Back to Journals » Patient Preference and Adherence » Volume 15
Benefits of Switch from Oral to Subcutaneous Route on Adherence to Methotrexate in Patients with Rheumatoid Arthritis in Real Life Setting
Authors Senbel E, Tropé S , Herman-Demars H, Zinovieva E, Courbeyrette A, Clerson P , Fardini Y, Flipo RM
Received 14 January 2021
Accepted for publication 13 March 2021
Published 14 April 2021 Volume 2021:15 Pages 751—760
DOI https://doi.org/10.2147/PPA.S301010
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Eric Senbel, 1 Sonia Tropé, 2 Hélène Herman-Demars, 3 Elena Zinovieva, 3 Agnès Courbeyrette, 3 Pierre Clerson, 4 Yann Fardini, 4 René-Marc Flipo 5
1Rheumatology Office, Marseille, France; 2French National Patient Organization Against Rheumatoid Arthritis (ANDAR), Montpellier, France; 3Medical Department, Nordic Pharma, Paris, France; 4Soladis Clinical Studies, Roubaix, France; 5University of Lille, Rheumatology Department, Hôpital Roger Salengro, Lille, France
Correspondence: Yann Fardini
Soladis Clinical Studies, 15 Boulevard Du Général Leclerc, Roubaix, 59100, France
Tel +33 6 46 32 95 85
Fax +33 3 28 09 94 76
Email [email protected]
Purpose: The purpose of the APRIM study (for Adherence Polyarthrite Rhumatoïde Injection Methotrexate) was to investigate the change in treatment adherence of patients with rheumatic arthritis (RA) who switched from oral to subcutaneous methotrexate (MTX).
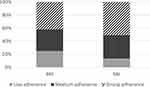
Patients and Methods: Prospective, observational study in RA patients treated with MTX and switching from oral to subcutaneous (SC) route in real-life conditions. Data on motivations for switch, disease activity (DAS28-CRP), quality of life (AISM-2 SF), disability (HAQ-DI), and adherence to MTX were collected at inclusion (M0) and 6 months later (M6). Adherence was assessed by the 8-item Morisky Medication Adherence Scale (MMAS-8) and defined as high (MMAS-8 = 8), medium (MMAS-8 = 6 or ≤ 8) or low (MMAS-8 < 6). The primary evaluation criterion was the proportion of patients who maintained strong adherence or improved adherence by at least one category (from low to medium or strong or from medium to strong) between M0 and M6.
Results: The analysis involved 207 patients (age 60.4± 12.7 years, 75.2% females). 6.7% were in remission and 15.5% had low disease activity (LDA) at baseline. 58.5% reached the primary criterion and strong adherence rate increased from 42.0% to 50.7%. Change of route was combined with increased MTX dose in 34.8% of patients. Switch to SC route increased the proportion of patients with remission or LDA from 22.8% to 52.9% and increased quality of life even in patients with unchanged MTX dose.
Conclusion: Overall, change from oral to SC route improved adherence to MTX, RA control and quality of life independently of change in MTX dose.
Keywords: rheumatoid arthritis, methotrexate, oral, subcutaneous, compliance, switch
Corrigendum for this paper has been published
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease involving pain, inflammation, stiffness and progressive joint destruction. Methotrexate (MTX) is a conventional synthetic Disease Modifying Anti-Rheumatic Drug (csDMARD) that holds a particular place in the management of RA. Due to its efficacy, safety, various routes of administration (parenteral or oral), versatility of doses available for titration and cost-effectiveness, MTX plays a role in every step of the disease management.1,2 MTX can be used as a monotherapy and as an “anchor drug” in many DMARDs combinations including either conventional or biological.3 This drug is the main first-line therapy used worldwide.4 Early RA is usually managed through a “step-up” approach. This strategy relies on the initiation with a MTX dose considered as well tolerated. Up-titration is then applied according to the patient’s specific characteristics and response.5 Switching from oral to subcutaneous (SC) MTX may improve clinical response in RA patients with inadequate response.6–9 Indeed, MTX bioavailability when injected subcutaneously is not affected by the limitation of active gut absorption in the case of oral route administration. Furthermore, patients with RA receiving oral MTX and exhibiting suboptimal or poor clinical response may benefit from an increased drug exposure by switching to the SC route of administration.6,10 Patients switched to SC MTX experience gastrointestinal side effects with lower intensity compared with patients receiving oral MTX,11 thus potentially supporting better adherence. Optimization of MTX monotherapy with SC administration is supported by various international recommendations.2,12
Adherence is defined as the adequacy between the recommendations of the health-care provider and patient behavior regarding treatment intake, diet or lifestyle modifications. As for any chronic medication, adherence to MTX is a keystone of its efficacy. Flares are four times more frequent in non-adherent patients than in adherent patients.13 Adherence to RA therapy has been reported to not exceed 66%.14 Adherence to MTX may be optimized by relevant patient information on the delay for reaching maximal efficacy, mitigation of the risk of adverse events by folic acid and MTX dose escalation based on tolerance and efficacy.15 Five overarching principles and 10 recommendations regarding adherence to DMARDs have recently been defined in an expert consensus. They stress out that informing and educating patients and defining treatment through patient/physician sharing process are fundamental for adherence optimization.16 In addition, change from oral to SC route has been reported to increase adherence to MTX.17,18 However, this is mainly based on expert recommendations and prospective longitudinal data investigating this issue are lacking. The APRIM study (standing for Adherence Polyarthrite Rhumatoïde Injection Methotrexate) investigated adherence to MTX in patients switching from oral to SC route. The main objective was to estimate the proportion of patients who maintained strong adherence or improved adherence by at least one category (from low to medium or strong adherence or from medium to strong adherence) according to the self-administered 8-item Morisky Medication Adherence Scale (MMAS-8).19–22 It further explored the evolution of the disease activity and the physician’s expectations regarding the switch of MTX route.
Patients and Methods
APRIM was a prospective, observational, multicenter study conducted by French rheumatologists in private or hospital settings (registration number: NCT02897817). The study has been approved by the French Ethics Committee (Comité de Protection des Personnes, approval #SC16/06, 18th of October 2016), the French Data Protection Authority (CNIL) and the French Advisory Committee on Information Processing in Research in the Field of Health (CCTIRS). This study was conducted in accordance with the Declaration of Helsinki.
Adult patients meeting ACR/EULAR criteria for RA diagnosis, receiving oral MTX and requiring a switch to SC route in the investigator’s opinion could enter the study. Patient recruitment was performed during a routine visit after providing proper information about the objectives, details and constraints of the study and obtaining the signature of a non-opposition form.
Data were collected at enrollment visit and 6 months after the switch to SC route. In the case of further change of MTX route or MTX discontinuation, the patients prematurely withdrew from the study and end-of-study data were collected. At inclusion visit, collected data included demographics, occupation, comorbidities, history of RA, current and new MTX regimen. New MTX regimen was chosen at the discretion of the physician based on marketed products for MTX injection that were available at that time which were all prefilled syringes (Biodim®, Metoject®, iMeth®). Physicians were asked about the reasons for switching MTX route encompassing RA worsening, need for corticosteroids sparing, tolerability concerns, and wish to improve adherence. At each visit, RA activity was assessed by the Disease Activity Score 28 (DAS28-CRP and DAS-28-ESR)23 and function was evaluated by the self-administered Health Assessment Questionnaire Disability Index (HAQ-DI).24 At both visits, adherence to MTX was evaluated by the self-administered 8-item Morisky Medication Adherence Scale (MMAS-8).19–22 MMAS-8 explores the patient’s behaviors regarding the treatment. Adherence is classified as “strong” (MMAS-8 = 8), “medium” (MMAS-8 = 6 or <8) or “low” (MMAS-8 less than 6). The MMAS-8 questionnaire is widely used for the assessment of intentional and non-intentional non-adherence and has been validated in French.25 Furthermore, it was used in patients with RA.26 Independently of MMAS-8 and during patient interview at the follow-up visit, the physician reported the number of missed injections over the study and the likely reasons for omissions. Patients separately reported the number of missed MTX injections during the 4 weeks prior to the 6-month follow-up visit and the reasons for omission. Quality of life was evaluated by the Arthritis Impact Measurement Scale Short Form (AIMS 2 SF), a RA-specific self-administered questionnaire with 26 items evaluating at what frequency the patient was able or not to perform some tasks (from every day to never) with higher score indicating more severe impact.27 At 6-month follow-up visit, the physician was asked to rate which expectations having motivated the change of route have actually been satisfied. Patients and physicians rated their level of satisfaction regarding MTX on a 5-point Likert scale (1 = totally; 5 = not at all).
In the case of premature MTX discontinuation or withdrawal from the study, date of last MTX injection, last MTX dosing and reasons for not maintaining the new MTX regimen were collected.
Results were reported as mean ± standard deviation (m±SD) or number (percentage on observed data). Proportions were estimated with an exact two-sided 95% confidence interval (CI) using the Clopper-Pearson method. Obesity was defined as body mass index greater or equal to 30 kg/m2. Partial missing data for MMAS-8 were imputed by a zero value representing the worst case scenario. Patients who did not fill any item of MMAS-8 at inclusion and/or at 6-month follow-up visit were excluded from analysis. Other missing values were not replaced. Apart from the global MMAS-8 score, sub-scores for intentional and non-intentional omissions were calculated. Baseline predictors of strong or improved adherence were individualized by logistic regression. Predictive value of each variable was tested beforehand in univariate models and variables with p-value < 0.20 were retained for the multivariate analysis with stepwise forward selection. The relationship between change in DAS28-CRP and change in MMAS-8 were assessed by multiple regression. Comparisons between M0 and M6 used Student’s t-test for paired samples for continuous variables and measures of agreement for categorical variables. The analyses were run with SAS 9.4 software (SAS Institute, Cary, NC, USA).
Of the 309 patients who were enrolled by 100 rheumatologists (90% private practice – recruitment from July 2016 to June 2017), 5 did not respect eligibility criteria. Of the 304 remaining patients, 38 prematurely withdrew from the study: 5 patients resumed oral route and 33 patients were lost to follow-up. Of the 266 having visited the physician at M6, 25 did not fill the MMAS-8 self-questionnaire at inclusion and a further 34 patients did not document MMAS-8 at M6. Values were imputed for partial missing data of MMAS-8 in 27 (13.0%) patients at baseline and 25 (12.1%) patients at M6. Therefore, the analysis involved 207 patients (Figure 1). Analyzed and lost to follow-up patients had similar demographics and RA-related characteristics except for the DAS28-CRP score which was higher in the lost to follow-up patients (4.3±1.1 vs 3.9±0.9, p = 0.0127), although the difference was below the reported threshold of 1 for minimal clinical important difference in RA patients28 (Supplementary Table 1).
 |
Figure 1 Study flow chart. |
Results
Baseline Characteristics
Patient’s characteristics are summarized in Table 1. Most common comorbidities included hypertension (52.7%), hypercholesterolemia (15.0%), type 2 diabetes (11.1%), depression (9.6%) and osteoporosis (8.6%).
 |
Table 1 Patients’ Characteristics |
The median time from RA diagnosis to enrollment in the study was 3 years; DAS28-CRP was 3.9±0.9 at inclusion with 6.7% of patients being in remission and 15.5% in low disease activity. Seventy-three patients (41.1%) had erosive RA. Extra-articular manifestations such as rheumatoid nodules and sicca were reported in 6.3% of patients.
MTX treatment started 17.5 months [7.0; 51.7] (median, quartiles) before enrollment and the baseline MTX regimen had been stable for 10.2 months [3.6; 24.5] (median, quartiles). Mean MTX dose was 15.0±3.9 mg per week (0.22±0.07 mg/kg/week). MTX was combined to biologics in 9.7% of patients. Biologics were mostly administered by prefilled syringes (58.8%), pens (29.4%) or intravenous perfusions (11.8%) and injections of biologics were performed by the patient (73.7%), a relative (15.8%) or by a nurse (10.5%).
Methotrexate Switch
While changing from oral to SC route, MTX dose was increased in 34.8% of patients, remained unchanged in 59.9% and decreased in 5.3%. Mean MTX dose was 16.1±3.6 mg per week (0.24±0.07 mg/kg/week). Reasons for switching from oral to SC route were RA worsening (44.0%), need for corticosteroids sparing (21.3%), adverse events (5.8%), and search for improving adherence (26.6%). During the study, patients performed the injection themselves (64.7%) or asked a relative to make it (24.2%). Only 11.1% of patients used the services of a nurse.
According to MMAS-8 questionnaire, at baseline, 42.0% of patients were strongly adherent to MTX. In patients with medium or low adherence, non-adherence was intentional in 49.2% of patients, non-intentional in 43.3% and neutral in 7.5%. Eight patients who switched to SC MTX due to poor tolerability had suboptimal adherence.
Evolution of Adherence After 6 Months
MMAS-8 score improved from baseline to 6-month visit (p = 0.002, Figure 2). The proportion of strongly adherent patients increased from 42.0% to 50.7%. One hundred and twenty-one (58.5%) patients maintained strong adherence or improved adherence by at least one category (Table 2). A sensitivity analysis using LOCF imputation of MMAS-8 at M6 in lost to follow-up patients showed similar results (Supplementary Table 2). In 102 patients with medium or low adherence at 6-month visit, non-adherence was intentional in 45.1% of patients, non-intentional in 50.0% and neutral in 4.9%. Of 87 patients with strong adherence at inclusion, 53 (60.9%) maintained strong adherence; of 120 patients with medium or low adherence at inclusion, 68 (56.7%) gained at least one category. Adherence decreased by at least one category in 40 (19.3%) patients. Three out of 8 patients with suboptimal adherence to MTX and poor tolerability of oral MTX as main reason for switch improved their adherence to MTX from M0 to M6. Adherence to oral MTX was lower at baseline in patients receiving biologics (p = 0.005). There was no more difference at M6 (p = 0.85) thanks to a larger improvement of adherence between M0 and M6 in this group (p = 0.008). In a separate analysis in patients switching for efficacy (RA worsening or need for corticosteroids sparing) and in those switching for improving adherence, mean MMAS-8 score increased significantly (Supplementary Table 3).
 |
Table 2 Adherence to MTX (N = 207) |
In a multivariate model, predictors for maintaining strong adherence or improving adherence were younger age (OR 0.97 [0.95; 0.99] per year), higher HAQ-DI (OR 1.81 [1.08; 3.06]), and absence of depression (OR 4.31 [1.19; 15.71]).
According to the physician, 13.5% of patients missed at least one MTX injection over the study. Most of them (82.1%) missed between 1 and 5 injections. During the 4 weeks preceding the 6-month follow-up visit, 9.8% of patients reported having missed one injection, and 3.4% missed more than one injection.
Evolution of Disease Activity
In patients with measures of DAS28-CRP available at M0 and at M6, the proportion of patients with remission or low disease activity dramatically increased from 22.2% to 52.3% (Table 3). The proportion of patients having gained LDA or remission was similar in obese and non-obese patients (p = 0.91). Furthermore, mean DAS28-CRP decreased significantly both in patients switching for efficacy and in those switching for improving adherence (Supplementary Table 3). There was no linear relationship between change in DAS28-CRP and change in MMAS-8 score (p = 0.62) even when the analysis was restricted to patients with unchanged MTX dosing (p = 0.81).
 |
Table 3 Evolution Between Baseline and 6-Month Follow-Up Visit |
Physician’s Expectation, Satisfaction and Quality of Life
Change in the modalities of MTX regimen overall met physicians’ expectations leading to satisfaction of both physicians and patients (Supplementary Figure 1A and B). Eighty-one percent of patients were rather satisfied or very satisfied with the easiness of use of the device used for MTX injection. Quality of life improved during the study in physical (p = 0.002), symptoms (p < 0.0001) and affect dimensions (p < 0.0001) (Figure 3, Table 3).
Interestingly, RA activity and quality of life improved in a similar way when the analysis was restricted to patients with maintained or decreased MTX dose when MTX route had been switched (data not shown).
Tolerance
On 12 patients who prematurely interrupted MTX, three discontinued for adverse event or drug intolerance. Of 207 patients analyzed, 32 patients reported a total of 38 adverse events (four pain at injection site, three abdominal pains, one erythema, one nausea and one diarrhea; details are lacking for 22 patients). No serious adverse events were reported.
Discussion
This observational study gave interesting insights in the physicians’ motivations when switching from oral to SC route in RA patients treated with MTX: better control of the disease, better adherence and improved tolerability. Switching from oral to SC route was associated with improved adherence to MTX. MMAS-8 score improved from baseline to 6-month visit (p = 0.002). The proportion of strongly adherent patients increased from 42.0% to 50.7%. One hundred and twenty-one (58.5%) patients maintained strong adherence or improved adherence by at least one category. However, only 50% of patients were strongly adherent at the 6-month follow-up visit, with a slight decrease in intentional non-adherence. Adherence to MTX was largely overestimated by the physician.
Physicians’ motivations when switching from oral to SC route are in line with the Treat-to-Target strategy and with known pharmacokinetics of injectable MTX.1 The proton-coupled folate transporter is responsible for the active absorption of oral MTX in the small gut.29
Oral MTX bioavailability is reported to be between 30% to 70%30,31 and reaches a plateau with single oral dose over 15 mg,6 suggesting an absorption limitation.32 The SC route increases MTX bioavailability, regardless of the dose.6 MTX is a prodrug that becomes active when glutamated within cells exhibiting a high binding activity for dihydrofolate reductase.29 The SC administration route is associated with a significant increase in long-chain MTXGlun when compared with the oral route33,34 and higher intracellular MTXGlun levels have been associated with better clinical response.35 Switching from oral to SC MTX may improve clinical response in RA patients with inadequate response,6–9 and prevent gastrointestinal side effects.11 Furthermore, the SC route has been previously reported to improve adherence to MTX.17,18 Switch from oral to SC MTX was driven by poor tolerability in only 5.8% of patients, making it a minor reason for switch.
Baseline MTX dose was certainly suboptimal. Despite the fact that only 22.2% of patients were in remission or had low disease activity, the MTX dose had been stable for a median of 10.2 months and 9.7% of patients were receiving biologics, certainly reflecting a part of inertia. It should be highlighted, however, that in France rheumatologists exclusively working in a liberal setting cannot initiate biologics. Change in MTX route was associated with increased MTX dose in one third of patients. Mean MTX dose increased from 15.0 mg/week to 16.1 mg/week. Changes in MTX regimen led to a better control of the disease activity as suggested by the decrease in DAS28-CRP and the increased proportion of patients with remission or low disease activity at the 6-month visit (from 22.2% to 52.3%). Quality of life significantly improved during the study in physical, symptoms and affect dimensions. There was no significant linear relationship between change in adherence to MTX and change in disease activity even when the analysis was restricted to patients with unchanged MTX dosing. This could be due to the mathematical properties of MMAS-8 which is not strictly continuous. The favorable effect of improved adherence may also have been hindered by the change in MTX bioavailability. Indeed, RA patients with inadequate clinical response to oral MTX may benefit from the higher drug exposure offered when switching to the SC formulation.6 When MTX dose is maintained stable, the change of route may correspond to a bioequivalent increase of more than 6 mg MTX per week.10 Unfortunately, MTX bioavailability has not been measured in the study and we cannot be more affirmative. However, RA activity and quality of life improved in a similar way when the analysis was restricted to patients with maintained or decreased MTX dose when MTX route has been changed. Higher MTX doses, better adherence and potentially improved bioavailability probably acted in combination to decrease RA activity and to improve patients’ quality of life. Switch to SC MTX has been motivated by sparing corticosteroids in 44 (21.3%) of patients. Among them, MTX dose was increased at the time of switch in 16 patients (36.4%).
Albeit improved during the study, adherence remained low at the 6-month follow-up visit with no more than 58% of strongly adherent patients. Replacing partially missing data in the MMAS-8 by the worst possible value may have contributed to these results. To the best of our knowledge, evidence from real life settings highlighting the switch to the use of SC MTX and the improvement of patient’s adherence is scarce. Current references are rather based on expert recommendations.17,18 One originality of the APRIM study was to provide contemporary longitudinal data addressing this point. Overall, these results are in line with recently published results36 with adherence to RA therapy not exceeding 66%.14 In a study conducted in US RA patients, 42% reported not taking their MTX treatment as prescribed mostly due to forgetfulness, feeling of not needing the treatment anymore after symptoms have improved and doubts or questions regarding long-term safety.37 In APRIM, the part of intentionality in non-adherence of 49.2% at baseline only slightly decreased over the study to 45.1% at the 6-month follow-up visit. Such findings leave some room for improvement. Shared decision-making is embedded as an overarching principle in most recommendations.5,16,38,39 Communication with the patient to clarify and agree on the treatment goal and the means to attain this goal is of utmost importance and enhances adherence.16,39,40 Patients exhibit a complex range of beliefs regarding DMARD therapy41,42 whose misinterpretations may complicate a shared decision-making approach and impair adherence.43 For example, patients have frequent fears after reading the package insert or due to social media. This should be addressed by an open, balanced and reassuring discussion.1
Physicians overestimated the patient adherence to MTX. Various tools have been proposed to estimate adherence from the measure of blood concentration of MTX glutamate, medication event monitoring systems (MEMS) recording openings of jars containing pills or use of injection pens, and various questionnaires. Considering MEMS as a gold standard, Pasma et al. found no or weak correlation between compliance questionnaire and MTX polyglutamate concentration in a population of patients with RA.44 The discrepancy between MMAS-8 and the physician’s adherence assessment may be partly due to the recall period. One MMAS-8 item refers to the day before and another one to the previous two weeks; there is no recall period for the remaining 6 items. On the other hand, physician assessment referred to the whole study duration.
This study has evident limitations due to its observational nature. It was conducted by a sample of 100 French rheumatologists mostly in private settings. We cannot assure this sample is representative of all French rheumatologists. Physicians were asked to enroll consecutive patients, but a selection bias cannot be ruled out. Furthermore, potential cognitive effect from participating in the study on the overall compliance of the patient may not be excluded. Such effect is largely discussed but has been described as temporary and of relatively short duration.45 Here, patients were followed for 6 months but were left alone without reminders or questionnaires to fill in until the final evaluation, thus limiting the feeling of being observed. It is likely that by the end of the follow-up period, the patient’s natural habits were developed. Despite the absence of a control group, the improvement in disease activity over the study is likely to be related to change in MTX regimen.
Conclusion
Overall, change from oral to SC route improved adherence to MTX, RA control and quality of life independently of change in MTX dose. Switch from oral to SC route can be considered as a part of the Treat-to-Target strategy as demonstrated by the better control of RA.
Acknowledgments
The authors thank Karen Tayarani, Universal Medica for the study management and the analysis of MMAS-8. Use of the ©MMAS is protected by US copyright and registered trademark laws. Permission for use is required. A license agreement is available from: MMAR, LLC., Donald E. Morisky, 294 Lindura Court, Las Vegas, NV 89138-4632; [email protected].
Funding
The study has been sponsored by NORDIC Pharma.
Disclosure
RMF received honoraria from NORDIC Pharma for the study coordination. ES and ST received honoraria from Nordic for scientific advice. PC and YF work as independent statisticians and have no conflict of interest to declare. AC, HHD and EZ are employed by NORDIC Pharma. The authors report no other conflicts of interest in this work.
References
1. Taylor PC, Balsa Criado A, Mongey AB, Avouac J, Marotte H, Mueller RB. How to get the most from methotrexate (MTX) treatment for your rheumatoid arthritis patient?-MTX in the treat-to-target strategy. J Clin Med. 2019;8(4). doi:10.3390/jcm8040515
2. Kruger K, Wollenhaupt J, Albrecht K, et al. [German 2012 guidelines for the sequential medical treatment of rheumatoid arthritis. Adapted EULAR recommendations and updated treatment algorithm]. Z Rheumatol. 2012;71(7):592–603. German. doi:10.1007/s00393-012-1038-0
3. O’Dell JR, Curtis JR, Mikuls TR, et al. Validation of the methotrexate-first strategy in patients with early, poor-prognosis rheumatoid arthritis: results from a two-year randomized, double-blind trial. Arthritis Rheum. 2013;65(8):1985–1994. doi:10.1002/art.38012
4. Weinblatt ME. Methotrexate in rheumatoid arthritis: a quarter century of development. Trans Am Clin Climatol Assoc. 2013;124:16–25.
5. Daien C, Hua C, Gaujoux-Viala C, et al. Update of french society for rheumatology recommendations for managing rheumatoid arthritis. Joint Bone Spine. 2018.
6. Schiff MH, Jaffe JS, Freundlich B. Head-to-head, randomised, crossover study of oral versus subcutaneous methotrexate in patients with rheumatoid arthritis: drug-exposure limitations of oral methotrexate at doses >/=15 mg may be overcome with subcutaneous administration. Ann Rheum Dis. 2014;73(8):1549–1551. doi:10.1136/annrheumdis-2014-205228
7. Osman A, Mulherin D. Is parenteral methotrexate worth trying? Ann Rheum Dis. 2001;60(4):432. doi:10.1136/ard.60.4.432
8. Bingham SJ, Buch MH, Lindsay S, Pollard A, White J, Emery P. Parenteral methotrexate should be given before biological therapy. Rheumatology. 2003;42(8):1009–1010. doi:10.1093/rheumatology/keg246
9. Braun J, Kastner P, Flaxenberg P, et al. Comparison of the clinical efficacy and safety of subcutaneous versus oral administration of methotrexate in patients with active rheumatoid arthritis: results of a six-month, multicenter, randomized, double-blind, controlled, Phase IV trial. Arthritis Rheum. 2008;58(1):73–81. doi:10.1002/art.23144
10. Pichlmeier U, Heuer KU. Subcutaneous administration of methotrexate with a prefilled autoinjector pen results in a higher relative bioavailability compared with oral administration of methotrexate. Clin Exp Rheumatol. 2014;32(4):563–571.
11. Rutkowska-Sak L, Rell-Bakalarska M, Lisowska B. Oral vs. subcutaneous low-dose methotrexate treatment in reducing gastrointestinal side effects. Reumatologia/Rheumatology. 2009;47(4):207–211.
12. Chakravarty K, McDonald H, Pullar T, et al. BSR/BHPR guideline for disease-modifying anti-rheumatic drug (DMARD) therapy in consultation with the British Association of Dermatologists. Rheumatology. 2008;47(6):924–925. doi:10.1093/rheumatology/kel216a
13. Contreras-Yanez I, Ponce De Leon S, Cabiedes J, Rull-Gabayet M, Pascual-Ramos V. Inadequate therapy behavior is associated to disease flares in patients with rheumatoid arthritis who have achieved remission with disease-modifying antirheumatic drugs. Am J Med Sci. 2010;340(4):282–290. doi:10.1097/MAJ.0b013e3181e8bcb0
14. Scheiman-Elazary A, Duan L, Shourt C, et al. The rate of adherence to antiarthritis medications and associated factors among patients with rheumatoid arthritis: a systematic literature review and metaanalysis. J Rheumatol. 2016;43(3):512–523. doi:10.3899/jrheum.141371
15. Mazaud C, Fardet L. Relative risk of and determinants for adverse events of methotrexate prescribed at a low dose: a systematic review and meta-analysis of randomized placebo-controlled trials. Br J Dermatol. 2017;177(4):978–986. doi:10.1111/bjd.15377
16. Gossec L, Molto A, Romand X, et al. Recommendations for the assessment and optimization of adherence to disease-modifying drugs in chronic inflammatory rheumatic diseases: a process based on literature reviews and expert consensus. Joint Bone Spine. 2019;86(1):13–19. doi:10.1016/j.jbspin.2018.08.006
17. Pavy S, Constantin A, Pham T, et al. Methotrexate therapy for rheumatoid arthritis: clinical practice guidelines based on published evidence and expert opinion. Joint Bone Spine. 2006;73(4):388–395. doi:10.1016/j.jbspin.2006.01.007
18. Bello AE, Perkins EL, Jay R, Efthimiou P. Recommendations for optimizing methotrexate treatment for patients with rheumatoid arthritis. Open Access Rheumatol. 2017;9:67–79. doi:10.2147/OARRR.S131668
19. Berlowitz DR, Pajewski NM, Kazis LE. Intensive blood-pressure treatment and patient-reported outcomes. N Engl J Med. 2017;377(21):2097. doi:10.1056/NEJMoa1611179
20. Bress AP, Bellows BK, King JB, et al. Cost-effectiveness of intensive versus standard blood-pressure control. New Engl J Med. 2017;377(8):745–755. doi:10.1056/NEJMsa1616035
21. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi:10.1111/j.1751-7176.2008.07572.x
22. Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: response to authors. J Clin Epidemiol. 2011;64(3):
23. van der Heijde DM, van ‘T Hof MA, van Riel PL, et al. Judging disease activity in clinical practice in rheumatoid arthritis: first step in the development of a disease activity score. Ann Rheum Dis. 1990;49(11):916–920. doi:10.1136/ard.49.11.916
24. Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–145. doi:10.1002/art.1780230202
25. Korb‐Savoldelli V, Gillaizeau F, Pouchot J, et al. Validation of a French version of the 8‐item Morisky medication adherence scale in hypertensive adults. J Clin Hypertens. 2012;14(7):429–434. doi:10.1111/j.1751-7176.2012.00634.x
26. Gadallah MA, Boulos DN, Dewedar S, Gebrel A, Morisky DE. Assessment of rheumatoid arthritis patients’ adherence to treatment. Am J Med Sci. 2015;349(2):151–156. doi:10.1097/MAJ.0000000000000376
27. Guillemin F, Coste J, Pouchot J, Ghezail M, Bregeon C, The SJ. AIMS2-SF: a short form of the arthritis impact measurement scales 2. french quality of life in rheumatology group. Arthritis Rheum. 1997;40(7):1267–1274. doi:10.1002/1529-0131(199707)40:7<1267::AID-ART11>3.0.CO;2-L
28. Ward MM, Guthrie LC, Alba MI. Clinically important changes in individual and composite measures of rheumatoid arthritis activity: thresholds applicable in clinical trials. Ann Rheum Dis. 2015;74(9):1691–1696. doi:10.1136/annrheumdis-2013-205079
29. Brown PM, Pratt AG, Isaacs JD. Mechanism of action of methotrexate in rheumatoid arthritis, and the search for biomarkers. Nat Rev Rheumatol. 2016;12(12):731–742.
30. Herman RA, Veng-Pedersen P, Hoffman J, Koehnke R, Furst DE. Pharmacokinetics of low-dose methotrexate in rheumatoid arthritis patients. J Pharm Sci. 1989;78(2):165–171. doi:10.1002/jps.2600780219
31. Lebbe C, Beyeler C, Gerber NJ, Reichen J. Intraindividual variability of the bioavailability of low dose methotrexate after oral administration in rheumatoid arthritis. Ann Rheum Dis. 1994;53(7):475–477. doi:10.1136/ard.53.7.475
32. Hoekstra M, Haagsma C, Neef C, Proost J, Knuif A, van de Laar M. Bioavailability of higher dose methotrexate comparing oral and subcutaneous administration in patients with rheumatoid arthritis. J Rheumatol. 2004;31(4):645–648.
33. Stamp LK, Barclay ML, O’Donnell JL, et al. Effects of changing from oral to subcutaneous methotrexate on red blood cell methotrexate polyglutamate concentrations and disease activity in patients with rheumatoid arthritis. J Rheumatol. 2011;38(12):2540–2547. doi:10.3899/jrheum.110481
34. Dervieux T, Zablocki R, Kremer J. Red blood cell methotrexate polyglutamates emerge as a function of dosage intensity and route of administration during pulse methotrexate therapy in rheumatoid arthritis. Rheumatology. 2010;49(12):2337–2345. doi:10.1093/rheumatology/keq216
35. Dervieux T, Furst D, Lein DO, et al. Pharmacogenetic and metabolite measurements are associated with clinical status in patients with rheumatoid arthritis treated with methotrexate: results of a multicentred cross sectional observational study. Ann Rheum Dis. 2005;64(8):1180–1185. doi:10.1136/ard.2004.033399
36. De Cuyper E, De Gucht V, Maes S, Van Camp Y, De Clerck LS. Determinants of methotrexate adherence in rheumatoid arthritis patients. Clin Rheumatol. 2016;35(5):1335–1339. doi:10.1007/s10067-016-3182-4
37. DiBenedetti DB, Zhou X, Reynolds M, Ogale S, Best JH. Assessing methotrexate adherence in rheumatoid arthritis: a cross-sectional survey. Rheumatol Ther. 2015;2(1):73–84. doi:10.1007/s40744-015-0011-1
38. Singh JA, Saag KG, Bridges SL
39. Smolen JS, Landewe R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–977. doi:10.1136/annrheumdis-2016-210715
40. Viller F, Guillemin F, Briancon S, Moum T, Suurmeijer T, van den Heuvel W. Compliance to drug treatment of patients with rheumatoid arthritis: a 3 year longitudinal study. J Rheumatol. 1999;26(10):2114–2122.
41. Fraenkel L, Nowell WB, Michel G, Wiedmeyer C. Preference phenotypes to facilitate shared decision-making in rheumatoid arthritis. Ann Rheum Dis. 2018;77(5):678–683. doi:10.1136/annrheumdis-2017-212407
42. Goodacre LJ. Factors influencing the beliefs of patients with rheumatoid arthritis regarding disease-modifying medication. Rheumatology. 2004;43(5):583–586. doi:10.1093/rheumatology/keh116
43. Gossec L, Berenbaum F, Chauvin P, et al. Development and application of a questionnaire to assess patient beliefs in rheumatoid arthritis and axial spondyloarthritis. Clin Rheumatol. 2018;37(10):2649–2657. doi:10.1007/s10067-018-4172-5
44. Pasma A, den Boer E, van ‘T Spijker A, et al. Nonadherence to disease modifying antirheumatic drugs in the first year after diagnosis: comparing three adherence measures in early arthritis patients. Rheumatology. 2016;55(10):1812–1819. doi:10.1093/rheumatology/kew247
45. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi:10.1016/j.jclinepi.2013.08.015
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.