Back to Journals » Clinical Ophthalmology » Volume 13
Barriers to adoption of a personal health record in an ophthalmic setting: lessons from implementation of a Glaucoma Patient Passport
Authors Badran I, Bruynseels A , Khan S, Sii F , Shah P
Received 11 March 2019
Accepted for publication 3 May 2019
Published 25 July 2019 Volume 2019:13 Pages 1369—1375
DOI https://doi.org/10.2147/OPTH.S208377
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Imad Badran,1,2 Alice Bruynseels,1,3 Salim Khan,2 Freda Sii,1,3 Peter Shah1,3–5
1Ophthalmology Department, Queen Elizabeth Hospital Birmingham, Birmingham, UK; 2Department for Therapies and Public Health, Birmingham City University, Birmingham, UK; 3Birmingham Institute for Glaucoma Research, Institute for Translational Medicine, Birmingham, UK; 4Institute of Ophthalmology, University College London, London, UK; 5Centre for Health and Social Care Improvement, School of Health and Wellbeing, University of Wolverhampton, Wolverhampton, UK
Purpose: Self-care in chronic disease is increasingly important. In glaucoma services, there is an unmet need for a self-care tool such as a patient passport. This study aims to evaluate adoption of a new self-care tool, the Glaucoma Patient Passport (GPP) within a tertiary hospital glaucoma service.
Patients and methods: The GPP was designed following consultation exercises between patients and clinicians at the first and second UK National Glaucoma Think Tanks. A patient questionnaire, comprising a mixed methods quantitative and qualitative research approach was used to explore the utility of GPP, patient attitude to GPP and barriers to adoption, 6 months after GPP receipt.
Results: GPP feedback was received from 62 patients. On-going utilization of the GPP after receipt was high, at 84%, with patients most commonly using the GPP at home, to “look for information.” Seventy-three percent reported improved knowledge of glaucoma care since using the GPP, with two-thirds (63%) reporting that the GPP had improved their glaucoma care. Three main themes were identified in exploring barriers to GPP adoption; clinician involvement in GPP use, GPP size, and GPP use in visual impairment.
Conclusion: Implementation and adoption of the world’s first GPP were a success. GPP utility was high and patient attitudes were predominantly positive, with improved self-care. However, several areas were identified for future GPP improvement. The GPP has the potential to improve patient self-care in glaucoma, bridging the care gap created by the increased workload in glaucoma services.
Keywords: chronic disease, self-care, patient passport, ophthalmology
Plain language summary
Self-care in chronic disease has been enhanced in recent years though the introduction of patient passports. These passports can help patients and clinicians in disease monitoring. Passports are already available to patients for conditions such as asthma and epilepsy. However as yet there is no patient passport for adults with glaucoma, a chronic eye condition. In glaucoma services, increasing patient numbers and clinical workload mean there is an unmet need for a patient passport to enhance glaucoma self-care.
This study evaluates the adoption of the world’s first patient passport for glaucoma and the journey of its implementation into a glaucoma service within a tertiary hospital. It identifies that the Glaucoma Patient Passport can be successfully implemented into a service and adopted by patients, ultimately improving patient self-care. It also explores the patient-identified barriers to uptake and adoption of the passport in an ophthalmic setting, highlighting areas to improve future passport development and implementation.
Introduction
Self-care in chronic disease has been enhanced in recent years by the introduction of patient passports. These patient passports, already in use for chronic conditions such as asthma, epilepsy, and diabetes are personal health records designed to help patients and clinicians in disease monitoring.1–3 Patient outcomes have been shown to improve following patient passport use, through increasing patient confidence to self-care and facilitating inter-disciplinary communication.4–6
In glaucoma, the recent significant increase in workload and patient numbers due to improved early identification of the disease and an aging population has created an enormous challenge for hospital glaucoma services in the UK.7–11 As a consequence, patient–clinician contact time is limited and there is an unmet need for effective tools to enhance glaucoma self-care. The patient passport in an ophthalmology setting has been successfully integrated into pediatric glaucoma care and is undergoing implementation for uveitis.12 This has the potential to bridge the patient–clinician gap and improve patient outcomes.
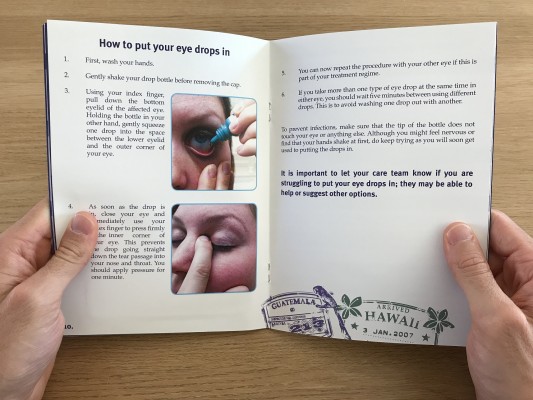
The world’s first Glaucoma Patient Passport (GPP) was created to improve patient self-management (Figure 1). Its design was developed in consultation with patients, clinicians, nurses, and relatives at the first and second UK National Glaucoma Think Tanks.13 The GPP contains several unique features, integrated to enhance both patient self-management and preparation for clinic appointments in order to optimize time within the clinic setting and clinician interactions (Table 1).
 |
Table 1 Key contents features of the GPP, with descriptions and purpose of each feature |
Adoption of a new personal health record, such as the GPP is multifaceted. A wide range of factors are influential from patient health-literacy to patient ethnicity.14,15 Potential barriers to adoption include environmental issues such as organization, cost, and privacy, as well as individual clinician issues such as workflow and recognition of the value to behavioral change.4 These factors which have previously been amalgamated in a concept map, can aid health care professionals in predicting and avoiding obstacles when implementing a new tool.12 However, several challenges will be unique to ophthalmic health records, including the GPP, due to visual impairment; such as difficulty with reading and writing secondary to reduced visual function.16,17
The creation and implementation of the GPP into our service are to our knowledge the first of its kind. In this paper, we aim to evaluate the GPP through exploring its utility, patients’ attitudes to the GPP, and barriers to its adoption into a tertiary glaucoma service.
Methods
Study population
The GPP was distributed to patients within our tertiary glaucoma service at Queen Elizabeth Hospital Birmingham (QEHB). Eligibility criteria for study inclusion were age 18 years and above, with a confirmed diagnosis of glaucoma, requiring on-going hospital follow-up. A non-probability, convenience sampling method was used. Written informed consent was obtained from all study participants, with the study approved by the QEHB Research and Development Team.
GPP introduction
The Information-Motivation-Behavioural skills model (IMB) was used within a one-to-one initial consultation with the patient.18 This consultation was carried out by our Glaucoma Clinical Nurse Specialist (CNS), as part of the patients’ routine follow-up appointment, prior to the patient consultation with the usual clinician. The IMB model encompassed three areas of discussion with each patient; (i) individual glaucoma-care information (clinical team, glaucoma diagnosis, treatment), (ii) personal and social motivations for glaucoma self-management, (iii) behavioral change (explanation and use of GPP). The patients were asked to use the GPP in their consultation with the usual clinician that followed the IMB interview. Following this introduction of the GPP, it was left at the patients’ discretion to bring the GPP to appointments and use it outside of the clinic setting.
GPP evaluation
Six months after receiving the GPP, one-to-one, clinic-based, structured interviews of 20–40 mins were held, in order to gain an understanding of the utility and attitudes toward the GPP. The interview was structured around an 11-item GPP evaluation questionnaire, designed by the authors. The questionnaire included a combination of white-space questions and dichotomous categorical question and answers. The interview was led by the CNS, who distributed the questionnaire and transcribed any extraneous comments made by the patient regarding the GPP. Domains covered by the questionnaire included the patient utility of the GPP, patient attitude to the GPP and patient adoption of the GPP. Patient demographic information such as self-determined ethnicity and gender were collected, coded, and stored separately to the questionnaire to retain anonymity.
Analysis
The primary outcome was to evaluate the adoption of the GPP through exploring its utility, patients’ attitudes to the GPP and barriers to its uptake. Questionnaire data were analyzed using a divided approach to separate responses containing quantitative or qualitative data. This approach which incorporated both inductive and deductive methods, enabled combined analysis of both the spontaneous speech recorded by the lead researcher (IB) and white-space questionnaire responses. Qualitative data were analyzed using standard thematic analysis methods.19 Analyses were performed by the lead researcher (IB), identifying key themes in patient responses and were validated by co-investigators (AB, FS, and PS).
Results
The GPP questionnaire was completed by 62 patients who had received the GPP within the previous two years. Demographic data for these patients are displayed in Table 2.
 |
Table 2 Socio-demographic information for the study sample |
Utility of GPP
Fifty-two (84%) patients reported that they had used the GPP since receiving it. The majority (90%) of these patients were using the GPP at home and 67% were using the GPP both at home and when at their clinic appointment. The GPP was most commonly used “to look for information” and “if I have an eye problem” (Table 3). Eighteen patients, a third of patients who reported using the GPP, brought the GPP to every clinic visit, with two-thirds of these patients actually using the GPP within the clinic setting at every attendance. The GPP was also used by two patients at their General Practitioner appointment and one patient at their opticians to document glasses prescription.
 |
Table 3 Patient-reported reasons for using the Glaucoma Patient Passport (GPP ) at home |
 |
Table 4 Table of quotes |
Ten (16%) patients had not used their GPP since receiving it 6 months prior. The main reason documented was because they had forgotten to use it (60%), but also due to poor vision and practical difficulties in using the GPP (20%) and furthermore due to a lack of belief in its usefulness (20%).
Patient attitude toward GPP
Of the patients that had been using the GPP, three quarters (83%) found the information in the GPP helpful, with a similar number (73%) reporting improved knowledge of glaucoma care since using the GPP. Around two-thirds (63%) felt it had helped to improve their glaucoma care and 75% would recommend the GPP to someone else with glaucoma. A significant number of patients (75%) also felt that the GPP gave them more confidence to discuss concerns related to their glaucoma with health care professionals.
Barriers to GPP adoption
Three main themes were encountered from analysis of the transcripts from both the questionnaires and extraneous verbal comments given by patients within the IMB interviewing. Quotations from these data are used to illustrate these themes (Table 4).
Several patients, predominantly those who were not utilizing the GPP within their care wanted greater interaction from the clinician with the GPP within the clinic. Some patients had forgotten to use the GPP as a consequence of not being prompted to use it when attending their clinic appointment (quote 1). Similarly, some patients had not gone on to use the GPP since its initial introduction as they had forgotten the instructions for its use which were provided in the IMB interviewing and had not been prompted since then to use it or bring it to clinic (quote 2). One patient had initially found the GPP useful, but had lost belief in its importance or utility since none of the clinic staff had asked to see it (quote 3).
A few participants were dissatisfied with the size of the GPP. They felt that the GPP was too big and this made it impractical to carry the GPP around as it did not fit in their bag or coat pocket (quote 4 and quote 5). Some patients voiced this as the reason for them not bringing the GPP with them to clinic (quote 6).
Difficulty in interacting with the GPP due to the patient’s visual impairment was voiced by some patients. This was directly referred to by the daughter of a patient who had accompanied her father to clinic (quote 7) and by a patient themselves (quote 8). Further patients mentioned that they had to use visual aids when reading day to day and so struggled to use the GPP (quote 9).
Discussion
Implementation and adoption of the world’s first GPP into our glaucoma service were predominantly successful. At the end of our process of implementation, a large majority of the patients who had received the GPP were using it as a tool within their routine care. This demonstrates not only acceptability of the GPP to the patients, but also the effectiveness of IMB as a method of GPP distribution and introduction. Furthermore, through utilizing the GPP, patients perceived that they were benefitting from the GPP use with improved knowledge of their glaucoma care. These factors are likely to benefit the patient significantly in self-care of their glaucoma.
The GPP has also demonstrated its potential for reducing utilization of health care resources both within the clinic environment and when the patient is at home. Patients reported a number of different uses for the GPP including when they had “an eye problem”, “to look for information”, and “when I am not sure about my treatment.” The use of the GPP as a self-management or educational tool in these circumstances may not only help to reduce administrative burden by directing the patient to the most appropriate resource, or point of contact within the department, but also maximize efficiency and utility of the patient–clinician interaction during a clinic appointment. Although initially, the IMB implementation process may require increased resources, this is likely to be significantly outweighed by the GPP’s benefits long term. These key findings demonstrate that the GPP can be successfully adopted into a service and has the ability to make a significant impact within a glaucoma service.
However, this process has further highlighted several barriers to the successful adoption of this patient self-care tool, some specific to our service and some which are applicable to developing any health care innovation within an ophthalmic setting. A limitation that was encountered in successful GPP adoption was that some participants lacked belief in the GPP’s utility or even forgot to use it, primarily because their clinician did not interact with their GPP within the clinic appointment. It is clear from these results that in implementing the GPP, the clinician should play a central role to improve utility and consequently the adoption of the new patient tool.
A further key factor in the uptake of the new GPP was its size. Some patients felt that it was too large to carry around, and this is a barrier that should be addressed in the next editions of the GPP. However, in addressing this element of the GPP design, this would need to be balanced with the issues face in the final barrier identified in this study; patient’s visual impairment as an obstacle to GPP use. Here further research would be needed in this area to explore the exact difficulties faced by patients when interacting with the GPP; however, some adjustments to the GPP may include larger font type and matte finish instead of gloss finish to pages of GPP. A further option is to create an app-based iteration of the GPP.
Identification of barriers to patient adoption of the GPP was limited in this study as data were not collected on patients who declined to participate in the study at the initial convenience sampling stage. It is possible that some of these patients may have had differing reasons for not adopting the GPP into their care and consequently declining to take part in the study. This would be an interesting group of patients to capture in future studies in this area.
This study has demonstrated the successful implementation of the GPP into a glaucoma service, through the use of IMB interviewing. The GPP has the potential to increase efficiency and improve patient outcomes through improving patient self-management and education. However, when implementing future personal health records within an ophthalmic setting, there is a need for greater clinician-led interaction with the innovation, alongside specific design considerations.
Acknowledgment
We are very grateful to the International Glaucoma Association for their support throughout this project. This work was funded by the International Glaucoma Association. The funding organization had no role in the design or conduct of this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Newell K, Corrigan C, Punshon G, Leary A. Severe asthma: emergency care patient driven solutions. Int J Health Care Qual Assur. 2017;30:628–637. doi:10.1108/IJHCQA-09-2016-0127
2. Drewett O, Hann G, Price N, Tipper C, Devereux E. A qualitative study to explore the use of the RCPCH epilepsy passport. Br Inherit Metab Dis Gr Br Paediatr Neurol Assoc. 2017;102:A150.
3. Dijkstra RF, Braspenning JCC, Huijsmans Z, et al. Introduction of diabetes passports involving both patients and professionals to improve hospital outpatient diabetes care. Diabetes Res Clin Pract. 2005;68:126–134. doi:10.1016/j.diabres.2004.09.020
4. Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Informatics Assoc. 2006;13:121–126. doi:10.1197/jamia.M2025
5. Kennedy AP, Rogers AE. Improving patient involvement in chronic disease management: the views of patients, GPs and specialists on a guidebook for ulcerative colitis. Patient Educ Couns. 2002;47:257–263.
6. Malone K, Pope AL, Cowie E, Dunne E. Development of a multidisciplinary brain tumour patient passport. Int J Integr Care. 2017;17:A210. doi:10.5334/ijic.3520
7. Burr J, Botello-Pinzon P, Takwoingi Y, et al. Surveillance for ocular hypertension: an evidence synthesis and economic evaluation. Health Technol Assess. 2012;16:1–272. doi:10.3310/hta16290
8. Pappa C, Hyphantis T, Pappa S, et al. Psychiatric manifestations and personality traits associated with compliance with glaucoma treatment. J Psychosom Res. 2006;61:609–617. doi:10.1016/j.jpsychores.2006.03.050
9. Lacey J, Cate H, Broadway DC. Barriers to adherence with glaucoma medications: a qualitative research study. Eye. 2009;23:924–932. doi:10.1038/eye.2008.103
10. Lunnela J, Kääriäinen M, Kyngäs H. The views of compliant glaucoma patients on counselling and social support. Scand J Caring Sci. 2010;24:490–498. doi:10.1111/j.1471-6712.2009.00739.x
11. McLaughlan B, Winyard S. Don’t blame the patient! A call for action to eliminate unneccessary sight loss from glaucoma. London: Royal National Institute of Blind People; 2007.Report No.:27.
12. Bruynseels A, Cross V, Sii F, Shah P, Abbott J. Developing a children’s glaucoma passport: mapping innovations in healthcare. Eye. 2017;31:1635. doi:10.1038/eye.2017.115
13. Somner J, Sii F, Bourne R, Cross V, Burr J, Shah P. Moving from PROMs to POEMs for glaucoma care: a qualitative scoping exercise. Invest Ophthalmol Vis Sci. 2012;53:5940–5947. doi:10.1167/iovs.12-10223
14. Liu LS, Shih PC, Hayes GR Barriers to the adoption and use of personal health record systems.
15. Kondylakis H, Kazantzaki E, Koumakis L, et al. Development of interactive empowerment services in support of personalised medicine. Ecancermedicalscience. 2014;8:400. doi:10.3332/ecancer.2014.400
16. Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol. 2009;20:92–98. doi:10.1097/ICU.0b013e32832401a9
17. Aspinall PA, Johnson ZK, Azuara-Blanco A, Montarzino A, Brice R, Vickers A. Evaluation of quality of life and priorities of patients with glaucoma. Investig Opthalmology Vis Sci. 2008;49:1907–1915. doi:10.1167/iovs.07-0559
18. Fisher J, Fisher W, Misovich S, Kimble D, Malloy T. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Heal Psychol. 1996;15:114–123. doi:10.1037/0278-6133.15.2.114
19. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi:10.1191/1478088706qp063oa
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

