Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Awareness of COPD and Its Risk Factors Among the Adult Population of the Aseer Region, Saudi Arabia
Authors Esam Mahmood S , A Alqahtani AT, Alghamdi BAA, Gazzan MA, A Alqahtani MY, Y Alfaifi NA, Alsaleem SA, Riaz F , Tauheed Ahmad M, Ahmad A, Suhail Khan M, Saquib Abullais S
Received 21 June 2022
Accepted for publication 17 September 2022
Published 9 January 2023 Volume 2023:18 Pages 23—35
DOI https://doi.org/10.2147/COPD.S378064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Syed Esam Mahmood,1 Abdullah Thabit A Alqahtani,2 Bader Abdulmohsen A Alghamdi,2 Mohammed Ali Gazzan,2 Meshari Yahya A Alqahtani,2 Nada Ali Y Alfaifi,3 Safar A Alsaleem,1 Fatima Riaz,1 Mohammad Tauheed Ahmad,4 Ausaf Ahmad,5 Mohammad Suhail Khan,6 Shahabe Saquib Abullais7
1Department of Family & Community Medicine, College of Medicine, King Khalid University, Abha, Saudi Arabia; 2College of Medicine, King Khalid University, Abha, Saudi Arabia; 3College of Medicine, Jazan University, Jazan, Saudi Arabia; 4Department of Medical Education, College of Medicine, King Khalid University, Abha, Saudi Arabia; 5Department of Community Medicine, Integral Institute of Medical Science and Research, Integral University, Lucknow, India; 6Department of Public Health, College of Applied Medical Sciences, KhamisMushait, King Khalid University, Abha, Saudi Arabia; 7Department of Periodontics and Community Dental Sciences, College of Dentistry, King Khalid University, Abha, Saudi Arabia
Correspondence: Syed Esam Mahmood, Department of Family & Community Medicine, College of Medicine, King Khalid University, Abha, 62529, Saudi Arabia, Tel +966550484344, Email [email protected]
Introduction: Epidemiological studies are urgently needed to assess the prevalence of COPD in the region to determine the baseline, against which the future trends in the risk factor levels can be assessed and preventive strategies be planned to promote health among the population. Therefore, this study was undertaken to assess the awareness of COPD and its risk factors in Saudi Arabia.
Materials and Methods: The cross-sectional study was conducted among the general adult population aged 18 years and above living in the Aseer region. A minimum sample of 385 was targeted, using the Raosoft sample size calculator. An online questionnaire was prepared in both English and Arabic language using Google forms and distributed among participants through social media.
Results: It was observed that less than one-third (116, 30.12%) of the study population had ever heard about COPD. Nearly one-third spent time with smokers. Among all, 223 (57.3%) respondents had never heard and 46 (11.9%) respondents did not know anything about COPD. The majority correctly knew that the lungs are the primary organ affected by COPD (92, 79.3%). Age, sex, marital status, income, and occupation showed a significant association with COPD awareness. Nearly 41.4% knew that COPD progresses exclusively with age, COPD is more expensive for society than lung cancer (49.0%), cigarette smoking affects COPD (34.5%), COPD is fully recoverable with short-term antibiotics (35.0%), COPD lasts more than 18 months (48.1%), COPD can worsen with smoke exposure (37.4%), lead to disability (46.7%) and quitting smoking has an important role in preventing COPD (34.0%).
Conclusion: The awareness regarding the disease was low among the respondents. Only one-third correctly knew that quitting smoking has an important role in preventing COPD. This study projects an urgent need of improving awareness of COPD and its risk factors in the general population.
Keywords: COPD, knowledge, Saudi Arabia, survey, questionnaire
Introduction
Chronic obstructive pulmonary disease (COPD) is generally characterized by the presence of chronic bronchitis or emphysema that can lead to airway obstruction.1 It is a disease of the airways and lungs that is characterized by a progressive airflow limitation, which is not fully reversible and is associated with an abnormal inflammatory response of the lungs to noxious particles or gases.2 This leads to poor airflow, cough, shortness of breath, and frequent exacerbations, which are often due to infections. In severe cases, it would progress into respiratory failure and pulmonary heart disease, which can have a significant impact on patient’s quality of life.3 COPD is a major cause of morbidity and mortality worldwide.4 Currently, it is the third leading cause of death5,6 and reported as the fifth-largest economic burden worldwide.7 The development of COPD is multifactorial and the risk factors of COPD include both genetic and environmental factors. Some important environmental factors are outdoor air pollution, cigarette smoking, occupational exposure to dust and fumes, biomass smoke inhalation, exposure to second-hand smoke, and previous tuberculosis.8 Interestingly, passive smoking and exposure to smoke from biomass fuel combustion for heating have also been involved in the development of COPD in women.9,10
The global prevalence of COPD is increasing with an estimated mean prevalence of 13% among the general population aged 40 years and above.11,12 Data on COPD prevalence from regions such as the Middle East are virtually absent or often based on inadequate definitions. One population-based` study observed a COPD prevalence of 3.5% in Middle Eastern populations based on reported symptoms of COPD or diagnosed COPD and smoking history. In a study among Saudi smokers aged more than 40 years in primary care clinics, the prevalence of spirometry-confirmed COPD was 14.2%. These regional studies suggest that individuals who are asymptomatic or who have never smoked are unlikely to receive an early diagnosis of COPD, and the true prevalence of the disease is thus underestimated.13–15 There is a low level of awareness of COPD reported among smokers in Saudi Arabia.16 This lack of awareness probably contributes to the marked underdiagnosis of the disease, which is apparent virtually everywhere in the world, although to various degrees. Studies have shown that health education regarding COPD is insufficient not only in general population but also among disease sufferers17 and even the family members of patients who have COPD.18,19
The high prevalence of smoking in Saudi Arabia, the low number of chest physicians, and poor compliance with the COPD guidelines increase the burden of respiratory diseases such as COPD.12,13 The prevalence of COPD will increase even further, unless broad and effective preventive measures are implemented. Hence, awareness is crucial to promote prevention by smoking cessation, enable early diagnosis, and tailor treatment accordingly.12 The increase in awareness of the disease, treatment, and management in the populations shall result in better COPD care and management.13 In fact, lack of knowledge about COPD is one of the major barriers regarding combating against COPD.20 There is a need to conduct more epidemiological studies regarding COPD.21 Decreasing the incidence of COPD would substantially benefit the overall health of the individuals.7 Many individuals can prevent themselves from the disease or get the right treatment at the right time if they know about the disease. To the best of our knowledge, there is no published data or study about the knowledge of COPD and its risk factors among the general population of Saudi Arabia, especially in the Aseer region. Epidemiological studies are urgently needed22 to assess the prevalence of COPD in the region to determine the baseline, against which the future trends in the risk factor levels can be assessed and preventive strategies be planned to promote health among the populations. Therefore, this study was undertaken to assess the awareness of COPD and its risk factors among the adult population in the region.
Materials and Methods
Study Area and Population
The descriptive cross-sectional study was conducted in the Aseer Region, the southern of the Kingdom of Saudi Arabia. The general adult population aged 18 years and above living in the Aseer region during the study period from 1st August 2021 to 31st May 2022 was included.
Sample Size and Technique
All conveniently accessible populations who are fulfilling the eligibility criteria were invited to participate in the study. A minimum sample of 385 was targeted, using the formula.
n = (z)2 p (1 – p)/d2
where Sample size = n, p = 50%, the confidence level 95%, so Z score = 1.96, margin of error (E)=5% and Population 100,000.
The necessary calculated sample was 385 individuals.
Non-probability sampling technique, ie convenience sampling, was used. Patients were included based on their easy availability and willingness to participate in our research project.
Inclusion and Exclusion Criteria
All adult patients aged 18 years and above currently living in the Aseer region were included. Those below 18 years of age and not willing to participate in the study were excluded.
Ethical Approval and Data Collection
Approval was obtained from the Research Ethics Committee of King Khalid University, Aseer, KSA. Data was not disclosed for patient confidentiality. The use of these confidential data in this research project was reviewed and approved by the research ethics committee. The collected data was kept safely in a password-protected cloud.
An anonymous, self-explanatory, questionnaire was designed to assess the knowledge of COPD among the participants. The online questionnaire was prepared in both English and Arabic language using Google forms and distributed among participants through social media and E-mail as face-to-face interviews had to be avoided following the social distancing norms enforced by the government. Electronic voluntary informed consent was attached before the questionnaire in the provided links, and the participants had approved before filling the questionnaire. A pilot study was conducted on 20 participants, to increase the credibility of the questionnaire. The pilot responses were excluded from the final responses of the study. The questionnaire was categorized into the following parts: (1) Demographics and general characteristics were obtained. (2) Awareness of COPD: information was obtained through closed-ended questions that should be answered only in “Yes”, “No” or “Don’t know”.
Data Management and Analysis Plan
The collected data were coded and entered into an Excel software (Microsoft office Excel 2010) database. Data were analyzed using Statistical Package for Social Sciences, version 16.0 (SPSS, Inc., Chicago, IL, USA). Data were presented in descriptive statistics like, frequency and percentage as appropriate.
Tests of significance like the Chi-square test are applied to find out the statistical significance of the difference in percentages. Univariate analysis was done using respondent awareness about COPD as the dependent variable and the sociodemographic and behavioral factors were identified as independent variables. A p-value of <0.05 was taken as statistically significant for the calculations of variables.
Results
Out of 385 respondents, 10.9% were cigarette smokers, 9.9% were electronic smokers and 9.1% were shisha smokers. Majority
(36.4%) of respondents usually spent time or sat with their smoker friends. Dust exposure (26.2%) was the second most common form of risk among the respondents. A higher proportion of the respondents used heating devices based on coal (19.0%), followed by those who spent time in a shisha cafe (11.7%) (Figure 1).
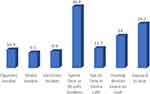 |
Figure 1 Distribution of study population based on their type of exposure to smoke/dust. |
In the present study, it was observed that less than one-third (116, 30.12%) of the study population had ever heard about COPD. Among all, 223 (57.3%) respondents had never heard and 46 (11.9%) respondents did not know anything about COPD. Figure 2 also shows the percentage of respondents who knew about the primary organ affected by COPD (116, 30.12%). Among those who had heard about COPD (n = 116), when queried “Which organ is affected by COPD?”, 92 (79.3%) correctly responded lungs, 12 (10.3%) responded heart, nine (7.7%) responded trachea, one (0.8%) responded throat, and two (1.7%) did not know (Figure 2).
 |
Figure 2 Distribution of the respondents based on their awareness about COPD and their knowledge of the primary organ affected by COPD. |
Only 1.3% of respondents self reported that they had been diagnosed with COPD. All those diagnosed with COPD were Saudi males, were aged between 18 and 39 years and the majority of them were smokers (80%) (Figure 3).
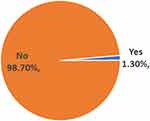 |
Figure 3 Percent distribution of respondents ever diagnosed with COPD. |
Table 1 illustrates the association of respondents who had ever heard of COPD with their sociodemographic status. Almost 99% were Saudi nationals. The majority of respondents were aged between 18 and 29 years out of which 41.9% had ever heard of COPD. A higher proportion of male (41.1%) respondents had heard of COPD as compared to the female respondents (17.4%). A higher proportion of the respondents were unmarried (n = 211) followed by married (n = 170), out of which 89 (42.2%) unmarried and 25 (14.7%) married respondents had ever heard of COPD. More than fifty percent of respondents had an income of less than 5000 SAR. Nearly 37.8% of them had heard of COPD. Almost more than three-fourth of respondents were having a higher university degree. However, only 31.9% of respondents from the university level had ever heard of COPD. Most of the respondents were students (41.03%) and officers (39.2%). Sociodemographic variables such as age group, sex, marital status, income, and occupation showed a significant association with awareness of COPD.
 |
Table 1 Association Between Socio-Demographic Variables and Awareness of COPD Among Respondents |
Table 2 illustrates the association between respondents smoking behaviours (cigarette smoker, shisha smoker, electronic smoker, spending time or sit with smokers, spending time in shisha cafes), heating devices based on coal and exposure to dust with awareness of COPD. The study outcome reported that smoking behaviours were not found to be statistically significant, whereas only respondents having exposure to dust were found statistically significant among those who had ever heard of COPD. Among smokers, cigarette smoking was more common among respondents. The majority of respondents (140/385, 36.3%) spent time or sitting with smokers, out of which 35.7% had heard about COPD. Out of 385 respondents, only 101 (26.2%) were exposed to dust. Among those who were exposed to dust, one-fifth of respondents had ever heard of COPD.
 |
Table 2 Association Between Smoke and Dust Exposure and Awareness of COPD |
Table 3 represents awareness of the respondents pertaining to COPD. Among those who were aware of COPD (n = 116), the most common symptom known was cough (52.17%) followed by shortness of breath (39.6%). Out of a total of 116 respondents who had heard of COPD, nearly 41.4% knew that COPD is exclusive because of progress in age, COPD is expensive for society more than lung cancer (49.0%), cigarette smoking affects COPD (34.5%), COPD is fully recoverable with short-term use of antibiotics (35.0%), COPD is rare (18.8%), COPD lasts more than 18 months (48.1%), COPD can get worse with smoke exposure (37.4%), COPD can lead to disability (46.7%), and quitting smoking has an important role in preventing COPD (34.0%).
 |
Table 3 Respondents Answers Pertaining to Awareness of COPD |
Discussion
Chronic obstructive pulmonary disease is one of the commonest diseases among smokers and passive smokers as well. It affects the lungs and causes breathing difficulties hence having an impact on the daily adjusted life years (DALYs) of patients. StigHagstad et al reported the prevalence of COPD in Sweden, which showed that among non-smokers prevalence was found to be 7.7%, whereas among smokers it was 18.3%.23
DD Ghorpade et al reported that 99.1% of the Indian population never heard of the word COPD, whereas only 0.9% heard about COPD. Out of the population who heard about COPD 72% think that the lungs, 6% think that the heart is affected by COPD, whereas 22% do not know which organ is affected by COPD.24 While our study reported that 30% had heard the term COPD, about 57.9% of the population never heard, and 11.9% did not know about COPD. Out of 30% of the population who heard had about COPD, 79.3% thought that it affects the lungs, 7.7% thought that it affects the heart, 10.34% thought that it affects the throat, 1.72% thought trachea, and 0.86% did not know about the organ affected by COPD.
Awareness of COPD in our study is almost similar to the study conducted by MasaharuAsai et al which showed 21.3% awareness in the Japanese population.25 A population-based study in north-eastern Italy had a prevalence of COPD at about 6.8% according to self-reported physician diagnosis.26
Data obtained from the National Health and Nutrition Examination Survey (NHANES) reported an age-standardized prevalence of self-reported COPD of about 3.47%,27 whereas in our study we found that only 1.30% of respondents were ever diagnosed with COPD. About 14.33% have mineral dust exposure and 5.2% have exhaust fumes exposure. However, more than half of our respondents also believe that COPD is not a rare disease. The difference might be associated with the awareness, exposure to the risk factors, or even correct diagnosis by the physicians. Cigarette smokers are thought to be the most at risk of developing COPD. However, recent studies have shown that people with life-long exposure to biomass smoke are also at high risk of developing COPD. Most common in developing countries, biomass fuels such as wood and coal are used for cooking and heating indoors daily. Women and children have the highest amounts of exposure and are therefore more likely to develop the disease. Despite epidemiological studies providing evidence of the causative relationship between biomass smoke and COPD, there are still limited mechanistic studies on how biomass smoke causes, and contributes to the progression of COPD.28 Among nonsmokers, there is 10.2% environmental tobacco exposure (ETS) at home and 12.6% have ETS in public places and 20.3% have exposure in dedicated spaces.29
According to our study awareness of COPD was more among the Saudi population than the non-Saudis. This can be attributed to the fact that the newly arrived expatriates might not be aware of the health care programs available in the Kingdom. In our study, about 41.9% of the population who were aware of COPD belonged to the 18–29 years of age group, and those who have university education 31.9% were also more aware than higher education 24%, which is showing the direct relationship of educational status with awareness regarding COPD. The majority of our respondents also believe that COPD is an age-related disease in this study. This reflects that they also think that as age progresses COPD worsens. In Saudi Arabia, the prevalence of smoking (cigarettes and waterpipes) is estimated to be 20%, compared with 16.2% in Canada, 16.8% in the United States, 14.7% in Australia, and 12.1% in Qatar.30 Majority of Saudi smokers are of young age as well and its prevalence keeps on rising among young adolescents, which is quite alarming.31 Household air pollution is generated from cooking and heating using biomass and coal, collectively known as solid fuels. Exposure to household air pollution, including dust, heating devices, wood, coal, and fuel burning, is associated with increased prevalence and mortality of COPD.32
Household air pollution is considered one of the primary risk factors for non-smoking-related COPD especially in low- and middle-income countries.33 In our study, we found that 19% of our respondents have exposure to heating devices and 26.2% have exposure to dust. This is alarming in terms of the development of COPD in the future, and suitable preventive measures should be taken for such people. According to the 2018 National Health Interview Survey (NHIS), 27.6% of the population were smokers, 12.0% of females, and 15.6% of males were current cigarette smokers in adults aged ≥18 years in the United States.34
Among our study population, about 29.9% of total respondents were having tobacco smoke exposure, 10.9% were cigarette smokers, 9.9% were electronic smokers, and 9.1% were shisha smokers. These exposures keep them at high risk to the development of respiratory diseases including COPD, whereas 19.4% of Spanish general population was smoker.35
Electronic cigarettes (e-cigarettes) are battery-operated electronic nicotine devices, which consist of a mouthpiece (to inhale), a power source, a heating element (atomizer), and a disposable cartridge or refillable tank with liquid solution (e-liquid). The e-liquid contains propylene glycol, glycerin, nicotine, and flavor chemicals. Upon puffing-activated heating, the e-liquid is atomized, and the smoker inhales the resulting aerosol or vapor. These chemicals are well-known causative agents for the development of not only respiratory diseases but also cancers.36 Cai et al reported that in August 2018, the FDA declared e-cigarette use in youth an epidemic thereafter several immediate actions were taken to establish new policies aimed at preventing youth access to e-cigarettes. These actions and their implementations should be conducted by the Ministry of the health of Saudi Arabia as well to prevent youth from using e-cigarettes and their health hazards.37 Not only active smoking, shisha, and e-cigarettes, passive smoking also causes COPD. StigHagstad et al reported that passive smoking through environmental exposure to smoke (ETS) ever at home was associated with a higher prevalence of COPD compared with non-exposed subjects (8.0% vs 4.2%, P 5 0.004).29
A large percentage 36.4% of our study population usually spend time or sit with his/her smoker friends, 19.0% were in habit of using heating devices based on coal and 11.7% spend time in shisha cafes. So a total of 67.1% of our study population have exposure to passive smoking. This is proven to be as dangerous as smoking itself and imposes bad health outcomes in the future. The majority of our respondents who were aware of COPD think that it affects the throat (50%), heart (42.9%), and trachea (40%), whereas in another study by Ghorpade et al respondent’s knowledge was more about the lung (71.4%) as an affected organ for COPD. About 34.5% think that it is caused by smoking.24
Mohigefer et al reported that medical student’s knowledge regarding commonest symptom was dyspnea (80.3%) and giving up smoking prevented worsening of COPD (96.6%), whereas in our general population of respondents they think cough was 52% as the commonest symptom of COPD and dyspnea thereafter (39.66%).38 About 30% of people think that quitting smoking can prevent COPD in our study. The difference in knowledge regarding common symptoms is obvious because among the general population idea about COPD is not much understood as compared to medical students. This imposes great responsibility on health care professionals about public health education regarding COPD and quitting smoking.
Nearly half of our respondents think that COPD lasts a maximum of 18 months, 37.4% think that further smoke exposure worsens the COPD and 46.7% think that it can cause disabilities. Almost half of our respondents also think that the treatment of COPD is very expensive even more than the treatment of cancer. This is comparable to another study where majority of respondents (80%) believe that life expectancy is about 14 years among patients with COPD, 85% believe that it causes arrhythmias and 88% think it can cause lung cancer as well.39 In the previous study, it is been shown that severity of COPD increases with progressive age.40 Age is one of the concomitant factors regarding worsening COPD.41
In 2015, COPD caused 2.6% of global disability-adjusted life years (DALYs) and ranked eighth globally, and recently, it is reported as the fifth-largest economic burden worldwide.7,42 These figures reflect that there is a need to provide correct information to the people about the disease itself and lifelong consequences including the impact on disability-adjusted life years as well which a patient might face in their life if having COPD. It increases the importance of avoidance of risk factors for COPD for prevention and control of the disease.
Almost half of our respondents also think that the treatment of COPD is very expensive even more than the treatment of cancer. More than half of the respondents also believe that it cannot be cured with the use of antibiotics. Trends were observed in multiple studies of direct and healthcare costs for European countries measured by patient and year, where the higher costs were associated with more severe COPD and a frequent history of exacerbations. The highest costs reported corresponded to hospitalizations and the associated pharmacological treatment. The importance of the loss of productivity and premature retirement within the profile of the COPD patient was also highlighted as the main generator of indirect costs of the disease.43 However, we can also enumerate in future studies that web-based interventions might be beneficial for the health education regarding COPD.44
Our study has a few limitations. The cross-sectional nature of this study and convenience sampling used cannot confirm the causality association between the compared variables. The self-reported responses could over or underestimate the results. Also, the subjects for the study were chosen from a particular region, and thus they may not have been the representatives of the entire Kingdom. Considering that patients were included through social media, there could be a high risk of selection bias toward younger people and from a high social class. However, our study area had a representative mix of subjects, with all the different age groups and socioeconomic classes. A larger nationwide study can be conducted involving different regions to know the trends of the increasing blood COPD among the general population. However, making an attempt to assess the awareness of COPD in the general population in Saudi Arabia is the strength of our study. Most of the previous studies have been conducted in health professionals before.45,46
Conclusion
In the present study, we found that less than one-third of the study population had ever heard about COPD. Nearly one-third spent time or sat with smokers. A higher percentage of population was cigarette smokers (10.9%), followed by electronic smokers (9.9%) and shisha smokers (9.1%). The awareness regarding the disease was low among the respondents. Only 34.0% correctly knew that quitting smoking has an important role in preventing COPD. This study projects an urgent need of improving awareness of COPD and its risk factors in the general population. This subject should be strengthened in the curriculum and discussed in public campaigns and seminars. Further nationwide study is required to help the policymakers for implementing suitable preventive and curative strategies to promote the pulmonary health of the population.
Funding
The authors extend their appreciation to the Deanship of Scientific Research at King Khalid University, Saudi Arabia for funding this work through Small Groups Project under grant number RGP.1/62/43.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Carré PC, Roche N, Neukirch F., et al. The effect of an information leaflet upon knowledge and awareness of COPD in potential sufferers. A randomized controlled study. Respir Int Rev Thorac Dis. 2007;76:53–60.
2. Ken RB, Brusselle GG. Chronic obstructive pulmonary disease. In: Mestecky J, Strober W, editors. Mucosal Immunology.
3. Śliwiński P, Puchalski K. Chronic obstructive pulmonary disease in the awareness of Polish society. Report from the public opinion survey by the Polish Respiratory Society and TNS Polska. Pneumonol Alergol Pol. 2015;83(1):1–13. doi:10.5603/PiAP.2015.0001
4. Cook S, Eggen AE, Hopstock LA, et al. Chronic Obstructive Pulmonary Disease (COPD) in population studies in Russia and Norway: comparison of prevalence, awareness and management. Int J Chron Obstruct Pulmon Dis. 2021;16:1353. doi:10.2147/COPD.S292472
5. Tan WC, Lo C, Jong A, et al. Marijuana and chronic obstructive lung disease: a population-based study. Can Med Assoc J. 2009;180(8):814–820. doi:10.1503/cmaj.081040
6. Mehta AJ, Miedinger D, Keidel D, et al.; SAPALDIA Team. Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss cohort study on air pollution and lung and heart diseases in adults. Am J Respir Crit Care Med. 2012;185(12):1292–1300. doi:10.1164/rccm.201110-1917OC.
7. Kida K, Wakabayashi R, Mizuuchi T, et al. Screening for suspected chronic obstructive pulmonary disease with an eleven-item preinterview questionnaire (11-Q). Intern Med. 2006;45(21):1201–1207. doi:10.2169/internalmedicine.45.1694
8. Nelson SB, Lavange LM, Nie Y, et al. Questionnaires and pocket spirometers provide an alternative approach for COPD screening in the general population. Chest. 2012;142(2):358–366. doi:10.1378/chest.11-1474
9. Beeh KM, Kornmann O, Beier J, et al. Clinical application of a simple questionnaire for the differentiation of asthma and chronic obstructive pulmonary disease. Respir Med. 2004;98(7):591–597. doi:10.1016/j.rmed.2004.01.004
10. Sana A, Somda SMA, Meda N, Bouland C. Chronic obstructive pulmonary disease associated with biomass fuel use in women: a systematic review and meta-analysis. BMJ Open Respir Res. 2018;5(1):e000246. PMID: 29387422; PMCID: PMC5786909. doi:10.1136/bmjresp-2017-000246
11. Seo JY, Hwang YI, Mun SY, et al. Awareness of COPD in a high risk Korean population. Yonsei Med J. 2015;56(2):362–367. doi:10.3349/ymj.2015.56.2.362
12. Tinkelman DG, Price D, Nordyke RJ, et al. COPD screening efforts in primary care: what is the yield? Prim Care Respir J. 2007;16:41–48. doi:10.3132/pcrj.2007.00009
13. Kögler H, Metzdorf N, Glaab T, et al. Preselection of patients at risk for COPD by two simple screening questions. Respir Med. 2010;104(7):1012–1019. doi:10.1016/j.rmed.2010.01.005
14. Pinkerton M, Chinchilli V, Banta E, et al. Differential expression of microRNAs in exhaled breath condensates of patients with asthma, patients with chronic obstructive pulmonary disease, and healthy adults. J Allergy Clin Immunol. 2013;132(1):217–219. doi:10.1016/j.jaci.2013.03.006
15. Tan WC, Sin DD, Bourbeau J, et al.; Can COLD collaborative research group. Characteristics of COPD in never-smokers and ever-smokers in the general population: results from the CanCOLD study. Thorax. 2015;70(9):822–829. doi:10.1136/thoraxjnl-2015-206938.
16. Alhomayani FKH, Almalki SH, Alqahtani M, Almalki AH. Awareness of Chronic Obstructive Pulmonary Disease (COPD) among smokers in Saudi Arabia: a cross-sectional study. Am J Med Sci Med. 2019;7(5):184–189.
17. Raptis DG, Rapti GG, Papathanasiou IV, Papagiannis D, Gourgoulianis KI, Malli F. Level of knowledge about COPD among patients and caregivers. In: GeNeDis 2020. Cham: Springer; 2021:299–305).
18. Lee SH, Lee H, Kim YS, Park HK, Lee MK, Kim KU. Predictors of low-level disease-specific knowledge in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2020;15:1103. doi:10.2147/COPD.S244925
19. Robinson SA, Cooper JA, Goldstein RL, et al. A randomised trial of a web-based physical activity self-management intervention in COPD. ERJ Open Res. 2021;7(3):00158–2021. doi:10.1183/23120541.00158-2021
20. O’Toole J, Krishnan M, Riekert K, Eakin MN. Understanding barriers to and strategies for medication adherence in COPD: a qualitative study. BMC Pulm Med. 2022;22(1):1–8. doi:10.1186/s12890-022-01892-5
21. Golpe R, Dacal-Rivas D, Blanco-Cid N, Castro-Añón O. Need for epidemiological studies on chronic obstructive pulmonary disease in Rural Spain. Arch Bronconeumol. 2021;1:S0300–2896.
22. Price DB, Yawn BP, Jones RCM. Improving the differential diagnosis of chronic obstructive pulmonary disease in primary care. Mayo Clin Proc. 2010;85(12):1122–1129. doi:10.4065/mcp.2010.0389
23. StigHagstad H, Backman AB, Ekerljung L, et al. Prevalence and risk factors of COPD among never-smokers in two areas of Sweden e Occupational exposure to gas, dust or fumes is an important risk factor. Respir Med. 2015;109(11):1439–1445. doi:10.1016/j.rmed.2015.09.012
24. Ghorpade DD, Raghupathy A, Londhe JD, et al. COPD awareness in the urban slums and rural areas around Pune city in India. NPJ Prim Care Respir Med. 2021;31(1):6. doi:10.1038/s41533-021-00220-4
25. Asai M, Tanaka T, Kozu R, et al. Effect of a Chronic Obstructive Pulmonary Disease (COPD) intervention on COPD awareness in a regional city in Japan. Intern Med. 2015;54(2):163–169. doi:10.2169/internalmedicine.54.2916
26. Guerriero M, Caminati M, Viegi G, et al. COPD prevalence in a north-eastern Italian general population. Respir Med. 2015;109(8):1040–1047. doi:10.1016/j.rmed.2015.05.009
27. Doney B, Kurth L, Halldin C, et al. Occupational exposure and airflow obstruction and self-reported COPD among ever-employed US adults using a COPD-job exposure matrix. Am J Ind Med. 2019;62(5):393–403. doi:10.1002/ajim.22958
28. Capistrano SJ, van Reyk D, Chen H, et al. Evidence of biomass smoke exposure as a causative factor for the development of COPD. Toxics. 2017;5(4):36. doi:10.3390/toxics5040036
29. Hagstad S, Bjerg A, Ekerljung L, et al. Passive smoking exposure is associated with increased risk of COPD in never smokers. Chest. 2014;145(6):1298–1304. doi:10.1378/chest.13-1349
30. Alsubaiei ME, Cafarella PA, Frith PA, et al. Factors influencing management of chronic respiratory diseases in general and chronic obstructive pulmonary disease in particular in Saudi Arabia: an overview. Ann Thorac Med. 2018;13(3):144–149. doi:10.4103/atm.ATM_293_17
31. Moradi-Lakeh M, El Bcheraoui C, Tuffaha M, et al. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: findings from a national survey. BMC Public Health. 2015;15(1):611. doi:10.1186/s12889-015-1902-3
32. Siddharthan T, Grigsby MR, Goodman D, et al. Association between household air pollution exposure and chronic obstructive pulmonary disease outcomes in 13 Low- and middle-income country settings. Am J Respir Critic Care Med. 2018;197(5):611–620. doi:10.1164/rccm.201709-1861OC
33. Gut-Gobert C, Cavailles A, Dixmier A, et al. Women and COPD: do we need more evidence? Eur. Respir. Rev. 2019;28(151):180055. doi:10.1183/16000617.0055-2018
34. Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults — United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68:1013–1019. doi:10.15585/mmwr.mm6845a2
35. Rubio MC, Hermosa JL, Miravitlles M, López-Campos JL. Knowledge of chronic obstructive pulmonary disease, presence of chronic respiratory symptoms and use of spirometry among the Spanish population: CONOCEPOC 2019 study. Arch Bronconeumol. 2021;57(12):741–749. doi:10.1016/j.arbr.2021.10.003
36. Centers for Disease Control and Prevention [CDC] (2019b). Outbreak of lung injury associated with the use of E-cigarette, or vaping, products. Available from: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
37. Cai H, Garcia JGN, Wang C. More to add to E-cigarette regulations: unified approaches. Chest. 2020;157(4):771–773. doi:10.1016/j.chest.2019.11.024
38. Mohigefer J, Calero-Acuña C, Marquez-Martin E, et al. Understanding of COPD among final-year medical students. Int J Chron Obstruct Pulmon Dis. 2017;13:131–139. doi:10.2147/COPD.S138539
39. Akshaya A, Priya VV, Don KR, et al. Awareness on risk factors of Chronic Obstructive Pulmonary Disease (COPD) among college students. Eur J Mol Clin Med. 2020;7(1):2681–2699.
40. Fathima M, Bawa Z, Mitchell B, Foster J, Armour C, Saini B. COPD management in community pharmacy results in improved inhaler use, immunization rate, COPD action plan ownership, COPD knowledge, and reductions in exacerbation rates. Int J Chron Obstruct Pulmon Dis. 2021;83:519. doi:10.2147/COPD.S288792
41. Elsa LP, Justo G, Blanca L. Patient’s awareness on COPD is the strongest predictor of persistence and adherence in treatment-naïve patients in real life: a prospective cohort study. BMC Pulm Med. 2021;21(1):1. doi:10.1186/s12890-020-01377-3
42. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. Erratum in: Lancet Respir Med. 2017 Oct;5(10): e30.PMID: 28822787; PMCID: PMC5573769. doi:10.1016/S2213-2600(17)30293-X
43. Gutiérrez Villegas C, Paz-Zulueta M, Herrero-Montes M, et al. Cost analysis of chronic obstructive pulmonary disease (COPD): a systematic review. Health Econ Rev. 2021;11(1):31. PMID: 34403023; PMCID: PMC8369716. doi:10.1186/s13561-021-00329-9
44. Mongiardo MA, Robinson SA, Finer EB, Rivera PN, Goldstein RL, Moy ML. The Effect of a web-based physical activity intervention on COPD knowledge: a secondary cohort study. Respir Med. 2021;190(190):106677. doi:10.1016/j.rmed.2021.106677
45. Alshahrani A, Gautam AP, Aseeri F, et al. Knowledge, attitude, and practice among physical therapists toward COVID-19 in the Kingdom of Saudi Arabia—A cross-sectional study. Healthcare. 2022;10(1):105. doi:10.3390/healthcare10010105
46. Asdaq SMB, Alshrari AS, Imran M, Sreeharsha N, Sultana R. Knowledge, attitude and practices of healthcare professionals of Riyadh, Saudi Arabia towards covid-19: a cross-sectional study. Saudi J Biol Sci. 2021;28(9):5275–5282. doi:10.1016/j.sjbs.2021.05.036
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
