Back to Journals » International Journal of Women's Health » Volume 13
Birth Preparedness and Complication Readiness and Associated Factors Among Recently Delivered Mothers in Mizan-Aman Town, Southwest Ethiopia, 2019
Authors Wudu MA , Tsegaye TB
Received 18 October 2020
Accepted for publication 4 February 2021
Published 15 February 2021 Volume 2021:13 Pages 177—187
DOI https://doi.org/10.2147/IJWH.S279201
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Muluken Amare Wudu,1 Tesfa Birlew Tsegaye2
1Department of Pediatrics and Child-Health Nursing, College of Medicine and Health Sciences, Wollo University, Dessie, 1145, Ethiopia; 2Department of Public-Health, College of Medicine and Health Sciences, Debre Markos University, Debre-Markos, 269, Ethiopia
Correspondence: Muluken Amare Wudu
Department of Pediatrics and Child-Health Nursing, College of Medicine and Health Sciences, Wollo University, Dessie, 1145, Ethiopia
Tel +251912975922
Fax +251 333115052
Email [email protected]
Background: Pregnancy and childbirth-related deaths have become a global public health issue and the burden is more prevalent in sub-Saharan Africa, including Ethiopia. While several attempts have been made to minimize maternal mortality, the practice of birth preparedness and complication readiness is still inadequate in Ethiopia. As a result, this study was initiated to identify the gaps in birth preparedness and complication readiness practice in Southwest Ethiopia.
Objective: Aimed to assess the magnitude of birth preparedness, anticipated complication practices, and associated factors among recently delivered women in Mizan-Aman Town, southwestern Ethiopia, 2019.
Methods: A community-based cross-section study was conducted on 491 recently delivered mothers between May and June 2019. A multistage sampling technique was employed and data were collected via face-to-face interviews using a structured questionnaire. The result was analyzed via SPSS version 25 and binary logistic regression was used to determine the association. Finally, the results were deemed significant when the P-value was < 0.05.
Results: Out of 491 mothers, only 109 (22.2%) of respondents were well prepared for birth and its complications. Having a history of stillbirth 3.646 (AOR: 95% CI: 1.72, 5.65), being informed the term BP/CR from their friends 3.05 (AOR: 95% CI: 1.04, 8.89), being aware of pregnancy danger signs 2.82(AOR: 95% CI: 1.21,6.57) and being aware of two out of four postpartum danger signs 3.571(AOR: 95% CI: 1.511,8.443) were found to be important predictors of birth preparedness and its complication practice. In addition, having infants birth order between 4– 6 and being a housewife mother by occupation were considered as protective factors.
Conclusions and Recommendations: The status of birth preparedness and its complication was found to be low in this study and, therefore, intensive awareness-raising and promotion activities shall be implemented at the community and health facility level.
Keywords: birth preparedness, complication readiness, southwestern Ethiopia
Background
Birth preparedness and complication preparation (BP/CR) is the method of preparing for normal birth and anticipating the intervention required in the case of an emergency. It includes the identification of the places where they will give birth, the identification of a potential blood donor, the identification of a skilled birth attendant. Identifying and selecting their means of transport in the case of an emergency and saving money are also the essential components of birth preparedness and complication preparation.1
Maternal death due to pregnancy and childbirth has become a global problem. As evidence, there have been about 810 and 295,000 maternal deaths daily and annually worldwide, respectively. Despite much progress, maternal death is prevalent in low and lower-middle-income countries, since about 94% of maternal deaths occurring in these countries. In fact, about 66% of maternal deaths were in sub-Saharan Africa alone2. The maternal mortality ratio is therefore about 216 per 100,000 live births worldwide and 542 per 100,000 live births in Africa. As a result, the maternal mortality ratio in low-income countries is almost 29 times higher than in high-income countries.3 Ethiopia is one of the countries with a higher maternal mortality rate of 401/100,000 live births. In addition, nearly 14,000 women die each year as a result of childbirth-related causes, resulting in 19% of maternal mortality among women in the child-bearing age group.3 Despite trends in the use of antenatal care (ANC) increased to 74% in Ethiopia, just 43% of women have four or more ANC visits and only 48% of births were in the health facility.4 Besides, the studies revealed that only 32% of mothers were prepared for birth and its complications.5
Regarding birth complications, about 300 million women have undergone anemia, uterine prolapse, fistula, pelvic inflammatory disease, infertility, and neonatal effects such as stillbirth, preterm birth, restricted growth, as well as other problems globally.6,7 Similarly, up to 500,000 pregnant women can have short-term and/or long-term illnesses or injuries every year in Ethiopia due to pregnancy- and childbirth-related problems.8
Moreover, delays in women’s access to health care often add another dimensional aspect to maternal mortality and related problems. There are three major delays for women’s access to health care; the first step is delaying the decision to seek care and then delaying the arrival of care, followed by delays in receiving care. As a result, these three delays can be handled by the appropriate use of birth preparedness and complication readiness plan.9 On this basis, the current studies have shown that cultural beliefs, socio-demographic factors, inadequate health service and poor awareness about obstetrics danger signs and BP/CR have been associated with poor national BP/CR practice.5,9
The Sustainable Development Goals (SDGs) seek to reduce maternal mortality worldwide from 216 per 100,000 live births to less than 70 per 100,000 live births by 2030.10 The World Health Organization (WHO) has integrated birth preparedness and complication readiness as part of a focused ANC package, and Ethiopia has also introduced this intervention and addressed it in routine antenatal care.11 Despite many efforts to boost BP/CR practice, Ethiopia is one of the 60 countries that has not met the SDGs goal to reduce maternal death as expected yet,3 only one in three mothers has good BP/CR practice nationally.5
Although previous researches were conducted on the study area, they were merely institution-based studies and did not use a standardized measurement tool. In addition, they did not consider the role of husbands in the practice of in BP/CR and they are outdated studies as well. Therefore, this study was initiated in order to assess the magnitude of BP/CR and associated factors among recently delivered women in Mizan-Aman town, southwestern Ethiopia. This helps to narrow the information gap and to provide possible recommendations for health managers, professionals, and other stakeholders working in maternal and child health institutions.
Methods and Materials
Study Area and Period
The study was conducted between May 20 and June 20/2019 in the town of Mizan-Aman, located 561 km southwest of Addis Ababa. The city is administratively organized with 5 kebeles and has a total population of 49,590, of which 26,392 are male and 23,197 are female residents. 11, 554 female residents are also in the reproductive age group (15–49yr). It has one teaching hospital, one public health center, 10 private health institutions and 17 drug stores.
Study Design and Population
A community-based cross-section study was conducted. Mothers of infants less than one year of age who are permanent residents of Mizan-Aman town and willing to take part in the study were involved. Those who get serious medical illness, mental problems or unwilling to participate in this study were excluded.
Sampling Size
A single population proportion formula was employed to determine the sample size. The following assumptions were considered: 95% level of confidence, 5% margin of error as well as 23.3% of women estimated to have participated in birth preparedness in a similar study done in Jimma.12 Since the source of population was 1561, which is less than 10,000, the sample size was adjusted using a correction formula, 2 design effects were considered and by adding a 5% non-response rate, therefore, the final sample size became 491.
Sampling Procedure
A multi-stage sampling technique was employed since the town of Mizan-Aman has two administration sub-cities (Mizan sub-city and Aman sub-city) and five kebeles. Kebeles were considered to be the primary sample unit. Therefore, two kebeles from the Mizan sub-city and one kebele from the Aman sub-city were selected using the lottery method. And then proportional allocation to size was employed. Afterwards, a systematic random sampling technique was used to select the study subjects. After random selection of the first household with a woman who meets the eligibility criteria, subsequent households with women fulfilling the criteria were selected from every three houses until the desired sample size was reached in each kebele.
Operational Definitions
Birth preparedness and complication readiness have five intervention components: Identifying the place of the delivery, skilled birth attendant, blood donor, and means of transport during an emergency case as well as saving money that can be used during an emergency. Those women who practiced at least three of the five BP&CR components were deemed “prepared for birth and its complication”.1
Those women who mentioned at least three of the five BP&CR components were considered knowledgeable about BP&CR.1
Those women who mentioned at least two of the three key danger signs for pregnancy (vaginal bleeding, swollen hands/face, and blurred vision) were considered knowledgeable about key danger signs of pregnancy.1
Those women who mentioned at least three of the key four danger signs for labor/childbirth (severe vaginal bleeding, prolonged labor (>12huors), convulsion, and retained placenta) were considered knowledgeable about key danger signs of labor/childbirth.1
Those women who mentioned at least two of the three key danger signs for postpartum (severe vaginal bleeding, foul-smelling vaginal discharge, and high fever) were considered knowledgeable about the key danger signs of postpartum.1
Those husbands who followed at least three of the five BP&CR components were deemed “prepared for birth and its complication”.1
Data Collection and Analysis
The tool was adapted from JHPIEGO: Maternal and Neonatal Health program1 and translated into the local Amharic language. A structured questionnaire was used to collect data via a face-to-face interview. In order to ensure the quality of data, a pre-test was carried out in 5% of the sample size in Sheko town, and training was also provided for eight data collectors and two supervisors. The data were cleaned, coded, and entered into Epi Info version 3.5.3 and exported to SPSS version 25 statistical package for analysis. Descriptive statistics were computed to determine the magnitude of BP&CR practice. Furthermore, a bivariate logistic regression technique was done. Subsequently, those variables with p< 0.2 were moved to multivariate analysis and analyzed by a stepwise multivariate logistic regression technique to control the effects of confounding and to identify predictors of BP&CR practices. A P-value of <0.05 was considered as statistical significance at a 95% confidence interval.
Results
Socio-Demographic Characteristics of the Respondents
All study participants, i.e. those who gave birth in the last 12 months prior to the study were interviewed and reported a response rate of 100%. The majority of women, 193 (39.3%), were between 25 and 29 years of age, and the mean and standard deviation (±SD) of maternal age was 25.92 (±4.96). Of the total study participants, 474 (96.5%) were married, 279 (56.8%) had a family size of 4–6, and 200 (40.7%) were housewives by occupation. In addition, about 236 (48%) of women had primary education (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Mothers of Children Aged Less Than One Year in Mizan-Aman Town, Southwestern Ethiopia, 2019 (N=491) |
Obstetrics and Maternal Health Service Utilization Characteristics
Forty-five (9.2%) mothers had a history of stillbirth, and 32 (6.5%) mothers had a history of one stillbirth in number. The majority of mothers, 304 (61.6%) were multipara. A total of 476 (96.9%) women attended the ANC and 471 (95.9%) had BP/CR counseling at the ANC clinic during their pregnancy. Besides, 467 (95.1%) of the study participants delivered their child to the government health facility, assisted by a health professional, while 359 (73.1%) gave birth through normal spontaneous delivery (Table 2).
 |
Table 2 Obstetrics and Maternal Health Service Utilization Characteristics Among Mothers of Children Aged Less Than One Year in Mizan-Aman Town, Southwestern Ethiopia, 2019 (N=491) |
With respect to obstetrics health problem experience, 60 (12.2%) of respondents reported that they had encountered health problems during pregnancy. On the other hand, 52 (10.6%) and 45 (9.2%) of the respondents reported that their health problem was during childbirth, and postpartum periods, respectively. Moreover, the most common health problems experienced were; 38 (7.7%) blurring of vision during pregnancy, 33 (6.7%) prolonged labor during labor/childbirth and 32 (6.5%) severe vaginal bleeding during the postpartum period (Table 3).
 |
Table 3 Obstetrics Health Problem Experienced Characteristics Among Mothers of Children Aged Less Than One Year in Mizan-Aman Town, Southwestern Ethiopia, 2019 (N=491) |
Knowledge of Obstetrics Danger Sings
With regard to obstetrics danger signs, 104 (21.2%), 65 (13.2%), and 61 (12.4%) of the respondents mentioned at least three key obstetric danger signs during pregnancy, childbirth and the postpartum period, respectively (Table 4). Besides, 420 (85.5%), 376 (76.6%), and 431 (87.8%) of the respondents spontaneously mentioned severe vaginal bleeding as a danger sign during pregnancy, labor/childbirth and postpartum, respectively.
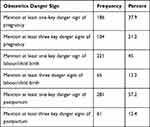 |
Table 4 Knowledge of Obstetrics Danger Signs Among Mothers of Children Aged Less Than One Year in Mizan-Aman Town, Southwestern Ethiopia, 2019 (N=491) |
Knowledge of Respondents About Prepared for Birth and Its Complication
According to the study, 360 (73.3%) of the study participants described that they have heard the term birth preparedness and complication readiness, of which 238 (48.5%) of the respondents’ sources of information were health professionals.
With respect to BP/CR knowledge, 418 (85.1%), 264 (53.8%), 259 (52.7%), 82 (16.7%) and 36 (7.3%) of respondents indicated that it is useful to identify the place of delivery, to identify skilled providers, to save money, to identify means of transport and blood donors, respectively. Therefore, 132 (26.9%) of the respondents were knowledgeable about BP/CR according to the measurement tool (Figure 1).
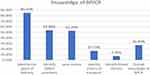 |
Figure 1 Knowledge of BP/CR among mothers of children’s less than one year of age, Mizan-Aman town, southwestern Ethiopia, 2019 (N=491). |
Practice of Birth Preparedness and Complication Readiness
The practice of birth preparedness and complication preparedness among the study participants was found to be 22.2%. The majority of respondents, 477 (97.1%), indicated that they identified the place of delivery, while 400 (81.5%) of respondents identified a skilled provider. In addition, 169 (34.4%) of them saved money. On the contrary, only 66 (13.4%) of the participants identified means of transport for their delivery and emergency situations, and about 16 (3.3%) of the participants identified blood donors when needed (Table 5).
 |
Table 5 Status of Birth Preparedness and Complication Readiness Practice Among Mothers of Children Aged Less Than One Year in Mizan-Aman Town, Southwestern Ethiopia, 2019 (N=491) |
Husband Involvement of Birth Preparedness and Complication Readiness
Three hundred and fifty-four (72.1%) husbands were prepared for birth and its complication. The majority (86.8%) of respondents reported that their husbands had participated in the identification of a place of delivery. In addition, only 67 (13.6%) of the respondents indicated that their husbands had engaged in the arrangement of blood donor. The majority of respondents reported that they were accompanied by their husbands at the ANC clinic,382 (77.8%), and in the labor room, 419 (85.3%). With regard to medical decision-making; the majority of 460 (93.7%) of respondents indicated that their medical decisions were taken by both themselves and their husbands. On the other hand, 28 (5.7%) of the respondents revealed that their medical decisions are taken by themselves only (Figure 2).
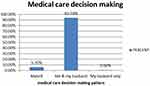 |
Figure 2 Medical care decision-making status among mothers of children’s less than one year of age, Mizan-Aman town, southwestern Ethiopia, 2019 (N=491). |
Factors Associated with Birth Preparedness and Complication Readiness Practice
According to the bivariate logistic regression analysis, the following study variables were significantly associated with BP/CR practice (p < 0.05): mothers who had primary education, mother’s income between 500 and 1000 ETH Birr/month, infants birth order 4–6, mothers who had a history of stillbirth, mothers who did know the term BP/CR from a health professional, and mothers who spontaneously mentioned at least one and two pregnancy danger signs and at least two postpartum danger signs.
In addition, the variables with p<0.2 from the bivariate analysis were shifted and analyzed by multivariate analysis. Accordingly, those mothers who had a history of stillbirth, mothers who knew the term BP/CR from their friends, mothers who knew pregnancy danger signs, mothers who mentioned at least two postpartum danger signs, and those with an income between 1001 and 1500 Birr/month were important predictors of birth preparedness and complication readiness practice. Likewise, infants birth order 4–6 and housewife mother by occupation were found to protector factors for BP/CR practice (Table 6).
 |
Table 6 Birth Preparedness and Complication Readiness Practices and Associated Factors Among Mothers of Children Aged Less Than 12 Months in Mizan-Aman Town, Southwestern Ethiopia, 2019 |
The odds of birth preparedness and complication readiness of mother’s income between 1001 and 1500 Birr/month was almost three times higher (AOR=2.679, 95% CI: 1.096, 6.552) than those mothers’ income >1500 Birr/month. Furthermore, mothers who had a history of stillbirth were nearly four times (AOR=3.646, 95% CI: 1.722, 5.653) more likely to be well prepared for BP/CR as compared to mothers who had no history of stillbirth. The odds of birth preparedness and complication readiness of mothers who knew the term BPCR from their friends were three times higher (AOR=3.046, 95% CI: 1.044, 8.889) than those mothers who did know the term BP/CR from their mothers. Mothers who mentioned at least two postpartum danger signs were nearly four times (AOR=3.571, 95% CI: 1.511, 8.443) more likely to be well prepared for BP/CR as compared to mothers who mentioned all three postpartum danger signs. Finally, the odds of birth preparedness and complication readiness of mothers who knew pregnancy danger signs were nearly three times higher (AOR=2.82, 95% CI: 1.211, 6.565) than those mothers who did not (Table 6).
Discussion
This study revealed that the practice of birth preparedness and complication preparedness was found to be 22.2%, suggesting that birth preparedness was less practiced in the study area. The finding is comparable with other studies conducted in the Jimma zone and Adigrat Town, 23.3% and 22.1%, respectively.12,13 However, the practice of BP/CR in this study was higher than the studies in Arsi zone (16.5%) and Duguna Fango district (18.3%).14,15 The difference might be due to fact that our study subjects were merely urban-dwelling women who are expected to have better information regarding the potential pregnancy-related complication and the ideal place where to give birth. Whereas the mentioned studies have further included rural women who may be far less aware of reproductive health-related services.
Other studies in Addis Ababa, Dire-Dawa, Nigeria, and India (56.3%, 54.7%, 64.4%, and 62.4%, respectively) showed a higher BP/CR rate than our study has shown (22.2%).16–19 The difference might be due to the population character, the study subjects were pregnant women, they might mention the birth plan rather than what they actually did. The other possible explanation may be that the above studies have been conducted in a well-developed city where people are presumed to have adequate information and good access to health services.
The study found that mothers with income levels between 1001 and 1500 ETH Birr/month were almost three times (AOR=2.679, 95% CI: 1.096, 6.552), more likely planed the places where they should give birth and so did ready for any potential complications too. Thus, the finding is consistent with studies conducted in India,20 Arsi Robe woreda, Ethiopia,14 and Ogbomosho Nigeria.21 The majority of our respondents were under the category of middle socio-economic class, earning between 500 and 1500 Birr/month. These two mentioned reasons might have a positive impact on women’s medical decision-making ability and utilization of health services provided during pregnancy, delivery, and thereafter, antenatal care services.
Mothers who had a history of stillbirth were nearly four times (AOR=3.646, 95% CI: 1.722, 5.653), more likely to plan where to give birth and got ready for any potential complication which may happen then. The finding is concordant with the study findings done in Adigrat and North Eastern Ethiopia.13,22 This could be the fact that those women who have experienced stillbirth may probably anticipate similar phenomena to their future pregnancies. Hence, these women are expected to seek frequent medical advice than pregnant women who had no previous history of stillbirth which in turn drives them to be prepared for birth and avert any complication.
Mothers who stated at least two postpartum danger signs were 3.571 (AOR: 95% CI: 1.511, 8.443) more likely to be prepared for BP/CR. This is consistent with studies in Nepal,23 Uganda24 and Arsi robe.14 The reason might be due to the fact that mothers who are informed about postpartum complications would be concerned more about the safety/survival of themselves and their own offspring too. Furthermore, a woman who has better knowledge of postpartum danger signs will possibly be prepared to avert the worst before it happens. It also helps her to ensure the safety and wellbeing of herself and her child’s health. This, in turn, leads to the need for medical advice and assistance from healthcare providers. This indicates that a better understanding of postpartum danger signs would have a major positive impact on BP/CR practice.
Those participants who knew pregnancy danger signs were nearly three times (AOR=2.82, 95% CI: 1.211, 6.565), more likely to be well prepared for BP/CR. This is also found in line with studies in Abeshige district, Gurage district, and Goba woreda.25,26 This could be due to the fact that recognizing the danger signs in pregnancy would lead women to seek solutions from medical staff and be willing to take some better action. Knowing the pregnancy danger signs is a key step in recognition of the complication. This, in turn, leads to the awareness of the need for medical care, the decision to seek treatment and to behave where it needs to obtain emergency care from a skilled provider. This suggested that it is important for BP/CR to have a pre-informed knowledge of pregnancy danger signs.
Strength and Limitation of the Study
This study was community-based with the maximum possible sample size inclusion upon which inference has been made. We have also used a standardized, expert reviewed, and pretested data collection tool, but it shares the specific limitations of cross-sectional study design.
Conclusion and Recommendation
The magnitude of BP/CR practice in the study area has been found to be less practiced. The majority of women planned the places where they gave birth, identified the skilled birth attendants, and then saved money for any emergency supplies. Mother’s income between 1001 and 1500 Birr/month, mothers of the infant’s birth order 4–6, housewife mother by occupation, mothers with a history of stillbirth, mothers who knew the term BP/CR from their friends, mothers who knew pregnancy danger sign and mothers who stated at least two postpartum danger signs were important predictors of BP/CR practice. Promoting the BP/CR Intensive health education program and growing mothers to mother’s/peer education at the community level and paying particular attention to; multipara, with lower incomes and housewife mothers during the ANC visit at the facility level is recommended.
Abbreviations
AOR, adjusted odds ratio; ANC, antenatal care; BPCR, birth preparedness and complication readiness; JHPIEGO, John Hopkins Program for International Education in Gynecology and Obstetrics; SDG, sustainable developmental growth; WHO, World Health Organization.
Data-Sharing Statement
All data generated or analyzed during this study are included in the manuscript and are also available from the corresponding author upon request.
Ethical Approval and Consent to Participate
The study protocol was evaluated and approved by Wollo University College of Medicine and Health Science with reference no_(WU/CMHS/281/2019) and ethical clearance was obtained. Permission letters were also obtained from Mizan-Aman town health unit and respective kebeles. After giving a clear and deep understanding of the aim of the study, written consent was obtained from each respondent before the interview is conducted. In addition, prior to interviews with participants under 18 years of age, written informed consent was obtained from their parent or legal guardian. Any study participant who was found to be less practiced and informed about BP/CR was advised and referred to the ANC clinic for further assistance. Moreover, this study was conducted in compliance with the Declaration of Helsinki. Mothers who are unwilling were exempted from the study. Anonymous data were taken and the confidentiality of participant’s information was secured.
Acknowledgment
The authors would like to thank Mizan-Aman town health unit staff and community health workers for their kind cooperation. We are also thankful to data collectors and the study participants.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Wollo University sponsored financial issue to accomplish this work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Maternal JH. Neonatal Health: Monitoring Birth Preparedness and Complication Readiness, Tools and Indicators for maternal and Newborn Health. Johns Hopkins, Bloomberg school of Public Health. Center for communication programs, Family Care International; 2004.
2. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. 2019.
3. World Health Organization. World Health Statistics Overview 2019: Monitoring Health for the SDGs, Sustainable Development Goals. World Health Organization; 2019.
4. Ethiopian public health institute, Federal Ministry of Health Ethiopia, The DHS program ICF. Mini Demographic and Health Survey. 2019.
5. Berhe AK, Muche AA, Fekadu GA, Kassa GM. Birth preparedness and complication readiness among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2018;15(1):182. doi:10.1186/s12978-018-0624-2
6. Lincetto O, Mothebesoane-Anoh S, Gomex P, Munjanja S. Opportunities for Africa’s Newborns. Antenatal Care. World Health Organisation; 2018.
7. Basic Emergency Obstetric & Newborn Care (BEmONC). Training Manual Federal Democratic Republic of Ethiopia Ministry of Health. 2013.
8. Federal ministry of health safe motherhood program, Ethiopia. 2010.
9. Moore M, Copeland R, Chege I, Pido D, Griffiths M. A Behavior Change Approach to Investigating Factors Influencing Women’s Use of Skilled Care in Homa Bay District. Washington DC: Kenya, the CHANGE Project; 2002:105–108.
10. United Nations. Time for Global Action. Sustainable Development Goals. New York: United Nations; 2015.
11. World Health Organization (WHO). Birth and Emergency Preparedness in Antenatal Care: Integrated Management of Pregnancy and Childbirth (IMPAC). Geneva, Swaziland: WHO Department of Making Pregnancy Safer; 2006.
12. Debelew GT, Afework MF, Yalew AW. Factors affecting birth preparedness and complication readiness in Jimma Zone, Southwest Ethiopia: a multilevel analysis. Pan Afr Med J. 2014;19:19. doi:10.11604/pamj.2014.19.272.4244
13. Hiluf M, Fantahun M. Birth preparedness and complication readiness among women in Adigrat town, north Ethiopia. Ethiop J Health Dev. 2008;22(1):14–20. doi:10.4314/ejhd.v22i1.10057
14. Kaso M, Addisse M. Birth preparedness and complication readiness in Robe Woreda, Arsi Zone, Oromia Region, Central Ethiopia: a cross-sectional study. Reprod Health. 2014;11(1):55. doi:10.1186/1742-4755-11-55
15. Gebre M, Gebremariam A, Abebe TA, Leone T. Birth preparedness and complication readiness among pregnant women in Duguna Fango District, Wolayta Zone, Ethiopia. PLoS One. 2015;10(9):e0137570. doi:10.1371/journal.pone.0137570
16. Musa A, Amano A. Determinants of birth preparedness and complication readiness among pregnant woman attending antenatal care at Dilchora Referral Hospital, Dire Dawa City, East Ethiopia. Gynecol Obstet. 2016;6(2):356. doi:10.4172/2161-0932.1000356
17. Envuladu EA, Zoakah AI. Assessment of the birth and emergency preparedness level of pregnant women attending antenatal care in a primary health care centre in Jos, Plateau State, Nigeria. Int J Basic Appl Innov Res. 2014;3(1):2–7.
18. Saha R. The status of birth preparedness and complication readiness among rural Indian mothers. Int J Public Health Res. 2014;4(2):510–518.
19. Tiku S. Awareness on birth preparedness and complication readiness among antenatal care clients in federal police referral Hospital Addis Ababa, Ethiopia. Am J Health Res. 2015;3(6):362–367. doi:10.11648/j.ajhr.20150306.18
20. Idowu A, Deji SA, Aremu OA, Bojuwoye OM, Ofakunrin AD. Birth preparedness and complication readiness among women attending antenatal clinics in Ogbomoso, South West, Nigeria. Int J MCH AIDS. 2015;4(1):47–56. doi:10.21106/ijma.55
21. Kaur A, Kaur M, Kaur R. Birth preparedness among antenatal mothers. Nurs Midwifery Res. 2015;11(4):153.
22. Bitew Y, Awoke W, Chekol S. Birth preparedness and complication readiness practice and associated factors among pregnant women, Northwest Ethiopia. Int Sch Res Notices. 2016;2016:2016. doi:10.1155/2016/8727365
23. Subedi S. Knowledge and practice on birth preparedness and complication readiness among pregnant women in selected ward of Biratnagar municipality, Nepal. Tribhuvan Univ J. 2019;33(1):53–66. doi:10.3126/tuj.v33i1.28682
24. Kabakyenga JK, Östergren PO, Turyakira E, Pettersson KO. Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health. 2011;8(1):33. doi:10.1186/1742-4755-8-33
25. Zepre K, Kaba M. Birth preparedness and complication readiness among rural women of reproductive age in Abeshige district, Guraghe zone, SNNPR, Ethiopia. Int J Women's Health. 2017;9:11. doi:10.2147/IJWH.S111769
26. Markos D, Bogale D. Birth preparedness and complication readiness among women of child bearing age group in Goba woreda, Oromia region, Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):282. doi:10.1186/1471-2393-14-282
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
