Back to Journals » Open Access Journal of Sports Medicine » Volume 9
Bilateral femoroacetabular impingement syndrome managed with different approaches: a case report
Authors Öhlin A, Ayeni OR, Swärd L, Karlsson J, Sansone M
Received 19 January 2018
Accepted for publication 24 April 2018
Published 21 September 2018 Volume 2018:9 Pages 215—220
DOI https://doi.org/10.2147/OAJSM.S162304
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Andreas Imhoff

Axel Öhlin,1 Olufemi R Ayeni,2 Leif Swärd,1 Jón Karlsson,1 Mikael Sansone1
1Department of Orthopaedics, University of Gothenburg, Gothenburg, Sweden; 2Division of Orthopaedic Surgery, Department of Surgery, McMaster University, Hamilton, ON, Canada
Purpose: The purpose of this case report is to present the successful management of symptomatic bilateral femoroacetabular impingement (FAI) syndrome in a patient who underwent surgical treatment on one side and non-surgical treatment on the other side.
Methods: We evaluated the treatment outcome of a young female presenting with bilateral FAI syndrome of cam morphology. A follow-up was performed at 5 years following surgical treatment on the right hip and 2 years following non-surgical treatment on the left hip. The evaluation included a clinical examination, patient-reported outcome measurements (PROM), plain radiographs, and magnetic resonance imaging (MRI).
Results: The patient experienced subjective improvements bilaterally. The clinical examination revealed differences in range of motion between the surgically treated and the non-surgically treated sides, with internal rotation differing the most (20° vs almost 0°). Flexion was, however, the same on both sides (125°). The PROM results were satisfactory on both sides, with slightly better results for the surgically treated side (the short version of the International Hip Outcome Tool [iHOT-12]: 96.9 vs 90, the Copenhagen Hip and Groin Outcome Score [HAGOS]: 90–100 vs 65–100). On the surgically treated side, the alpha angle decreased by 19° postoperatively. An MRI did not reveal any injury to the cartilage or labrum on either side.
Conclusion: This patient with bilateral FAI syndrome treated with arthroscopic surgery on one side and physiotherapy together with reduced physical activity on the other side, presented with good results bilaterally at follow-up.
Keywords: arthroscopy, physiotherapy, outcome, comparison
Introduction
Femoroacetabular impingement (FAI) syndrome is a cause of hip pain and reduced range of motion (ROM) in the young adult. FAI syndrome is due to bony abnormalities, causing acetabular over-coverage (pincer morphology) or femoral head-neck asphericity (cam morphology).1 A combination of the two types is also known.2 By causing abnormal mechanical stress with motion in the hip joint, FAI syndrome has the potential to cause damage to the soft tissue of the hip joint.3 It is thought that cartilage overload can cause the degeneration of the articular surface that leads to osteoarthritis (OA). The amount of stress the articular surface is able to tolerate and how rapidly OA may develop is, however, less well understood.4 Despite this gap in knowledge, FAI syndrome has been proposed as a cause of OA.1,5–7
In a study of presumed active military personnel with complaints of hip pain in general, 87% demonstrated radiological findings consistent with FAI, but the rate of a clinical diagnosis of FAI syndrome was not reported.8 For Swiss military recruits with limited hip ROM, the prevalence of imaging findings of FAI was 48%, compared with 24% prevalence for all asymptomatic recruits, regardless of hip ROM.9 Kapron et al later reported a correlation between internal rotation and radiographic measurements of cam morphology and also that subtle anatomic features were able to dictate underlying hip biomechanics, including reduced ROM in patients with FAI.10,11 The prevalence of imaging findings of FAI among asymptomatic young adults has been reported to be 14%, while it is as high as 95% among asymptomatic competitive athletes.12,13
Surgical intervention for FAI syndrome aims to restore normal hip anatomy and repair damaged soft tissue.14 Several studies have reported good results following the arthroscopic treatment of FAI syndrome in both the short to medium term and at longer term.15–17 Non-surgical treatment in the form of physiotherapy does not alter the anatomy of the hip but instead aims to adapt to a safe, pain-free ROM.18 Contrasting results have been reported in terms of the efficiency of non-surgical treatment, ranging from favorable to less favorable.18–21
The main purpose of this case report is to present the successful management of bilateral FAI syndrome in a patient who underwent different treatment regimens on each side.
Case report
Ethical approval for this study was granted by the Regional Ethical Review Board in Gothenburg at the Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden (registration number EPN 071-12) and is in accordance with the Helsinki Declaration. Written informed consent to have the case details and images published was obtained from the patient.
A 31-year-old female physiotherapist presented to an orthopedic surgeon in December 2009 with an 18-month history of right-sided hip and groin pain. The symptoms had started at the 70 km mark during a 100 km bicycle race. A clinical examination was performed with the patient in the supine position. Internal rotation with the hip flexed at 90° was reduced by 15° compared with the contralateral side and the anterior hip impingement test was positive for recreating symptoms.22
As the patient was pregnant at the time of evaluation, it was decided to defer all radiographic evaluations. During the first 16 weeks post-partum, the patient’s activity level was limited to short walks of under 10 minutes due to non-orthopedic reasons. After this period, the patient described a partial improvement and a new clinical examination revealed a slight improvement in internal rotation of 10° with the hip flexed at 90°.
Plain radiographs of the right hip in the anterior-posterior view (modified Dunn projection, hip flexed 45° and abducted 20°) revealed an alpha angle of 60° compared with 50° for the left hip.23 The center-edge (CE) angle was 30° for the right hip and 32° for the left hip. The cross-over sign and ischial spine sign were negative bilaterally. Radiographs are shown in Figures 1 and 2. The joint space was 5 mm in the central weight-bearing zone and the Tönnis grade was 0 for the right hip.
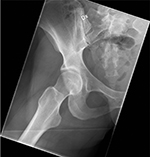  | Figure 1 Right hip, preoperatively. |
  | Figure 2 Left hip, pretreatment and before debut of symptoms in the left hip. |
After 18 months of non-surgical management including failed physiotherapy, the patient expressed a desire to improve. The decision was made to treat the patient surgically and the cam morphology was resected using an arthroscopic approach.
A supine, two-portal approach was used. The capsule was opened with a longitudinal incision, avoiding interportal capsulotomy and using a ballooning technique for visualization. Visually, the joint was inspected and found to be normal. Osteochondroplasty was then performed using a burr under fluoroscopic guidance and dynamic hip rotation under visualization to confirm a good result. The alpha angle was reduced 19°; a postoperative radiograph is shown in Figure 3. No thrombosis prophylaxis and no antibiotic prophylaxis was used. The postoperative instructions consisted of unloading with crutches for 4 weeks, 14 days of non-steroidal anti-inflammatory drugs (NSAIDs), and physiotherapy.24 Physiotherapy was initiated during the first 4 weeks and included daily active hip movements without a load and, after 4 weeks, the load was first increased to body weight, followed by a stepwise increase with respect to what was tolerated by the patient. The total postoperative physiotherapy period was 6 months.
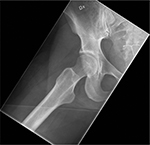  | Figure 3 Right hip, postoperatively. |
At the return visit 2 weeks postoperatively, as measured and recorded by the same surgeon, the internal rotation of the hip with the hip flexed at 90° had improved slightly to 30°, compared with 20–25° preoperatively. Postoperatively, the patient experienced no pain in the hip. A few months after the surgery, she was able to sit in a car for a drive of about 1,000 km without pain, which had been impossible before surgery, and, nearly 3 years after surgery, she completed a running competition of 90 km with no pain. However, the patient experienced a slight reduction in strength in the treated hip compared with the untreated hip when running more than 30 km. The weakness was described as general and not specified to a single muscle group. About 3 years postoperatively, the patient started to develop pain in the previously unaffected left side. The symptoms were now limited to pain on terminal flexion. A clinical examination revealed that internal rotation with the hip flexed at 90° was reduced to 0° from the initial 30° before the onset of symptoms. The alpha angle, CE angle, cross-over sign, and ischial spine sign were unchanged compared with before the onset of symptoms in the left hip. The joint space was 4.7 mm in the central weight-bearing zone and the Tönnis grade was 0. The patient underwent non-surgical treatment for the left hip in the form of physiotherapy aimed mainly at strengthening and stabilizing the hip girdle in a pain-free ROM. Physiotherapy consisted of exercises for core, hip, and thigh strengthening. The program was performed three times a week for the first 6 months and then in periods based on the patient’s needs. The patient experienced a temporary improvement with intermittent pain with intensive sporting activity. The patient was examined again, now more than 6 years after the index examination. On the left side, the patient was able to flex the hip to 120° and the internal rotation with the hip flexed at 90° was reduced by 30° compared with the initial assessment. Despite this reduction in function, the patient decided not to undergo surgical treatment of the left hip and instead agreed to exclude provocative exercises such as cycling and squats.
Post-intervention final follow-up
The detailed follow-up was completed 5 years after arthroscopic treatment of the right hip and 2 years following the initiation of non-surgical treatment of the left hip. The right hip was still pain-free with a slight subjective reduction in strength. The left hip was in the same state since the onset of symptoms, with pain in conjunction with provocative exercises, and had neither improved nor worsened during non-surgical treatment consisting of physiotherapy and activity modification. The patient was still capable of performing 90 km runs. Flexion in the hip joint was 125° bilaterally (the patient was in the supine position with a stable pelvis but not rigidly fixed). Internal rotation with the hip flexed at 90° was 20° for the right hip and almost 0° for the left hip. External rotation with the hip flexed at 90° was 45° for the right hip and 60° for the left hip. The flexion, abduction, and external rotation (FABER) test was 20 cm (distance between the examination table and the lateral side of the knee) or 25° for the right hip and 25 cm or 20° for the left hip. No pain was present in either hip during the FABER test. The results of the short version of the International Hip Outcome Tool (iHOT-12), the Copenhagen Hip and Groin Outcome Score (HAGOS), and EuroQol-5 Dimensions (EQ-5D) are presented in Table 1.25,26 The patient scored seven on the Hip Sports Activity Scale (HSAS) and stated that it had not changed from before the onset of pain to follow-up.27 On plain radiographs in the anterior-posterior view (modified Dunn projection), there was no sign of further osteophytes and the alpha angle was still 41° for the right hip and 50° for the left hip. The CE angle, cross-over sign, and ischial spine sign were unchanged bilaterally. The joint space in the central weight-bearing zone was still 5 mm and 4.7 mm for the right and left hip, respectively. The Tönnis grade was 0 bilaterally. Magnetic resonance imaging (MRI) (3 Tesla) did not reveal any injury to the cartilage or labrum in either the right or the left hip.
Discussion
This case report gives us an opportunity to compare surgical treatment followed by postoperative physiotherapy with non-surgical treatment only of FAI syndrome in a single patient. Non-surgical treatment did not improve or worsen either the subjective symptoms of pain or internal rotation with the hip flexed at 90°. Surgical treatment reduced the alpha angle by 19°, reduced the patient’s subjective symptoms of pain, and increased internal rotation with the hip flexed at 90° by 5°. The results of the internal hip rotation must be evaluated with caution due to the risk of significant intra-observer variation. The patient-reported outcome measurements (PROM) data at follow-up suggested good function bilaterally, with slightly higher scores for the surgically treated hip. An MRI did not reveal any injury to the cartilage in either hip. In terms of the MRI, T1rho or delayed gadolinium-enhanced MRI of cartilage (DGEMRIC) could have added more information about the status of the cartilage; unfortunately, this was not available at our institution.
The strengths of the presented case report are the opportunity to compare surgical treatment and non-surgical treatment in the same patient, as well as a long follow-up period for the surgically treated hip and the use of PROM validated for use in a young and active population. The limitations in the present case report are the lack of pre-treatment PROM data for both hips, which limits the opportunity to draw any firm conclusions about the baseline condition and amount of improvement. The different alpha angles for the two hips, 60° for the surgically treated side and 50° for the non-surgically treated side, also limit the opportunity for comparison, as we are unable to exclude the possibility that different degrees of alpha angle are more or less suited to different treatment regimens. No gait analysis was performed and it is therefore possible that the patient was unloading one hip, generating a false favorable result for the other hip. The different follow-up periods, 5 years and 2 years, respectively, also impair the potential for comparison. As the treatment for the two hips was performed in a staged manner, it is possible that the patient’s expectations were different for the surgically and the non-surgically treated sides and, according to Mannion et al, the fulfillment of expectations might influence the effectiveness of treatment.28 However, this situation does not differ from staged bilateral treatment of the same type. A single case study also limits the opportunity to make any generalization of the results. It is worth mentioning that both treatment regimens included physiotherapy, but the postoperative physiotherapy was mainly aimed at gradually increasing the load on the hip, while the physiotherapy for the non-surgically treated hip was aimed at strengthening and stabilizing the hip girdle in pain-free ROM. Peri-operatively, there were no macroscopic findings of injury to the cartilage or the labrum. With pain from the hip, this is, however, unlikely to be true and highlights the difficulty involved in assessing less extensive soft-tissue damage visually.
Several studies have reported good results following the arthroscopic treatment of FAI syndrome in both the short and medium term but also at longer follow-up.15–17 The non-operative treatment regimen is less well studied and there is no consensus in terms of the most favorable non-surgical treatment. Emara et al reported the results of the non-surgical treatment of mild FAI syndrome (mean alpha angle 47°), among 37 patients, where four finally underwent surgery and the remaining 33 patients experienced both a decrease in the visual analog scale score and an improvement in the Harris Hip Score following physiotherapy and activity modification.18 Similar positive results have been reported by Feeley et al, who studied National Football League players, where eight of eight players successfully managed with non-surgical treatment were able to return to play.19 Contrasting results have been published by Hunt et al, who reported that, of 18 patients undergoing physiotherapy and activity modifications, eleven patients eventually underwent surgical treatment as they did not experience any temporary relief or improvement in function.20 Moreover, Jäger et al reported that nine of nine patients with FAI syndrome treated with physiotherapy and NSAIDs continued to experience significant pain and hip dysfunction.21
This patient’s history illustrates FAI syndrome, treated both surgically and non-surgically. It has been shown that the surgical treatment of FAI syndrome is able to produce improvements in terms of symptoms, physical activity level, and quality of life.16 Improvements after treatment can also be attributed to a decrease in physical activity which this patient reported after the start of symptoms in the left hip. We maintain that it is important to understand this when discussing different treatment options with patients. Since it is as yet unknown whether surgical treatment affects the onset or progression of OA, only symptoms or expected symptoms may guide the surgical decision. Patients wishing to maintain their physical activity level may have a greater opportunity to do this after surgical treatment, whereas non-surgical treatment may be a sufficient and a good option when lifestyle changes, especially including activity modification, are possible.
To better evaluate the efficacy of the non-surgical treatment of FAI syndrome, there is a need for more trials to compare the surgical and non-surgical treatment of FAI syndrome.29,30 To date, there are a few registered randomized controlled trials including both non-surgical treatment and sham surgery as controls.31–33
Conclusion
This patient with bilateral FAI syndrome treated with arthroscopic surgery on one side and physiotherapy together with reduced physical activity on the other side presented good overall results bilaterally at follow-up.
Disclosure
The authors report no conflicts of interest in this work.
References
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. | ||
Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. | ||
Beck M, Kalhor M, Leunig M, Ganz K. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. | ||
Buckwalter JA, Martin JA, Brown TD. Perspectives on chondrocyte mechanobiology and osteoarthritis. Biorheology. 2006;43(3,4):603–609. | ||
Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. | ||
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;(418):67–73. | ||
Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M. Femoroacetabular Impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2003;21 Suppl 1:S7-S15. | ||
Ochoa LM, Dawson L, Patzkowski JC, Hsu JR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res. 2010;468(10):2710–2714. | ||
Reichenbach S, Juni P, Werlen S, et al. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken). 2010;62(9):1319–1327. | ||
Kapron AL, Anderson AE, Peters CL, et al. Hip internal rotation is correlated to radiographic findings of cam femoroacetabular impingement in collegiate football players. Arthroscopy. 2012;28(11):1661–1670. | ||
Kapron AL, Aoki SK, Peters CL, Anderson AE. Subject-specific patterns of femur-labrum contact are complex and vary in asymptomatic hips and hips with femoroacetabular impingement. Clin Orthop Relat Res. 2014;472(12):3912–3922. | ||
Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. | ||
Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93(19):e111(1–10). | ||
Sansone M, Ahlden M, Jonasson P, et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):774–780. | ||
Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54–59. | ||
Sansone M, Ahldén M, Jonasson P, et al. Outcome after hip arthroscopy for femoroacetabular impingement in 289 patients with minimum 2-year follow-up. Scand J Med Sci Sports. 2017;27(2):230–235. | ||
Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39 Suppl:S7-S13. | ||
Emara K, Samir W, Motasem el H, Ghafar K. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong). 2011;19(1):41–45. | ||
Feeley BT, Powell JW, Muller MS, Barnes RP, Warren RF, Kelly BT. Hip injuries and labral tears in the national football league. Am J Sports Med. 2008;36(11):2187–2195. | ||
Hunt D, Prather H, Harris Hayes M, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM R. 2012;4(7):479–487. | ||
Jäger M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9(3):256–263. | ||
Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423–429. | ||
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. | ||
Beckmann JT, Wylie JD, Kapron AL, Hanson JA, Maak TG, Aoki SK. The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. 2014;42(6):1359–1364. | ||
Jonasson P, Baranto A, Karlsson J, et al. A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement: cross-cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):826–834. | ||
Thomee R, Jonasson P, Thorborg K, et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):835–842. | ||
Naal FD, Miozzari HH, Kelly BT, Magennis EM, Leunig M, Noetzli HP. The Hip Sports Activity Scale (HSAS) for patients with femoroacetabular impingement. Hip Int. 2013;23(2):204–211. | ||
Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Fulfilment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthritis Cartilage. 2013;21(1):44–50 | ||
Wall PD, Brown JS, Parsons N, Buchbinder R, Costa ML, Griffin D. Surgery for treating hip impingement (femoroacetabular impingement). Cochrane Database Syst Rev. 2014;(9):CD010796. | ||
Wall PD, Fernandez M, Griffin DR, Foster NE. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R. 2013;5(5):418–426. | ||
Griffin DR, Dickenson EJ, Wall PD, et al. Protocol for a multicentre, parallel-arm, 12-month, randomised, controlled trial of arthroscopic surgery versus conservative care for femoroacetabular impingement syndrome (FASHIoN). BMJ Open. 2016;6(8):e012453. | ||
Palmer AJ, Ayyar-Gupta V, Dutton SJ, et al. Protocol for the Femoroacetabular Impingement Trial (FAIT): a multi-center randomised controlled trial comparing surgical and non-surgical management of femoroacetabular impingement. Bone Joint Res. 2014;3(11):321–327. | ||
FIRST Investigators. A multi-centre randomized controlled trial comparing arthroscopic osteochondroplasty and lavage with arthroscopic lavage alone on patient important outcomes and quality of life in the treatment of young adult (18–50) femoroacetabular impingement. BMC Musculoskelet Disord. 2015;16:64. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.