ο–50ο (35% success rate) in a retrospective cohort of 54 patients, but recommended brace as an alternative option for those refusing surgical intervention. Two years later, they measured an increased success rate of 51.1% (Cobb 40ο–45ο, 37.8% improved, 13.3% stabilized, 48.9% progressed).37
To summarize, low evidence (Level of Evidence III) supports brace effectiveness for curves above 40ο, so it could serve as a treatment option when surgery is refused. The variable success rate is attributed to different brace types and use of PSSE in some studies. More prospective studies, including patients at peak of growth, are needed to confirm brace effectiveness in surgical ranges.
Predictive Factors For Successful Bracing
Initial In-Brace Correction
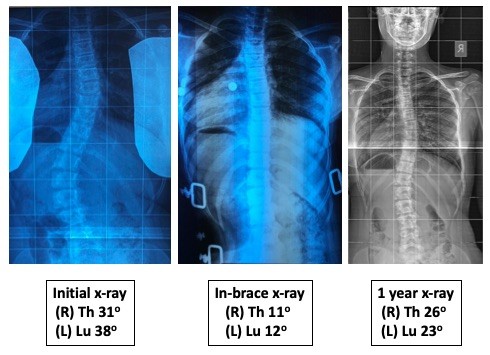
In-brace correction (IBC) is defined as the percentage of Cobb angle reduction during an X-ray with the brace fitted on the patient (Figure 1).
 |
Figure 1 In-brace correction is the most important predictive factor for successful brace treatment. |
Katz and Durani (2001)38 found that a minimum 25% of the IBC is required for double curves to have successful treatment. Castro et al (2003)39 concluded that bracing should not be recommended for IBC less than 20%. Landauer et al (2003)40 reported that IBC over than 40% and good compliance significantly influence the treatment outcome. Weiss and Rigo (2011)41 got into the same conclusion, but they did not mention the threshold for success. Goodbody et al (2016)42 concluded that brace failure was increased when IBC was less than 45%, while Xu et al (2017)43 found a significantly less IBC needed for successful brace treatment (16.3%) and defined at least 10% IBC as the optimal cut-off point.
Some authors that reported success rates above 90% had achieved significantly larger IBC. Weiss et al (2013)29 measured 66% of the IBC and De Mauroy et al (2014)44 achieved an average IBC of 70% (64% for thoracic and 76% for lumbar curves). According to a recent systematic review by Van de Bogaart el (2019),45 IBC is the strongest predictor for a successful brace treatment, but El Hawary et al (2019) found lower evidence.46 The difference occurs due to the different methodological criteria to quantify the level of evidence. However, both found no consensus on the cut-off percentage which increases the risk for failure. Further research is necessary to establish a minimum in-brace correction rate to be considered as good brace correctability.
Compliance
Compliance is described as the percentage of brace wearing time according to doctor’s prescription. BrAIST study (Level I) proved that there is a dose–effect response of bracing, which increases with longer wearing times.5 The average brace wearing time for the successful treatment group in BrAIST study was 12.9 hrs/day, but this should not be considered as the general threshold for being compliant.5
Rowe et al (1997)47 measured proportion of success 0.93 for bracing 23 hrs/day, which was significantly higher than for 8 or 16 hrs (0.6 and 0.62, respectively). Katz and Durani (2001)39 found that wearing an orthosis more than 18 hrs/day can significantly decrease the likelihood of progression. Landauer et al (2003)40 concluded that bad compliance was correlated with curve progression. Rahman et al (2005),48 considering high compliant patients those who wore the brace more than 90% of the prescribed hours, found 5 times less progression rate (11%) for compliant compared to non-compliant (56%).
Brox et al (2012)49 in a large prospective cohort of 459 AIS patients predefined compliance as brace wear more than 20 hrs/day and concluded that risk for progression was significantly less for the compliant group, 19.5% compared to 55.7% for the non-compliant group. Aulisa et al (2014)50 included 645 juvenile and AIS patients and measured that completely compliant patients (brace worn as prescribed) had better outcomes than incompletely compliant. Interestingly, the authors concluded that bracing discontinuation less than 1 month per year had no influence on the treatment outcome.
Kuroki et al (2015)51 had a success rate of 67.7%, statistically higher for those wearing the brace more than 15 hrs/day. Karol et al (2016)52,53 found that more brace wearing time led to less progression rates. The authors proposed that children at Risser 0, with greater risk for progression, should wear the brace at least 18 hrs/day.53 Lou et al (2016)54 created a predictive model for brace success, identifying quantity of bracing as an important prognostic factor. Thompson et al (2017)55 found 30% progression rate above 50ο in compliant patients, but they used 13 hrs as the threshold wearing time for compliance, which was definitely low for curves at high risk of progression. According to the existed literature, there is moderate to strong evidence (Level I or II) that limited brace wearing time is related to increased risk of treatment failure.45,46
SRS recognizes compliance as an important parameter for final outcome and recommends for brace studies to always report adherence to treatment. Monitoring devices can give more accurate data than self-reported or family reported compliance and should be implemented in orthotic management research.54 But, so far, only four studies used a sensor device to measure compliance.5,48,52,54
SOSORT guidelines (2016) recommend the built of a multi-professional team, consisted of Orthopedic Surgeon, Orthotist and Physiotherapist, to enhance treatment adherence and improve outcomes.2 Tavernaro et al (2012)56 compared two groups, one with a full team approach and another with insufficient collaboration between professionals. The lack of team management increased by five times the potential of non-compliance. The results confirmed by Donzelli et al (2015)57 who found significantly higher brace compliance rates than the published literature and pinpointed the necessity of interprofessional approach to improve compliance. In both studies, the team management also led to better quality of life (QoL) scores. Chan et al (2014)58 also showed that higher brace wear compliance was positively related with better QoL.
The term “quality of bracing” was firstly introduced by Lou et al (2004)59 to describe the tightness of brace during wearing hours. They assessed the forces exerted by the brace by tightening the straps and found a positive correlation between tightness and treatment outcomes. Similar correlations were found in 2006.60 Ten years later, they proposed a prognostic model of brace treatment outcome, based on Cobb angle, risk for progression, in-brace correction and brace quantity (hours/day) and quality (tightness of the brace), which provided reliable scientific evidence to be used in clinical practice.54 However, there was no specific recommendation on how to tighten the brace, and this exclusively relies on orthotist’s experience.
Curve Magnitude
Emans et al (1986),61 using a Boston brace, stated that higher initial curve magnitude increased the potential for surgery. Katz and Durani (2001)38 found that double curves, with initial thoracic curve above 35ο are more likely to be progressed. Sun et al (2010)62 observed that initial Cobb angle over 30ο was an independent risk factor for progression. Ovadia et al (2012)63 concluded that low baseline Cobb angle values are associated with less progression rate, but they did not find a statistically significant correlation. Karol et al (2016) reported higher risk of progression for curves 30ο–39ο at Risser 0 with open triradiate cartilage (OTC)53 (Prognostic Level II).
Kuroki et al (2015)51 found insignificantly lower success rate in Cobb angles between 20ο and 30ο, compared to above 30ο, so they concluded that there is no association of curve magnitude and treatment success. Same conclusion was made by Xu et al (2017)64 and Sun et al (2017),65 who did not recognize initial curve magnitude as predictive factor.
Van de Bogaart et al (2019)45 in a systematic review found moderate scientific evidence that initial Cobb angle is not related with treatment failure and limited evidence about treatment success. This conclusion was made for scoliosis curves within the brace indication range according to SRS (25ο to 45ο). On the other hand, El Hawary et al (2019) recognized initial Cobb angle >30ο as one of the three main risk factors for brace failure.46
Although we know that scoliosis progression in natural history depends mainly on Cobb angle and growth stage,3 it is unclear whether brace treatment success is dependent on curve magnitude. As already discussed in the previous section, there is also low evidence (Level III) for brace effectiveness even for curves over 40ο. Some studies assumed that curve magnitude could be a prognostic factor, but the advanced materials and technology in brace fabrication during the last decade have not supported this assumption, so the evidence remains debatable.45
Curve Type
Some authors have found that main thoracic and double curves are more prone to progression and this can be attributed to the reduced flexibility of thoracic spine and less potential for correction.45 Emans et al (1986)61 found that major curves with apical level below T8 and above L2 demonstrated better control and IBC. Katz and Durani (2001)38 found increased likelihood of progression in double curves, especially when thoracic curve was initially more than 35ο. Analogous results were reported by Sun et al (2010)62 and Thompson et al (2017),55 finding that main thoracic curves and above 30ο pre-brace led to high risk of worsening. In contrast, Kuroki et al (2015),51 Sun et al (2017)65 and Xu et al (2017)64 did not identify curve type as a significant prognostic factor. A very recent systematic review concluded that curve type has moderate evidence as a determinant of predicting brace treatment success.45
Growth Stage
An old study by Hanks et al (1988)66 identified Risser sign and onset of menarche as significant prognostic factors for brace success, and they recommended no bracing for patients being post-menarche or Risser 1 and greater, but this is in conflict with the SRS bracing guidelines. Sun et al (2010)62 found lower Risser grade and pre-menarche status to be significant risk variables, but in a later study, they did not get statistical significance.65 Ovadia et al (2012)63 revealed that high Risser score was correlated with treatment success. Low Risser sign was also a significant predictor in two other studies.50,64
Karol et al (2016)53 associated Risser 0 and open triradiate cartilage (OTC) with higher risk of failure. Patients with OTC (Risser 0−) and Cobb angle >30ο had 63% risk of progression compared to 32.4% for those with closed (Risser 0+). However, four studies of moderate quality (Level of Evidence III) did not recognize growth stage as a prognostic factor for treatment success.38,51,64,67 Dolan et al (2014) using BrAIST data found that Sanders scale was more predictive for brace failure than Risser stage and combined with Cobb angle and treatment gave the best-fitting prediction model.68
Van de Bogaart et al (2019)45 concluded that there is conflicting evidence regarding growth stage and menarche status as predictors for successful brace treatment. El Hawary et al (2019) in their review recognized low level of skeletal maturity as a consistent risk factor for progression.46 (Level II).
CAD/CAM And FEM Technology
For many decades, the traditional approach for brace manufacturing was the plaster-cast approach to take the measures from the patient and produce a hand-made brace. A technological revolution occurred in the first years of the 21st century and more technicians changed to computer-assisted technology, by taking the measures with a laser scanner and using CAD/CAM programs. Initially, the purpose was to achieve at least similar correction with the conventional plaster-cast method, and this was proven by a few early studies that evaluated CAD/CAM corrections.69–73 Many later studies demonstrated significantly better IBC with CAD/CAM compared to traditional approach, adding consistent scientific evidence (Level of Evidence II).29,44,72 Furthermore, CAD/CAM braces could save time,69 be lighter and more comfortable for the patients, which could have a positive impact on compliance70,74 and could substitute plaster-cast braces.73
Nowadays, it is clear that CAD/CAM braces are superior to traditional plaster-cast braces, but a CAD/CAM brace cannot “a priori” guarantee a successful treatment result, as many other parameters play important role.40 Weiss and Kleban (2015)75 compared CAD/CAM bracing based on curve classification (CBA) with CAD/CAM based on Finite Element Modelling (FEM) approach. CBA presented to have 66% IBC and FEM 42%, but no statistical significance was obtained. Cobetto et al (2016 and 2017)76,77 in two RCTs demonstrated that a combination of CAD/CAM and FEM can further improve IBC and 3D correction by the brace. The FEM group showed 47% and 48% IBC for thoracic and lumbar curves, respectively, compared to 25% and 26% of control CAD/CAM braces and axial rotation correction 46% compared to 30% by control braces. Furthermore, the FEM braces were 50% thinner and had 20% less covering surface, being more comfortable for the patients.76,77
Body Mass Index (BMI)
BMI is defined as a value derived from body mass divided by the square of body height.78 It is used to determine if an adolescent is under-weight (<5th percentile of sex and age-specific BMI), normal weight (5th to 85th percentile) or over-weight (>84th percentile). O’Neill et al (2005)79 found that over-weight AIS patients had 3.1 times more possibilities to fail in brace treatment than those not over-weighted. Progression over 45ο happened in 45% of over-weight and 28% of normal. Gilbert et al (2015)80 reported that patients with high BMI more frequently have a first diagnosis with larger Cobb angles, potentially due to difficulties in scoliosis detection in obese patients, but not more likely for surgical intervention.
Goodbody et al (2016)41 concluded that both high and low BMI patients have greater risk for brace failure. High BMI patients failed because they appeared to have significantly lower IBC and less compliance, but a subsequent analysis, taking into consideration compliance and IBC, disappeared the significance. However, for the low BMI group, the poor outcome remained significant. Sun et al (2017)64 confirmed that low BMI could be a prognostic variable for brace failure in AIS patients. As high as 43.1% of the failure group were under-weight and 17.6% of the success group, so BMI was significantly correlated with bracing failure. The retrospective studies by Vachon et al (2007)81 and Zaina et al (2017)82 reported similar brace results for overweight and normal-weight patients. Van de Bogaart et al (2019),44 analyzing the published literature, found limited evidence that low BMI is associated with brace failure and conflicting evidence regarding high BMI. Further research is required to highlight the role of BMI in the prediction of brace success.
Other Prognostic Factors
Many other parameters have been studied to find out their association with brace success or failure, but there is no conclusive evidence to date. Upadhyay et al (1995)83 were the first who showed that reduction of vertebra rotation in-brace, was an indicator of successful outcome. Ovadia et al (2012)62 reported that low Angle Trunk Rotation (ATR), measured by scoliometer during Adam’s test, was associated with increased potential for successful treatment. Yamane et al (2016)84 found that insufficient in-brace correction of rotation increased the likelihood of progression. It seems that vertebra and trunk rotation are factors that can influence the final result, but the quality of evidence is still very low.
Katz and Durani (2001)37 identified that lumbar pelvic relationship (LPR) greater than 12ο was a significant factor of brace failure. Xu et al (2011)85 recognized two genes (ERα and TPH-1) as potential predictors of brace outcome. Mao et al (2016)86 defined initial Cobb angle reduction velocity (ARV) as the value occurred after dividing the Cobb angle reduction divided by the time interval between first and second measurement (3 or 6 months for the study). They found that ARV was better predictor than IBC. Although these publications have shown some correlation between those parameters and brace treatment result, the evidence is very scarce to be considered as important factors. Osteopenia was also found in some papers to be correlated with increased risk of failure (Level of Evidence II).45
Other studies found that menarche, growth velocity, Cobb ratio, vertebral tilt angle, rib vertebra angle, coronal decompensation, apical vertebral translation, relative apical distance, lateral trunk shift and curve flexibility were not associated with brace failure.45 Retroverted orientation of the vertebrae was associated with brace failure, while major curve apex, correction at 6 months follow-up and angle of thoracic rotation were associated with successful brace treatment, but with poor scientific evidence.45
Comparing Brace Types
Rigid Versus Soft Braces
Weiss and Weiss (2005)87 found that Cheneau thoraco-lumbo-sacral orthosis (TLSO) provided significantly less progression rate (20%), compared to SpineCor brace (92%), even though the average Cobb angle at baseline was 33.7ο for the Cheneau group and 21.3ο for the SpineCor group. Some of the progressed patients from SpineCor group changed to Cheneau brace and 70% of them stopped further progression. Wong et al (2008)88 reported 32% failure rate of SpineCor, while 5% for rigid brace, but similar patient’s acceptance for wearing the brace. Gammon et al (2010)89 included only patients fulfilling the SRS research criteria and compared a rigid TLSO with SpineCor brace, with both groups having the same baseline characteristics. The success rate in terms of 5ο progression was 60% for TLSO and 53% for SpineCor, while 80% and 72% accordingly regarding passing 45ο. Although the results slightly favored the TLSO group, no statistical significance was obtained.
Guo et al (2014)90 in a prospective randomized controlled study, using SRS criteria, compared a rigid TLSO with the SpineCor brace. Curve progression occurred in 5.6% of rigid group and 35% of SpineCor. When SpineCor brace changed to TLSO, 71.4% avoided progression. Gutman et al (2016)91 also used SRS criteria in a retrospective analysis and found 76% progression rate for SpineCor, compared to 55% for Boston brace. Misterska et al (2019)92 in a cross-sectional study concluded that the rigid brace group reported better QoL outcomes than SpineCor group. From the published literature, there is clear evidence that rigid brace is more effective than elastic, especially for patients at high risk of progression during growth spurt (Figure 2).
 |
Figure 2 A rigid brace on the left side and a soft brace on the right side of the photo. |
Day-Time Versus Night-Time Brace
Katz et al (1997)93 showed that Boston brace was more effective than Charleston brace in avoiding progression. Their findings were most notable for curves initially between 36ο and 45ο, as 83% of Charleston and 43% of Boston groups progressed. According to the authors, Charleston could be useful only in mild curves. Howard et al (1998)94 compared a TLSO with Charleston and Milwaukee braces and found that TLSO was superior than both other braces at preventing curve progression. Janicki et al (2007)95 evaluated the effectiveness of Providence night-time brace and TLSO, using SRS criteria. Totally 85% of TLSO and 69% of Providence groups progressed more than 5ο, while 79% of TLSO and 60% of Providence required surgery. The authors concluded that Providence was more effective for curves below 35ο, but the overall high failure rate, compared to other studies, could raise doubts about the quality of brace designs in this study.
Simony et al (2019) in a retrospective cohort, including patients wearing Providence brace, with initial IBC >60%, less than 12 months post-menarche (no Risser sign referred), found a success rate of 89%.96 They recommended that at least 70% IBC is required for successful treatment. This was the first study to provide some very low evidence (Level of Evidence III) for the use of night-time braces in curves above 35ο during growth.
Symmetric Versus Asymmetric Brace
Von Deimling et al (1995)97 found significantly better results for Cheneau brace in reduction of spinal decompensation compared to Milwaukee brace. Minsk et al (2017)98 retrospectively analyzed the effectiveness of Rigo-Cheneau brace (RCB) and Boston TLSO. No patient from RCB and 34% of Boston groups progressed beyond surgical threshold. As high as 31% of RCB and 13% of Boston improved more than 6ο. The results revealed that RCB was more effective, but the poor methodological design and the small sample of RCB (13 individuals) cannot generalize the results. Sy et al (2016)99 in a mini-review compared the published results of in-brace correction and claimed that asymmetric braces can lead to greater corrections in single curve patterns. However, to date, there is no clear evidence whether asymmetric brace is more effective than symmetric brace. (Figure 3).
 |
Figure 3 An asymmetric brace on the left side and a symmetric brace on the right side of the photo. |
Same Brace Concepts
Some authors compared similar brace designs, having recent advancements, with old styles. Montgomery and Wilner (1989)100 found that Boston brace was superior in comparison with Milwaukee brace, regardless of initial scoliosis angle and growth stage. Negrini and Marchini (2007)101 showed that the new SPoRT (Symmetrical, Patient-Oriented, Rigid, Three-dimensional, active) concept proved to more efficient than the traditional three-point system obtained by Lyon brace. Zaina et al (2015)102 in a multi-center study compared 2 super-rigid braces, Sforzesco (SPoRT concept) and ART (Asymmetrical, Rigid, Torsion) brace. They are made by the same material and the main difference is that ART brace had more asymmetric envelope but cannot be considered as importantly asymmetric brace. Both braces were successful in short term, although the ART brace had slightly better in-brace correction, but not statistically and clinically significant. De Mauroy et al (2015)103 found significantly better in-brace correction for the “new” Lyon brace (ART brace) compared to old Lyon and proposed the complete replacement of old Lyon and plaster cast, by the ART brace.
Brace Weaning Phase
SOSORT guidelines proposed that brace weaning phase should initiate at Risser 4.2 At brace weaning, some loss of correction is expected in 30% to 43% of patients, mostly in the first 6 months.90,104,105 A few researchers tried to determine a proper process of brace weaning to avoid this progression. Steen et al (2015)106 identified that an unplanned early weaning led to greater progression rates and recommended regular monitoring every 4–6 months until reaching skeletal maturity. Piantoni et al (2018)107 also suggested gradual brace weaning at Risser 4 and after 24 months post-menarche.
In contrast, Minkara et al (2018)108 revealed a 21.8% mismatch between Sanders 3–5 and Risser 2–5 growth scales, which means that some patients might be undertreated, being considered as skeletally mature but actually with remained growth. Cheung et al (2019)109 concluded that Risser sign is an inadequate indicator for brace weaning and recommended Sanders stage 8 and radius grade 10/ulna grade 9, as the most proper timepoint for weaning. Zaina et al (2009)110 found that scoliosis-specific exercises (PSSE) can markedly reduce the loss of correction at brace weaning, so the implementation of PSSE at that stage could potentially stabilize curve progression.
Brace And PSSE
PSSE are curve pattern-specific exercises, based on 3D auto-correction, self-elongation and activities of daily living training2 (Figure 4). Many studies were conducted to evaluate the effect of a complete non-operative scoliosis treatment with brace and PSSE. In all but one study until 2014, the surgical rate was below 10% (0%–9.6%). Only Zaborowska et al (2011)18 found 51.8% progression above 50ο, but it is unclear whether the exercises were scoliosis-specific and the quality of bracing questionable. Rivett et al (2014)111 reported that high compliant patients with Rigo-Cheneau brace and PSSE resulted in significant improvement of 10.2ο, while non-compliant worsened by 5.5ο.
 |
Figure 4 Physiotherapeutic scoliosis-specific exercises. |
Schreiber et al (2015, 2016)112,113 in an RCT added Schroth exercises to the standard of care (either brace or observation) and found reduced Cobb angle, improved QoL and muscle endurance compared to standard care alone. Same results were achieved by Kwan et al (2017),114 with 21% progression rate for the brace and Schroth group and 50% for the brace alone group. Zheng et al (2018)115 in an RCT compared bracing with PSSE and found that bracing was more successful in improving Cobb angle and body symmetry, while PSSE significantly better in QoL, functional and psychological outcomes.
There is Level of Evidence I, supported by 3 RCTs, that PSSE can improve bracing treatment result. SOSORT guidelines (2016)2 states that PSSE along with bracing can provide better results than the brace without exercises and are highly recommended.
Adult Bracing
In general, SRS does not recommend bracing for adult patients with scoliosis. However, many patients reject surgical intervention and the role of non-operative treatment need to be studied. De Mauroy et al (2016)116 attempted to classify adult scoliosis and create a rationale for brace treatment, proposing that patients with degenerative scoliosis with rotatory dislocation and disc instability could potentially become good candidates for a short brace. They evaluated their first result, reporting 80% stabilization or improvement for adult patients, who followed brace treatment and scoliosis-specific exercises, at a follow-up of 8 years.117 Palazzo et al (2017)118 at 5 years follow-up found that bracing can slow down the progression rate that was observed in their participants 10 years pre-brace. Zaina et al (2018)119 used Peak scoliosis brace, for 2 hrs per day, to manage pain with satisfied short-term results. There is an increasing interest in adult bracing, but there is still no good evidence to support its effectiveness (Level of Evidence IV).
Discussion
Analyzing the results, it seems that there is strong evidence to support the use of brace for AIS treatment. Brace is superior than natural history and according to SRS, it should be used for curves between 25ο and 40ο–45ο, with a residual growth. However, there is lack of high-quality, randomized/prospective control studies, and further research with adequate inclusion criteria and methodological design are of paramount importance. SRS established the brace research criteria to standardize research quality, by including only patients at high risk of progression for analysis.
Some studies provided low evidence that brace could be an alternative treatment option for patients above 40ο that refused surgery, while no actual evidence exists for adult bracing, although some authors reported short-term improvement in pain and curve stabilization. The role of PSSE in combination with bracing still needs to be studied, but there is good evidence so far that the treatment result can be enhanced. PSSE could also aid in correction loss at brace weaning, so future studies combining brace and PSSE are highly recommended. Some of PSSE disadvantages are the limited access to therapists, compliance with home-program, time-consuming and lack of coverage by insurances.
Although brace is efficient in the general population, there is still a remarkable percentage of patients that will not be benefited from bracing, for many reasons. A recent meta-analysis demonstrated statistically significant better treatment results and quality of life for bracing compared to observation.6 The authors also mentioned some adverse events of bracing (pain, skin irritation, kidney disorders and psychosocial issues, etc.) that should be better analyzed in future studies. A serious attempt has been made to identify predictive factors that are related to treatment success. There is strong evidence for the in-brace correction (IBC) and moderate evidence for compliance. The role of team management is crucial to increase adherence to treatment. Good evidence suggests that CAD/CAM braces provide better IBC than traditional plaster braces.
Moderate evidence exists that double scoliosis, major thoracic curves and Cobb angle above 35ο have greater potential for progression. Limited evidence relates low and high BMI with an increased risk of brace failure. Thus, there is an imperative need for early detection of scoliosis. Scoliosis Research Society (SRS), American Academy of Orthopedic Surgeons (AAOS), Pediatric Society of North America (POSNA) and American Academy of Pediatrics (AAP) in their position statement recommended efficient screening programs by well-trained personnel and when diagnosed recent high-quality studies demonstrated the conservative treatment with bracing and PSSE can prevent progression to the surgical threshold.120 Finally, there is clear evidence that for curves at high risk of progression, rigid and day-time braces are superior than soft and night-time braces. No conclusion can be drawn regarding symmetric and asymmetric brace superiority.
Our study had some limitations and results therefore should be interpreted with caution. In our analysis, we included all the relevant articles despite their methodological quality and the majority was subject to various biases. Many studies established progression above 5ο as treatment failure, while others used the reach of surgical threshold (40ο−50ο). Brace design was not always clearly described. However, we attempted to mention the Level of Evidence for every predicting factor, in order to provide a balanced synthesis.
Conclusion
To conclude, there is strong evidence for bracing as AIS treatment. The most important predicting factors for treatment success are in-brace correction and compliance, followed by curve magnitude and early growth stage. For curves at high risk of progression, rigid and day-time braces are recommended. PSSE can further improve the treatment result, so they are recommended as supplementary to bracing. Finally, despite the existed evidence, there is a need for future research with prospective and randomized controlled trials, using SRS inclusion criteria for bracing.
Abbreviations
AAOS, American Academy of Orthopedic Surgeons; AAP, American Academy of Pediatrics; AIS, Adolescent Idiopathic Scoliosis; ART, Asymmetrical, Rigid, Torsion; ARV, Angle Reduction Velocity; ATR, Angle Trunk Rotation; BMI, Body Mass Index; BrAIST, Bracing in Adolescent Idiopathic Scoliosis Trial; CAD/CAM, Computer-Aided Design/Computer-Aided Manufacturing; EOS, Early Onset Scoliosis; FEM, Finite Element Modelling; IBC, In-Brace Correction; NNT, Number Needed to Treat; OMC, Osaka Medical College; OTC, Open triradiate Cartilage; PASB, Progressive Action Short Brace; POSNA, Pediatric Society of North America; PSSE, Physiotherapeutic Scoliosis-Specific Exercises; QoL, Quality of Life; RCB, Rigo Cheneau Brace; RCT, Randomized Controlled Trial; SEAS, Scientific Exercises Approach to Scoliosis; SOSORT, Society on Scoliosis Orthopedic and Rehabilitation Treatment; SPoRT, Symmetrical, Patient-Oriented, Rigid, Three-Dimensional; SRS, Scoliosis Research Society; TLSO, Thoraco-Lumbo-Sacral Orthosis.
Acknowledgments
I would like to thank Dr. Manuel Rigo for his contribution in the final review of the paper.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Negrini S, Hresko T, O’Brien J, Price N; SOSORT Boards and SRS Non-Operative Committee. Recommendations for research studies on treatment of idiopathic scoliosis: consensus 2014 between SOSORT and SRS non-operative management committee. Scoliosis. 2015;10:8. doi:10.1186/s13013-014-0025-4
2. Negrini S, Donzelli S, Aulisa A, et al. SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2016;2018(13):3.
3. Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66(7):1061–1071.
4. Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2015;18(6):CD006850.
5. Weinstein S, Dolan L, Wright J, Dobbs M. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369:1512–1521. doi:10.1056/NEJMoa1307337
6. Zhang Y, Li X. Treatment of bracing for adolescent idiopathic scoliosis patients: a meta-analysis. Eur Spine J. 2019. doi:10.1007/s00586-019-06075-1
7. Marx RG, Wilson SM. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1–2. doi:10.2106/JBJS.N.01112
8. Lenssinck ML, Frijlink AC, Berger MY, Bierman-Zeinstra SM, Verkerk K, Verhagen AP. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther. 2005;85(12):1329–1339.
9. Weiss HR, Goodall D. The treatment of adolescent idiopathic scoliosis (AIS) according to present evidence. A systematic review. Eur J Phys Rehabil Med. 2008;44(2):177–193.
10. Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2010;20(1):CD006850.
11. Wong MS, Cheng JC, Lam TP, et al. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine. 2008;33(12):1360–1365. doi:10.1097/BRS.0b013e31817329d9
12. Nachemson A, Peterson L. Effectivenss of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77(6):815–822. doi:10.2106/00004623-199506000-00001
13. Davies E, Norvell D, Hermsmeyer J. Efficacy of bracing versus observation in the treatment of idiopathic scoliosis. Evid Based Spine Care J. 2011;2(2):25–34. doi:10.1055/s-0030-1267102
14. Maruyama T, Grivas T, Kaspiris A. Effectiveness and outcomes of brace treatment: a systematic revies. Physiother Theory Pract. 2011;27(1):26–42. doi:10.3109/09593985.2010.503989
15. Sanders J, Newton P, Browne R, Herring A. Bracing in adolescent idiopathic scoliosis, surrogate outcomes, and the number needed to treat. J Pediatr Orthop. 2012;32(Suppl 2):S153–S157. doi:10.1097/BPO.0b013e31825199e5
16. Sanders J, Newton P, Browne R, Katz D, Birch J, Herring J. Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am. 2014;96(8):649–653. doi:10.2106/JBJS.M.00290
17. Rigo M, Reiter C, Weiss HR. Effect of conservative management on the prevalence of surgery in patients with adolescent idiopathic scoliosis. Pediatr Rehabil. 2003;6(3–4):209–214. doi:10.1080/13638490310001642054
18. Negrini S, Atanasio S, Zaina F, Romano M, Parzini S, Negrini A. End-growth results of bracing and exercises for adolescent idiopathic scoliosis. Prospective worst-case analysis. Stud Helath Technol Inform. 2008;135:395–408.
19. Zaborowska-Sapeta K, Kowalski I, Kotwicki T, Protasiewicz-Faidowska H, Kiebzak W. Effectiveness of Cheneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis. 2011;6(1):2. doi:10.1186/1748-7161-6-2
20. Aulisa A, Guzzanti V, Galli M, Perisano C, Falciglia F, Aulisa L. Treatment of thoraco-lumbar curves in adolescent females affected by idiopathic scoliosis with a progressive action short brace (PASB): assessment of results according to the SRS committee on bracing and nonoperative management standardization criteria. Scoliosis. 2009;18(4):21. doi:10.1186/1748-7161-4-21
21. Aulisa A, Guzzanti V, Perisano C, Marzetti E, Falciglia F, Aulisa L. Treatment of lumbar curves in scoliotic adolescent females with progressive action short brace: a case series based on the Scoliosis Research Society Committee Criteria. Spine (Phila Pa 1976). 2012;37(13):E786–E791. doi:10.1097/BRS.0b013e31824b547d
22. Coillard C, Circo A, Rivard C. A prospective randomized controlled trial of the natural history of idiopathic scoliosis versus treatment with the SpineCor brace: SOSORT Award 2011 Winner. Eur J Phys Rehabil Med. 2014;50:479–487.
23. Richards B, Bernstein M, D’Amato C, Thompson G. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on bracing and nonoperative management. Spine (Phila Pa 1976). 2005;30(18):2068–2075. doi:10.2106/JBJS.15.01313
24. Negrini S, Atanasio S, Fusco C, Zaina F. Effectiveness of complete conservative treatment for adolescent idiopathic scoliosis (bracing and exercises) based on SOSORT management criteria: results according to the SRS criteria for bracing studies – SOSORT Award 2009 Winner. Scoliosis. 2009;4(4):19. doi:10.1186/1748-7161-4-19
25. De Giorgi S, Piazzola A, Tafuri S, Borracci C, Martucci A, De Giorgi G. Cheneau brace for adolescent idiopathic scoliosis: long-term results.Can it prevent surgery? Eur Spine J. 2013;22(Suppl 6):S815–S822. doi:10.1007/s00586-013-3020-1
26. Negrini S, Donzelli S, Lusini M, Minnella S, Zaina F. The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis on SRS and SOSORT criteria: a prospective study. BMC Musculoskelet Disord. 2014;15:263. doi:10.1186/1471-2474-15-263
27. Maruyama T, Kobayashi Y, Miura M, Nakao Y. Effectiveness of brace treatment for adolescent idiopathic scoliosis. Scoliosis. 2015;10(Suppl S2):S12. doi:10.1186/1748-7161-10-S2-S12
28. Kuroki H, Inomata N, Hamanaka H, Higa K, Chosa E, Tajima N. Efficacy of the Osaka Medical College (OMC) brace in the treatment of adolescent idiopathic scoliosis following Scoliosis Research Society brace studies criteria. Scoliosis. 2015;10:12. doi:10.1186/s13013-015-0036-9
29. Weiss HR, Seibel S, Moramarco M, Kleban A. Bracing scoliosis: the evolution to CAD/CAM for improved in-brace corrections. Hard Tissue. 2013;2(5):43. doi:10.13172/2050-2303
30. Aulisa A, Guzzanti V, Falciglia F, Giordano M, Marzetti E, Aulisa L. Lyon bracing in adolescent females with thoracic idiopathic scoliosis: a prospective study based on SRS and SOSORT criteria. BMC Musculoskelet Disord. 2015;24(16):316. doi:10.1186/s12891-015-0782-0
31. Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65(4):447–455.
32. Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst Rev. 2015;24(4):CD010663.
33. Lusini M, Donzelli S, Minnella S, Zaina F, Negrini S. Brace treatment is effective in idiopathic scoliosis over 45ο: an observational prospective cohort-controlled study. Spine. 2014;14(9):1951–1956. doi:10.1016/j.spinee.2013.11.040
34. Weiss HR, Tournavitis N, Seibel S, Kleban A. A prospective cohort study of AID patients with 40ο and more treated wih a Gensingen Brace (GBW): preliminary results. Open Orthop J. 2017;11(Suppl–9, M8):1558–1567. doi:10.2174/1874325001711011558
35. Aulisa A, Guzzanti V, Falciglia F, Giordano M, Galli M, Aulisa L. Brace treatment of idiopathic scoliosis is effective for a curve over 40 degrees, but is the evaluation of Cobb angle the only parameter for the indication of treatment? Eur J Phys Rehabil Med. 2019;55(2):231–240. doi:10.23736/S1973-9087.18.04782-2
36. Zhu Z, Xu L, Jiang L, et al. Is brace treatment appropriate for adolescent idiopathic scoliosis patients refusing surgery with Cobb angle between 40 and 50 degrees. Clin Spine Surg. 2017;30(2):85–89. doi:10.1097/BSD.0b013e3182a1de29
37. Xu L, Yang X, Wang Y, et al. Brace treatment in adolescent idiopathic scoliosis patients with curve between 40ο and 45ο: effectiveness and related factors. World Neurosurg. 2019;pii: S1878-8750(19):30620–30625.
38. Katz D, Durrani A. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2001;26(21):2354–2361. doi:10.1097/00007632-200111010-00012
39. Castro FP. Adolescent Idiopathic Scoliosis, bracing and the Hueter-Volkmann principle. Spine Surg. 2003;3(3):180–185.
40. Landauer F, Wimmer C, Behensky H. Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil. 2003;6(3–4):201–207. doi:10.1080/13638490310001636817
41. Weiss HR, Rigo M. Expert-driven Cheneau applications: description and in-brace corrections. Physiother Theory Pract. 2011;27(1):61–67. doi:10.3109/09593985.2010.503991
42. Goodbody C, Asztalos I, Sankar W, Flynn J. It’s not just the big kids: both high and low BMI impact bracing success for adolescent idiopathic scoliosis. J Child Orthop. 2016;10(5):395–404. doi:10.1007/s11832-016-0763-3
43. Xu L, Qin X, Qiu Y, Zhu Z. Initial correction rate can be predictive of the outcome of brace treatment in patients with adolescent idiopathic scoliosis. Clin Spine Surg. 2017;30(4):E475–E479. doi:10.1097/BSD.0000000000000343
44. De Mauroy JC, Lecante C, Barral F, Pourret S. Prospective study and new concepts based on scoliosis detorsion of the first 225 early in-brace radiological results with the new Lyon brace: aRTbrace. Scoliosis. 2014;9:19. doi:10.1186/1748-7161-9-19
45. Van Den Bogaart M, Van Royen B, Haanstra T, De Kleuver M, Faraj S. Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: a best-evidence synthesis. Eur Spine J. 2019;28:511–525. doi:10.1007/s00586-018-05870-6
46. El Hawary R, Zaaror DR, Floman Y, Lonner B, Alkhalife YI, Betz R. Brace treatment in AIS: risk factors for failure – A literature review. Spine. 2019. doi:10.1016/j.spinee.2019.07.008
47. Rowe D, Bernstein S, Riddick M, Adler F, Emans J, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments of idiopathic scoliosis. J Bone Joint Surg Am. 1997;79(5):664–674. doi:10.2106/00004623-199705000-00005
48. Rahman T, Bowen J, Takemitsu M, Scott C. The association between brace compliance and outcome for patients with idiopathic scoliosis. J Pediatr Orthop. 2005;25(4):420–422. doi:10.1097/01.bpo.0000161097.61586.bb
49. Brox J, Lange J, Gunderson R, Steen H. good brace compliance reduced curve progression and surgical rates in patients with idiopathic scoliosis. Eur Spine J. 2012;21(10):1957–1963. doi:10.1007/s00586-012-2386-9
50. Aulisa A, Giordano M, Falciglia F, Marzetti E, Roscia A, Guzzanti V. Correlation between compliance and brace treatment in juvenile and adolescent idiopathic scoliosis: SOSORT 2014 award winner. Scoliosis. 2014;9:6. doi:10.1186/1748-7161-9-6
51. Kuroki H, Inomate N, Hamanaka H, Higa K, Chosa E, Tajima N. Predictive factors of Osaka Medical College (OMC) brace treatment in patients with adolescent idiopathic scoliosis. Scoliosis. 2015;10:11. doi:10.1186/s13013-015-0038-7
52. Karol L, Virostek D, Felton K, Wheeler L. Effect of compliance counselling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2016;98(1):9–14. doi:10.2106/JBJS.O.00359
53. Karol L, Virostek D, Felton K, Jo C, Butler L .The effect of the Risser stage on bracing outcome in adolescent idiopathic scoliosis. J Bone Joint Surg Am.2016;98:1253–1259. tavernaro. doi:10.2106/JBJS.15.01313
54. Lou E, Hill D, Raso J, Moreau M, Hedden D. How quantity and quality of brace wear affect the brace treatment outcomes for AIS. Eur Spine J. 2016;25:495–499. doi:10.1007/s00586-015-4233-2
55. Thompson R, Hubbard E, Jo C, Virostek D, Karol L. Brace success is related to curve type in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2017;99(11):923–928. doi:10.2106/JBJS.16.01050
56. Tavernaro M, Pellegrini A, Tessadri F, Zaina F, Zonta A, Negrini S. Team care to cure adolescents with braces (avoiding low quality of life, pain and bad compliance): a case-control retrospective study. 2011 SOSORT Award winner. Scoliosis. 2012;7(1):17. doi:10.1186/1748-7161-7-17
57. Donzelli S, Zaina F, Negrini S. Compliance monitor for scoliosis braces in clinical practice. J Child Orthop. 2015;9(6):507–508. doi:10.1007/s11832-015-0703-7
58. Chan S, Cheung K, Luk K, Wong K, Wong M. A correlation study between in-brace correction, compliance to spinal orthosis and health-related quality of life of patients with adolescent idiopathic scoliosis. Scoliosis. 2014;9:1. doi:10.1186/1748-7161-9-1
59. Lou E, Raso J, Hill D, Durdle N, MahoodJ MM. Correlation between quantity and quality of orthosis wear and treatment outcomes in AIS. Prosth Orthot Int J. 2004;28:49–54.
60. Lou E, Hill D, Raso J, Mahood J, Moreau M. Prediction of brace treatment outcome by monitoring brace usage. Stud Health Technol Inform. 2006;123:239–244.
61. Emans J, Kaelin A, Bancel P, Hall J, Miller M. The Boston bracing system for idiopathic scoliosis: follow-up results in 295 patients. Spine. 1986;11(8):792–801. doi:10.1097/00007632-198610000-00009
62. Sun X, Wang B, Qiu Y, et al. Outcomes and predictors of brace treatment for girls with adolescent idiopathic scoliosis. Orthop Surg. 2010;2(4):285–290. doi:10.1111/j.1757-7861.2010.00101.x
63. Ovadia D, Eylon S, Mashiah A, Wientroub S, Lebel E. Factors associated with the success of the Rigo System Cheneau brace in treating mild to moderate adolescent idiopathic scoliosis. J Child Orthop. 2012;6(4):327–331. doi:10.1007/s11832-012-0429-8
64. Xu L, Qin X, Qiu Y, Zhu Z. Initial correction rate can be predictive of the outcome of brace treatment in patients with adolescent idiopathic scoliosis. Clin Spine Surg. 2017;30(4):E475–E479. doi:10.1097/BSD.0000000000000343
65. Sun W, Zhou J, Sun M, et al. Low body mass index can be predictive of bracing failure in patients with adolescent idiopathic scoliosis: a retrospective study. Eur Spine J. 2017;26(6):1665–1669. doi:10.1007/s00586-016-4839-z
66. Hanks G, Zimmer B, Nogi J. TLSO treatment of idiopathic scoliosis. An analysis of the Wilmington jacket. Spine. 1988;13:626–629.
67. O’Neill P, Karol L, Shindle M, et al. Decreased orthotic effectiveness in overweight patients with adolescent idiopathic scoliosis. J Bone Joint Surg. 2005;87(5):1069–1074. doi:10.2106/JBJS.C.01707
68. Dolan L, Weinstein SL, The BrAIST Study Group. To brace or not? The answer is “it depends”. Preliminary results from BrAIST. Scoliosis Spinal Disord. 2014;9:O26.
69. Wong M, Cheng J, Lo K. A comparison of treatment effectiveness between the CAD/CAM method and the manual method for managing adolescent idiopathic scoliosis. Prosthet Orthot Int. 2005;29(1):105–111. doi:10.1080/17461550500069547
70. Wong M, Cheng J, Wong W, So S. A work study of the CAD/CAM method and conventional manual method in the fabrication of spinal orthoses for patients with adolescent idiopathic scoliosis. Prosthet Orthot Int. 2005;29(1):93–104. doi:10.1080/17461550500066782
71. Sankar W, Albrektson J, Leman L, Tolo V, Skaggs D. Scoliosis in-brace curve correction and patient preference of CAD/CAM versus plaster molded TLSOs. J Child Orthop. 2007;1(6):345–349. doi:10.1007/s11832-007-0066-9
72. Desbiens-Blais F, Clin J, Parent S, Labelle H, Aubin CE. New brace design combining CAD/CAM and biomechanical simulation for the treatment of adolescent idiopathic scoliosis. Clin Biomech. 2012;27(10):999–1005. doi:10.1016/j.clinbiomech.2012.08.006
73. Wong M. Computer-aided design and computer-aided manufacture (CAD/CAM) system for construction of spinal orthosis for patients with adolescent idiopathic scoliosis. Phys Theory Pract. 2011;27(11):74–79. doi:10.3109/09593980903269741
74. Cobetto N, Aubin CE, Clin J, Le May S, Desbiens-Blais F, Parent S. Braces optimized with computer-assisted design and simulations are lighter, more comfortable, and more efficient than plaster-cast braces for the treatment of adolescent idiopathic scoliosis. Spine Deform. 2014;2(4):276–284. doi:10.1016/j.jspd.2014.03.005
75. Weiss HR, Kleban A. Development of CAD/CAM based brace models for the treatment of patients with scoliosis-classification based approach versus finite element modelling. Asian Spine J. 2015;9(5):661–667. doi:10.4184/asj.2015.9.5.661
76. Cobetto N, Aubin CE, Parent S, et al. Effectiveness of braces designed using computer-aided design and manufacturing (CAD/CAM) and finite element simulation compared to CAD/CAM only for the conservative treatment of adolescent idiopathic scoliosis: a prospective randomized controlled trial. Eur Spine J. 2016;25(10):3056–3064. doi:10.1007/s00586-016-4434-3
77. Cobetto N, Aubin CE, Parent S, Barchi S, Turgeon I, Labelle H. 3D correction of AIS in braces designed using CAD/CAM and FEM: a randomized controlled trial. Scoliosis Spinal Disord. 2017;12:24. doi:10.1186/s13013-017-0128-9
78. Dehghan M, Akhtar-Daneshand N, Merchant A. Childhood obesity, prevalence and prevention. Nutr J. 2005;4:24. doi:10.1186/1475-2891-4-24
79. Zhang Y, Yang Y, Dang X, et al. Factors relating to curve progression in female patients with adolescent idiopathic scoliosis treated with a brace. Eur Spine J. 2015;24(2):244–248. doi:10.1007/s00586-014-3674-3
80. Gilbert S, Savage A, Whitesell R, Conklin M, Fineberg N. BMI and magnitude of scoliosis at presentation to a specialty clinic. Pediatrics. 2015;135(6):e1417–e1424. doi:10.1542/peds.2014-2000
81. Vachon V, Circo A, Coillard C, Rivard C. Positive outcome in obese patients with adolescent idiopathic scoliosis treated with the SpineCor Brace. Scoliosis. 2007;2(Suppl 1):S22. doi:10.1186/1748-7161-2-S1-S22
82. Zaina F, Donzelli S, Negrini S. Overweight is not predictive of bracing failure in adolescent idiopathic scoliosis: results from a retrospective cohort study. Eur Spine J. 2017;26(6):1670–1675. doi:10.1007/s00586-017-4985-y
83. Upadhyay S, Nelson I, Ho E, Hsu L, Leong J. New prognostic factors to predict the final outcome of brace treatment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 1995;20(5):537–545. doi:10.1097/00007632-199503010-00006
84. Yamane K, Takigawa T, Tanaka M, Sugimoto Y, Arataki S, Ozaki T. Impact of rotation correction after brace treatment on prognosis in adolescent idiopathic scoliosis. Asian Spine J. 2016;Oct; 10(5):893–900. doi:10.4184/asj.2016.10.5.893
85. Xu L, Qiu X, Sun X, et al. Potential genetic markers predicting the outcome of brace treatment in patients with adolescent idiopathic scoliosis. Eur Spine J. 2011;20(10):1757–1764. doi:10.1007/s00586-011-1874-7
86. Mao S, Shi B, Xu L, et al. Initial cobb angle reduction velocity following bracing as a new predictor for curve progression in adolescent idiopathic scoliosis. Eur Spine J. 2016;25(2):500–505. doi:10.1007/s00586-015-3937-7
87. Weiss HR, Weiss G. Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): a prospective trial comparing two different concepts. Pediatr Rehabil. 2005;8(3):199–206. doi:10.1080/13638490400022212
88. Wong M, Cheng J, Lam T, et al. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2008;33(12):1360–1365. doi:10.1097/BRS.0b013e31817329d9
89. Gammon S, Mehlman C, Chan W, Helfetz J, Durrett G, Wall E. A comparison of thoracolumbosacral orthoses and SpineCor treatment of adolescent idiopathic scoliosis patients using the Scoliosis Research Society standardized criteria. J Pediatr Orthop. 2010;30(6):531–538. doi:10.1097/BPO.0b013e3181e4f761
90. Guo J, Lam T, Wong M, et al. A prospective randomized controlled study on the treatment outcome of SpineCor brace versus rigid brace for adolescent idiopathic scoliosis with follow-up according to the SRS standardized criteria. Eur Spine J. 2014;23(12):2650–2657. doi:10.1007/s00586-013-3146-1
91. Gutman G, Benoit M, Joncas J, et al. The effectiveness of the SpineCor brace for the conservative treatment of adolescent idiopathic scoliosis. Comparison with the Boston brace. Spine J. 2016;16(5):626–631. doi:10.1016/j.spinee.2016.01.020
92. Misterska E, Glowacki J, Kolban M. Does rigid spinal orthosis carry more psychosocial implications than the flexible brace in AIS patients? A cross-sectional study. J Back Musculoskelet Rehabil. 2019;32(1):101–109. doi:10.3233/BMR-181121
93. Katz D, Richards B, Browne R, Herring J. A comparison between the Boston brace and the Charleston bending brace in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 1997;22(12):1302–1312. doi:10.1097/00007632-199706150-00005
94. Howard A, Wright J, Hedden D. A comparative study of TLSO, Charleston, and Milwaukee braces for idiopathic scoliosis. Spine (Phila Pa 1976). 1998;23(22):2404–2411. doi:10.1097/00007632-199811150-00009
95. Janicki J, Poe-Kochert C, Armstrong D, Thompson G. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27(4):369–374. doi:10.1097/01.bpb.0000271331.71857.9a
96. Simony A, Beuschau I, Quisth L, Jespersen SM, Carreon LY, Andersen MO. Providence nighttime bracing is effective in treatment for adolescent idiopathic scoliosis even in curves larger than 35ο. Eur Spine J. 2019. doi:10.1007/s00586-019-06077-z
97. Von Deimling U, Wagner U, Schmitt O. Long-term effect of brace treatment on spinal decompensation in idiopathic scoliosis. A comparison of Milwaukee brace-Cheneau corset. Z Orthop Ihre Grenzgeb. 1995;133(3):270–273.
98. Minsk M, Venutti K, Daumit G, Sponseller P. Effectiveness of the Rigo Cheneau versus Boston-style orthoses for adolescent idiopathic scoliosis: a retrospective study. Scoliosis Spinal Disord. 2017;20(12):7. doi:10.1186/s13013-017-0117-z
99. Sy N, Borysov M, Moramarco M, Nan X, Weiss HR. Bracing scoliosis – state of the Art (Mini-review). Curr Pediatr Rev. 2016;12(1):36–42.
100. Wilner MF. Prognosis of brace-treated scoliosis. Comparison of the Boston and Milwaukee Methods in 244 Girls. Acta Orthop Scand. 1989;60(4):383–385.
101. Negrini S, Marchini G. Efficacy of the symmetric, patient-oriented, rigid, three-dimensional, active (SPoRT) concept of bracing for scoliosis: a prospective study of the Sforzesco versus Lyon brace. Eura Medicophys. 2007;43(2):171–181.
102. Zaina F, De Mauroy JC, Donzelli S, Negrini S, Award Winner SOSORT. 2015: a multicentre study comparing the SPoRT and ART braces effectiveness according to the SOSORT-SRS recommendations. Scoliosis. 2015;10:23. doi:10.1186/s13013-015-0049-4
103. De Mauroy JC, Journe A, Gagaliano F, Lecante C, Barral F, Pourret S. The new Lyon ARTbrace veruss the historical Lyon brace: a prospective case series of 148 consecutive scoliosis with short time results after 1 year compared with a historical retrospective case series of 100 consecutive scoliosis; SOSORT award 2015 winner. Scoliosis. 2015;10:26. doi:10.1186/s13013-015-0047-6
104. Shi B, Guo J, Mao S, et al. Curve progression in adolescent idiopathic scoliosis with a minimum of 2 years follow-up after completed brace weaning with reference to the SRS standardized criteria. Spine Deform. 2016;4(3):200–205. doi:10.1016/j.jspd.2015.12.002
105. Aulisa A, Guzzanti V, Falciglia F, Galli M, Pizzetti P, Aulisa L. Curve progression after long-term brace treatment in adolescent idiopathic scoliosis: comparative results between over and under 30 degrees – SOSORT 2017 award winner. Scoliosis Spinal Disord. 2017;12:36. doi:10.1186/s13013-017-0142-y
106. Steen H, Lange JE, Brox J. Early weaning in idiopathic scoliosis. Scoliosis. 2015;10:32. doi:10.1186/s13013-015-0059-2
107. Piantoni L, Tello C, Ramondino R, Francheri W, Galaretto E, Noel M. When and how to discontinue bracing treatment in adolescent idiopathic scoliosis: results of a survey. Scoliosis Spinal Disord. 2018;26(13):23. doi:10.1186/s13013-018-0158-y
108. Minkara A, Bainton N, Tanaka M, et al. High risk of mismatch between Sanders and Risser staging in adolescent idiopathic scoliosis: are we guiding treatment using the wrong classification? J Pedriat Orthop. 2018;22.
109. Cheung J, Cheung P, Luk K. When should we wean bracing for adolescent idiopathic scoliosis? Clin Orthop Relat Res. 2019;13:2145–2157.
110. Zaina F, Negrini S, Atanasio S, Fusco C, Romano M, Negrini A. Specific exercises performed in the period of brace weaning can avoid loss of correction in Adolescent Idiopathic Scoliosis (AIS) patients; Winner of SOSORT’s 2008 Award for Best Clinical Paper. Scoliosis. 2009;4:8. doi:10.1186/1748-7161-4-8
111. Rivett L, Stewart A, Potterton J. The effect of compliance to a Rigo System Cheneau brace and a specific exercise programme on idiopathic scoliosis curvature: a comparative study: SOSORT 2014 award winner. Scoliosis. 2014;9:5. doi:10.1186/1748-7161-9-5
112. Schreiber S, Parent E, Moez E, et al. The effect of Schroth exercises added to standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis-an assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner”. Scoliosis. 2015;18(10):24. doi:10.1186/s13013-015-0048-5
113. Schreiber S, Parent E, Moez E, et al. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better cobb angle outcomes in adolescents with idiopathic scoliosis-an assessor and statistician blinded randomized controlled trial. PLoS One. 2016;11(12):e0168746. doi:10.1371/journal.pone.0168746
114. Kwan K, Cheng A, Koh H, Chiu A, Cheung K. Effectiveness of Schroth exercises during bracing in adolescent idiopathic scoliosis: results from a preliminary study-SOSORT Award 2017 Winner. Scoliosis Spinal Disord. 2017;12:32. doi:10.1186/s13013-017-0139-6
115. Zheng Y, Dang Y, Yang Y, et al. Whether orthotic management and exercise are equally effective to the patients with adolescent idiopathic scoliosis in mainland China: A randomized controlled trial study. Spine (Phila Pa 1976). 2018;43(9):E494–E503. doi:10.1097/BRS.0000000000002412
116. De Mauroy JC, Lecant C, Barral F, Pourret S. bracing in adult with scoliosis: experience in diagnosis and classification from a 15-year prospective study of 739 patients. Scoliosis Spinal Disord. 2016;11(2):29. doi:10.1186/s13013-016-0090-y
117. De Mauroy JC, Lecante C, Barral F, Pourret S. Prospective study of 158 adult scoliosis treated by a bivalve polyethylene overlapping brace and reviewed at least 5 years after brace fitting. Scoliosis Spinal Disord. 2016;11(2):28. doi:10.1186/s13013-016-0091-x
118. Palazzo C, Montigny J, Barbot F, et al. Effects of bracing in adult with scoliosis: A retrospective study. Arch Phys Med Rehabil. 2017;98(1):187–190. doi:10.1016/j.apmr.2016.05.019
119. Zaina F, Poggio M, Donzelli S, Negrini S. Can bracing help adults with chronic back pain and scoliosis? Short-term results from a pilot study. Prosthet Orthot Int. 2018;42(4):410–414. doi:10.1177/0309364618757769
120. SRS/POSNA/AAOS/AAP. Position statement – screening for the early detection of idiopathic scoliosis in adolescents. Available from: https://www.srs.org/about-srs/news-and-announcements/position-stetement-screening-for-the-early-detection-for-idiopathic-scoliosis-in-adolescents.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
