Back to Journals » Orthopedic Research and Reviews » Volume 12
Being Underweight Is Associated with Worse Surgical Outcomes of Total Knee Arthroplasty Compared to Normal Body Mass Index in Elderly Patients
Authors Kwon HM, Han CD, Yang IH, Lee WS , Kim CW, Park KK
Received 23 December 2019
Accepted for publication 24 March 2020
Published 5 April 2020 Volume 2020:12 Pages 53—60
DOI https://doi.org/10.2147/ORR.S243444
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Hyuck Min Kwon, Chang Dong Han, Ick-Hwan Yang, Woo-Suk Lee, Chan Woo Kim, Kwan Kyu Park
Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea
Correspondence: Kwan Kyu Park
Department of Orthopedic Surgery, Yonsei University, College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea
Tel +82 2-2228-2180
Fax +82 2-363-1139
Email [email protected]
Purpose: Being underweight has never been studied in relation to the radiologic and clinical outcomes of total knee arthroplasty (TKA) in elderly patients. The aim of this study was to determine the effect of being underweight on TKA radiological and clinical outcomes and to investigate whether being underweight influences postoperative complications compared to normal body mass index (BMI) in elderly patients.
Patients and Methods: A total of 118 female patients aged 65 years or older with BMI < 25 kg/m2 who underwent primary TKA were divided into two groups based on BMI: group A: 18.5 kg/m2 < BMI < 25 kg/m2; group B: BMI < 18.5 kg/m2. The radiologic and clinical outcomes were evaluated at follow-up of 6, 12, and 24 months after surgery such as the hip-knee-ankle angle, the American Knee Society (AKS) score, Western Ontario and McMaster University score (WOMAC), and patellofemoral (PF) scale. Moreover, postoperative complications during follow-up were investigated.
Results: Preoperative clinical scores did not differ significantly between the two groups. Postoperative WOMAC pain (1.8 ± 1.9 versus 3.4 ± 2.6, p = 0.02), WOMAC function (12.4 ± 8.1 versus 16.5 ± 8.5, p = 0.012) and PF scales (26.1 ± 3.6 versus 23.7 ± 4.1, p = 0.002) were worse in the underweight group at 12 and 24 months after surgery. The frequency of postoperative complications did not differ significantly between groups. In multivariate linear regression analysis, underweight patient group was significantly associated with worse postoperative WOMAC and PF scores (p = 0.002, 0.005).
Conclusion: Although postoperative complications of TKA did not differ between groups, underweight patients had worse clinical outcomes of TKA compared to patients with normal BMI in elderly patients. Therefore, care should be taken when performing TKA in elderly underweight patients.
Keywords: total knee arthroplasty, clinical outcome, body mass index, underweight
Introduction
Obesity is closely related to the development of osteoarthritis and may be one of its main risk factors.1–3 Obesity in TKA patients is associated with poor clinical outcomes and increased early failure rates because obesity increases the mechanical stresses on the implant, as well as reactions by the surrounding bone.1,4,5 Since morbidity is related to obesity and increased complications, many orthopedic surgeons are concerned about the poor outcomes of TKA in obese patients.3,6-8 Despite concerns about the negative effects of obesity on TKA, many studies have found no difference in the clinical outcomes, rehabilitation, complication rate, and survival rate of TKA between obese and non-obese patients.9–11 Studies on the effect of BMI on the outcomes of TKA have primarily focused on obesity. However, poor nutritional status and sarcopenia of the quadriceps muscle could also influence the clinical outcomes of TKA, and these variables are closely related to low body mass index (BMI).12–14 In many cases, the being underweight in elderly patients is often associated with the patient’s frailty, which may indicate a poor quality of life for the patient.15 Several studies suggested that being underweight in elderly patients could be a predictor of various unhealthy conditions such as undernutrition, worse cognitive status or depression as well as functional disability.16–18 Therefore, TKA in elderly underweight patients could have poor surgical outcomes.
BMI is an easy and widely used measurement of obesity that correlates with total body fat.19 According to World Health Organization (WHO) classification of BMI, obesity is defined as BMI ≥ 30 kg/m2, and overweight is defined as BMI ≥ 25 kg/m2, and underweight is defined as BMI < 18 kg/m2. In Asia, few patients exhibit Western-style obesity, yet quite a few patients who are normal or underweight have TKA. Nevertheless, studies on the effect of BMI on the outcomes of TKA have so far focused on obesity. Although some studies have shown that being underweight has disadvantages in postoperative anemia and cost in total joint arthroplasty compared to morbid obesity, little has been studied on the effect of being underweight in TKA.20
Therefore, we aimed to determine the effect of being underweight on clinical and radiologic outcomes of TKA and to investigate whether being underweight influences postoperative complications compared to normal BMI in elderly patients. We hypothesized that elderly underweight patients would have poor clinical outcomes of TKA because being underweight might be often associated with poor nutrition status and sarcopenia, indirectly leading to poor clinical outcomes.21,22
Patients and Methods
Patient Recruitment and Study Design
For this retrospective comparative study, we recruited a total of 298 female patients who underwent unilateral TKA between March 2012 and December 2016. We included a total of 118 female patients aged 65 years or older with BMI < 25 kg/m2 who underwent unilateral TKA and completed at least 2 years of follow-up. Patients with lower extremity deformities, such as severe varus or valgus knee deformity more than 15 degrees, and those who required osteotomy together with TKA or special implants, such as varus or valgus constraint, revision surgery, secondary osteoarthritis, or inflammatory osteoarthritis, including rheumatoid arthritis, were not included in this study. All of the recruited patients were women, and the mean age was 70 years (range, 65–84 years). Mean BMI was 22.7 kg/m2 (range, 17.3–24.9 kg/m2). The BMI of patients was calculated based on height and weight measured by an electronic device on the day before surgery. Preoperative serum levels of albumin, hemoglobin, C-reactive protein (CRP), and total cholesterol were investigated and the manual test of quadriceps strength were evaluated. Patients were divided into two groups to compare underweight and normal BMI according to WHO classification of BMI: group A had 77 patients with BMI greater than or equal to 18.5 kg/m2 and lower than 25 kg/m2; and group B had 41 patients with BMI lower than 18.5 kg/m2. We retrospectively reviewed pre- and postoperative clinical information and radiologic findings on the 118 patients who were enrolled in this study, and the differences between the groups were compared. Sample sizes were estimated based on a previous study of patient-report outcomes for total knee arthroplasty in relation to BMI.23 Using values reported therein, an alpha of 0.05, a statistical power of 90%, and a drop rate of 20%, the sample size of each group was calculated at 30 patients, giving us a number of 60 as a minimum total number of subjects required for this study.
TKA Procedure and Clinical Outcomes
All procedures were performed by a single surgeon using the standard medial patellar approach with tourniquet inflation and the measured resection technique, including selective soft tissue release. A posteriorly stabilized prosthesis (LPS-Flex Gender Knee, Zimmer, Warsaw, IN, USA) was implanted in all patients. The patella was not resurfaced in all cases, and cement fixation was used for all components.
All clinical information was collected using predesigned datasheets in the outpatient clinic pre- and postoperatively and was maintained in our database by an independent investigator. The clinical information included demographic data, preoperative clinical status, and postoperative outcomes. The preoperative clinical status and postoperative outcomes were evaluated with the following at 6, 12, and 24 months after surgery: arc of motion of the knee, American Knee Society (AKS) score,24 Western Ontario McMaster University Osteoarthritis Index scale (WOMAC),25,26 and the Kujala patellofemoral score.27 The arc of motion of the knee was represented by maximum flexion and range of motion (ROM), which was calculated by subtracting the degree of flexion contracture from the degree of maximum flexion. An independent investigator used a goniometer to measure flexion contracture and maximum flexion to the nearest 5°, with the patient in the supine position.28 At 24 months after surgery follow-up visits, radiologic outcomes were evaluated such as hip-knee-ankle angle and loosening of implant.
Statistics
All statistical analyses were performed with SPSS version 20 for Windows (SPSS Inc., Chicago, IL, USA), and p values <0.05 were considered statistically significant. Mean and standard deviations were calculated to describe characteristics. Student t-test was used for between-group comparison of continuous data. And, Chi-squared test of Fisher exact test was used to compare categorical data. A multivariate linear regression analysis was used to determine whether BMI group impacted postoperative clinical outcomes while controlling for multiple variables.
Results
In all patients, the degree of degenerative osteoarthritis was Kellgren-Lawrence grade III or IV. The mean follow-up period was 2.3 years. Table 1 compares pre- and postoperative clinical data between groups. There was no significant difference in age, hip-knee-ankle (HKA) angle, serum levels of CRP, and total cholesterol between two groups (p > 0.05). However, serum levels of albumin and hemoglobin of underweight patients were lower than patients with normal BMI (albumin, 4.2 ± 0.6 vs 3.8 ± 0.5, p=0.02; hemoglobin, 13.7 ± 1.0 vs 12.8 ± 1.5, p<0.001). The manual test of quadriceps strength was better in the normal BMI group (4.8 ± 0.6 vs 4.5 ± 0.8, p=0.044). There was no significant difference in preoperative flexion contracture, ROM of the knee, AKS, WOMAC and PF scores between two groups. Table 2 and Figure 1 show comparison of postoperative clinical outcomes between two groups at 6, 12, and 24 months after surgery. At 6 months after surgery, there was no significant difference in clinical outcomes of two groups. However, postoperative WOMAC pain score (group A, 1.8 ± 1.9; group B, 3.4 ± 2.6, p = 0.02, effect size d = 0.70), WOMAC function score (group A, 12.4 ± 8.1; group B, 16.5 ± 8.5, p = 0.012, effect size d = 0.49), and PF scales (group A, 26.1 ± 3.6; group B, 23.7 ± 4.1, p = 0.002, effect size d = 0.62) were worse in the underweight group at 12 and 24 months after surgery. Effect sizes were moderate for these postoperative WOMAC pain scores, WOMAC function scores, and PF scales. No other significant differences were found between groups (p > 0.05).
 |
Table 1 Comparison of Demographics and Preoperative Evaluation Between the Two Groups |
 |
Table 2 Comparison of Postoperative Outcomes of TKA Between Two Groups |
Multivariate linear regression analysis controlling for age, preoperative HKA angle, preoperative serum level of albumin, hemoglobin, total cholesterol, CRP, quadriceps strength, preoperative clinical status (AKS, WOMAC, PF scores) demonstrated that BMI group was significantly associated with postoperative WOMAC and PF scores. Table 3 summarizes the output of the linear regression analysis.
Table 4 summarizes all complications associated with TKA. The two groups did not differ in the rate of postoperative complications (p=0.294). There were 7 cases of superficial wound problems, including wound dehiscence and superficial wound infection with no organism confirmed; this included 4 cases in the group A (18.5≤BMI<25 kg/m2), 3 cases in the group B (BMI < 18.5 kg/m2). Only 1 patient developed deep infection and need revision surgery; this patient was in the group B. 3 cases of peri-operative morbidity occurred in the group A, including 1 cases of hypovolemic shock, 1 cases of deep vein thrombosis, and 1 case of pneumonia. In the group B, 2 case of peri-operative morbidity occurred, including 1 case of hypovolemic shock and 1 case of deep vein thrombosis. No patients in between groups required revision surgery for aseptic failure.
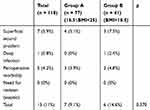 |
Table 4 Comparison of Complications in 118 Patients Who Underwent Total Knee Arthroplasty |
Discussion
The current study investigated whether being underweight affects the clinical outcomes of TKA in elderly patients. Since pain and discomfort of patients may still be present at 6 months after surgery, there was no significant difference in clinical outcomes for TKA between BMI groups at that time. However, we discovered that being underweight could influence the early postoperative clinical outcomes of TKA at 2 years after surgery. Although there was no significant difference in early postoperative complications and radiologic outcomes between the study groups, postoperative WOMAC pain score, WOMAC function score, and PF scales at 2 years after surgery reflected worse clinical outcomes in the underweight group than the normal BMI group, and the effect size was moderate.
Numerous studies have focused on the influence of obesity on the morbidity and clinical outcomes of TKA, probably because there are few underweight patients with osteoarthritis in Western countries.1,3,6,29-31 However, many patients with osteoarthritis are underweight in Asia, and being underweight in the elderly patients could be predictor of functional disability, so it is also important to determine the clinical outcomes of underweight elderly patients who have TKA. This is the first study to assess the effect of being underweight on clinical and radiologic outcomes of TKA. In many older female patients, being underweight might be associated with sarcopenia or nutritional deficiencies as well as worse cognitive status or depression16,21,22 In addition, there have been several studies explaining the underweight of elderly patients with chronic pain, osteoporosis, and the associated frailty, which may be related to the worse outcomes of TKA.15,32 Several studies have shown that patients with severe degenerative osteoarthritis can experience depression and anorexia after TKA due to pain and limitation of knee function, factors that might be closely related to poor nutritional status.33,34 Poor nutritional status may affect both peri-operative morbidity and postoperative recovery of general conditions.35 Low serum levels of albumin and hemoglobin in underweight patients of our study might suggest indirectly poor nutrition status. In addition, there was a mild decrease in quadriceps strength in underweight patients. Since sarcopenia is a risk factor for poor rehabilitation of knee function and postoperative infection after TKA,36,37 the decrease of quadriceps strength might cause worse clinical outcomes. However, it is difficult to say that mild decrease in quadriceps strength is the main cause of worse clinical outcome, as it could have resulted from a combination of many factors, such as poor nutrition and frailty. Since we confirmed that underweight elderly patients had worse clinical outcomes after TKA compared to patients with normal BMI, surgeons should be aware that outcomes may not be good when considering TKA for underweight elderly patients. Since being underweight might be associated with sarcopenia and poor nutrition status, additional studies including evaluations of nutritional status or quantified sarcopenia of patients are required.
Fibrosis and inflammation caused by soft tissue impingement and overhang of the implant might cause increased postoperative knee pain and discomfort after TKA.38,39 Although we could not clarify the relationship between overhang of the implant or impingement and being underweight, we confirmed that postoperative PF scales associated with anterior knee pain were higher in underweight patients. For these reasons, underweight patients can experience poor clinical outcomes after TKA due to fibrosis and inflammation induced by soft tissue impingement and overhang of the implant. Further studies of this are needed. In addition, although the risk of a common wound complication may be higher in obese patients, the risk of a wound complication might also be high in patients who are so thin that they lack proper soft tissue for sutures. Thus, underweight patients should undergo proper evaluation of the soft tissue around the knee before surgery.
There were several limitations to our study. First, this study was designed as a retrospective cohort study, and the follow-up period was relatively short, with clinical outcomes assessed at 2 to 3 years after surgery. Although we confirmed that early clinical outcomes differed significantly between the groups, longer-term study is needed. This will facilitate comparison with long-term studies of the obesity-related outcomes of TKA. In addition, selection bias may be present because only patients who were followed up for at least 2 years were enrolled. Second, we did not evaluate other risk factors that could affect the clinical outcomes of TKA, such as age, comorbidities and pain in other joints or the back; only BMI was considered. An age- and sex-matched study that excludes other comorbidities and pain could provide more accurate information on the relationship between being underweight and the clinical outcomes of TKA. In addition, there was no information on comorbidities and frailty diagnosis, which may lead to being underweight. Finally, we evaluated the effect of being underweight in an all-female cohort, and only one type of implant (posterior substituting and fixed bearing type TKA) was used in this study, as we analyzed only primary TKA cases. Using different types of implants (cruciate retaining) may lead to different results. In Asia, women are more likely to undergo TKA than men, and most underweight patients are women. Therefore, the results of this study should be applied with caution to different patient groups or types of implant. Although obese patients are more common than underweight patients, and obesity is generally known to be associated with worse clinical outcomes, complications, and survival rates after TKA, we found that underweight elderly patients with BMI lower than 18.5 kg/m2 also had worse clinical outcomes. Therefore, orthopedic surgeons should consider the risk of poor outcomes of TKA in underweight elderly patients as well as obese patients.
Conclusion
The complication rate of TKA did not differ significantly between underweight elderly patients with (<18.5 kg/m2) and those with normal (18.5 kg/m2 ≤ BMI < 25 kg/m2) in the current study. However, postoperative WOMAC pain score, WOMAC function score, and PF scales at 2 years after surgery showed worse clinical outcomes in the underweight group than in the normal BMI group, and the effect size was moderate. Since underweight elderly patients (<18.5 kg/m2) could have worse clinical outcomes after TKA, orthopedic surgeons performing TKA in underweight elderly patients should use caution to ensure appropriate preoperative evaluation and careful intraoperative procedures.
Abbreviations
BMI, Body Mass Index; TKA, Total Knee Arthroplasty; AKS score, American Knee Society score; WOMAC score, Western Ontario and McMaster University score; PF scale, Patellofemoral scale; WHO, World Health Organization; ROM, Range of Motion; HKA angle, hip-knee-ankle angle; CRP, C-reactive protein.
Data Sharing Statement
The datasets generated and/or analyzed during the current study that involve patient data are not publicly available because this was not established, nor would it have been accepted, as part of the ethics application.
Ethics and Consent Statement
This retrospective study was approved by the Institutional Review Board of Severance Hospital (date of approval December 31, 2018; IRB number 4-2018-1055). Since this study was a retrospective comparative study, informed consent was waived by the ethics committee. All patient data were anonymously analyzed. Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Disclosure
The authors report no funding and no conflicts of interest in this work.
References
1. Sridhar MS, Jarrett CD, Xerogeanes JW, Labib SA. Obesity and symptomatic osteoarthritis of the knee. J Bone Joint Surg Br. 2012;94(4):433–440. doi:10.1302/0301-620X.94B4.27648
2. Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109(1):18–24. doi:10.7326/0003-4819-109-1-18
3. Kulkarni K, Karssiens T, Kumar V, Pandit H. Obesity and osteoarthritis. Maturitas. 2016;89:22–28. doi:10.1016/j.maturitas.2016.04.006
4. Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3(1):51–61. doi:10.1016/0021-9290(70)90050-3
5. Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(7 Suppl 3):46–50. doi:10.1016/j.arth.2005.04.023
6. Jiganti JJ, Goldstein WM, Williams CS. A comparison of the perioperative morbidity in total joint arthroplasty in the obese and nonobese patient. Clin Orthop Relat Res. 1993;289:175–179.
7. Miric A, Lim M, Kahn B, Rozenthal T, Bombick D, Sculco TP. Perioperative morbidity following total knee arthroplasty among obese patients. J Knee Surg. 2002;15(2):77–83.
8. Maniar RN, Maniar PR, Singhi T, Gangaraju BK. WHO class of obesity influences functional recovery post-TKA. Clin Orthop Surg. 2018;10(1):26–32. doi:10.4055/cios.2018.10.1.26
9. Bonnefoy-Mazure A, Martz P, Armand S, et al. Influence of body mass index on sagittal knee range of motion and gait speed recovery 1-year after total knee arthroplasty. J Arthroplasty. 2017;32(8):2404–2410. doi:10.1016/j.arth.2017.03.008
10. Paterson KL, Sosdian L, Hinman RS, et al. Effects of sex and obesity on gait biomechanics before and six months after total knee arthroplasty: a longitudinal cohort study. Gait Posture. 2018;61:263–268. doi:10.1016/j.gaitpost.2018.01.014
11. Stickles B, Phillips L, Brox WT, Owens B, Lanzer WL. Defining the relationship between obesity and total joint arthroplasty. Obes Res. 2001;9(3):219–223. doi:10.1038/oby.2001.24
12. Burgess LC, Phillips SM, Wainwright TW. What is the role of nutritional supplements in support of total hip replacement and total knee replacement surgeries? A systematic review. Nutrients. 2018;10(7):7. doi:10.3390/nu10070820
13. Cao G, Huang Q, Xu B, Huang Z, Xie J, Pei F. Multimodal nutritional management in primary total knee arthroplasty: a randomized controlled trial. J Arthroplasty. 2017;32(11):3390–3395. doi:10.1016/j.arth.2017.06.020
14. Furu M, Ito H, Nishikawa T, et al. Quadriceps strength affects patient satisfaction after total knee arthroplasty. J Orthop Sci. 2016;21(1):38–43. doi:10.1016/j.jos.2015.10.002
15. Chen C, Winterstein AG, Fillingim RB, Wei YJ. Body weight, frailty, and chronic pain in older adults: a cross-sectional study. BMC Geriatr. 2019;19(1):143. doi:10.1186/s12877-019-1149-4
16. Estrella-Castillo DF, Gomez-de-Regil L. Comparison of body mass index range criteria and their association with cognition, functioning and depression: a cross-sectional study in Mexican older adults. BMC Geriatr. 2019;19(1):339. doi:10.1186/s12877-019-1363-0
17. Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48(4):445–469. doi:10.1016/S0277-9536(98)00370-0
18. Bahat G, Tufan A, Aydin Y, et al. The relationship of body mass index and the functional status of community-dwelling female older people admitting to a geriatric outpatient clinic. Aging Clin Exp Res. 2015;27(3):303–308. doi:10.1007/s40520-014-0291-2
19. Bray GA. Overweight is risking fate. Definition, classification, prevalence, and risks. Ann N Y Acad Sci. 1987;499:14–28. doi:10.1111/j.1749-6632.1987.tb36194.x
20. Sayeed Z, Anoushiravani AA, Chambers MC, et al. Comparing in-hospital total joint arthroplasty outcomes and resource consumption among underweight and morbidly obese patients. J Arthroplasty. 2016;31(10):2085–2090. doi:10.1016/j.arth.2016.03.015
21. Gonzalez-Montalvo JI, Alarcon T, Gotor P, et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. 2016;16(9):1021–1027. doi:10.1111/ggi.12590
22. Lainscak M, Filippatos GS, Gheorghiade M, Fonarow GC, Anker SD. Cachexia: common, deadly, with an urgent need for precise definition and new therapies. Am J Cardiol. 2008;101(11A):8E–10E. doi:10.1016/j.amjcard.2008.02.065
23. Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23(6):795–800. doi:10.1016/j.arth.2007.08.005
24. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248(248):13–14.
25. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840.
26. Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol. 1986;5(2):231–241. doi:10.1007/BF02032362
27. Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi:10.1016/S0749-8063(05)80366-4
28. Kwon HM, Yang IH, Lee WS, Yu ARL, Oh SY, Park KK. Reliability of intraoperative knee range of motion measurements by goniometer compared with robot-assisted arthroplasty. J Knee Surg. 2019;32(3):233–238. doi:10.1055/s-0038-1641140
29. Collins RA, Walmsley PJ, Amin AK, Brenkel IJ, Clayton RA. Does obesity influence clinical outcome at nine years following total knee replacement? J Bone Joint Surg Br. 2012;94(10):1351–1355. doi:10.1302/0301-620X.94B10.28894
30. Della Valle CJ. Body mass index and outcomes of TKA: insight for counseling patients: commentary on an article by Jamie E. Collins, PhD, et al: “effect of obesity on pain and functional recovery following total knee arthroplasty”. J Bone Joint Surg Am. 2017;99(21):e116. doi:10.2106/JBJS.17.00991
31. Collins JE, Donnell-Fink LA, Yang HY, et al. Effect of obesity on pain and functional recovery following total knee arthroplasty. J Bone Joint Surg Am. 2017;99(21):1812–1818. doi:10.2106/JBJS.17.00022
32. Shin JI, Keswani A, Lovy AJ, Moucha CS. Simplified frailty index as a predictor of adverse outcomes in total hip and knee arthroplasty. J Arthroplasty. 2016;31(11):2389–2394. doi:10.1016/j.arth.2016.04.020
33. Stubbs B, Aluko Y, Myint PK, Smith TO. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing. 2016;45(2):228–235. doi:10.1093/ageing/afw001
34. Ahn H, Weaver M, Lyon D, Choi E, Fillingim RB. Depression and pain in Asian and white Americans with knee osteoarthritis. J Pain. 2017;18(10):1229–1236. doi:10.1016/j.jpain.2017.05.007
35. Stowers MD, Lemanu DP, Coleman B, Hill AG, Munro JT. Review article: perioperative care in enhanced recovery for total hip and knee arthroplasty. J Orthop Surg (Hong Kong). 2014;22(3):383–392. doi:10.1177/230949901402200324
36. Babu JM, Kalagara S, Durand W, Antoci V, Deren ME, Cohen E. Sarcopenia as a risk factor for prosthetic infection after total hip or knee arthroplasty. J Arthroplasty. 2019;34(1):116–122. doi:10.1016/j.arth.2018.09.037
37. Devasenapathy N, Maddison R, Malhotra R, Zodepy S, Sharma S, Belavy DL. Preoperative quadriceps muscle strength and functional ability predict performance-based outcomes 6 months after total knee. Phys Ther. 2018. doi:10.1093/ptj/pzy118
38. Takahashi M, Miyamoto S, Nagano A. Arthroscopic treatment of soft-tissue impingement under the patella after total knee arthroplasty. Arthroscopy. 2002;18(4):E20. doi:10.1053/jars.2002.31968
39. Bonnin MP, Van Hoof T, De Kok A, et al. Imaging the implant-soft tissue interactions in total knee arthroplasty. J Exp Orthop. 2016;3(1):24. doi:10.1186/s40634-016-0061-5
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


