Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Behavioral Activation Therapy for Subthreshold Depression in Stroke Patients: An Exploratory Randomized Controlled Trial
Authors Sun Q, Xu H, Zhang W, Zhou Y, Lv Y
Received 5 October 2022
Accepted for publication 22 November 2022
Published 29 November 2022 Volume 2022:18 Pages 2795—2805
DOI https://doi.org/10.2147/NDT.S392403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Richard J Porter
Qiuxue Sun,1,* Hailian Xu,2,* Wenyue Zhang,3 Yuqiu Zhou,1 Yumei Lv1
1School of Nursing, Harbin Medical University (Daqing), Daqing, People’s Republic of China; 2School of Medical, Quzhou College of Technology, Quzhou, People’s Republic of China; 3Department of Rehabilitation, People’s Hospital of Daqing, Daqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yumei Lv, School of Nursing, Harbin Medical University (Daqing), No. 39 Xinyang Road, Longfeng District, Daqing, People’s Republic of China, Email [email protected]
Background: Subthreshold depression (SD) is known to be a major risk factor for the development of post-stroke depression (PSD). Appropriate intervention to prevent the transition from SD to PSD is thus imperative. As a form of short-term psychotherapy adapted for individuals with cognitive and communication impairments, behavioral activation therapy (BAT) may be a suitable choice. However, the effects of BAT on psychological outcomes in stroke patients with SD has not been established. This study investigated the feasibility and effectiveness of BAT in reducing the development of depressive symptoms in this patient population.
Methods: A double-blind, randomized controlled trial was performed. Seventy participants were randomized to either a BAT group (n=35) or a control group (n=35). Participants in the BAT group received a six-week BAT intervention. The feasibility of BAT was assessed by the number of sessions attended by participants, and the acceptability of BAT to participants and the incidence of adverse events were recorded. The primary clinical outcome measure was the Center for Epidemiological Studies Depression Scale (CES-D) and the 17-item Hamilton Depression Scale (HAMD-17) at baseline, six weeks, and three months after the group allocation. Secondary outcomes included behavioral activation and the incidence of depression.
Results: The intervention was feasible and acceptable, with 94.3% of participants in the BAT group (33 of 35) attending at least five sessions. No adverse events were reported in either group. Compared with the control group, the BAT group showed significant improvements in the CES-D (F=67.689, P< 0.05), HAMD-17 (F=4.170, P< 0.05), and behavioral activation (F=25.355, P< 0.05) scores after intervention, and these differences were maintained at the three-month assessment.
Conclusion: BAT appears to be feasible and efficacious for reducing depressive symptoms and increasing behavioral activation among stroke patients with SD. The findings of this study may contribute to the primary prevention of PSD.
Keywords: stroke, subthreshold depression, post-stroke depression, behavioral activation therapy
Introduction
Stroke is a common age-related disease that poses a significant threat to human health and is both the second leading cause of death and the main reason for disability.1 Researchers revealed that the prevalence of stroke in China increased by 13.2% from 2013 to 2019, and the annual increase rate was 2.2%.2 Stroke survivors may face a variety of complications like cognitive impairment and aphasia, or even affective disorder. While there are many emotional consequences of stroke, one of the most prevalent is depression. Post-stroke depression (PSD) can occur at every stage of the disease and is characterized by reduced motivation for rehabilitation and an increased incidence of adverse events.3,4 PSD thus poses a challenge for the rehabilitation of stroke patients. While there is evidence for the effective treatment of PSD, there is an opportunity to prevent depression before it occurs.5,6 Subthreshold depression(SD) is known to be a major risk factor for the development of PSD, it is well established that SD can also progress to PSD if not treated in time.7,8 Identifying and treating SD from the outset could thus help reduce the future incidence of PSD and its accompanying adverse effects.
SD is also relatively common, with estimates of 60% prevalence during the acute stroke episode and 38% in patients on discharge.9 SD has been conceptualized in multiple ways, with some researchers referring to it as an intermediate stage between an absence of clinically relevant depressive symptoms and a full clinical disorder.7,10 Studies have consistently reported that SD patients not only suffer from persistent depressive symptoms and reduced quality of life but also require more health services at greater economic cost.8,11
Early interventions for SD that can reduce the risk of developing depression have attracted wide attention. There is evidence that people with SD may benefit from appropriate low-intensity psychosocial interventions.12 There are various psychosocial intervention strategies for SD, mainly including cognitive behavioral therapy (CBT) and behavior activation therapy (BAT).13 While both CBT and BAT are effective in treating SD and could prevent its transformation to depression, CBT must be delivered by health professionals with adequate training, whereas BAT is much simpler and more cost-effective.12,14 BAT can also overcome the limitations of traditional psychological interventions in the selection of patients, and can be applied to patients with cognitive and communication impairments.15 Therefore, BAT may have the possible practical advantages for stroke patients with SD.
There has been a steady increase in the number of clinical trials assessing the efficacy of BAT in various populations. This has led to the use of BAT in treating the elderly, patients with diabetes and cancer, and adolescents with SD.14,16,17 While there is some support for BAT in treating PSD,15 there is little to no information regarding the effectiveness of BAT for SD in post-stroke patients nor have the long-term benefits of BAT been elucidated in this population. Therefore, in this present study, stroke patients with SD were enrolled and treated with BAT, aiming to evaluate the feasibility and effectiveness of BAT in reducing depressive symptoms and whether these benefits persisted until a three-month follow-up. We hypothesized that BAT would be effective for stroke patients with SD and would thus lead to significant improvement in the symptoms of depression.
Methods
Study Design
This study was an exploratory randomized controlled trial comparing BAT with standardized usual care, conducted between March and July 2022. Participants were recruited from a cross-sectional study (ie, the incidence and predictors of subthreshold depression in stroke patients) conducted in the departments of neurology and rehabilitation at a tertiary hospital between January and March 2022. Patients in the original sample (274 stroke patients) who met the current criteria were considered potential participants. The inclusion criteria were the following: stroke patients who 1) age 18 years or older; 2) the duration of the disease was less than 3 months; 3) had subthreshold symptoms of depression, CES-D score≥16, HAMD score between 7 and 17; no current PSD according to Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) criteria; 4) were able to travel to the hospital for weekly interventions and follow-up assessments; 5) provided informed consent. Exclusion criteria were: patients with severe cognitive impairment (MMSE<10), global aphasia, other major physical or psychiatric conditions, and who were taking antidepressant medication or participating in a clinical intervention to improve depression. Patients who met the eligibility criteria were planned to randomly assign 1:1 to either the BAT group or control group to receive the corresponding intervention for six weeks. Written informed consent was obtained prior to inclusion in the study. The study protocol was approved by the Ethics Committee of the Harbin Medical University (HMUDQ2021111502) and performed according to the Declaration of Helsinki. The clinical registered number: ChiCTR2200057721.
Procedure
We used three steps to recruit the participants. First, the participants who had participated in the cross-sectional study and who had a CES-D score ≥16 and a HAMD score between 7 and 17 were defined as the preliminary screening group. Second, the study coordinator screened the potential participants via telephone for eligibility and invited eligible patients to the hospital for a final screening. Third, the final screening was conducted by four trained and equally experienced researchers (two neurologists and two clinical psychologists). The potential participants were interviewed face to face in a constant environment and completed a questionnaire and a structured clinical interview for DSM (SCID).18 During the data collection process, the researcher read each item on the questionnaire and recorded the patient’s response. Finally, 70 participants were enrolled, which is larger than the minimum sample size recommended for feasibility studies.19 The participants were randomly allocated to the BAT and control groups by an independent trained assistant using a random number table. The information on the randomization was kept in sequentially numbered envelopes and the participants were blinded to their allocation until the end of the intervention. After randomization, a six-week BAT intervention was carried out in the psychological interview room at the hospital by a professor specializing in psychological therapy. Subsequent assessments were conducted at two time points (at the end of the intervention and three months after the random allocation) and were analyzed by two graduate students who were blinded to the grouping information and the trials. After the follow-up evaluations, the participants in the control group were able to receive the same BAT intervention. The entire study flow is illustrated in Figure 1.
 |
Figure 1 Study flow diagram: enrollment to analysis. Abbreviation: BAT, behavioral activation therapy. |
Interventions
The BAT Group
Participants allocated to the intervention group received a BAT program. The BAT program consisted of weekly 50-minute sessions for six consecutive weeks. All the sessions in the BAT program were developed based on the brief outline developed by Lejuez.20 This included the following: baseline assessment; determination of life goals; hierarchical task assignment; behavioral experiment; behavioral monitoring; elimination of barriers to behavioral activation; review of behavioral activation. The intervention schedule was relatively fixed and could be adjusted according to the patient’s specific case. The intervention process focused on the patient’s behavior, targeting and increasing activities that they enjoyed and valued and supporting a strong sense of control and satisfaction. The patient’s motivation to participate was assessed before each session to ensure that the patient could fully understand and accept BAT throughout the intervention process. The fidelity of the BAT intervention was assessed using therapy record forms for every session. Furthermore, in this process, we maintained a strong vigilance for the development of PSD or suicidal tendencies. See Table 1 for specific details.
 |
Table 1 Outline of Behavioral Activation Therapy |
The Control Group
All participants had unrestricted access to standardized usual care (rehabilitative training and psychoeducation) delivered by nurses, neurologists, rehabilitation therapists, and psychologists. Rehabilitative training consisted of six weekly 40-minute sessions for six weeks. Rehabilitation therapists standardized this training to ensure that the same intensity was provided to the two groups. Psychoeducation was carried out in the form of individual intervention, group discussion, and distribution of health brochures, once a week for six weeks and for 15–30 minutes each time. During the intervention period, the control group participants received no additional mental health intervention.
Measures
Feasibility Criterion
The measures related to the feasibility of BAT were the following: the number of sessions attended by the participants; the acceptability of BAT to the participants; the incidence of adverse events. Participants completed an anonymous questionnaire via the internet after the intervention. The questionnaire included three items that collected relevant information about the acceptability of the intervention to the participant: 1) Do you think that the therapy sessions are acceptable? 2) Would you recommend this therapy to other patients with subthreshold depression? 3) Are there any comments or suggestions you would like to share with us?
Clinical Outcomes
Primary Outcome
The Center for Epidemiological Studies Depression Scale (CES-D)
The CES-D consists of 20 self-reported items that are rated on a four-point scale and scored as never (0) to almost all the time (3), with scores ranging from 0 to 60. Scores from 0 to 15 indicated normal, scores from 16 to 19 suggested the possibility of depression, and scores above 20 indicated depression. Good reliability and validity have been reported for the use of the CES-D for Chinese stroke survivors.21
The 17-Item Hamilton Depression Scale (HAMD-17)
The HAMD-17 consists of 17 items that assess the severity of depression symptoms. Nine of the items are rated from 0 to 4 (0 = none; 1 = suspicious or slight; 2 = mild; 3 = medium; 4 = severe), eight items are rated from 0 to 2 (0 = none, 1 = suspicious or mild; 2 = obviously present). Scores from 0 to 7 indicated normal, scores from 8 to 16 suggested the possibility of depression, whereas scores above 17 indicated depression. HAMD-17 has been tested among Chinese patients and revealed good reliability and validity.22
Secondary Outcome
The Behavioral Inhibition/Behavioral Activation System Scales (BIS/BAS)
The Chinese version of BIS/BAS was translated by Li et al23 and has been well-validated. The BIS subscale consists of five items that assess the dispositional sensitivity to punishment, whereas the BAS subscale (13 items, scores ranging from 13 to 52) assesses approach behaviors, with higher scores reflecting stronger behavioral activation.
Statistical Analysis
The data were processed and analyzed using IBM SPSS 20.0. Dichotomous variables were compared by chi-square test. Continuous variables were compared by independent sample t-test or Wilcoxon test. The effectiveness of BAT at different time points were analyzed by repeated measures ANOVA. The significant level of all statistical tests was set at 0.05.
Results
Participant Characteristics
A total of 70 stroke patients with SD were included in the study (intervention group, n=35; control group, n= 35). One participant in the BAT group and one in the control group who underwent other psychological treatments during the intervention were excluded. At follow-up, one BAT group participant and two participants in the control group did not complete the rating scales. Overall, 65 participants (92.9%) participated in the follow-up interviews. There were no significant differences between patients who were included in the analysis or who were not included. Table 2 displays the detailed comparison of characteristics. In brief, there were no differences between the BAT and control group.
 |
Table 2 Characteristics of Participants by Group (n = 65) |
Feasibility Outcomes
In all, 94.3% of participants in the BAT group (33 of 35) attended at least five sessions and 77% (27 of 35) attended all the sessions. The sessions lasted for a mean of 52 minutes, and the delivery of the intervention was good, with high attendance. The main reasons for intervention participants missing sessions were illness and time conflict. A total of 30 participants completed the anonymous questionnaire survey through the internet, with all stating that the intervention was acceptable and that they would recommend it to others. They were generally positive about their experiences during the intervention and found that goal-setting or activity scheduling during the sessions was helpful. Several participants reported having some trouble with filling out the activity logs and completing the homework. No adverse events were reported in either group.
The Subthreshold Depression Outcome Between Two Groups
We assessed the rates of SD and PSD between the BAT group (n=33) and the control group (n=32) based on the SCID. The incidence of both SD and PSD was lower in the BAT group than in the control group. Four participants (12.12%) in the BAT group developed PSD during follow-up, while 10 control group participants (31.25) met the criteria for PSD. We applied Fisher’s exact test to analyze the differences between the two groups (Table 3).
 |
Table 3 Depression Outcome by Group at 3-Month Follow-Up (n=65) |
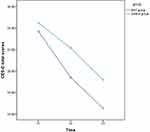
Effectiveness of the Intervention
A series of two (group) by two (time) repeated measures ANOVA were conducted to examine the changes across time between the BAT and control groups in the CES-D, HAMD-17, and BAS scores. Table 4 shows the descriptive statistics with the mean scores of the outcome measures at the three time points and the significance of time and time-group interactions. Figures 2–4 provide a graphical representation of the changes in the CES-D, HAMD-17, and BAS scores between the two groups over time. As shown in Figures 2 and 3, the decreases in CES-D and HAMD-17 scores from baseline to follow-up were greater in the BAT group as compared with the control group, and there was a significant main effect of group (both P<0.001, Table 4). In addition, the BAS scores improved significantly in the BAT group, with the results showing a significant difference in terms of both time and group (Figure 4, Table 4).
 |
Table 4 Impact of the Intervention on Outcome Measures at Three Time-Points |
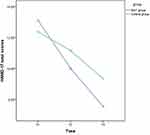 |
Figure 3 HAMD-17 scores for two groups on T1, T2, and T3. Abbreviations: HAMD-17, 17-item Hamilton Depression Scale; T1, baseline; T2, six weeks; T3, three months after the group allocation. |
 |
Figure 4 BAS scores for two groups on T1, T2, and T3. Abbreviations: BAS, Behavioral Activation System Scales; T1, baseline; T2, six weeks; T3, three months after the group allocation. |
Discussion
To the best of our knowledge, this is a rare study to evaluate the feasibility of BAT for use in stroke patients with SD. The present study demonstrated both the feasibility and effectiveness of BAT in these patients, finding significant improvements in the outcome measures, namely, the CES-D, HAMD-17, and BAS scores. At the same time, the study showed an SD incidence of 27.4% (75 of the 274 patients) within the first three months following the stroke. This is higher than that reported in the general population.24 We are of the view that the first three months after stroke are a period of particular vulnerability and suggest that health service departments should pay more attention to this population. Previous evidence has also suggested that the incidence of depression varies over time with an obvious peak between three and six months after stroke.25 Timely identification and predictive intervention implemented in the early phase could reduce the risk of transition from SD to PSD.
BAT is derived from the behavioral model of depression, which indicates that depression occurs with the decrease in frequency of response-contingent positive reinforcement (RCPR). Positive reinforcement comes from individual activities, and less activity reduces the chance of positive reinforcement.26 Influenced by the limitations of physical disease, stroke patients have fewer opportunities for rewarding activities and thus a lower frequency of RCPR than other populations, which easily leads to depression. BAT facilitates activities that individuals value most and brings more opportunities for deriving positive reinforcement from the living environment, and thus plays an important role in improving psychological well-being.12,14 In the current study, the researchers guided the patients to participate in activities such as “Clarify values in life”, “Set life goals”, “Identify achievable activities”, “Identify difficult situations” so that they could experience positive reinforcement of healthy behaviors, leading to the remission of depression. By the end of the six-week intervention and follow-up, the incidence of PSD in the BAT group was lower than that in the control group, indicating that BAT could effectively prevent the occurrence of PSD by stabilizing or improving the depressive symptoms of stroke patients with SD. Due to the short follow-up time, the possibility of BAT delaying the occurrence of PSD cannot be ruled out, and a longer follow-up would be needed to further evaluate the prophylactic effect.
Previous studies have noted that subjects with reduced BAS scores are at increased risk for developing depression,27 suggesting that interventions targeting BAS may help alleviate depressive symptoms. Therefore, our study specifically addressed the behavior of stroke patients with SD, based on function assessments of the patients, and oriented by the patients’ specific life goals; the findings revealed that promoting and enhancing management of daily activities could increase sensitivity toward rewards and drive, enhancing both positive affect and the efficacy of the approach. After the intervention, the BAS scores in the intervention group who had received BAT were higher than those in the control group, and there was a significant difference in the BAS scores between the two groups. This difference was also observed to persist, indicating that BAT can improve the level of BAS and has long-term efficacy, which is consistent with other work.28
Apart from demonstrating the feasibility of BAT, this exploratory study also identified several cautions and proposed solutions based on participant feedback. First, life goals need to be changed according to the patient’s functional status; these should not be too high or too low as patients may not then derive a sense of achievement from the activities directed toward completing the goal. Second, the activity log is an important foundation for assessing and monitoring patients’ behavior, and for those with limited literacy, family members can assist with completion of the log. In other cases, patients can indicate the type of activities by drawing, or use a tape recorder, or activities can be presented by digitally coded pictures with the patients only required to record the numbers. Third, if the patient is not sufficiently motivated or does not finish the homework, it is difficult to implement the next plan of BAT. Therefore, from the perspective of patients, it is important to choose pleasant, practical, healthy, and meaningful activities to enhance their motivation. Homework can be arranged in terms of a schedule, for instance, a plan to meet Mr./Ms. Zhang at a square at 17:00 for a walk. Appointments can also be made for patients to create a sense of task for them, which can stimulate their executive power.
Study Limitations
This study has several limitations. First, the study was based on a small sample of participants from a single hospital. The findings should be verified and extended in large-sample multicenter studies. Second, the participants were limited to stroke patients with a disease duration of three months, and the representativeness of the sample was limited. The duration of BAT intervention is flexible. Based on the core principles, the BAT program might be revised for stroke patients at different stages, for example, the acute stage, convalescent stage, and sequelae stage, so that BAT can be more widely promoted for use in stroke patients with SD at different stages. Third, in this study, only psychological measures were used; physiological and social assessment indicators could be included in the future to evaluate the effect of BAT on improving the physiological and social functions of stroke patients with SD. In addition, the observation time was limited; we plan to extend the observation time in future studies to determine the long-term sustainability of BAT.
Conclusion
Despite the limitations, this exploratory study indicated that BAT is feasible for stroke patients. The results of the study showed that BAT may be effective in reducing the development of depressive symptoms and cultivating behavioral activation, leading to stabilization and improvements in the psychological state and thus potentially contributing to the primary prevention of PSD. In future studies, the use of BAT in addressing SD at different stages of stroke can be investigated, leading to the improvement of the psychological health of this population.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author (Yumei Lv) upon request.
Acknowledgments
The authors would like to thank all the reviewers who participated in the review and MJEditor (www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ding Q, Liu S, Yao Y, et al. Global, regional, and national burden of ischemic stroke, 1990–2019. Neurology. 2022;98(3):e279–e290. doi:10.1212/WNL.0000000000013115
2. Tu WJ, Hua Y, Yan F, et al. Prevalence of stroke in China, 2013–2019: a population-based study. In The Lancet Regional Health-Western Pacific. Elsevier; 2022:100550.
3. Tsuchiya K, Fujita T, Sato D, et al. Post-stroke depression inhibits improvement in activities of daily living in patients in a convalescent rehabilitation ward. J Phys Ther Sci. 2016;28(8):2253–2259. doi:10.1589/jpts.28.2253
4. Perna R, Harik L, Begali V. The role of rehabilitation psychology in stroke care described through case examples. NeuroRehabilitation. 2020;46(2):195–204. doi:10.3233/NRE-192970
5. Ahrens J, Shao R, Blackport D, et al. Cognitive-behavioral therapy for managing depressive and anxiety symptoms after stroke: a systematic review and meta-analysis. In: Topics in Stroke Rehabilitation. Taylor & Francis; 2022:1–16.
6. Wang SB, Wang YY, Zhang QE, et al. Cognitive behavioral therapy for post-stroke depression: a meta-analysis. J Affect Disord. 2018;235:589–596. doi:10.1016/j.jad.2018.04.011
7. Lee YY, Stockings EA, Harris MG, et al. The risk of developing major depression among individuals with subthreshold depression: a systematic review and meta-analysis of longitudinal cohort studies. Psychol Med. 2019;49(1):92–102. doi:10.1017/S0033291718000557
8. Tuithof M, Ten Have M, van Dorsselaer S, et al. Course of subthreshold depression into a depressive disorder and its risk factors. J Affect Disord. 2018;241:206–215. doi:10.1016/j.jad.2018.08.010
9. Saxena SK, Ng TP, Yong D, et al. Subthreshold depression and cognitive impairment but not demented in stroke patients during their rehabilitation. Acta Neurol Scand. 2008;117(2):133–140. doi:10.1111/j.1600-0404.2007.00922.x
10. Gilbody S, Lewis H, Adamson J. Effect of collaborative care vs usual care on depressive symptoms in older adults with subthreshold depression: the CASPER randomized clinical trial. JAMA. 2017;317(7):728–737. doi:10.1001/jama.2017.0130
11. Schönenberg A, Zipprich HM, Teschner U, et al. Impact of subthreshold depression on health-related quality of life in patients with Parkinson’s disease based on cognitive status. Health Qual Life Outcomes. 2021;19(1):1–8. doi:10.1186/s12955-021-01753-5
12. Wong SYS, Sun YY, Chan ATY, et al. Treating subthreshold depression in primary care: a randomized controlled trial of behavioral activation with mindfulness. Annals Fam Med. 2018;16(2):111–119. doi:10.1370/afm.2206
13. Krishna M, Lepping P, Jones S, Lane S. Systematic review and meta-analysis of group cognitive behavioural psychotherapy treatment for sub-clinical depression. Asian J Psychiatr. 2015;16(6):7–16. doi:10.1016/j.ajp.2015.05.043
14. Ayudhaya WSN, Pityaratstian N, Jiamjarasrangsi W. Effectiveness of behavioral activation in treating Thai older adults with subthreshold depression residing in the community. Clin Interv Aging. 2020;15:2363. doi:10.2147/CIA.S274262
15. Thomas SA, Drummond AE, Lincoln NB, et al. Behavioural activation therapy for post-stroke depression: the BEADS feasibility RCT. Health Technol Assess. 2019;23(47):1–176. doi:10.3310/hta23470
16. Hirayama T, Ogawa Y, Yanai Y, et al. Behavioral activation therapy for depression and anxiety in cancer patients: a case series study. Biopsychosoc Med. 2019;13(1):1–6. doi:10.1186/s13030-019-0151-6
17. van der Feltz‐Cornelis C, Allen SF, Holt RIG, et al. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: systematic review and meta‐analysis. Brain Behav. 2021;11(2):e01981.
18. First MB. Structured Clinical Interview for the DSM (SCID). New York, NY: John Wiley & Sons, Inc; 1995.
19. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–191. doi:10.1002/nur.20247
20. Lejuez CW, Hopko DR, Acierno R, et al. Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behav Modif. 2011;35(2):111–161. doi:10.1177/0145445510390929
21. Lau SCL, Baum CM, Connor LT, et al. Psychometric properties of the Center for Epidemiologic Studies Depression (CES-D) scale in stroke survivors. In Topics in Stroke Rehabilitation. Taylor & Francis; 2022:1–10.
22. Zheng Y, Zhao J, Phillips M, et al. Validity and reliability of the Chinese Hamilton depression rating scale. Br J Psychiatry. 1988;152(5):660–664. doi:10.1192/bjp.152.5.660
23. Li YZ, Zhang Y, Jiang Y, et al. The Chinese Version of the BIS/BAS scale: reliability and validity. Chin Ment Health J. 2008;22(8):613–616.
24. Cuijpers P, Vogelzangs N, Twisk J, et al. Differential mortality rates in major and subthreshold depression: meta-analysis of studies that measured both. Br J Psychiatry. 2013;202(1):22–27. doi:10.1192/bjp.bp.112.112169
25. Zavoreo I, Bašić-Kes V, Bosnar-Puretić M, et al. Post-stroke depression. Acta Clinica Croatica. 2009;48(3):329–333.
26. Donde C, Moirand R, Carre A. Behavioral activation programs: a tool for treating depression efficiently. ENCEPHALE. 2017;44(1):59–66. doi:10.1016/j.encep.2017.02.006
27. Masuyama A, Kubo T, Shinkawa H, et al. The roles of trait and process resilience in relation of BIS/BAS and depressive symptoms among adolescents. PeerJ. 2022;10:e13687. doi:10.7717/peerj.13687
28. Collado A, Calderón M, MacPherson L, et al. The efficacy of behavioral activation treatment among depressed Spanish-speaking Latinos. J Consult Clin Psychol. 2016;84(7):651. doi:10.1037/ccp0000103
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.