Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Benign paroxsymal positional vertigo – recommendations for treatment in primary care
Authors Wang YH, Chan CY, Liu QH
Received 29 January 2019
Accepted for publication 9 May 2019
Published 11 June 2019 Volume 2019:15 Pages 719—725
DOI https://doi.org/10.2147/TCRM.S203291
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Yi-Hong Wang,1,* Ching Yee Chan,2,* Qing-Hua Liu1
1Department of Otorhinolaryngology, The Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, People’s Republic of China; 2Department of Otolayngology, KK Women’s and Children’s Hospital, Duke-NUS Medical School, Singapore
*These authors contributed equally to this work
Background: Benign paroxysmal positional vertigo (BPPV) is a common cause of vertigo that can be easily diagnosed and treated in primary care.
Purpose: We describe our experience with a large cohort of patients and include recommendations for diagnosis and treatment in the primary care setting.
Patients and methods: Three hundred and fifty-nine patients were diagnosed with BPPV between June 2011 and March 2017 at the dizziness clinic of Fujian Provincial Hospital, Fuzhou, China. We mainly used Epley’s maneuver and barbecue roll for the treatment of PSC-BPPV and HSC-BPPV respectively.
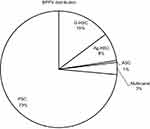
Results: Our results show that posterior semicircular canal (PSC) involvement is the most common (n=264, 73.5%), followed by horizontal semicircular canal (HSC, n=81, 22.5%) and multicanal (n=12, 3.3%) involvement. Anterior semicircular canal (ASC) BPPV is the rarest (n=2). Particle repositioning maneuvers (PRM) are the treatment of choice and have a high success rate (1 month after treatment), from 75% (9 out of 12) for multicanal to 95.8% (253 out of 264) for PSC, and to 100% for HSC and ASC involvement respectively.
Conclusion: We recommend the use of the Epley’s maneuver and barbecue roll for the treatment of PSC-BPPV and HSC-BPPV, respectively. Patients should be reviewed regularly and repeated maneuvers can be performed. Unresolving symptoms require tertiary evaluation.
Keywords: giddiness, benign paroxysmal positional vertigo, Epley’s maneuver, diagnosis, treatment
Introduction
Vertigo is one of the commonest complaints in medical practice and may present to a wide range of clinicians, including general practitioners, otolaryngologists and neurologists. Benign Paroxysmal positional vertigo (BPPV) accounted for 35.6% of 5,348 outpatient visits in a tertiary referral hospital1 and accounts for 1 to 2.4 million outpatient visits in the United States annually.2 Symptoms are characterized by recurrent, brief episodes of vertigo triggered by changes in head position. This occurs due to abnormal endolymphatic flow, caused by free-floating otoliths (canalithiasis)3 or less commonly from otoliths adherent to the cupula (cupulolithiasis)4 in any of the three semicircular canals.
The diagnosis is made with targeted history taking and a positive positional test. Treatment with particle repositioning maneuvers (PRMs) can be performed immediately after diagnosis in the office setting to return the otoliths to the utricle.2 Patients with BPPV are often referred to tertiary dizziness centers. Our tertiary dizziness center receives large numbers of such referrals, and the purpose of this clinical observational study is to share our experience of diagnosis and treatment of BPPV in a cohort of 359 patients. We want to empower primary care physicians to diagnose and manage BPPV. With accurate diagnosis, most BPPV cases can be managed by primary care physicians with immediate relief of symptoms, reducing the need for medication and lost productivity.
Methods
Three hundred and fifty-nine patients were diagnosed with BPPV between June 2011 and March 2017 at the dizziness clinic of Fujian Provincial Hospital, Fuzhou, China. To protect patient privacy, the study patients were recorded using an anonymized code without any identifiable information. This study was approved by the Ethics Committee of Fujian Provincial Hospital with a waiver of patient consent.
The diagnoses of posterior semicircular canal (PSC) BPPV, horizontal semicircular canal (HSC) canalithiasis and HSC cupulolithiasis were made based on the American Academy of Otolaryngology – Head and Neck Surgery 2017 clinical practice guideline on BPPV.2 A history and detailed physical examination looking for other causes of dizziness (migraine, Menière’s disease, vestibular insufficiency, vestibular neuronitis or vestibular schwannoma) was also performed. The supine roll test was used to diagnose and differentiate between the types of HSC-BPPV. Canalithiasis yielded geotropic nystagmus, and the affected ear was the side with the strongest nystagmus (G-HSC). Cupulolithiasis or canaliths in the ampullary arm of the HSC yielded apogeotropic nystagmus (Ag-HSC). The affected ear was opposite the side with the strongest nystagmus. None of the patients received premedication before physical examination.
PSC-BPPV and anterior semicircular canal (ASC)-BPPV were treated with Epley’s maneuver5 and reverse Epley’s maneuver,6 respectively. G-HSC BPPV was treated with the barbecue roll maneuver.7 Ag-HSC BPPV was treated by converting it to G-HSC BPPV and then proceeding with the barbecue roll maneuver. If there was no conversion after the supine roll test, another maneuver was performed. The patient was placed supine with the affected ear downward. The head was rotated rapidly in the direction of the healthy side by 90° (to a nose-up position) and then another 90° to bring the normal ear downward and affected ear upward. The head was then rotated slowly back to the starting position.8 In multicanal involvement, the side causing more severe nystagmus was treated first.
Patients were reviewed a week after PRM. If the positional test was negative, they returned a month from the first consultation for follow-up. If the positional test was positive, PRM was repeated and the patients were reevaluated a week later. If the positional test was still positive, the PRM was repeated. The same procedure was continued till the PRM was performed for a maximum of four times. All patients were reassessed a month from the first consultation (Figure 1).
 | Figure 1 Summary of patient treatment protocol.Abbreviations: BPPV, benign paroxysmal positional vertigo; PRMs, particle repositioning maneuvers. |
Results
Of 359 patients, 133 (37%) were men and 226 (63%) were women. Patients were between 18 and 90 years old. The mean age was 52±16 years (Table 1). None of the patients had findings suggestive of other causes of dizziness, including migraine, Menière’s disease, vestibular insufficiency, vestibular neuronitis or vestibular schwannoma. Nine patients had a history of head trauma.
 | Table 1 The success rates and recurrence according to the types of BPPV (n=359) |
Majority of patients had PSC-BPPV (n=264, 73.5%) followed by HSC-BPPV (n=81, 22.5%). Among the 81 patients with HSC-BPPV, 53 had G-HSC and 28 had Ag-HSC. Six patients (2.3%) with PSC-BPPV and 3 patients (3.7%) with HSC-BPPV had prior head trauma. Twelve patients (3.3%) had multicanal involvement and 2 patients had ASC-BPPV (Figure 2). Right-sided BPPV was more common, comprising 171 (65%) of PSC-BPPV patients and 52 (64%) of HSC-BPPV patients.
In the PSC-BPPV group, the success rate of the first PRM was 78.4%.The remaining 57 patients (21.6%) had a positive positional test on the seventh day. Of these, 48 patients had a positive Dix-Hallpike maneuver, seven patients had a positive supine roll test and two patients were positive for both maneuvers (Table 1). In other words, the residual PSC-BPPV rate was 18.6%, conversion to HSC-BPPV was 1.9% and 0.8% had both residual and canal conversion.
In the HSC-BPPV group, the success rate of the first PRM was 88.9%. Of the nine remaining patients with symptoms (11.1%), five patients (6.2%) had a positive roll maneuver (Ag-HSC: three patients, G-HSC: two patients) and four patients had a positive Dix-Hallpike maneuver (Ag-HSC: three patients, G-HSC: one patient). After classification into Ag-HSC BPPV and G-HSC BPPV, the success rate of Ag-HSC was 78.6%. Of the failures, half had residual BPPV and half experienced canal conversion to PSC-BPPV. The success rate was 94.3% in the g-HSC group. Of the failures, two-thirds had residual BPPV and one-third had canal conversion to PSC-BPPV.
In the ASC-BPPV group, the success rate was 50% after the first PRM.
In the multicanal BPPV group, the success rate was 25% after the first PRM. Six patients had a positive Dix-Hallpike maneuver, one patient had a positive roll maneuver and two patients were positive for both maneuvers.
After 30 days, the PRM success rate was 95.8% for PSC-BPPV, 100% for HSC-BPPV, 100% for ASC-BPPV and 75% for multicanal BPPV.
Discussion
BPPV is more prevalent in women and older patients.9 Our study confirms these findings. Our study also confirms that right-sided BPPV is more common. This is proposed to be due to increased preference of sleeping in the right lateral position.10
Most BPPV cases are diagnosed with a focused history and accurate physical examination. During positional testing, the Dix-Hallpike maneuver is performed first. The maneuver is positive when there is a period of latency followed by upbeating, torsional, geotropic nystagmus that crescendos and lasts for less than a minute.11 A positive maneuver gives a straightforward diagnosis of PSC-BPPV. When the Dix-Hallpike maneuver is negative, the supine roll test is administered. Two key points to note in this test are 1) nystagmus direction (should remain in the same direction, either geotropic or apogeotropic) and 2) the side with worse symptoms. The direction of nystagmus differentiates between HSC canalithiasis and cupulolithiasis and canalithiasis of the ampullary side. The side with worse symptoms identifies the affected side. If the affected side is unclear, secondary clinical tests such as the “Bow and Lean” test12 can be used.
Upon diagnosis, the patient is treated in the same setting using the PRM. The Epley maneuver5 is effective in treating PSC-BPPV, the most common BPPV variant. A Cochrane review including 11 trials with 745 patients showed it to be more effective than sham maneuvers and controls,13 and we have shown the success rate to be 78.4% after the first PRM. With repeated Epley maneuvers, the success rate increases to 95.8%.
We used the barbecue roll maneuver to treat HSC-BPPV in this study. Variations of this maneuver are the most widely studied. Fife TD et al estimate the success rate to be <75%, though rates between 50% and 100% have been quoted.14 In a 2015 review article, this maneuver had 38.4–69.1% success for G-HSC BPPV and 75% for Ag-HSC BPPV.15 Casani AP et al described their success rates for G-HSC to be 61% after one PRM (barbecue maneuver and forced prolonged positioning), 70% after two PRM and 79.6% after three PRMs. Their 30-day success rate was 81% and the Gufoni maneuver was found to be superior.16 Our study success rate after one PRM is 94.3% for G-HSC BPPV and 78.6% for Ag-HSC BPPV. The 30-day success rate for both is 100%. Our study supports findings that G-HSC BPPV has a higher initial response rate than Ag-HSC; eventual outcomes are similar after repeated PRMs. Our data also show a higher success rate with the barbecue roll maneuver than the previous studies and support the use of this maneuver in patients with both variants of HSC-BPPV.
The success rate of HSC-BPPV after PRM is lower than PSC-BPPV because of the large proportion (34.6%) of patients with Ag-HSC BPPV. Clinicians need to differentiate between G-HSC and Ag-HSC as well as identify the affected side to treat it accurately. When Ag-HSC BPPV is diagnosed, we recommend converting it to the g-HSC form to increase the success rate.17 If Ag-HSC BPPV remains, the clinician may proceed with the barbecue maneuver anyway as the success rate is still high, ranging from 71.418 to 100%. Symmetrical responses during the supine roll test can occur in up to 9.7% of Ag-HSC-BPPV patients but should not affect their prognosis. If the patient does not seem to respond to the barbecue maneuver for one side, the maneuver can be performed for the opposite side during the next follow-up. Alternatively, the affected side can be identified using secondary clinical signs.12
- Aside from the barbecue roll, other maneuvers have been used to treat HSC-BPPV, including the Gufoni maneuver,19 forced prolonged positioning, Vannucchi-Asprella,20 affected-ear-up 120° maneuver21 etc. These maneuvers have been described and used by departments with high volumes of vertiginous patients. Differences in study design and variations of the PRMs have resulted in varied outcomes (Tables 2 and 3). In the primary care setting, we recommend mastery of one maneuver, before attempting other maneuvers.
 | Table 2 Summary of studies comparing success rates of treatment maneuvers for Ag-HSC (%) |
 | Table 3 Summary of studies comparing success rates of treatment maneuvers for G-HSC (%) |
Uncommon BPPV variants
Other kinds of PSC-BPPV have been described. When canaliths are localized to the nonampullary arm of the posterior canal, near the common crus, an apogeotropic variant of posterior BPPV is observed.22 During the Dix-Hallpike maneuver, paroxysmal positional nystagmus occurs in the direction opposite to that evoked in posterior canal BPPV: downbeating, torsional nystagmus, clockwise for the right and counterclockwise for the left.23,24 It can be treated with the demi Semont maneuver or 45° forced prolonged positioning.24 Cupulolithiasis of the PSC, with persistent torsional/vertical (upbeating) positional nystagmus in the head-hanging position, has also been described25 .
A subset of HSC-BPPV patients have been described to have direction-changing positional nystagmus (DCPN).26 The pathophysiology is unclear,27 and the “light cupula” hypothesis has been used to explain the findings, which include a) nystagmus stops when patient’s head is turned to the affected ear at 20 degrees, b) horizontal nystagmus toward the affected side in bowing position, c) horizontal nystagmus toward the unaffected side in leaning position and c) persistent geotropic DCPN without latency when the patient’s head is turned right or left in the supine position. PRMs have not found to be effective and symptoms resolve spontaneously within two weeks.
None of these uncommon variants of BPPV were present in our study. Videonystagmography was not part of our physical examination, and perhaps this group of patients were misdiagnosed. In primary practice, it will be extremely difficult to diagnose this subset of patients. Thus, we recommend these patients to be referred on to a tertiary center for further evaluation to exclude more sinister causes such as neurological pathology.
ASC-BPPV is an uncommon diagnosis. Our study showed an incidence of 0.6% while Heidenreich KD et al found it to be between 1% and 3%28 and Casani AP et al quoted an incidence between 2% and 21%.29 It can occur following a canal switch, where the debris exits the PSC via the common crus into the ASC. Refractory cases occur when debris lodge on the ampullated ends of the ASC, near the cupula. Debris in this position is held in place by gravity. A high index of suspicion is required, and specific maneuvers must be used. Yacovino DA et al described a new therapeutic maneuver for ASC-BPPV that does not require identification of the affected side,30 thus facilitating immediate treatment and increasing the success rate.29 In another study, the success rate was 75.9% for the reverse Epley’s maneuver, 78.8% for Yacovino and 92% for other nonstandard therapeutic maneuvers.31 Our study had too few numbers of patients with ASC-BPPV for comparison.
Canal conversion
Our rate of canal conversion from HSC-BPPV to PSC-BPPV was 4.9% following the barbecue roll maneuver. The rate of conversion was higher for Ag-HSC BPPV (10.7%) than G-HSC BPPV (1.9%). Interestingly, in a study by Riggio F et al, the conversion rate was 13.8% for G-HSC BPPV treated with Gufoni maneuver.32 Another study by Casani et al also showed the canal conversion rate to be higher in patients who underwent the Gufoni maneuver (6.9%) than the barbecue and forced prolonged positioning method (1.8%).16 It could be that the head positioning for the Gufoni maneuver predisposes the canaliths to fall into the posterior canal more than the barbecue roll maneuver. If canal conversion occurs, it does not pose a significant problem as long as the treating physician picks it up and treats the patient with the Epley’s maneuver.
After successful PRMs, it is common for patients to experience a period of imbalance without positional vertigo (residual dizziness). While the pathophysiology is unclear with many proposed theories, the key point is to reassure patients that residual dizziness usually resolves after a period of time and that pharmacological therapy may not be helpful in preventing its onset.33
In summary, doctors should familiarize themselves with the diagnostic tests for BPPV. The two key points to note during the positional tests are the presence of nystagmus and its direction. The diagnosis is made instantaneously and the patient can be treated at the same office setting, leading to relief of symptoms. The PRMs we recommend are the Epley’s maneuver for PSC-BPPV and the barbecue roll for HSC-BPPV as they have been proven to be effective. Familiarity with PRMs and repeat practice may improve the success rate. Patients that have been treated should be reevaluated in a timely fashion so the maneuver can be repeated if necessary. Patients who are unable to comply with the maneuvers (such as neck stiffness), whose symptoms persist after repeated maneuvers or whose symptoms are atypical should be referred to a tertiary center for further evaluation to exclude other causes.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li F, Wang XG, Zhuang JH, et al. Etiological analysis on patients in department of vertigo and dizziness oriented outpatient. Zhonghua Yi Xue ZaZhi. 2017;97(14):1054–1056.
2. Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical practice guideline: benign paroxysmal positional vertigo (Update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1–S47.
3. Hall SF, Ruby RR, McClure JA. The mechanics of benign paroxysmal vertigo. J Otolaryngol. 1979;8(2):151–158.
4. Schuknecht HF. Cupulolithiasis. Arch Otolaryngol. 1969;90(6):765–778.
5. Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399–404. doi:10.1177/019459989210700310
6. Imbaud-Genieys S. Anterior semicircular canal benign paroxysmal positional vertigo: a series of 20 patients. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130(6):303–307. doi:10.1016/j.anorl.2012.10.004
7. Lempert T, Tiel-Wilck K, Positional A. Maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope. 1996;106(4):476–478.
8. Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 2009;118(4):455–460.
9. Brevern von M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2006;78(7):710–715. doi:10.1136/jnnp.2006.100420
10. Brevern von M. Benign paroxysmal positional vertigo predominantly affects the right labyrinth. J Neurol Neurosurg Psychiatry. 2004;75(10):1487–1488. doi:10.1136/jnnp.2003.031500
11. Bhattacharyya N, Baugh RF, Orvidas L, et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139(5suppl4):47–81.
12. Choung YH, Shin YR, Kahng H, Park K, Choi SJ. “Bow and lean test” to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116(10):1776–1781. doi:10.1097/01.mlg.0000231291.44818.be
13. Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014;8(12):CD003162.
14. Fife TD, Iverson DJ, Lempert T, et al. Practice Parameter: therapies for benignparoxysmal positional vertigo(an evidence-based review). Neurology. 2008;70:2067–2074.
15. Oron Y, Cohen-Atsmoni S, Len A, Roth Y. Treatment of horizontal canal BPPV: pathophysiology, available maneuvers, and recommended treatment. Laryngoscope. 2015;125(8):1959–1964. doi:10.1002/lary.25138
16. Casani AP, Nacci A, Dallan I, Panicucci E, Gufoni M, Sellari-Franceschini S. Horizontal semicircular canal benign paroxysmal positional vertigo: effectiveness of two different methods of treatment. AudiolNeurotol. 2011;16(3):175–184.
17. Fife TD, von Brevern M. Benign paroxysmal positional vertigo in the acute care setting. Neurol Clin. 2015;33(3):601–617. doi:10.1016/j.ncl.2015.04.003
18. Riga M, Korres S, Korres G, Danielides V. Apogeotropic variant of lateral semicircular canal benign paroxysmal positional vertigo: is there a correlation between clinical findings, underlying pathophysiologic mechanisms and the effectiveness of repositioning maneuvers? Otol Neurotol. 2013;34(6):1155–1164. doi:10.1097/MAO.0b013e318280db3a
19. Gufoni M, Mastrosimone L, Di Nasso F. Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal. Acta Otorhinolaryngol Ital. 1998;18(6):363–367.
20. Asprella Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. 2005;25(5):277–283.
21. Ichijo H. Affected-ear-up 120° maneuver for treatment of lateral semicircular canal benignparoxysmal positional vertigo. Eur Arch Otorhinolaryngol. 2017;274(9):3351–3357. doi:10.1007/s00405-017-4663-z
22. Vannucchi P, Pecci R, Giannoni B. Posterior semicircular canal benign paroxysmal positional vertigo presenting with torsionaldownbeating nystagmus: an apogeotropic variant. Int J Otolaryngol. 2012;2012:413603. doi:10.1155/2012/413603
23. Califano L, Salafia F, Mazzone S, Melillo MG, Califano M. Anterior canal BPPV and apogeotropic posterior canal BPPV: two rare forms of vertical canalolithiasis. Acta Otorhinolaryngol Ital. 2014;34(3):189–197.
24. Vannucchi P, Pecci R, Giannoni B, Di Giustino F Santimone R, Mengucci A. Apogeotropic posterior semicircular canal benign paroxysmal positional vertigo: some clinicaland therapeutic considerations. Audiol Res. 2015;5(1):130. doi:10.4081/audiores.2015.130
25. Ichijo H. Cupulolithiasis of the posterior semicircular canal. Am J Otolaryngol. 2013;34(5):458–463. doi:10.1016/j.amjoto.2013.04.001
26. Kim CH, Kim MB, Ban JH. Persistent geotropic direction-changing positional nystagmus with a null plane: the light cupula. Laryngoscope. 2014;124(1):E15–9. doi:10.1002/lary.24048
27. Kim MB, Hong SM, Choi H, et al. The light cupula: an emerging new concept for positional vertigo. J Audiol Otol. 2018;22(1):1–5. doi:10.7874/jao.2017.00234
28. Heidenreich KD, Kerber KA, Carender WJ, Basura GJ, Telian SA. Persistent positional nystagmus. Laryngoscope. 2011;121(8):1818–1820. doi:10.1002/lary.21848
29. Casani AP, Cerchiai N, Dallan I, Sellari-Franceschini S. Anterior canal lithiasis: diagnosis and treatment. Otolaryngol Head Neck Surg. 2011;144(3):412–418. doi:10.1177/0194599810393879
30. Yacovino DA, Hain TC, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256(11):1851–1855. doi:10.1007/s00415-009-5123-5
31. Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. J Clin Neurol. 2015;11(3):262–267. doi:10.3988/jcn.2015.11.3.262
32. Riggio F, Dispenza F, Gallina S, Kulamarva G, Gargano R, Speciale R. Management of benign paroxysmal positional vertigo of lateral semicircular canal by Gufoni’smanoeuvre. Am J Otolaryngol. 2009;30(2):106–111. doi:10.1016/j.amjoto.2008.03.001
33. Giommetti G, Lapenna R, Panichi R, et al. Residual dizziness after successful repositioning maneuver for idiopathic benign paroxysmal positional vertigo: a review. Audiol Res. 2017;7(1):178. doi:10.4081/audiores.2017.178
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.