Back to Journals » OncoTargets and Therapy » Volume 9
β-Elemene treatment of glioblastoma: a single-center retrospective study
Authors Ma C, Zhou W, Yan Z, Qu M, Bu X
Received 27 August 2016
Accepted for publication 1 October 2016
Published 12 December 2016 Volume 2016:9 Pages 7521—7526
DOI https://doi.org/10.2147/OTT.S120854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samir Farghaly
Chunxiao Ma, Wei Zhou, Zhaoyue Yan, Mingqi Qu, Xingyao Bu
Department of Neurosurgery, Henan Provincial People’s Hospital, Zhengzhou, People’s Republic of China
Abstract: Glioblastoma (GBM) is the most common primary malignancy in the central nervous system. In this study, we investigated the therapeutic effects of β-elemene (ELE) treatment in patients with newly diagnosed GBM who received concomitant chemoradiotherapy and adjuvant chemotherapy with temozolomide. Our results indicated that compared with control, patients who received ELE showed significantly longer median progression-free survival (PFS) (8 months vs 11 months; P<0.001) and overall survival (OS) (18 months vs 21 months; P<0.001). Despite the O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status, ELE treatment could significantly prolong the PFS (P=0.038) and OS (P=0.016). In multivariate analysis, ELE was a significant prognostic factor for PFS (hazard ratio [HR], 0.34; 95% confidence interval [95% CI]: 0.15–0.62; P=0.011) and OS (HR, 0.31; 95% CI: 0.14–0.69; P=0.006). Furthermore, ELE could significantly reduce the hematologic toxicities induced by chemoradiotherapy. In conclusion, ELE might provide a survival benefit in patients with GBM. Further study for verification might be needed.
Keywords: glioblastoma, chemoradiotherapy, temozolomide, β-elemene
Introduction
Glioblastoma (GBM) is the most common primary malignant brain tumor in adults. The current treatments include surgery followed by concomitant chemoradiotherapy with temozolomide (TMZ) and adjuvant chemotherapy with TMZ as described in the randomized European and Canadian trial (EORTC/NCIC).1,2 Although advances in treating GBM have been accomplished, the prognosis of patients with GBM is rather poor and the median overall survival (OS) is only ~14.6 months.1 At present, there is a great demand to identify therapeutic drugs for GBM.3
β-Elemene (ELE) is a broad-spectrum antitumor drug extracted from the medicinal herb Curcuma wenyujin.4 ELE has been shown to be effective in treating many cancers, including gastric,5 lung,6 and ovarian cancers7 and leukemia.8 Because of its small molecular weight and lipid solubility, ELE can penetrate the blood–brain barrier4 and has been used to treat glioma.9 Recently, several in vitro studies showed that ELE treatment inhibited GBM cell proliferation,10,11 promoted differentiation,12 induced apoptosis,13 and chemo- and radiosensitized GBM cells.11,12,14 All these findings indicated the potential survival benefit of ELE in treating GBM. However, so far, no clinical investigation about ELE treatment with special focus on GBM has been done. In this study, we retrospectively analyzed the use of ELE in patients with newly diagnosed GBM and also assessed the survival benefit of ELE.
Methods
This study was approved by the institutional ethics committee at Henan Provincial People’s Hospital and performed in compliance with the Declaration of Helsinki. Since this was a retrospective analysis, no informed consents were obtained from the patients involved in this study.
Patients and treatments
Data of the patients who were diagnosed with primary GBM between 2009 and 2014 at our hospital were retrospectively reviewed. The inclusion criteria for this study were as follows: 1) adult patients aged ≥18 years; 2) histopathologically confirmed, newly diagnosed GBM; 3) patients underwent surgery and postoperatively received concomitant chemoradiotherapy and adjuvant chemotherapy with TMZ; 4) preoperative checks showed no sign of dysfunctions in the heart, lung, liver, and kidney; 5) patients showed no postoperative complications; and 6) medical records were complete. In total, 63 patients were enrolled in this study.
Within 4 weeks after operation, patients received the standard treatments according to the protocol described by Stupp et al.1 Radiotherapy (RT) consisted of fractionated focal irradiation at a dose of 2 Gy per fraction given once daily, 5 days per week, for a period of 6 weeks, for a total dose of 60 Gy. Concomitant TMZ was administered at a dose of 75 mg/m2 daily, 7 days per week from the first day to the last day of RT. After an interval of 4 weeks, patients received up to 6 cycles of adjuvant TMZ according to a standard 5-day schedule every 4 weeks. The TMZ dose was 150 mg/m2 daily for the first cycle and increased to 200 mg/m2 daily at the beginning of the second cycle.
Evaluations
The baseline evaluations included magnetic resonance imaging (MRI), hematological and serological tests, physical and neurological examinations, and Karnofsky performance scale score (KPS). Enhanced MRI was performed within 48 hours after surgery, before RT, 4 weeks after concomitant chemoradiotherapy with TMZ, at the second, fourth, and sixth cycles of adjuvant chemotherapy, and every 3 months thereafter. The extent of resection and tumor progression was evaluated using a series of MRI taken as mentioned earlier. Complete resection was defined as ≥95% removal of the initial tumor, and partial resection was defined as <95%. Tumor progression was defined as an increase in tumor size of >25% or by the presence of a new lesion on imaging.15
The toxic effects of the treatment were determined according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE version 3.0), with a score of 1 indicating mild adverse effects, a score of 2 indicating moderate adverse effects, a score of 3 indicating severe adverse effects, a score of 4 indicating life-threatening adverse effects, and a score of 5 denoting death related to adverse effects.
The methylation status of O-6-methylguanine-DNA methyltransferase (MGMT) promoter was determined by methylation-specific polymerase chain reaction as reported previously.16
The primary end point was OS. The secondary end points were progression-free survival (PFS) and toxicity. OS was defined as the time from diagnosis to death or the last follow-up. PFS was defined as the time from diagnosis to documented progression or death, whichever occurred first.
Statistical analysis
SPSS software (SPSS version 21.0, Chicago, IL, USA) was employed to perform all the statistical analyses in this study. OS and PFS were analyzed by Kaplan–Meier method and tested by log-rank test. The risk factors for OS and PFS were analyzed by COX proportional hazards regression model. The factors with P<0.2 in the univariate COX analysis were used for further multivariate COX analysis. P<0.05 was considered as statistically significant.
Results
Baseline clinical characteristics of the patients
The baseline clinical characteristics of the patients with GBM are summarized in Table 1. Sixty-three patients comprising 38 men and 25 women were enrolled according to the aforementioned inclusion criteria. The average age was 42.49±13.16 years. In total, 28 patients (44.4%) received ELE treatment. The methylation status of the MGMT promoter was positive in 23 patients (36.5%), negative in 33 patients (52.4%), and unknown in 7 patients (11.1%). Thirty-one patients (49.2%) underwent complete resection, and 32 patients (50.8%) underwent partial resection. The clinical parameters of the patients who received treatment with and without ELE are summarized and compared in Table 2. As indicated in Table 2, no statistically significant differences existed with regard to age, gender, preoperative KPS, extent of resection, and the MGMT promoter methylation status between the patients treated with and without ELE.
Survival outcome
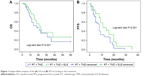
Kaplan–Meier method was used to analyze the PFS and OS. For the entire 63 patients, the median PFS was 9.2 months (95% confidence interval [95% CI]: 6.8–11.7 months) and the median OS was 19.6 months (95% CI: 16.5–24.2 months). For patients who received ELE, the median PFS was 11 months (95% CI: 9.4–12.6 months) and the median OS was 21 months (95% CI: 18.8–23.1 months) (Figure 1). For patients who did not receive ELE, the median PFS was 8 months (95% CI: 7.6–8.3 months) and the median OS was 18 months (95% CI: 15.5–20.5 months) (Figure 1). Both the median OS and the median PFS of the patients with ELE treatment were significantly longer than those of patients without ELE treatment (Figure 1, P<0.001 for both).
The influence of the MGMT promoter methylation status on the prognosis was also analyzed using Kaplan–Meier method (Figure 2). The results showed that the patients with methylated MGMT promoter had longer PFS (median: 9 months, 95% CI: 5.9–12.1 months, vs median: 5 months, 95% CI: 3.4–6.6 months, P<0.001) and OS (median: 14 months, 95% CI: 10.6–17.4 months, vs median: 7 months, 95% CI: 4.8–9.2 months, P=0.008) than patients with unmethylated MGMT promoter (Figure 2A and D), which indicated a better prognosis in patients with methylated MGMT promoter.
In order to further investigate the ELE treatment, the data were stratified according to the methylation status of MGMT promoter and analyzed using Kaplan–Meier method again. Results demonstrated that for the group with unmethylated MGMT promoter, the median PFS of patients with ELE treatment was 5 months (95% CI: 3–7 months), longer than that of patients without ELE treatment (median: 4 months, 95% CI: 1.4–6.6 months) (Figure 2B); the median OS of patients with ELE treatment was 11 months (95% CI: 4.7–17.3 months), longer than that of patients without ELE treatment (median: 7 months, 95% CI: 4.2–9.8 months) (Figure 2E). For the group with methylated MGMT promoter, the median PFS of patients with ELE treatment was 12 months (95% CI: 6.2–17.8 months), longer than that of patients without ELE treatment (median: 9 months, 95% CI: 7.8–10.2 months) (Figure 2C); the median OS of patients with ELE treatment was 15 months (95% CI: 11–32 months), longer than that of patients without ELE treatment (median: 12 months, 95% CI: 10.2–13.8 months) (Figure 2F). The earlier results indicated that ELE treatment could significantly prolong the PFS (P=0.038) and OS (P=0.016) despite the MGMT promoter methylation status (Figure 2B, C, E, and F).
COX proportional hazards regression model was used to assess the prognostic factors. As shown in Table 3, ELE was the only prognostic factor for PFS (hazard ratio [HR], 0.34; 95% CI: 0.15–0.62; P=0.011). The prognostic factors for OS included preoperative KPS (≥70) (HR, 0.26; 95% CI: 0.12–0.75; P=0.028), MGMT promoter methylation status (HR, 0.44; 95% CI: 0.19–0.83; P=0.004), and ELE (HR, 0.31; 95% CI: 0.14–0.69; P=0.006).
Toxicity
In patients without ELE treatment, 4 patients presented with neutropenia (grades 3–4) and 6 presented with thrombocytopenia (grades 3–4), while in ELE-treated patients, grades 3–4 neutropenia occurred in 1 patient and grades 3–4 thrombocytopenia in 1 patient. Hence, grades 3–4 hematologic toxic effects occurred more frequently in patients without ELE treatment (28.6%) than in those with ELE treatment (7.1%) (χ2=4.559, P=0.031). The hematologic toxic effects were resolved by treatment with recombinant human granulocyte colony-stimulating factor and chemotherapy was not stopped in any patients. Most of the other toxicities were under grade 2. The non-hematologic toxic effects such as nausea and vomiting were resolved by 5-hydroxytryptamine-3 receptor antagonist. In patients with ELE treatment, local pain and phlebitis occurred in some patients because of the intravenous injection. The local pain and phlebitis were resolved by local nursing or local washing with 5 mg dexamethasone in 100 mL physiological saline.
Discussion
ELE, a natural compound, is extracted from a traditional Chinese medicinal herb Curcuma wenyujin It has been used in cancer treatment in Chinese traditional medicine for many years.17 ELE shows no cytotoxic effect on normal cells, displays a broad-spectrum efficacy in treating tumors, and has some advantages over conventional chemotherapeutic drugs, such as enhancement of host immune system and sensitization of adjuvant radio- and chemotherapies.4,5,8,9,17 In the People’s Republic of China, ELE has been used to treat glioma clinically.9,18 Recent in vitro investigations have also shown that when treating GMB, ELE was not only an antitumor agent but also a chemo- and radiosensitizer.11–14 In this clinical study, we focused on the use of ELE in GBM patients.
As one of the most frequent primary central nervous system malignancies, GBM has a very poor prognosis.1 An international randomized European and Canadian trial (EORTC/NCIC) compared the RT alone and concomitant RT and TMZ for GBM patients and clearly proved the benefits of adjuvant TMZ chemotherapy.1,2 Since then, TMZ has been the first-line chemotherapeutic agent for GBM. TMZ is an oral alkylating drug that exerts its cytotoxicity through methylation of the O6-position of guanine.2,19 However, this DNA damage can be rapidly repaired by MGMT.20–22 Clinical analyses have illustrated that patients with epigenetic silencing of MGMT gene through promoter methylation could benefit more from TMZ treatment, and MGMT promoter methylation status was a prognostic factor for patients with GBM.16,23,24 In our investigation, we found a significant beneficial outcome in patients receiving ELE in addition to concomitant chemoradiotherapy with TMZ. What is more, the effectiveness of ELE in patients with GBM was independent of the MGMT promoter methylation status. This result confirmed the previously reported conclusion that MGMT prognostic impact on GBM was dependent on therapeutic modalities.25
Toxic effects, including myelosuppression associated with concomitant chemoradiotherapy with TMZ, limit the usage of TMZ in some patients.1 Previous clinical investigations demonstrated that in treating brain glioma, ELE could reduce the occurrence of toxic effects associated with chemoradiotherapy.4,9 In this study, our results confirmed the anti-toxicity effects of ELE in treating GBM. Especially, we found that ELE treatment could reduce grades 3–4 hematologic toxicities in GBM patients.
This study has several limitations. First, this is a single-center retrospective investigation and a certain selection bias occurs inevitably. Second, the case number might be still not enough. The results and conclusions in this study need further confirmation by a future multicenter prospective study.
In summary, the results of this retrospective study demonstrated that ELE treatment in patients with GBM provided survival benefit, which was independent of the MGMT promoter methylation status. Furthermore, ELE treatment could also reduce the hematological toxicity induced by chemoradiotherapy.
Acknowledgment
This work was supported by Key Science and Technology Program of Health and Family Planning Commission of Henan Province (No 201303158).
Disclosure
The authors report no conflicts of interest in this work.
References
Stupp R, Mason WP, van den Bent MJ, et al; European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. | ||
Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10(5):459–466. | ||
Domingo-Musibay E, Galanis E. What next for newly diagnosed glioblastoma? Future Oncol. 2015;11(24):3273–3283. | ||
Tang X, Qin S, Xie T. Status and progress of basic researches of elemene injection for anti-tumor. Chin Clin Oncol. 2010;15(3):266–273. | ||
Liu X, Hua BJ. Effect of traditional Chinese medicine on quality of life and survival period in patients with progressive gastric cancer. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2008;28:105–107. | ||
Zhao J, Li QQ, Zou B, et al. In vitro combination characterization of the new anticancer plant drug beta-elemene with taxanes against human lung carcinoma. Int J Oncol. 2007;31(2):241–252. | ||
Li X, Wang G, Zhao J, et al. Antiproliferative effect of beta-elemene in chemoresistant ovarian carcinoma cells is mediated through arrest of the cell cycle at the G2-M phase. Cell Mol Life Sci. 2005;62(7–8):894–904. | ||
Zou L, Liu W, Yu L. Beta-elemene induces apoptosis of K562 leukemia cells. Zhonghua Zhong Liu Za Zhi. 2001;23:196–198. | ||
Dong H, Jin F, Wu W, Chen H, Huang W, Liu X. Postoperative radiotherapy combined with elemene for brain glioma. Chin Clin Oncol. 2008;35(15):858–860. | ||
Yao Y-Q, Ding X, Jia Y-C, Huang C-X, Wang Y-Z, Xu Y-H. Anti-tumor effect of β-elemene in glioblastoma cells depends on p38 MAPK activation. Cancer Lett. 2008;264(1):127–134. | ||
Zhu T, Xu Y, Dong B, et al. β-elemene inhibits proliferation of human glioblastoma cells through the activation of glia maturation factor β and induces sensitization to cisplatin. Oncol Rep. 2011;26(2):405–413. | ||
Zhu T, Li X, Luo L, et al. β-elemene inhibits stemness, promotes differentiation and impairs chemoresistance to temozolomide in glioblastoma stem-like cells. Int J Oncol. 2014;45(2):699–709. | ||
Zhao YS, Zhu TZ, Chen YW, et al. Beta-elemene inhibits Hsp90/Raf-1 molecular complex inducing apoptosis of glioblastoma cells.J Neurooncol. 2012;107(2):307–314. | ||
Liu S, Zhou L, Zhao Y, Yuan Y. β-elemene enhances both radiosensitivity and chemosensitivity of glioblastoma cells through the inhibition of the ATM signaling pathway. Oncol Rep. 2015;34(2):943–951. | ||
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8(7):1277–1280. | ||
Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003. | ||
Zhu Y, Hu J, Shen F, Shen H, Liu W, Zhang J. The cytotoxic effect of beta-elemene against malignant glioma is enhanced by base-excision repair inhibitor methoxyamine. J Neurooncol. 2013;113(3):375–384. | ||
Xu H, Zhang J, Yue W, et al. Relationship between MGMT expression in gliomas and in vitro their sensitivity to drug as well as its clinical significance. Chin J Clin Neurosurg. 2007;12(5):263–266. | ||
Joo JD, Kim H, Kim YH, Han JH, Kim CY. Validation of the effectiveness and safety of temozolomide during and after radiotherapy for newly diagnosed glioblastomas: 10-year experience of a single institution. J Korean Med Sci. 2015;30(11):1597–1603. | ||
Ochs K, Kaina B. Apoptosis induced by DNA damage O6-methylguanine is Bcl-2 and caspase-9/3 regulated and Fas/caspase-8 independent. Cancer Res. 2000;60(20):5815–5824. | ||
Gerson SL. Clinical relevance of MGMT in the treatment of cancer. J Clin Oncol. 2002;20(9):2388–2399. | ||
Gerson SL. MGMT: its role in cancer aetiology and cancer therapeutics. Nat Rev Cancer. 2004;4(4):296–307. | ||
Esteller M, Garcia-Foncillas J, Andion E, et al. Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med. 2000;343(19):1350–1354. | ||
Hegi ME, Diserens AC, Godard S, et al. Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res. 2004;10(6):1871–1874. | ||
Criniere E, Kaloshi G, Laigle-Donadey F, et al. MGMT prognostic impact on glioblastoma is dependent on therapeutic modalities. J Neurooncol. 2007;83(2):173–179. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.