Back to Journals » ImmunoTargets and Therapy » Volume 9
Bacillus Calmette-Guérin (BCG) Therapy for Bladder Cancer: An Update
Authors Guallar-Garrido S , Julián E
Received 19 December 2019
Accepted for publication 28 January 2020
Published 13 February 2020 Volume 2020:9 Pages 1—11
DOI https://doi.org/10.2147/ITT.S202006
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Michael Shurin
Sandra Guallar-Garrido, Esther Julián
Departament de Genètica i de Microbiologia, Facultat de Biociències, Universitat Autònoma de Barcelona, Bellaterra (Barcelona), Spain
Correspondence: Esther Julián
Departament de Genètica i de Microbiologia, Facultat de Biociències, Universitat Autònoma de Barcelona, Bellaterra (Barcelona), Spain
Tel +34 93 5814870
Fax +34 93 5812387
Email [email protected]
Abstract: Physicians treating patients affected by nonmuscle-invasive bladder cancer (NMIBC) have been in shock during the last six years since manufacturing restrictions on the production of the first-option medicine, Mycobacterium bovis Bacillus Calmette-Guérin (BCG), have resulted in worldwide shortages. This shortage of BCG has led to a rethinking of the established treatment guidelines for the rationing of the administration of BCG. Some possible schedule modifications consist of a decrease in the length of maintenance treatment, a reduction in the dose of BCG in intravesical instillations or the use of different BCG substrains. All these strategies have been considered valuable in times of BCG shortage. In addition, the lack of availability of BCG has also led to the general recognition of the need to find new treatment options for these patients so that they are not dependent on a single treatment. Few alternatives are committed to definitively replacing BCG intravesical instillations, but several options are being evaluated to improve its efficacy or to combine it with other chemotherapeutic or immunotherapeutic options that can also improve its effect. In this article, we review the current state of the treatment with BCG in terms of all of the aforementioned aspects.
Keywords: mycobacteria, nonmuscle invasive, immunotherapy, alternative treatment
BCG History
Origin of BCG and Its Relationship with Bladder Cancer
Mycobacterium bovis Bacillus Calmette-Guérin (BCG) is a species originated after 230 recultures of the pathogen M. bovis. Over a period of thirteen years, Albert Calmette and Camille Guérin recultured isolated colonies from the originally pathogenic M. bovis. In 1921, they demonstrated that the obtained bacillus was not only non-pathogenic in animal models but also protected against tuberculosis challenge in vaccinated animals. Afterwards, the massive production of BCG was initiated for use in tuberculosis prevention in humans, and it is still the only commercially available vaccine against tuberculosis. At that time, the use of a mixture of two bacteria, Serratia marcescens and Streptococcus pyogenes, was investigated for cancer treatment, and the possibility to use the newly developed and safe BCG offered a novel therapeutic option for some cancer patients. Although some studies demonstrated the potential efficacy of the new BCG as a treatment for diverse types of cancer, it was not until the 1970s that BCG was approved as an immunotherapeutic treatment for bladder cancer (BC) patients.1
Since then, BCG has been the standard therapy for treating high-risk nonmuscle-invasive bladder cancer (NMIBC) patients to avoid the recurrence and progression of the disease. Intravesical instillations of hundreds of millions of bacilli are applied weekly in those patients over the course of six weeks (“induction treatment”) after the transurethral resection of tumors (TURBT) visible at the lumen surface of the bladder. If the patient responds appropriately to the therapy, a “maintenance treatment” consisting of six-week periods of instillation every three months for one to three years is then undertaken to reach the optimum effect for avoiding recurrence and progression episodes.
BCG Substrain Characteristics
When BCG was developed, seed lots were sent to different countries around the world. For over forty years, each laboratory recultured this mycobacterium with their own protocol for its maintenance and production; thus, BCG evolved differently in each laboratory, generating several substrains. The genetic comparison of the different BCG substrains has demonstrated the deletion of some regions of their genomes, the inclusion of single-nucleotide polymorphisms or insertion sequences, or the appearance of tandem duplications. The first elimination of the Region of Differentiation (RD) 1 and point mutations in the original M. bovis strain generated the earliest BCG substrains, formed by the parent BCG and the first daughter strains: BCG Russia, Moreau, Japan, Sweden and Birkhaug. Later, the deletion of RD2 led to the “late” group of strains, which included BCG Prague, Glaxo, Danish, Tice, Frappier, Connaught, Phipps and Pasteur.2–4
Changes in the genetic background led in some cases to different mycobacterial phenotypes. One of the main characteristics of mycobacteria is their cell wall, which contains long chains of mycolic acids, producing a highly hydrophobic and impermeable wall, as well as glycolipids, lipoproteins, glycans and proteins.5 Some of these lipids, such as mycolic acids, phthiocerol dimycocerosates (PDIM) or phenolic glycolipids (PGL), which have been related to the interaction with host cells, are not equally present on the surface of the different BCG substrains.6 For instance, BCG Moreau and Japan do not have PDIM and PGL, and both lipids have been related to the virulence and reactogenicity of mycobacteria. Otherwise, the substrains Moscow, Sweden, Birkhaug, Frappier, Pasteur, Phipps, Tice, Copenhagen, Prague and Connaught contain PDIM and PGL.7 Moreover, only early BCG strains contain three types of mycolic acids (alpha-, methoxy- and keto-mycolate), while the later strains contain only alpha- and keto-mycolates. The importance of the presence of the mentioned lipids is the differing ability to induce the activation of the immune system through distinct lipid immune receptors.5 Similarly, relevant proteinaceous antigens such as MPT64 or MBP70 are differentially expressed among BCG substrains. How those differences influence the immunogenic effect and safety of the different BCG substrains in NMIBC therapy is an issue that is still being researched.
Safety and Efficacy
As a therapeutic medicine in NMIBC patients, BCG is considered safe, although several adverse events have been described in BCG-treated NMIBC patients.8 Flu-like symptoms and/or burning discomfort in the bladder occur in the majority of patients. In the EORTC trial, the overall rate of adverse events in BCG-treated patients was as high as 70%, with 8% of patients discontinuing the treatment due to toxicity.9 Despite not being frequent, infections due to BCG, both local and, in rare cases, disseminated infections,10−13 have also been reported. In the case of BCG infection, antituberculosis drug treatment is prescribed, which consists of four daily antimicrobials for four months and two antimicrobials for two more months. When serious adverse events appear, intravesical instillations of BCG are stopped, and these patients are deprived of this efficacious treatment.
Regarding differences in safety and toxicity between the different BCG substrains, few studies have tried to address this issue. Recently, a comparison of the toxicity triggered by BCG Tice, Moreau and RIVM in 844 patients demonstrated that BCG Tice caused more local and mild systemic adverse effects than other tested BCG strains, while patients receiving BCG RIVM suffered more severe complications.14 Noticeably, those patients who received two different strains developed severe complications just after the treatment switch. In contrast, in another study in which BCG Connaught and BCG Japan were compared, the switch of substrains during the treatment reduced the adverse events found at the beginning of the treatment.15 All these data demonstrate the necessity of further studies to elucidate the safety of BCG strains in NMIBC patients.
Another relevant issue regarding BCG therapy is the efficacy of the different substrains. Some studies support the idea that no substrain seems to be clearly superior to the others. A recent meta-analysis comparing 10 BCG substrains was unable to find the best substrain,16 and a previously published retrospective study performed by Guerrero-Ramos et al found similar recurrence-free survival rates between patients who had received BCG Connaught and those who had received BCG Tice.17 Similar conclusions were reached by Unda-Urzaiz et al, who compared BCG Tokyo, Russian, Tice, Connaught and RIVM;18 Krajewski et al, who compared BCG Tice, Moreau and RIVM;14 and a recent study that compared the BCG Moreau and Tice substrains.19 However, Rentsh et al demonstrated that BCG Connaught was significantly more effective in terms of recurrence-free survival than BCG Tice.20 Hence, these results were not conclusive, and more research is required to determine whether shared features among all BCGs are the clue for the appropriate therapy or whether key components(s) exist in some strains that determine immunotherapeutic activity.
Current Situation for BC Treatment
BCG Shortages
The Beginning of the Problem
As explained above, different substrains spread during the last century when worldwide laboratories were mass producing BCG for tuberculosis vaccines in their own countries. When BCG was established for NMIBC therapy, the manufacturers modified the vial concentration (one dose of BCG for bladder cancer is similar to over 4000 doses of BCG for vaccination) and the formulation to be delivered into the bladder. Overall, few companies produce BCG for oncotherapy (Table 1) and export it worldwide. At the end of 2012, an unexpected event led to the collapse of the Sanofi factory producing BCG Connaught in Canada. In a routine Food and Drug Administration (FDA) inspection, mold was found in the area of BCG production due to previous natural floods. The forced closure of the factory to decontaminate the area stopped BCG production. At that time, the BCG Connaught produced and distributed by Sanofi was one of the main sources for BC treatment in North America and Europe, which are the regions with the highest incidence of BC around the world.21 Afterwards, Sanofi decided to stop the production of BCG and in mid-2017 confirmed that they were exiting the market. Moreover, during the last five years, problems in BCG production in other companies resulted in supply constraints from the main suppliers.22 Hence, the severity of the problem was dramatically increased due to both the increasing global demand for BC treatment and the announced anticipated shortages because suppliers depleted their stocks. Even the increased production of BCG by Merck of more than one hundred percent23 is still not enough to solve the enormous scarcity problem.
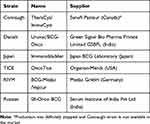 |
Table 1 BCG Production Worldwide for Bladder Cancer Treatment |
Clinical and Social Impact of BCG Shortages
BCG constraints have had an obvious clinical impact on BC treatment. Because of this situation, NMIBC patients might have received fewer doses of BCG than those recommended, might have received instillations of different BCG substrains depending on the BCG availability in each region, might have received a reduced length of standard maintenance therapy, and so forth. Moreover, there was an increased number of patients who had to be treated by cystectomy. Ourfali and coworkers estimated the clinical effect of BCG shortages between 2013 and 2016 in their unit of treatment.24 They found a significantly higher rate of recurrence at 24 months after TURBT for current intermediate- and high-risk NMIBC patients than for their patients diagnosed and treated during the three years before the BCG shortage. Apart from patient care, clinical trials have been affected, and BCG shortages have even partially affected the immunization programs for TB prevention in children around the world.25–27
From an economic point of view, Ourfali et al also found an increased cost due to the decrease in BCG production estimated at approximately €783 per patient with a new diagnosis of NMIBC during the period of restricted supply.24 Moreover, the prices of chemotherapies used for BC therapy spiked dramatically during a 2014 BCG shortage. In fact, that year, the price of mitomycin jumped by almost 100%. Data recorded in the USA demonstrated that the amount spent for mitomycin in the USA between 2012 and 2015 increased from $4.3 million to $15.8 million.28
Optimization of the Use of the Scarce Vials of BCG
As soon as BCG shortages began, different strategies were adopted at different levels, from improvements in BCG production to modifications of the recommended treatment.
Improving BCG Production
The production of BCG is not an easy matter. Due to the slow growth of the mycobacteria, any inaccuracy during the manufacturing process can lead to a large loss of time and money, as the BCG shortages have proven.22 For this reason, some researchers proposed optimizing BCG bulk production by modifying the growth in pellicles to the use of bioreactors29 or evaluating the possibility of extending the shelf life of the already manufactured BCG vials.30
Regulatory Issues/Favorable Policies
The effect of the decreased availability of BCG stocks is exacerbated in some countries where a particular BCG is the only source authorized for the treatment of BC patients. In the USA and Canada, for instance, OncoTICE from Merck is the only BCG available. A reasonable option would be importing BCG from other countries, but regulatory issues hinder a rapid supply, and clinical trials have to be conducted in some cases to introduce new substrains. In this sense, the SWOG Cancer Research Network is conducting a randomized control trial, S1602, that compares the Tokyo and TICE substrains, aiming to approve the use of other options for the treatment of US patients.31 Moreover, BC therapy becomes a serious issue in low- and middle-income countries where there are also limitations related to the higher cost of import taxes and shipment, as well as the longer time needed, for importing BCG.32 Thus, favorable policies should be implemented to facilitate access to alternative drugs in countries that cannot afford their current cost.
Variations in Clinical Guidelines Recommendations
There are multiple organizational guidelines that assist physicians in finding the most favorable intravesical BCG therapy. Since the first shortage of BCG and throughout the subsequent years when the shortage of BCG has persisted, international medical advisory boards have elaborated and adapted guideline recommendations to address the problem, although each strategy depends specifically on the BCG availability for each setting. For instance, guidelines such as those from the European Association of Urology (EAU),33,34 the American Urological Association (AUA)/Society of Urologic Oncology (SUO),35 the National Comprehensive Cancer Network (NCCN),36 and the National Institute for Health and Care Excellence (NICE)37,38 are constantly updated, taking advantage of published results addressing an improved NMIBC treatment to overcome BCG adverse events.39,40 Furthermore, all updated recommendations were collected and compared in a new guideline.41 Recently, the Bladder Cancer Advocacy Network (BCAN) released a joint statement with representatives of different urological societies to also help physicians in the current framework. The consensus of general recommendations to address BCG shortages is described below.
For intermediate-risk NMIBC patients (multicurrent-multifocal low-grade disease)
- Intravesical chemotherapy (mitomycin, gemcitabine or epirubicin) must be used as a first-option treatment instead of BCG. Induction once a week for six to eight weeks plus a monthly maintenance schedule for one year.
- For second-line treatment, a one-third dose of BCG instead of full-dose BCG can be used. In that case, different patients can be treated the same day clustered in groups of three to avoid BCG wastage.
- Maintenance BCG can be omitted.
For high-risk NMIBC
- Maintenance BCG therapy can be shortened to one year (instead of 3 years) for “low-tier” high-risk tumors (TaHG tumors).
- One-third of the BCG dose can be considered for both induction and maintenance.
- Other alternatives to BCG include mitomycin C (induction and maintenance up to one year) or electromotive mitomycin (EMDA-MMC). Other options, such as gemcitabine, epirubicin or sequential gemcitabine/docetaxel, may also be considered.
- Mandatory cystectomy is recommended in patients with very high-risk disease (T1HG tumors) associated with carcinoma in situ (CIS).
The uniform application of guideline recommendations in daily practice to guarantee drug availability is critically important. A recent study comparing daily practice with physicians’ knowledge of guidelines has found nonadherence by physicians to the recommendations. In this regard, an overtreatment with BCG instillations compared to the guideline recommendations has been found in both low-risk and intermediate-risk patients.42 Although an underuse of guideline-recommended intravesical treatments was previously reported,43,44 in the context of BCG shortage, it is especially relevant to understand why routine practice differs in some cases from the recommended guidelines to improve patient care. It is worth noting that the BCG shortage has resulted in an unusual increase in the prescription of BCG for CIS, which, although always recommended in the guidelines,33 was not applied properly by physicians.45
Future of Noninvasive BC Treatment
To rationalize the use of BCG, several valid strategies are performed, from designing different schedules of administration to manipulating BCG to improve its immunotherapeutic effect.
Improving BCG Treatment
Modification of Schedules. Priming–Boosting Strategy
On the one hand, an optimized immune effect triggered by intravesical BCG could lead to a reduction in the length of the treatment, saving BCG doses and potential adverse events, and could lead to the recovery of some nonresponsive BCG patients, who represent one of the main concerns for physicians due to the lack of treatment alternatives. An induction-boosting strategy could drive this increased immune effect. In 1976, Morales et al discarded the parallel intradermal vaccination with BCG and the intravesical BCG treatment in NMIBC patients, since no improvement was observed compared to BCG intravesical treatment alone.1 This was later confirmed in other studies.46–48 However, a recent study in a mice model showed that priming with BCG improved the triggered immune response of later intravesical treatments. In the same study, the authors performed a retrospective study in patients, showing that previous BCG vaccination had a significantly improved outcome compared with no previous BCG vaccination. Two clinical trials are in progress in which NMIBC patients are first intradermally vaccinated with mycobacteria and then further treated with intravesical BCG. Priming is performed in each trial with Tokyo BCG31 or RUTI (a therapeutic vaccine for tuberculosis).41,49 It is worth noting that Ji et al (2019) recently demonstrated the safety of BCG priming in NMIBC patients as well as the different responses of enhanced innate effector cells against some specific BC cell lines, suggesting a potential BCG resistance mechanism that could explain BCG nonresponsivity in some individuals.50
On the other hand, optimum maintenance schedule has not been clarified.51 Differences among the studies in the tumor stage of patients, treatment schedules, dose, BCG substrain and other parameters complicate the aim of achieving the best BCG maintenance schedule, and consequently, further research is needed to maximize the effect of the current treatment.
Recombinant BCGs
To maximize the antitumor effect of BCG as well as reduce the side effects, modifying BCG genetically to express additional immunomodulators such as cytokines or chemokines is widely explored.52 Notably, none of the constructs are currently considered in clinical trials. The most recently published studies focus on the use of bacterial antigens. Kanno et al improved the antitumor effect of BCG Moreau transformed with the detoxifed S1 subunit of pertussis toxin, which increased the Th1 immune response.53,54 Another approach consists of the use of recombinant BCG with the insertion of listeriolysin from Listeria monocytogenes, which modifies the phagosomal membrane in acidic conditions, and the deletion of urease C, which neutralizes the phagosome. These modifications lead to decreased pathogenicity and an increased release of antigens into the cytosol of infected macrophages and dendritic cells (DC), thus enhancing antigen presentation and T cell responses. After good toleration was shown in Phase I clinical trials, Phase II is currently ongoing.55,56 Finally, BCG effectiveness can be affected by antimicrobial peptides (AMPs) produced by mammalian cells to eliminate pathogens from the urinary tract. Cho et al produced recombinant BCG-expressing proteins that inhibit AMPs and lead to low survival of BC cells in vitro due to increased BCG internalization and cytokine secretion.57
Current Alternatives to BCG
Research on improving NMIBC therapy has mainly focused on rescue patients who do not respond to BCG therapy, since BCG is truly efficacious in the majority of patients for avoiding recurrence and progression episodes. The alternative treatment options include virus and other bacteria different from BCG as vehicles for specific tumor growth inhibition agents or immunostimulatory components, chemotherapeutic agents, new delivery options for current therapies, and systemic immunotherapies that have to be demonstrated to be efficacious in other types of cancers (Figure 1).
 |
Figure 1 Current alternative research for nonmuscle invasive bladder cancer treatment. |
Virus-Based Treatments
New approaches to improve the treatment of NMIBC also include the use of virus as a vehicle to specifically introduce genetic material into tumor cells. This approach is a hopeful technique for several reasons. Virus can be easily delivered into the bladder through the current procedure but has higher effectivity than BCG. In addition, due to its specificity and the use of a guided virus to a specific type of cells, the reported adverse events should decrease.58 Currently, there are several clinical trials ongoing. For instance, the enterovirus Coxsackievirus A21, which is in a phase I clinical trial, is an effective oncolytic virus targeting specifically intracellular adhesion molecule-1, enhancing cell lysis.59 Serotype 5 adenovirus (CG0070) with conditional replication that controls the expression of GM-CSF cytokine, important in durable antitumor activity, is in a phase II clinical trial in patients who failed BCG therapy. GM-CSF is also expressed in fowlpox virus, which is able to induce an immune response in unresponsive BCG patients after four intravesical doses.60 Moreover, a Phase III trial is currently evaluating the antitumor activity of a recombinant adenovirus that is able to transduce IFN-α into cancer cells with a polyamide surfactant to facilitate adherence.61 Due to the initial results in some studies demonstrating good response, we are waiting with high enthusiasm the coming results.
Bacteria-Based Treatments
One alternative to diminish the adverse events of BCG consists on using safer alternatives to intravesical instillations such as live or nonviable mycobacteria, bacteria other than mycobacteria or bacteria-derived components (reviewed in 62). For instance, the use of Salmonella has been proposed as a good alternative to treat the tumor because it is able to induce a massive infiltration of CD8+ cells, which correlates with better mouse survival rates.63 Salmonella enterica Choleraesuis or S. enterica Ty21a induced the infiltration of natural killer T cells with only one dose while BCG required multiple doses.64 A phase I clinical trial is currently assessing the safety of Ty21a (NCT03421236). In addition, Lactobacillus used as a food supplement is a safe microorganism that is able to induce NK cells, DCs and neutrophils, helping in the removal of the tumor.65 Another new immunotherapeutic agent is a vaccine using Pseudomonas aeruginosa mannose-sensitive hemagglutinin that increases antigen presenting function by activating the proliferation and differentiation of dendritic cells and further inhibits the proliferation of BC cell lines. This vaccine is available in China, although its efficacy and safety have not yet been verified.66,67 Moreover, because some mycobacterial components are ubiquitous in all mycobacterial species, the use of mycobacteria other than BCG has been studied for BC treatment. A M. phlei-derived complex called MCNA is being studied in clinical setting and is a good option for nonresponding BCG patients.68,69 Among nontuberculous mycobacteria, M. brumae has recently shown in preclinical studies a potential role in NMIBC since it inhibits tumor proliferation and triggers a proper antitumor immune response.70–72 One important issue of mycobacterial delivery remains their hydrophobicity and, consequently, clump formations. Hence, an optimized emulsion has been recently published to decrease clump formation, which leads to increased antitumor activity triggered by BCG and M. brumae.73
Chemotherapeutic Treatments and Improved Delivery
Different strategies can improve the use of chemotherapy for treating NMIBC. The appearance of new agents, the combination of different chemotherapeutic agents, the use of hyperthermia for improving intravesical instillation, or other strategies have been considered for improving the treatment of intermediate- and high-risk NMIBC patients.
Mitomycin C is a chemotherapeutic agent widely used in cases of BCG failure, but other options are also available, such as epirubicin, pirarubicin, and gemcitabine. In a recent study, intravesical gemcitabine induced a lower rate of recurrence, progression and treatment failure than epirubicin or pirarubicin.74 Furthermore, new multiagent intravesical chemotherapy regimens have been studied to improve the efficacy and tolerability of BCG (reviewed in 75). For instance, excellent responses have been found when administering gemcitabine with docetaxel, which seems to be an effective alternative to treat CIS when BCG cannot be administered, but further studies are needed.76
To decrease side effects, important for those patients who poorly tolerate BCG instillations while improving the efficacy of BCG, the combination of BCG with chemotherapeutic agents has also been studied. A recent meta-analysis concluded that the combination of both treatments appeared to be effective for intermediate- to high-risk NMIBC patients but not for other cases. Moreover, side effects were significantly decreased in patients who received BCG plus chemotherapy.77
The efficacy of intravesical therapies can also be improved through delivery adaptations such as hyperthermia, electromotive drug administration or new devices.
Hyperthermia is a safe and effective treatment that can also be combined with other therapies such as mitomycin C. Local delivery systems are approved in Europe and recommended for intermediate- and high-risk NMIBC patients, but further studies are required to decipher whether this technique can substitute for BCG instillations, which is the best system among all currently available; the right scheme to follow; and the best temperature of the device.78 Recently, Zhou et al demonstrated that three consecutive sessions, in which only the second session was combined with pirarubicin, was a safe and effective adjuvant treatment.79 Another possible solution to improve treatment delivery is electromotive administration to penetrate deeper into the tissue through an electrode while transporting the drug by iontophoresis. Despite encouraging results demonstrating the increased penetration of the drug using this technique, and the confirmation of excellent oncologic efficacy in high-risk BCG-unresponsive NMIBC patients,80–82 tolerability is still a challenge. As in other types of cancer, photodynamic therapy was also tested,83–86 but the efficacy of this treatment modality should be explored further in clinical trials.
Device-assisted therapies are also an attractive solution to improve the efficacy of chemotherapeutic treatments. With this aim, several devices are being developed to prolong the release of the drug over time, such as the GemRIS device, developed by Taris Biomedica. The device consists of a 5-cm semipermeable silicone tube that functions as an osmotic pump and slowly releases dissolving gemcitabine tablets.87 Pharmacokinetically, 60–70% of the drug load is delivered over 2 weeks, compared to the 2-h conventional dwell time for intravesical drugs. In the following years, it is highly expected that new device-assisted therapies will be improved and more offerings will be available due to the promising results after increasing the time of exposure together with BCG supply issues.
Checkpoint Inhibitors in Nonmuscle-Invasive BC
Many efforts have been focused on checkpoint inhibition therapies to block precise molecules, such as programmed death receptor 1 (PD-1), programmed death-ligand 1 (PD-L1), T-cell immunoglobulin and mucin domain-containing-3 (TIM-3), or cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), to rescue the suppressed antitumoral immune response. Success in preclinical and clinical studies for the treatment of muscle-invasive bladder cancer patients, for whom few therapeutic opportunities are available, led to FDA to approve some of these therapies. In the case of NMIBC, pembrolizumab, an anti-PD-1 therapy, has been granted by FDA as a priority review for a new supplemental Biologics License Application (sBLA).88 Merck is seeking approval for high-risk BCG-unresponsive NMIBC patients with CIS who are either ineligible for cystectomy or have chosen not to undergo the procedure (Keynote-057 and Keynote-676trial) (Keytruda, Merck). Despite hopeful results from checkpoint inhibitors, the combination of this therapy with chemotherapy or BCG is also being researched. For instance, the POTOMAC study, which analyzes the effect of combining the anti-PD-L1, durvalumab, plus BCG versus BCG alone, both in the induction and maintenance treatment of high-risk NMIBC patients, or the BMS-986205 study, which compares the administration of nivolumab or nivolumab in combination with BCG in BCG-unresponsive patients. Not only are safety and effectivity addressed in these studies but also the interest in obtaining a decreased cost of the treatment per patient.49,89
Concluding Remarks
BCG remains the gold-standard treatment for high-risk NMIBC patients. Although BCG is not easy to produce, today there are no real alternatives to BCG, and its production has to be maintained by any means. Nevertheless, the situation of recent years has prompted research for the study of possible therapeutic alternatives for these patients. Currently, most new therapeutic options are being tested in BCG-unresponsive patients. Few trials are performed to replace BCG. In view of the promising results that some of these new options show, new therapeutic options will be seen in the coming years. Another crucial point is to understand why BCG works in a percentage of patients while in others it does not. All of this will lead us to personalized treatment with a combination of therapies for longer bladder preservation times and better quality of life for patients.
Acknowledgments
This work was funded by the Spanish Ministry of Economy and Competitiveness (SAF2015-63867-R), the Spanish Ministry of Science, Innovation and Universities (RTI2018-098777-B-I00), the FEDER Funds, and the Generalitat of Catalunya (2017SGR-229). Sandra Guallar-Garrido is recipient of PhD fellowships (FI) from the Generalitat de Catalunya.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Morales A. BCG: a throwback from the stone age of vaccines opened the path for bladder cancer immunotherapy. Can J Urol. 2017;24(3):8788–8793.
2. Keller PM, Böttger EC, Sander P. Tuberculosis vaccine strain Mycobacterium bovis BCG Russia is a natural recA mutant. BMC Microbiol. 2008;8(1):120. doi:10.1186/1471-2180-8-120
3. Liu J, Tran V, Leung AS, Alexander DC, Zhu B. Human vaccines BCG vaccines: their mechanisms of attenuation and impact on safety and protective efficacy. Hum Vaccin. 2009;5(2):70–78. doi:10.4161/hv.5.2.7210
4. Zhang W, Zhang Y, Zheng H, et al. Genome sequencing and analysis of BCG vaccine strains. PLoS One. 2013;8:8. doi:10.1371/journal.pone.0071243
5. Noguera-Ortega E, Julián E. Mycobacteria-derived agents for the treatment of urological and renal cancers. Mycobacterium - Res Dev. 2018;305–324. doi:10.5772/intechopen.69659
6. Leung AS, Tran V, Wu Z, et al. Novel genome polymorphisms in BCG vaccine strains and impact on efficacy. BMC Genomics. 2008;9:1–12. doi:10.1186/1471-2164-9-413
7. Gan C, Mostafid H, Khan MS, Lewis DJM. BCG immunotherapy for bladder cancer–the effects of substrain differences. Nat Rev Urol. 2013;10(10):580–588. doi:10.1038/nrurol.2013.194
8. Liu Y, Lu J, Huang Y, Ma L. Clinical spectrum of complications induced by intravesical immunotherapy of bacillus calmette-guérin for bladder cancer. J Oncol. 2019;2019:1–11. doi:10.1155/2019/6230409
9. Brausi M, Oddens J, Sylvester R, et al. Side effects of bacillus calmette-guérin (BCG) in the treatment of intermediate- and high-risk Ta, T1 papillary carcinoma of the bladder: results of the EORTC genito-urinary cancers group randomised Phase 3 study comparing one-third dose with full dose an. Eur Assoc Urol. 2014;65(1):69–76. doi:10.1016/j.eururo.2013.07.021
10. Kaburaki K, Sugino K, Sekiya M, Takai Y, Shibuya K, Homma S. Miliary tuberculosis that developed after intravesical bacillus calmette-guerin therapy. Intern Med. 2017;56:1563–1567. doi:10.2169/internalmedicine.56.8055
11. Moussa M, Abou Chakra M. Granulomatous hepatitis caused by Bacillus Calmette-Guerin (BCG) infection after BCG bladder instillation: a case report. Urol Case Reports. 2018;20:3–4. doi:10.1016/j.eucr.2018.05.012
12. Ziegler J, Ho J, Gibson IW, et al. Disseminated Mycobacterium bovis infection post-kidney transplant following remote intravesical BCG therapy for bladder cancer. Transpl Infect Dis. 2018;20(5):e12931. doi:10.1111/tid.12931
13. Marques M, Vazquez D, Sousa S, Mesquita G, Duarte M, Ferreira R. Disseminated Bacillus Calmette-Guérin (BCG) infection with pulmonary and renal involvement: a rare complication of BCG immunotherapy. A case report and narrative review. Pulmonology. 2019. doi:10.1016/j.pulmoe.2019.10.001
14. Krajewski W, Matuszewski M, Poletajew S, Grzegrzółka J, Zdrojowy R, Kołodziej A. Are there differences in toxicity and efficacy between various Bacillus Calmette-Guerin strains in bladder cancer patients? Analysis of 844 Patients. Urol Int. 2018;101(3):277–284. doi:10.1159/000492722
15. Niwa N, Kikuchi E, Matsumoto K, Kosaka T, Mizuno R, Oya M. Does switching the bacillus Calmette-Guérin strain affect clinical outcome in patients with recurrent non–muscle-invasive bladder cancer after initial bacillus Calmette-Guérin therapy? Urol Oncol Semin Orig Investig. 2018;36(6):
16. Boehm BE, Cornell JE, Mukherjee N, Oppenheimer JS, Svatek RS. Efficacy of Bacillus Calmette-Guerin strains for the treatment of non-muscle invasive bladder cancer: a systematic review and network meta-analysis. J Urol. 2017;198(3):503–510. doi:10.1016/j.juro.2017.01.086
17. Guerrero-Ramos F, Lara-Isla A, Justo-Quintas J, Duarte-Ojeda JM, de la Rosa-kehrmann F, Villacampa-Aubá F. Adjuvant intravesical treatment for non-muscle invasive bladder cancer: the importance of the strain and maintenance. Actas Urológicas Españolas (English Ed). 2017;41(9):590–595. doi:10.1016/j.acuroe.2017.08.008
18. Unda-urzaiz M, Cozar-olmos JM, Miñana-Lopez B, et al. Safety and efficacy of various strains of bacille Calmette-Guérin in the treatment of bladder tumors in standard clinical practice. Actas Urológicas Españolas. 2018;42(4):238–248. doi:10.1016/j.acuroe.2018.03.004
19. D’Andrea D, Soria F, Gontero P, et al. Pd13-01 comparative effectiveness of intravesical bcg-tice and bcg-moreau in patients with non-muscle invasive bladder cancer. J Urol. 2019;201(Supplement4). doi:10.1097/01.ju.0000555381.73832.50
20. Rentsch CA, Birkhäuser FD, Biot C, et al. Bacillus calmette-guérin strain differences have an impact on clinical outcome in bladder cancer immunotherapy. Eur Urol. 2014;66(4):677–688. doi:10.1016/j.eururo.2014.02.061
21. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
22. Cernuschi T, Malvolti S, Nickels E, Friede M. Bacillus Calmette-Guérin (BCG) vaccine: a global assessment of demand and supply balance. Vaccine. 2018;36(4):498–506. doi:10.1016/j.vaccine.2017.12.010
23. Messing EM. The BCG shortage. Bl Cancer. 2017;3(3):227–228. doi:10.3233/BLC-179018
24. Ourfali S, Ohannessian R, Fassi-Fehri H, Pages A, Badet L, Colombel M. Recurrence rate and cost consequence of the shortage of bacillus calmette-guérin connaught strain for bladder cancer patients. Eur Urol Focus. 2019;19:30109. doi:10.1016/j.euf.2019.04.002
25. Working Group on BCG Vaccines S, WHO. Report on BCG Vaccine Use for Protection against Mycobacterial Infections Including Tuberculosis, Leprosy, and Other Nontuberculous Mycobacteria (NTM) Infections Prepared by the SAGE Working Group on BCG Vaccines and WHO Secretariat; 2017.
26. Li Z, Xu J, Xu J, Tan H, Zhang C. Current situation, causes, and countermeasures to NIP vaccine shortages in Guangzhou, China. Hum Vaccin Immunother. 2019;1–4. doi:10.1080/21645515.2019.1644883
27. SAGE, WHO. BCG vaccines Report on BCG vaccine use for protection against mycobacterial infections including tuberculosis, leprosy, and other nontuberculous mycobacteria (NTM) infections Prepared by the SAGE Working Group on BCG Vaccines and WHO Secretariat. 2017:1–77.
28. Davies BJ, Hwang TJ, Kesselheim AS. Ensuring access to injectable generic drugs - The case of intravesical BCG for bladder cancer. N Engl J Med. 2017;376(15):1401–1403. doi:10.1056/NEJMp1615697
29. Fitzpatrick M, Ho MM, Clark S, et al. Comparison of pellicle and shake flask-grown BCG strains by quality control assays and protection studies. Tuberculosis. 2019;114(October2018):47–53. doi:10.1016/j.tube.2018.10.013
30. Messina NL, Germano S, Bonnici R, et al. Can colony-forming unit testing be used to extend the shelf life of BCG vaccines? Tuberculosis. 2018;111:188–192. doi:10.1016/j.tube.2018.06.001
31. Svatek RS, Tangen C, Delacroix S, Lowrance W, Lerner SP. Background and update for s1602 “a phase III randomized trial to evaluate the influence of BCG strain differences and T cell priming with intradermal BCG before intravesical therapy for BCG-naïve high-grade non-muscle-invasive bladder cancer. Eur Urol Focus. 2018;4(4):522–524. doi:10.1016/j.euf.2018.08.015
32. Wroclawski ML, Schutz FA, Cha JD, Soares A. Alternative therapies to bacillus calmette-guérin shortage for nonmuscle invasive bladder cancer in Brazil and other underdeveloped countries: management considerations. J Glob Oncol. 2019;5:1–9. doi:10.1200/jgo.19.00112
33. Babjuk M, Böhle A, Burger M, et al. EAU guidelines on non–muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Assoc Urol. 2017;4(2):4–7. doi:10.1016/j.eururo.2016.05.041
34. Babjuk M, Burger M, Zigeuner R, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol. 2013;64(4):639–653. doi:10.1016/j.eururo.2013.06.003
35. AUA/SUO Joint Guideline. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Joint Guideline (2016); 2016.
36. The National Comprehensive Cancer Network. Non-Muscle-Invasive Bladder Cancer; 2015.
37. NICE guideline. Bladder cancer: diagnosis and management | Guidance | NICE. 2015.
38. NICE. 2019 Surveillance of Bladder Cancer: Diagnosis and Management (NICE Guideline NG2).; 2019.
39. Veeratterapillay R, Heer R, Johnson MI, Persad R, Bach C. High-risk non-muscle-invasive bladder cancer—therapy options during intravesical BCG shortage. Curr Urol Rep. 2016;17(68):1–7. doi:10.1007/s11934-016-0625-z
40. Oddens JR, Brausi M, Sylvester RJ, et al. Final results of an EORTC-GU cancers group randomized study of maintenance bacillus calmette-guérin in intermediate- and high-risk Ta, T1 papillary carcinoma of the urinary bladder: one-third dose versus full dose and 1 year versus 3 years of maintenance. Eur Urol. 2013;63(3):462–472. doi:10.1016/j.eururo.2012.10.039
41. Taylor J, Becher E, Steinberg GD. Review update on the guideline of guidelines: non- muscle-invasive bladder cancer. BJU Int. 2019. doi:10.1111/bju.14915
42. Hendricksen K, Aziz A, Bes P, et al. Discrepancy between European Association of Urology Guidelines and daily practice in the management of non-muscle-invasive bladder cancer: results of a European survey. Eur Urol Focus. 2019;2405(4569):681–688. doi:10.1016/j.euf.2017.09.002
43. Gontero P, Oderda M, Altieri V, et al. Are referral centers for non-muscle-invasive bladder cancer compliant to EAU guidelines? A report from the vesical antiblastic therapy Italian study. Urol Int. 2011;86(1):19–24. doi:10.1159/000321926
44. Witjes JA, Palou J, Soloway M, et al. Current clinical practice gaps in the treatment of intermediate-and high-risk non-muscle-invasive bladder cancer (NMIBC) with emphasis on the use of bacillus Calmette-Guérin (BCG): results of an international individual patient data survey (IPDS). BJU Int. 2013;112:742–750. doi:10.1111/bju.12012
45. Perera M, Papa N, Christidis D, et al. The impact of the global bacille Calmette–Guérin shortage on treatment patterns: population-based data. BJU Int. 2018;121(2):169–172. doi:10.1111/bju.14065
46. Lamm DL, DeHaven JI, Shriver J, Sarosdy MF. Prospective randomized comparison of intravesical with percutaneous bacillus Calmette-Guerin versus intravesical bacillus Calmette-Guerin in superficial bladder cancer. J Urol. 1991;145(4):738–740. doi:10.1016/s0022-5347(17)38439-2
47. Lüftenegger W, Ackermann DK, Futterlieb A, et al. Intravesical versus intravesical plus intradermal bacillus Calmette-Guerin: a prospective randomized study in patients with recurrent superficial bladder tumors. J Urol. 1996;155(2):483–487. doi:10.1016/S0022-5347(01)66427-9
48. Witjes JA, Fransen MPH, van der Meijden APM, Doesburg WH, Debruyne FMJ. Use of maintenance intravesical Bacillus Calmette-Guérin (BCG), with or without intradermal BCG, in patients with recurrent superficial bladder cancer. Urol Int. 1993;51(2):67–72. doi:10.1159/000282516
49. Packiam VT, Werntz RP, Steinberg GD. Current clinical trials in non-muscle-invasive bladder cancer: heightened need in an era of chronic BCG shortage. Curr Urol Rep. 2019;20(12):1–11. doi:10.1007/s11934-019-0952-y
50. Ji N, Mukherjee N, Morales EE, et al. Percutaneous BCG enhances innate effector antitumor cytotoxicity during treatment of bladder cancer: a translational clinical trial. Oncoimmunology. 2019;8:8. doi:10.1080/2162402X.2019.1614857
51. Chen S, Zhang N, Shao J, Wang X. Maintenance versus non-maintenance intravesical Bacillus Calmette-Guerin instillation for non-muscle invasive bladder cancer: a systematic review and meta-analysis of randomized clinical trials. Int J Surg. 2018;52:
52. Begnini KR, Buss JH, Collares T, Seixas FK. Recombinant Mycobacterium bovis BCG for immunotherapy in nonmuscle invasive bladder cancer. Appl Microbiol Biotechnol. 2015;99(9):3741–3754. doi:10.1007/s00253-015-6495-3
53. Kanno AI, Goulart C, Leite LCC, Pagliarone AC, Nascimento IP. A bivalent recombinant mycobacterium bovis BCG expressing the S1 subunit of the pertussis toxin induces a polyfunctional CD4 + T cell immune response. Biomed Res Int. 2019;2019:1–7. doi:10.1155/2019/9630793
54. Rodriguez D, Goulart C, Pagliarone AC, et al. In vitro evidence of human immune responsiveness shows the improved potential of a recombinant BCG strain for bladder cancer treatment. Front Immunol. 2019;10(JUN). doi:10.3389/fimmu.2019.01460
55. Nieuwenhuizen NE, Kulkarni PS, Shaligram U, et al. The recombinant bacille Calmette-Guérin vaccine VPM1002: ready for clinical efficacy testing. Front Immunol. 2017;8(1147):1–9. doi:10.3389/fimmu.2017.01147
56. Fletcher HA. Sleeping beauty and the story of the bacille Calmette-Guérin vaccine. MBio. 2016;7(4):1–3. doi:10.1128/mBio.01370-16
57. Cho MJ, Kim MJ, Kim K, et al. The immunotherapeutic effects of recombinant Bacillus Calmette-Guérin resistant to antimicrobial peptides on bladder cancer cells. Biochem Biophys Res Commun. 2019;509(1):167–174. doi:10.1016/j.bbrc.2018.12.097
58. Taguchi S, Fukuhara H, Homma Y, Todo T. Current status of clinical trials assessing oncolytic virus therapy for urological cancers. Int J Urol. 2017;24:342–351. doi:10.1111/iju.13325
59. Annels NE, Mansfield D, Arif M, et al. Phase I trial of an ICAM-1-targeted immunotherapeutic-coxsackievirus A21 (CVA21) as an oncolytic agent against non muscle-invasive bladder cancer. Clin Cancer Res. 2019;25(19):5818–5831. doi:10.1158/1078-0432.CCR-18-4022
60. Portal DE, Weiss RE, Wojtowicz M, et al. Phase I neoadjuvant study of intravesical recombinant fowlpox-GM-CSF (rF-GM-CSF) or fowlpox-TRICOM (rF-TRICOM) in patients with bladder carcinoma. Cancer Gene Ther. 2019;20. doi:10.1038/s41417-019-0112-z
61. Tse J, Singla N, Ghandour R, Lotan Y, Margulis V. Current advances in BCG-unresponsive non-muscle invasive bladder cancer. Expert Opin Investig Drugs. 2019;28(9):757–770. doi:10.1080/13543784.2019.1655730
62. Julián E, Noguera-Ortega E. Bacteria-derived alternatives to live Mycobacterium bovis Bacillus Calmette-Guerin for nonmuscle invasive bladder cancer treatment. Microb Infect Cancer Ther Recent Adv. 2019;1(4):123–188. doi:10.1201/9781351041904
63. Ronquillo Pangilinan C, Lee CH. Salmonella-based targeted cancer therapy: updates on a promising and innovative tumor immunotherapeutic strategy. Biomedicines. 2019;7:36. doi:10.3390/biomedicines7020036
64. Domingos-Pereira S, Sathiyanadan K, La Rosa S, et al. Intravesical Ty21a vaccine promotes dendritic cells and T cell–mediated tumor regression in the MB49 bladder cancer model. Cancer Immunol Res. 2019;7(4):621–629. doi:10.1158/2326-6066.CIR-18-0671
65. Feyisetan O, Tracey C, Hellawell GO. Probiotics, dendritic cells and bladder cancer. BJU Int. 2012;109(11):1594–1597. doi:10.1111/j.1464-410X.2011.10749.x
66. Zhu YP, Bian XJ, Ye DW, et al. Pseudomonas aeruginosa-mannose-sensitive hemagglutinin inhibits proliferation and induces apoptosis in a caspase-dependent manner in human bladder cancer cell lines. Oncol Lett. 2013;5(4):1357–1362. doi:10.3892/ol.2013.1201
67. Chang L, Xiao W, Yang Y, et al. Pseudomonas aeruginosa -mannose–sensitive hemagglutinin inhibits epidermal growth factor receptor signaling pathway activation and induces apoptosis in bladder cancer cells in vitro and in vivo. Urol Oncol Semin Orig Investig. 2014;32(1):
68. Li R, Amrhein J, Cohen Z, Champagne M, Kamat AM. Efficacy of Mycobacterium Phlei Cell Wall-Nucleic Acid Complex (MCNA) in BCG-unresponsive patients Abbreviations BCG Bacillus Calmette-Guerin BCG non-muscle invasive bladder cancer MCNA Mycobacterium phlei cell wall-nucleic acid complex. Bl Cancer. 2017;3:65–71. doi:10.3233/BLC-160084
69. Morales A, Herr H, Steinberg G, et al. Efficacy and safety of MCNA in patients with nonmuscle invasive bladder cancer at high risk for recurrence and progression after failed treatment with bacillus Calmette-Guérin. J Urol. 2015;193(4):1135–1143. doi:10.1016/j.juro.2014.09.109
70. Noguera-Ortega E, Rabanal RM, Gómez-Mora E, Cabrera C, Luquin M, Julián E. Intravesical Mycobacterium brumae triggers both local and systemic immunotherapeutic responses against bladder cancer in mice. Sci Rep. 2018;8(15102). doi:10.1038/s41598-018-33253-w
71. Noguera-Ortega E, Rabanal RM, Secanella-Fandos S, Torrents E, Luquin M, Julián E. Irradiated mycobacteria enhance survival in bladder tumor bearing mice although less efficaciously than live mycobacteria. J Urol. 2016;195(1):198–205. doi:10.1016/j.juro.2015.07.011
72. Noguera-Ortega E, Secanella-Fandos S, Eraña H, et al. Nonpathogenic mycobacterium brumae inhibits bladder cancer growth in vitro, ex vivo, and in vivo. Eur Urol Focus. 2015;2(1):
73. Noguera-Ortega E, Blanco-Cabra N, Rabanal RM, et al. Mycobacteria emulsified in olive oil-in-water trigger a robust immune response in bladder cancer treatment. Sci Rep. 2016;6:27232. doi:10.1038/srep27232
74. Wang T, Yuan H, Diao W, Yang R, Zhao X, Guo H. Comparison of Gemcitabine and Anthracycline Antibiotics in Prevention of Superficial Bladder Cancer Recurrence. 2019:1–5.
75. Steinberg RL, Thomas LJ, O’Donnell MA. Combination intravesical chemotherapy for non–muscle-invasive bladder cancer. Eur Urol Focus. 2018;4(4):503–505. doi:10.1016/j.euf.2018.07.005
76. Thomas L, Steinberg R, Nepple KG, O’Donnell MA. Sequential intravesical gemcitabine and docetaxel in the treatment of BCG-naive patients with non-muscle invasive bladder cancer. J Clin Oncol. 2019;37(7_suppl):469. doi:10.1200/jco.2019.37.7_suppl.469
77. Huang D, Jin YH, Weng H, Huang Q, Zeng XT, Wang XH. Combination of intravesical bacille calmette-guérin and chemotherapy vs. Bacille calmette-guérin alone in non-muscle invasive bladder cancer: a meta-analysis. Front Oncol. 2019;9(121). doi:10.3389/fonc.2019.00121
78. Wells BYH, Harris M. Bladder cancer: where are we with intravesical therapies? 2016;20(5):20–23.
79. Zhou J, Li L, Li X, et al. Efficacy analysis of a novel thermochemotherapy scheme with pirarubicin for intermediate- and high-risk nonmuscle-invasive bladder cancer: a single-institution nonrandomized concurrent controlled trial. Int J Hyperth. 2019;36(1):868–875. doi:10.1080/02656736.2019.1646929
80. Racioppi M, DI Gianfrancesco L, Ragonese M, Palermo G, Sacco E, PF B. ElectroMotive drug administration (EMDA) of Mitomycin C as first-line salvage therapy in high risk “bCG failure” non muscle invasive bladder cancer: 3 years follow-up outcomes. BMC Cancer. 2018;18(1):1–9. doi:10.1186/s12885-018-5134-7
81. Di Stasi SM, Valenti M, Verri C, et al. Electromotive instillation of mitomycin immediately before transurethral resection for patients with primary urothelial non-muscle invasive bladder cancer: a randomised controlled trial. Lancet Oncol. 2011;12(9):871–879. doi:10.1016/S1470-2045(11)70190-5
82. Gan C, Amery S, Chatterton K, Khan MS, Thomas K, O’Brien T. Sequential bacillus calmette-guérin/electromotive drug administration of mitomycin C as the standard intravesical regimen in high risk nonmuscle invasive bladder cancer: 2-year outcomes. J Urol. 2016;195:1697–1703. doi:10.1016/j.juro.2016.01.103
83. O’Brien T, Ray E, Chatterton K, Khan MS, Chandra A, Thomas K. Prospective randomized trial of hexylaminolevulinate photodynamic-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs conventional white-light TURBT plus mitomycin C in newly presenting non-muscle-invasi. BJU Int. 2013;112:1096–1104. doi:10.1111/bju.12355
84. Lee JY, Diaz RR, Cho KS, et al. Efficacy and safety of photodynamic therapy for recurrent, high grade nonmuscle invasive bladder cancer refractory or intolerant to bacille calmette-Guérin immunotherapy. J Urol. 2013;190(4):1192–1199. doi:10.1016/j.juro.2013.04.077
85. Railkar R, Agarwal PK. Photodynamic therapy in the treatment of bladder cancer: past challenges and current innovations. Eur Urol Focus. 2018;4(4):509–511. doi:10.1016/j.euf.2018.08.005
86. Bader MJ, Stepp H, Beyer W, et al. Photodynamic therapy of bladder cancer - a phase i study using Hexaminolevulinate (HAL). Urol Oncol Semin Orig Investig. 2013;31(7):1178–1183. doi:10.1016/j.urolonc.2012.02.007
87. Grimberg DC, Shah A, Inman BA. Overview of taris GemRIS, a novel drug delivery system for bladder cancer. Eur Urol Focus. 2019;2019–2021. doi:10.1016/j.euf.2019.09.006
88. FDA grants priority review to Merck’s Supplemental Biologics License Application (sBLA) for KEYTRUDA® (pembrolizumab) in certain patients with high-risk, Non-Muscle Invasive Bladder Cancer (NMIBC). Available from: https://www.businesswire.com/news/home/20191202005300/en/FDA-Grants-Priority-Review-Merck’s-Supplemental-Biologics.
89. Bilgin B, Sendur MAN, Hizal M, Yalçın B. An update on immunotherapy options for urothelial cancer. Expert Opin Biol Ther. 2019;19(12):1265–1274. doi:10.1080/14712598.2019.1667975
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
