Back to Journals » Infection and Drug Resistance » Volume 13
Bacterial Isolates from CSF Samples and Their Antimicrobial Resistance Patterns Among Children Under Five Suspected to Have Meningitis in Dilla University Referral Hospital
Authors Awulachew E , Diriba K , Awoke N
Received 26 May 2020
Accepted for publication 10 November 2020
Published 23 November 2020 Volume 2020:13 Pages 4193—4202
DOI https://doi.org/10.2147/IDR.S264692
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Ephrem Awulachew, Kuma Diriba, Netsanet Awoke
Department of Medical Laboratory Science, College of Health Science and Medicine, Dilla University, Dilla, Ethiopia
Correspondence: Ephrem Awulachew Tel +251 49181161
Email [email protected]
Introduction: Bacterial meningitis is a medical emergency that requires immediate medical attention. It causes an estimated 288,649 deaths worldwide per year, of which 94,883 death occur among children under 5 years old. Up to 24% of survivors suffer from long-term sequelae such as epilepsy, mental disability, or sensorineural deafness, especially when the disease is contracted during early childhood.
Objective: This study aimed to assess bacterial isolates of cerebrospinal fluid (CSF) samples and their antimicrobial resistance patterns among children under 5 years old in Dilla University Referral Hospital.
Material and Methods: Hospital-based cross-sectional study design was used to collect clinical data and CSF sample from children under 5 years old who were suspected for meningitis. Sediment of CSF samples was inoculated to blood agar plate, chocolate agar plate, and MacConkey agar for bacterial isolation and identification. Chemical analysis and cytological analysis were also conducted based on standard operating procedures.
Results: From a total of 287 CSF samples cultured, causative bacteria were detected in 38 (13.2%). From culture positive cases, the most frequent isolate was Streptococcus pneumoniae (13 (34.2%)) followed by Staphylococcus aureas (7 (18.4%)), Neisseria meningitidis (6 (16%)) and Escherichia coli (6 (16%)). Haemophilus influenzae type b was isolated in 4 (10.5%) children with meningitis. Another cause of meningitis was Streptococcus agalactiae which accounted for 10.5%. Cryptococcus neoformans was detected in 4 (1.9%) cases of meningitis. Of all bacterial isolates, about 42.1% (16/38) were multi-drug resistant. About 38.5% of S. pneumoniae had multi-drug resistance, while about 33.3% of N. meningitidis, 50% of H. influenzae, 57.1% of S. aureas and 40% of E. coli showed multi-drug resistance.
Conclusion: A high prevalence of bacterial meningitis and high rate of drug resistance were observed. Streptococcus pneumoniae was the leading cause of bacterial meningitis among children under 5 years old.
Keywords: antimicrobial resistance, bacterial meningitis, multi-drug resistant, Ethiopia
Introduction
Bacterial meningitis (BM) is an inflammation caused by bacterial infection of the meninges, the protective lining of the brain and spinal cord.1 In the past decades, the epidemiology and treatment strategies for bacterial meningitis have significantly changed.2 The introduction of conjugate vaccines has resulted in a reduction of Haemophilus influenzae type b, while conjugate pneumococcal and meningococcal vaccines have significantly reduced the burden of bacterial meningitis.3–5 Common etiologies of BM are Haemophilus influenzae b, Streptococcus pneumoniae, Neisseria meningitidis, group B Streptococcus (GBS), and Listeria monocytogenes, depending on age, sex, race, season and immunological status of the child.6
Bacterial meningitis is a medical emergency that requires immediate medical attention.7,8 Even with appropriate treatment, morbidity and mortality can be substantial.9,10 Despite modern antibiotics and improved critical care, BM case fatality rates remain high.11,12 It is causes an estimated 288,649 deaths worldwide per year, of which 94,883 death occur among children under 5 years old.13,14 Although an effective vaccine reduces the incidence and effective modern antibiotics kill bacteria efficiently, mortality rates are still up to 34% in developing countries.15 BM usually causes serious complications such as brain damage, hearing loss, and ultimately death if not diagnosed and treated promptly.16,17 Up to 24% of BM survivors suffer from long-term sequelae such as epilepsy, mental disability, or sensorineural deafness, especially when the disease is contracted during early childhood.18
A region of sub-Saharan Africa extending from Ethiopia in the east to Gambia in the west, encompassing 15 countries and over 260 million people is known as the “meningitis belt” because of its high endemic rate of disease with superimposed, periodic, large epidemics. During epidemics, children and young adults are most commonly affected, with infection rates as high as 1000/100,000 population, or 100 times the rate of sporadic disease.19,20 The highest rates of endemic or sporadic disease occur in children less than 2 years of age. Case-fatality rates (CFRs) of suspected meningitis cases in the African meningitis belt were 4–26% according to the country WHO weekly epidemiological record.21
In Ethiopia, the disease has remained a serious health threat for the community especially among children under 5 years old. Bacterial meningitis particularly occurs in Ethiopia in the dry season from December to June, and there have been frequent meningococcal epidemics in different parts of the country.22,23
Another challenging epidemiologic trend is the emergence of antimicrobial resistance among meningeal pathogens. Drug resistance has been reported worldwide.24,25 However, the situation in developing countries like Ethiopia is particularly serious. Because of the absence of well-equipped bacteriological laboratories in Ethiopia, no organized surveillance exists for drug resistance patterns among common bacterial isolates.26
The early signs of meningitis are entirely nonspecific in newborns and pediatric patients and the disease must be positively excluded. Early diagnosis and appropriate antibiotic treatment are necessary to avoid further complications. Knowledge of the locally predominant meningeal pathogens and their sensitivity pattern is essential to plan for management of bacterial meningitis and to minimize adverse outcomes. Thus the main aim of this study was to assess bacterial isolates of CSF samples and their antimicrobial resistance patterns among children under 5 years old in Dilla University Referral Hospital, South Ethiopia.
Materials and Methods
Study Area and Study Period
The study was conducted in Dilla University Referral Hospital from February 1, 2019 to March 30, 2020. Dilla University referral is located in Dilla Town, in the south of Ethiopia. It is located 356 km away from Addis Ababa. The hospital is the referral hospital in Gedeo zone, south of Ethiopia.
Study Design
Hospital-based cross-sectional study design was used to collect clinical data and CSF samples for bacterial isolation.
Study Population
Children under 5 years old who were suspected for meningitis and who underwent lumbar puncture during the study period were the study population.
Eligibility Criteria
All pediatrics patients (<5 years of age) who were clinically suspected for meningitis during the study period were included in the study. Meningitis was clinically suspected if the patient presented with any of the following signs and symptoms: lethargic, vomiting, poor feeding, irritable, fever (≥ 38°C), and headache (above 2 years), meningeal irritation signs (Kernig or Brudzinski signs or neck stiffness, ≥ 1 year) on examination were considered critical for suspicion of meningitis.27
Sample Size Determination and Sampling Technique
The sample size for this study was calculated using the formula for estimation of a single population proportion considering a prevalence of 30.6% from a study conducted in Jimma, Ethiopia.28 Therefore the total sample size was 287. The study participants were recruited consecutively until the required sample size was reached using convenient sampling techniques.
Data Collection Instrument and Techniques
An interviewer administered questionnaire was developed through critical thinking and review of literatures and then translated to Amharic. Demographic information and clinical data were collected using a structured, interviewer administered questionnaire among the children’s parents/guardians.
Cerebrospinal Fluid Sample Collection and Identification of Bacteria
CSF Specimen Collection
CSF specimens were collected with lumbar puncture by a physician and then immediately transported to Dilla University Microbiology Laboratory within 30 minutes for analysis. Each collected CSF sample was divided into three test tubes according to the standard of CSF analysis.29 The first test tube was used for chemical analysis (protein, glucose), the second test tube was used for microbiological analysis, while the third test tube was used for cytological analysis.
Processing CSF Sample
Microbiological analysis of CSF sample: Once the CSF arrived in the Microbiology Laboratory, the volume of CSF available for analysis was noted. The sediment of centrifuged CSF was plated on a blood agar plate (BAP) (Oxoid) and a chocolate agar plate (CAP) and onto MacConkey agar (MA) and was incubated aerobically and in 5% CO2 at 37°C for 24–48 h. Purity plates (negative growth control) were incubated after each new batch of produced media plates. Growth conditions were controlled by parallel incubation of the control strains S. pneumoniae ATCC 49619 and Escherichia coli ATCC 25922 obtained from the Ethiopian Public Health Institute in every batch of media preparation. Gram stain was conducted simultaneously using freshly prepared Gram stain reagents. Each CSF sample was also examined by fluorescent microscope for diagnosis of tubercular meningitis and Indian ink preparation was used to diagnose for cryptococcal meningitis.
Cytological examination of the CSF sample was conducted on the third test tube. CSF sample was checked for turbidity, leukocytosis (usually of polymorphonuclear (PMN) leukocytes); WBC counts >10 cells/mm. Chemical analysis of the CSF sample was conducted using a spectrophotometer to measure the glucose and protein concentration of the sample at 546 nm wavelength.
Isolation and Identification of Bacteria
After overnight incubation of the inoculum at 37 °C, BAP, CAP and MA culture plates were examined for colonies. All positive CSF cultures were identified and characterized on the basis of morphology, cultural characteristics, and biochemical testing and serogroup-specific antisera.
Identification of Neisseria meningitidis by their round, moist, glistening, and convex colonies on BAP or CAP, Gram negative diplococci, oxidase positive, acid production in glucose and maltose and not in sucrose or lactose. Then the serogroups of N. meningitidis were identified by using serogroup-specific antisera (Bio-Rad., PastorexTM Meningitis, lot No: - 64,247,667). Haemophilus influenzae isolate was identified by testing colorless-to-grey opaque colonies grown in the presence of X and V factor on chocolate agarfor oxidase positivity and finally it was serotyped using H. influenza type b serogroup-specific antisera (Bio-Rad., PastorexTM Meningitis). Streptococcus pneumonia was identified by their grey, moist, flattened, and depressed center colonies with a zone of alpha-hemolysis on BAP, Gram reaction, catalase negative, optochin sensitivity (>14 mm), and bile solubility. Then the S. pneumonia isolate was serotyped using serogroup-specific antisera (Bio-Rad., PastorexTM Meningitis, lot No:- 64,247,667). Streptococcus agalactiae was identified by characteristic translucent grey colonies, with complete ß hemolysis on BAP, Gram reaction, catalase negative, and esculin negative. Then the isolates were serotyped using serogroup-specific antisera (Bio-Rad., PastorexTM Meningitis, lot No: - 64,247,667).
Other Gram positive and Gram negative organisms were identified by a series of biochemical tests including catalase test, coagulase test, Triple Sugar Iron slant agar (TSI) (Oxoid), indole test and urase test (Oxoid) and Sulfide-Indole-Motility (SIM).
Antibiotic Sensitivity Test
Tests of the antibiotic resistance patterns of bacterial isolates against commonly used antibiotics were conducted on Mueller Hinton agar (MHA) (Oxoid) and incubated at 37°C for 24 h. The standard disk diffusion technique of the modified Kirby-Bauer method was used as recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST).30 For the susceptibility testing, the following nine antimicrobial drugs and concentrations were used: ampicillin (10 µg), chloramphenicol (30 µg), erythromycin (15 μg), ciprofloxacin (5 μg), tetracycline (30 µg), ceftriaxone (30 µg), clindamycin (2 µg), trimethoprim-sulphamethoxazole (1.25/23.75) and rifampicin (5 μg). Multidrug resistance was considered when resistance to two or more drugs belonging to different classes of antibiotics was found.31,32
Study Variables
Dependent Variables
Prevalence of bacterial meningitis
Patterns of drug resistance
Independent Variables
Socio-demographic variables such as age and sex
Clinical data (fever, irritability, stiff neck, poor feeding, light intolerance)
Operational Definition
The proportion of children infected with specific types of bacteria from total number of children who participated in the study.
Data Quality Assurance
Training was given to a laboratory assistant and data collector for 2 days on the procedures of data collection and handling of collected data. The collected data were checked for completeness at the end of data collection. During laboratory analysis of CSF cultures, standard operating procedures were followed. To maintain the quality of the result, any CSF samples either grossly contaminated with blood,not received within 2 hof collection, or not in an appropriate transport medium were rejected. Culture media were prepared and sterilized based on SOPs. The sterility of culture media was checked by parallel incubation of un-inoculated plates in every newly prepared culture plate and observed for bacterial growth. Control strains S. pneumoniae ATCC 49619 and E. coli ATCC 25922 obtained from the Ethiopian Public Health Institute were used as quality controls during CSF cultures, biochemical tests and antimicrobial susceptibility testing.
Data Analysis
The collected data were coded, entered, and cleaned using Epi-Data version 3.02 and transferred to SPSS version 20 for analysis. Descriptive statistics such as frequency, percentage, and cross tabulation were used to present the findings. Chi-square was performed to evaluate whether the variables have a significant association with the outcomes of interest at a 95% confidence interval.
Ethics Approval and Informed Consent
The protocol for patient recruitment and participation in the study followed the principles of the Declaration of Helsinki and was approved by the Dilla University Health Research Ethics Review Committee under protocol unique number 004/2019-01, date January 1, 2019. During data collection, each child’s parent/guardian was informed about the aim of the study. Written consent was obtained from parent/legal guardian for each patient before the start of data collection. The clinical samples were specifically collected for this research. Samples with positive culture results were communicated to physicians in order for patients to receive treatment according to the drug susceptibility results of the isolates.
Results
Socio-Demographic Characteristics
A total of 287 suspected pediatric meningitis cases were examined for bacterial isolates using culture techniques at Dilla University Microbiology Laboratory, of whom 163 (56.8%) were male and 124 (43.2%) were female. The mean age of the participants was 2.6+ 0.7 years. The majority (169 (58.9%)) of the patients were from rural areas and 41.5% of the children were in the age group 13–59 months (Table 1).
 |
Table 1 Socio Demographic Characteristics and Culture Positivity |
In about 95 (33.1%) and 83 (28.9%) patients, CSF samples were collected within 12 h and 24 h after empirical treatments respectively. About 109 (38%) of suspected meningitis pediatric patients started empirical treatment immediately after CSF samples were collected. The characteristics of 73 (25.4%) CSF samples collected were purulent with visible turbidity and 11 (3.8%) CSF samples were xanthochromic, while the remaining 203 (70.7%) CSF samples were clear in appearance. Pleocytosis (>50 cells/μl) was observed in 164 (57.1%) of CSF samples with a median white blood cell count of 340 cells/μl. From 164 patients with pleocytosis, granulocytosis (predominantly neutrophil) was seen in 97 (59.1%) of patients, while 67 (40.9%) patients had lymphocytosis. Spectrophotometric measurements of CSF protein and glucose showed that 183 (63.8%) CSF samples had normal protein with a mean protein level of 47.8 mg/dl ± 9.6 mg/dl and 87 (30.3%) CSF samples had elevated protein with a mean protein concentration of 79 mg/dl ± 11.6 mg/dl. About 201 (70%) CSF samples had normal glucose concentration with a mean glucose concentration of 64 mg/dl ± 6.9 mg/dl and 65 (22.6%) had reduced glucose concentration with a mean concentration of 32 mg/dl ± 4.7 mg/dl.
Clinical Data
Clinical signs and symptoms of children with suspected meningitis were collected using a standard questionnaire by trained nurses. According to the results of clinical data obtained, fever was demonstrated in 87% of cases, while irritability, rash, and poor feeding were seen in 67%, 26%, and 91%, respectively (Figure 1).
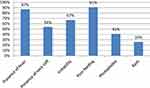 |
Figure 1 Clinical features of children with bacterial meningitis. |
Etiology of Meningitis
From a total of 287 CSF samples cultured, causative bacteria were detected in 38 (13.2%). This makes the overall prevalence of bacterial meningitis 13.2% (38/287). In the present study, Gram stains were performed directly on CSF samples and the yield was 7.3% (21/287). From culture positive cases, the most frequent isolate was Streptococcus pneumoniae (13 (34.2%)) followed by Staphylococcus aureas (7 (18.4%)), Neisseria meningitidis (6 (16%)) and Escherichia coli (6 (16%)). Haemophilus influenzae b was isolated in 4 (10.5%) of children with meningitisand S. agalactiae accounted for 3 cases (8%). Cryptococcus neoformans was detected in 4 (1.9%) cases of meningitis (Table 2).
 |
Table 2 Microbial Isolates of CSF Samples from Children under 5 years old Suspected for Meningitis |
Serotypes of the Isolate
Based on serological characterization, the most frequent Neisseria meningitidis was Y/W135, B, and A, with a prevalence of 50% (2/4), 25% (1/4), and 25% (1/4) respectively. All four of the H. influenzae isolates were type b.
There is no statistically significant association with isolated bacteria and gender of the patients (P = 0.521). The majority of the isolates (43.5%) of bacterial meningitis occurred in the 1–12 months and 13–59 months age groups. Regarding the statistical association of the bacterial isolates, S. agalactiae (group B streptococci (GBS)) were frequently found in infants aged 0–28 days (P = 0.010). H. influenzae b infection showed a statistical association with the age of the children, in that it significantly affects children aged 0–28 days (P < 0.001). Meanwhile, N. meningitidis was a significant cause of meningitis among children aged 1–5 years (OR= 1.8, P = 0.021)
AntiMicrobial Resistance
Antimicrobial susceptibility tests indicated that the resistance rates of S. pneumoniae isolates to ampicillin, chloramphenicol, erythromycin, and ceftriaxone were 38.5%, 38.5%, 15.3%, and 15.3%, respectively. The drug susceptibility test result of N. meningitidis to ampicillin was 33.3%, while resistance to chloramphenicol, tetracycline, and ceftriaxone was 16.7%, 33.3%, and 16.7%, respectively. N. meningitidis also showed 33.3% resistance to rifampicin. The resistance rate of H. influenzae to ampicillin was 50%, while the resistance rates to chloramphenicol, ciprofloxacin, and ceftriaxone were all 25%. The rates of resistance of E. coli to chloramphenicol, ciprofloxacin, and ceftriaxone were 60%, 40%, and 20%, respectively. Antimicrobial resistance rates of S. aureas to ampicillin, chloramphenicol, tetracycline, and trimethoprim-sulphamethoxazole were 28.6%, 57.1%, 42.9%, and 28.6%, respectively. S. agalactiae showed a resistance rate of 33.3% to erythromycin and rifampicin (Table 3).
 |
Table 3 Antimicrobial Resistance Patterns of the Bacterial Isolates in CSF Samples |
Multi-drug resistant isolates were also observed. Of all bacterial isolates, 42.1% (16/38) of the bacterial isolates were multi-drug resistant (MDR is considered when a bacteria is resistant to two or more drugs belonging to different classes of antibiotics). About 38.5% of S. pneumoniae showed multidrug resistance, while 33.3% of N. meningitis, 50% of H. influenzae, 57.1% of S. aureas, and 40% of E. coli showed multi-drug resistance (Table 4). The proportion of isolates resistant to two, three, and more than four drugs were 7.9%, 13.2%, and 21%, respectively.
 |
Table 4 Antimicrobial Resistance Pattern of Bacterial Isolates from CSF Samples |
Discussion
In this study the overall prevalence of bacterial meningitis among children aged under 5 years was 13.2%, which is lower than a study conducted in Jimma, Ethiopia, that reported a prevalence of 30.6% from the 85 CSF samples analyzed.28 This difference could be due to the small size of the study conducted at Jimma. The other possible causes of the difference could be the time of CSF sample collection. In this study, about 62% of CSF samples were collected after empirical antimicrobial treatment, while the study conducted at Jimma reported that CSF samples were collected after treatment in about 52.9% patients.28 CSF sample collection after prior antimicrobial treatment could indeed contribute to culture negative results. The overall prevalence of bacterial meningitis in the current study was also lower than in a study conducted at Bahr Dar that reported a prevalence of 69.8%.33 This difference could be due to differences in diagnostic method. For the diagnosis of bacterial meningitis, the study conducted at Bahr Dar was mainly dependent on clinical diagnosis and Gram stain. On the other hand, the overall prevalence of bacterial meningitis was comparable with a study conducted in Addis Ababa, Ethiopia, that reported a prevalence of 14.1%.34
In the present study, the predominant cause of bacterial meningitis among children <5 years was S. pneumoniae (34.2%), this is similar with a study conducted in China where S. pneumoniae was reported to be the predominant isolate.35 The finding of the present study could be supported by studies conducted at Gonder, Addis Ababa, and Jimma which reported that the predominant isolates were S. pneumoniae at 70%, 35.3%, and 50% respectively.28,36,37
In the current study, the prevalence of N. meningitidis was 16%. This is higher than studies conducted in China (3.8%)38 and Addis Ababa (3.2%).34 Haemophilus influenzae b was isolated in 4 (10.5%) of the children with meningitis. This finding is comparable with a study conducted in China that reported a prevalence rate of H. influenzae b (9.5%)35 and it is also consistent with a study conducted in Jimma, Ethiopia which demonstrated 11.5% prevalence of H. influenzae b from culture proven cases.28 On the other hand, this finding is slightly higher than the prevalence of H. influenzae b reported in a study conducted in India (1.4%). This difference could be due to the large sample size of the study conducted in India and also socio-economic differences of the countries.39
Escherichia coli (66.7%) and S. agalactiae (100%) were the predominant organisms causing bacterial meningitis in infants aged 0–28 days. This is consistent with a study conducted in China.38 The results in this age group may be due to accidental transfer to newborns from the birth canal during delivery.
Regarding the antimicrobial susceptibility tests, the majority of the isolates were resistant to commonly used antibiotics such as ampicillin, chloramphenicol, ciprofloxacin, and ceftriaxone. In our study, antimicrobial susceptibility tests indicated that about 38.5% of S. pneumoniae isolates were resistant to ampicillin which is in line with other studies in Gonder, Ethiopia (43%)40 and in Nigeria.41 On the other hand, the ampicillin resistance rate of S. pneumoniae in this study was slightly lower than a study conducted in China that reported the ampicillin resistance rate of S. pneumoniae as 78.9%.35 This high rate of ampicillin resistance in all reported studies indicates the need for continued monitoring for ampicillin resistance in pneumococcal isolates due to frequent use of the drug.
More than half of E. coli isolates (60%) were resistant to ampicillin in this study. This is in line with a study conducted in China, which showed more than half of E. coli isolates showed resistance to ampicillin.42 In the present study, E. coli showed the highest resistance to ampicillin (60%), followed by H. influenzae b (50%) and S. pneumoniae (38.5%). One isolate of H. influenzae b showed a lower rate of resistance to ciprofloxacin and ceftriaxone. This is in line with a study in China that reported lower rates of resistance to ciprofloxacin and ceftriaxone.35 Unlike the study conducted at Gonder where no organism was found to be resistant to ciprofloxacin, in the present study E. coli and S. aureas showed 40% and 28.6% of isolates to be resistant. This could be due to a gradual rise in multi-drug resistant species of bacteria.
The antimicrobial resistance rates of N. meningitidis to chloramphenicol and ampicillin were 16.7% and 33.3%, respectively. This is similar to the study conducted in Gonder, Ethiopia, that reported N. meningitidis was found to be resistant to chloramphenicol 30%, and ampicillin 20%.40
High rates of multi-drug resistant isolates were also observed. Of all bacterial isolates, 42.1% were multi-drug resistant. This finding is comparable with the study conducted at Gonder.40 About 38.5% of S. pneumoniae showed multi-drug resistance, while about 33.3% of N. meningitidis, 50% of H. influenzae, 57.1% of S. aureas, and 40% of E. coli showed multidrug resistance.
Limitation of the Study
Despite a good outcome, we acknowledge a few limitations. The first limitation was that this study considered only CSF samples while additional blood culture could be important. The small sample size was the other limitation of this study.
Conclusion
In the present study, a high prevalence of bacterial meningitis was detected. From culture proven meningitis, S. pneumoniae was the leading cause of bacterial meningitis among children under 5 years old. N. meningitidis serotype Y/W135 was the most common strain isolated from CSF samples. H. influenzae type b was an important cause of bacterial meningitis and relatively common among infants aged 0–28 days. High rates of resistance were observed for most of the isolates of CSF samples. About 38.5% of S. pneumoniae showed multi-drug resistance, while about 33.3% of N. meningitidis, 50% of H. influenzae, 57.1% of S. aureas, and 40% of E. coli showed multi-drug resistance.
Data Sharing Statement
All the datasets generated and analyzed during the review are included in this article.
Acknowledgments
First of all, I would like to thank Dilla University for opening this opportunity for researchers to come with problem solving project ideas and scientific questions, and we also acknowledge the Dilla University Research Dissemination Office for funding this study.
My acknowledgement also goes to librarians for their support in kindly providing journals and relevant literatures.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Dilla University Research Dissemination Office (DURDO).
Disclosure
The authors have no conflict of interest to declare.
References
1. CDC. Signs and Symptoms Meningococcal Disease. Center for Disease Control and Prevention; 2014.
2. WHO/EMC/BAC. Control of Epidemic Meningococcal Disease.
3. WHO. Vaccine-Preventable Diseases: Haemophilus Influenzae. World Health Organization; 2018.
4. World Health Organization. Haemophilus influenzae type b (Hib) vaccination position paper. Wkly Epidemiol Rec. 2013;88(39):413–428.
5. McIntyre PB, O’Brien KL, Greenwood B, van de Beek D. Effect of vaccines on bacterial meningitis worldwide. Lancet. 2012;380(9854):1703–1711. doi:10.1016/S0140-6736(12)61187-8
6. Basarab M, Ihekweazu C, George R, Pebody R. Effective management in clusters of pneumococcal disease: a systematic review. Lancet Infect Dis. 2011;11(2):119–130. doi:10.1016/S1473-3099(10)70281-4
7. Buchholz G, Koedel U, Pfister HW, Kastenbauer S, Klein M. Dramatic reduction of mortality in pneumococcal meningitis. Crit Care. 2016;20(1):312. doi:10.1186/s13054-016-1498-8
8. CDC. Bacterial meningitis. Atlanta: Centers for Disease Control and Prevention; 2018. Available from: https://www.cdc.gov/meningitis/bacterial.html.
9. Olaf Hoffman W, Weber JR. Pathophysiology and treatment of bacterial meningitis. Ther Adv Neurol Disord. 2009;2(6):401–412. doi:10.1177/1756285609337975
10. Dzupova O, Rozsypal H, Prochazka B, Benes J. Acute bacterial meningitis in adults: predictors of outcome. Scand J Infect Dis. 2009;41(5):348–354. doi:10.1080/00365540902849391
11. Feigin EP. Bacterial Meningitis Beyond the Neonatal period.Textbook of Pediatric Infectious Diseases.
12. van de Beek D. Progress and challenges in bacterial meningitis. Lancet. 2012;380(9854):1623–1624. doi:10.1016/S0140-6736(12)61808-X
13. WHO. Global Burden of Meningitis. World Health Organization; 2018.
14. Zunt JR, Kassebaum NJ, Blake N, et al. Global, regional, and national burden of meningitis, 1990–2016: a systematic analysis for the global burden of disease. Lancet Neurol. 2018;17(12):1061–1082. doi:10.1016/S1474-4422(18)30387-9
15. van de Beek D, de Gans J, Tunkel AR, Wijdicks EFM. Community-acquired bacterial meningitis in adults. N Engl J Med. 2006;354(1):44–53. doi:10.1056/NEJMra052116
16. Dong BQ, Tang ZZ, Lin M. Epidemiologic surveillance for bacterial meningitis in 140,000 children under 5 years of age in Nanning District, Guangxi Province [in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:391–395.
17. Elliott JO, Richardson VE. The biopsychosocial model and quality of life in persons with active epilepsy. Epilepsy Behav. 2014;41:55–65. doi:10.1016/j.yebeh.2014.09.035
18. Edmond K, Clark A, Korczak VS, Sanderson C, Griffiths UK, Rudan I. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(5):317–328. doi:10.1016/S1473-3099(10)70048-7
19. WHO/CDS/CSR/EDC. Laboratory Methods for the Diagnosis of Meningitis Caused by Neisseria Meningitidis, Streptococcus Pneumoniae, and Haemophilus Influenzae. 2010.
20. Trotter CL, Lingani C, Fernandez K, et al. Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–15: an analysis of surveillance data. Lancet Infect Dis. 2017;17(8):867–872.
21. WHO. Standardized treatment of bacterial meningitis in Africa in epidemic and non epidemic situations. World Health Organization; 2005. Available from: www.who.int/csr/resources/publications/.
22. Haimanot RT, Caugant DA, Fekadu D. Characteristics of serogroup A N. meningitidis responsible for an epidemic in Ethiopia. Scand J Infect Dis. 1990;22(2):171–174. doi:10.3109/00365549009037898
23. Trotter CL, Greenwood BM. Meningococcal carriage in the African meningitis belt. Lancet Infect Dis. 2007;7(12):797–803. doi:10.1016/S1473-3099(07)70288-8
24. Michael Scheld W, Koedel U, Barnett Nathan P, Pfister H-W. Pathophysiology of bacterial meningitis: mechanism(s) of neuronal injury. J Infect Dis. 2002;186(2):S225–33. doi:10.1086/344939
25. Van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR. Advances in treatment of bacterial meningitis. Lancet. 2012;380(9854):1693–1702. doi:10.1016/S0140-6736(12)61186-6
26. Ahmed A. Etiology of Bacterial Meningitis in Ethiopia. A Retrospective Study. University of Oslo; 2012.
27. WHO. Pocket Book of Hospital Care for Children. World Health Organization; 2013.
28. Gudina EK, Tesfaye M, Wieser A, Pfister H-W, Klein M. Outcome of patients with acute bacterial meningitis in a teaching hospital in Ethiopia: a prospective study. PLoS One. 2018;13(7):e0200067. doi:10.1371/journal.pone.0200067
29. Burgey. Bergey’s Manual of Determinative Bacteriology. 2015.
30. EUCAST. European Committee on Antimicrobial Susceptibility Testing. 2016.
31. Leung P. Interhospital Multi-Disciplinary Programme on Antimicrobial ChemoTherapy. 2012.
32. Li X, Robinson SM, Gupta A, et al. Functional gold nanoparticles as potent antimicrobial agents against multi-drug-resistant bacteria. ACS Nano. 2014;8(10):10682–10686. doi:10.1021/nn5042625
33. Tewabe T, Fenta A, Tegen A, et al. Clinical outcomes and risk factors of meningitis among children in in Felege Hiwot Referral Hospital, Amhara Regional State, Ethiopia: a retrospective chart review. Ethiop J Health Sci. 2018;28(5):663.
34. Teklehymanot F, Legese MH, Desta K. Bacterial profile and their antimicrobial resistance patterns from body fluids at Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia. Biol Med (Aligarh). 2017;9(05):408. doi:10.4172/0974-8369.1000408
35. Jiang H, Su M, Kui L, et al. Prevalence and antibiotic resistance profiles of cerebrospinal fluid pathogens in children with acute bacterial meningitis in Yunnan province, China, 2012–2015. PLoS One. 2017;12(6):e0180161. doi:10.1371/journal.pone.0180161
36. Amare AT, Kebede ZT, Welch HD. Epidemiology of bacterial meningitis in children admitted to Gondar University Hospital in the post pneumococcal vaccine era. Pan Afr Med J. 2018;31:193. doi:10.11604/pamj.2018.31.193.10254
37. Hassen M. Prevalence of Bacterial Isolates from Cerebrospinal Fluid, Their Antimicrobial Susceptibility Pattern and Associated Risk Factors with Special Emphasis on Streptococcus Pneumoniae Among Pediatrics Suspected Meningitis Patients at Tikur Anbessa and Yekatit 12 Specialized Hospitals. Addis Ababa, Ethiopia; 2014.
38. Li C, Feng W-Y, Lin A-W. Clinical characteristics and etiology of bacterial meningitis in Chinese children >28 days of age, January 2014–December 2016: a multicenter retrospective study. Int J Infect Dis. 2018;74:47–53. doi:10.1016/j.ijid.2018.06.023
39. Sudharshan Raj C, Pradeep Reddy MA. Pattern and antibiogram of bacterial meningitis in children at a tertiary care hospital. J Sci Innov Res. 2013;2(6):1012–1016.
40. Mulu A, Kassu A, Tessema B. Bacterial isolates from cerebrospinal fluids and their antibiotic susceptibility patterns in Gondar University Teaching Hospital, Northwest Ethiopia. Ethiop J Health Dev. 2005;19(2).
41. Temitayo Oluwajenyo AA, Eberechukwu Y-IL. Pattern of cerebrospinal fluid analysis in children above the neonatal age as seen at the University of Port Harcourt Teaching Hospital. Port Harcourt Med J. 2019;10(3).
42. Chi L, Feng W-Y, Linc A-W. Clinical characteristics and etiology of bacterial meningitis in Chinese children >28 days of age. A multicenter retrospective study. Int J Infect Dis. 2018;74:47–53.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
