Back to Journals » International Journal of Women's Health » Volume 7
Awareness and predictors of female genital mutilation/cutting among young health advocates
Authors Abolfotouh S, Ebrahim AZ, Abolfotouh M
Received 3 December 2014
Accepted for publication 15 January 2015
Published 20 February 2015 Volume 2015:7 Pages 259—269
DOI https://doi.org/10.2147/IJWH.S78664
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Elie Al-Chaer
Sherif M Abolfotouh,1,2 Ahmed Z Ebrahim,1,3 Mostafa A Abolfotouh4
On Behalf of IFMSA-Egypt
1IFMSA-Egypt, Alexandria, Egypt; 2Oulu University Hospital, Oulu, Finland; 3Alexandria Faculty of Medicine, Alexandria, Egypt; 4King Abdullah International Medical Research Center (KAIMRC), King Saud bin-Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Abstract: The act of female genital mutilation/cutting (FGM/C) is considered internationally as a violent act against girls and women and a violation of their human rights. This study sought to assess the awareness and predictors of FGM/C in young Egyptian health advocates. A cross-sectional study of 600 medical students from a total of 2,500 members of the International Federation of Medical Students’ Associations (IFMSA)-Egypt, across all Egyptian medical schools, was conducted using a previously validated online Google survey. The overall prevalence of circumcision was 14.7/100 female students, with a significantly higher prevalence in students from rural areas (25%) than in non-rural areas (10.8%, P=0.001), and in those residing in Upper (southern) Egypt (20.6%) than in Lower (northern) Egypt (8.7%, P=0.003). The students’ mean percentage score for knowledge about the negative health consequences of FGM/C was 53.50±29.07, reflecting a modest level of knowledge; only 30.5% had a good level of knowledge. The mean percentage score for the overall attitude toward discontinuation of the practice of FGM/C was 76.29±17.93, reflecting a neutral attitude; 58.7% had a favorable attitude/norms toward discontinuation of the practice. Of circumcised students, approximately one-half (46.8%) were unwilling to have their daughters circumcised, and 60% reported no harm from being circumcised. After controlling for confounders, a negative attitude toward FGM/C was significantly (P<0.001 in all cases) associated with male sex, residency in Upper Egypt, rural origin, previous circumcision, and the preclinical medical phase of education. The low level of knowledge among even future health professions in our study suggests that communication, rather than passive learning, is needed to convey the potentially negative consequences of FGM/C and to drive a change in attitude toward discontinuation of this harmful practice.
Keywords: FGM/FC, circumcision, IFMSA-Egypt, medical education, reproductive health, child abuse, women’s rights
Introduction
Female genital mutilation/cutting (FGM/C) is defined by the World Health Organization (WHO) as “all procedures that involve partial or total removal of the external female genitalia or other injury to the female genital organs for non-medical reasons.”1 It is typically carried out, with or without anesthesia, by a traditional circumciser using a knife or razor. The age of the girls who undergo this procedure varies from weeks after birth to puberty.2 Common early complications of FGM/C include uncontrolled bleeding, fever, wound infection, sepsis, and death.3 FGM/C is also reported to cause psychological consequences, such as anxiety, horror, posttraumatic stress disorders, and depression.4–6 Long-term complications include dysmenorrhea, dyspareunia, recurrent vaginal and urinary tract infections, infertility, cysts, abscesses, keloid formation, difficulty with childbirth, and sexual dysfunction.3,7–11
The origin of FGM/C remains unclear; however, the practice is thought to have occurred in ancient Egypt, Ethiopia, and Greece.12 Although these origins are pre-Islamic, FGM/C is often associated with Islam because of the religion’s focus on female modesty and chastity.13 However, it is worth noting that neither the Bible nor Quran make any reference to FGM/C.14 FGM/C is forbidden in Judaism, yet, in Ethiopia, there resides a Jewish minority group, often referred to as Falashas or Beta Israel, who practice this procedure.15
FGM/C is practiced as a cultural ritual by ethnic groups in 28 countries in Sub-Saharan and Northeast Africa,2 and, to a lesser extent, in Asia, the Middle East, and within immigrant communities in other regions.16 The practice is also found in South America, in some indigenous communities in Colombia.2 More than 125 million girls and women alive today have been subject to FGM/C in the 29 countries in Africa and the Middle East where the practice is highly concentrated. Of these individuals, approximately one in five live in Egypt.12 Indeed, the most recent Egyptian Demographic Health Survey (2008) estimated the prevalence of FGM/C in Egypt to be 91% of all 15- to 49-year-old women.16 Most of these women had undergone type I or type II circumcision, whereas type III FGM/C was predominant in Djibouti, Somalia, and Sudan, as well as in areas of Eritrea and Ethiopia. The United States Agency for International Development estimated in 2008 that approximately 8 million women in Africa over the age of 15 years had undergone type III circumcision.11
Opposition to FGM/C began in Egypt when The Egyptian Doctors’ Society called for a ban in the 1920s. In 1928, Ali Ibrahim Pasha – a surgeon and the director of Cairo University – spoke out against the practice. Following this, in 1951, an Egyptian medical journal, Al Doktor, published an article criticizing the act of FGM/C, as did an Egyptian women’s magazine, Hawwaa, in 1957. In 1958 it became illegal to perform FGM in any of Egypt’s state-run health facilities.17 However, the practice continued illegally in various venues across the country as was publicized internationally in 1995 when a US news channel broadcast images of a 10-year-old girl undergoing FGM in a barber’s shop in Cairo.18 As a result, the government reversed the 1959 ban so that physicians could legally perform FGM,17 but this legalization of the practice seemed to have little effect in protecting women and girls from illegal operations: in 2007, a 12-year-old girl died during an FGM/C procedure that was conducted by a physician in an illegal clinic. In 2008, the Al-Azhar Supreme Council of Islamic Research, the highest religious authority in Egypt, ruled that FGM/C has no basis in core Islamic law, enabling the government to completely outlaw FGM/C.19
Health workers may be confronted with FGM/C in various contexts and can have an important role in eliminating this practice.20 However, to solicit the active involvement of health workers as advocates against FGM/C, medical professionals and health workers should be equipped with the appropriate knowledge and skills to help them educate others about FGM/C, as well as to provide clinical and psychological care and support for girls and women who have undergone the procedure, taking into account sociocultural and personal sensitivities.20–22 In spite of this, many countries, including Egypt, rarely mention or cover FGM/C in detail in the training curricula for health professionals, nurses, midwives, and other health workers.20 However, a group of medical students from around the world has taken positive steps toward increasing awareness about FGM/C among medical students and young medical professionals as a part of a transnational project. This project was endorsed by the International Federation of Medical Students’ Associations (IFMSA), which recently adopted a policy statement in March 2013 calling for immediate action to stop this ongoing practice.23
In light of recent action toward increasing awareness of FGM/C among health professionals, the current study sought 1) to assess awareness of FGM/C among student members of IFMSA-Egypt in terms of their knowledge of the negative health consequences of FGM, attitude toward the discontinuation of FGM/C, and personal experience of FGM/C and 2) to identify predictors of their willingness to discontinue the practice of FGM/C. In addition, we sought to explore female students’ opinions about their own circumcision status. This study was performed as part of the FGM Peer-Education Project, which aims to reduce FGM/C in Egypt and ensure that medical students in Egypt adopt a positive attitude/norms toward the discontinuation of FGM/C by raising awareness about the religious, legal, and clinical aspects of the procedure. Thus, the aims of this study were: 1) to assess the members of IFMSA-Egypt’s level of knowledge of the negative health consequences of FGM/C, 2) to determine their attitude/norms toward discontinuation of this practice, and 3) to identify the predictors of FGM/C among female medical students.
Methods
Study design
A cross-sectional study was applied.
Study population and sampling techniques
The study was conducted on enrolled members of IFMSA-Egypt, a nonpolitical, nonreligious, student-run Egyptian non-governmental organization working in the fields of health awareness and advocacy, including reproductive health. The FGM Peer-Education Project researchers wanted to assess the knowledge and attitude of the organization’s members toward FGM, and thus assess their capacity to conduct and maintain the project as leading health advocates in Egypt. The study involved 600 members/medical students who constituted 24% of IFMSA-Egypt’s total 2,500 members in all Egyptian medical schools at the time the study was conducted (November 2012–April 2013).
Questionnaire
A Google survey was structured according to a similar questionnaire in English that was conducted and validated in Oslo in 2012,24 and was disseminated in English throughout the IFMSA-Egypt’s national and local online members’ mailing lists on Yahoo and Google Groups. All participants who responded were included in the study population, and all submitted an online informed consent form before they started the questionnaire.
Data collection
For all questions, except those relating to age and birthplace, the answers were selected from a multiple-choice grid to ensure the accuracy and completeness of the data collection and to standardize the procedures. The questionnaire was separated into four sections covering the following topics:
- Personal characteristics and sociodemographic details, including sex, educational year, education phase (preclinical and clinical), origin of birth (urban and rural), and residency (Upper and Lower Egypt).
- The participants’ knowledge about the medical complications of FGM/C was assessed through questions about whether FGM/C leads to bleeding, infection, complications during childbirth, and possible HIV transmission. The total knowledge and percentage scores for each participant were calculated based on the answers given to each question: “yes” was assigned a score of 1; “no/do not know” was assigned a score of 0. For subsequent analyses, mean percentage scores (MPS) <50% were combined to form the category “poor knowledge level”, scores of between 50% and 75% were categorized as “average knowledge level”, and scores >75% were combined to form the category “good knowledge level”.
- The attitude/norms of the participants toward the practice of FGM/C was assessed using questions including: “Is it a religious requirement?”, “Is it a harmful practice?”, “Does it protect girls’ honor, prevent adultery and lead to a trustworthy marriage?”, and “Do men prefer to marry a circumcised female or not?” Attitude was measured on a 5-point Likert scale as follows: strongly agree (1), mildly agree (2), neutral (3), mildly disagree (4), or strongly disagree (5), except for one statement – namely, “FGM/C is a harmful practice for girls and women”, for which the scoring was reverted. The total attitude and percentage scores for each participant were calculated. For subsequent analyses, MPS <50% were combined to form the category “negative attitude”, scores between 50% and 75% were categorized as a “neutral attitude”, and scores >75% were categorized as “positive attitude”, denoting a favorable attitude toward discontinuation of FGM/C practice.
- Personal experience and the female students’ opinions on FGM/C were assessed by first asking about their circumcision status and, based on their answer, asking subsequent questions to assess their knowledge and experience of the consequences of such practice.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) version 17 (SPSS Inc., Chicago, IL, USA) was used for the data analysis. The chi-squared test was used as a test of significance to compare categorical data. Student’s t and analysis of variance tests were used to evaluate the significance for comparisons of numerical data. Logistic regression analyses were performed to determine the significant predictors of positive attitudes and correct knowledge about FGM/C, with all possible confounders, such as sex (1= female), origin of birth (1= urban), geographical location (1= Lower Egypt), educational phase (1= clinical), and circumcision status (for female students) (1= non-circumcised), as independent variables. The choice of the variables in the model was based on the results of univariate analysis, and only the significant variables in the univariate analyses were subsequently used in the logistic regression analysis. For all statistical analyses, a P-value of <0.05 was considered significant.
Ethical considerations
Data were collected from medical students in different faculties of medicine in Egypt in their preclinical and clinical years of study using anonymous web surveys that were administered to both sexes. The surveys were distributed with an attached letter that provided further information on the study, including an explanation of rights and assurance of anonymity, wherein the students were informed that their decision regarding whether or not to participate would not affect their course grades or their relationships with the faculty members.
Students voluntarily participated in the study after being fully informed about the aim of the study and methodology, and only after providing informed consent. Additionally, students could easily withdraw from the study survey prior to its completion for whatever reason, without explanation or penalty. They were asked not to write their names on the questionnaire form so as to remain anonymous, and data were treated confidentially by the research team. The study protocol received ethical approval from the administration of Kasr El Eini School of Medicine, Cairo University, Cairo, Egypt.
Results
Personal characteristics and demographic data
The study sample consisted of 600 medical students from 19 Egyptian universities, each in a different governorate. The sample consisted of 53.3% females, 14.7% of whom had been subjected to FGM/C. Of the total study population (males and females), 75% were from an urban area and 25% were from a rural area. Geographically, 47.9% of the participants were located in Lower Egypt, and 52.1% were located in Upper Egypt. More participants living in Upper Egypt were male than were female (54% versus 46%, P<0.001) (Table 1). The study sample spanned the 6 years required for completion of medical education in Egypt; 44.8% of the participants were surveyed during their first 3 years of preclinical education, and 55.2% during their subsequent clinical years (Table 1). The majority of the responders (98.7%) were not married.
  | Table 1 Personal and sociodemographic characteristics of the study sample |
Knowledge of medical students about FGM/C
The MPS for overall knowledge about FGM/C was 53.50±29.07, indicating that the medical students had a modest level of knowledge about this practice. The MPS was significantly higher in female than in male students (59.43% versus 46.71%, t=5.42, P<0.001). Of all students surveyed, 41.2% had a poor level of knowledge and 30.5% had a good level of knowledge. Females displayed a good level of knowledge more frequently than males (χ2=22.93, degree of freedom =2, P<0.001) (Table 2).
Only one-third of the students correctly responded that FGM/C could cause difficulty with urination (33.3%) or result in complications during childbirth (37.5%). However, the majority correctly answered that FGM/C predisposes to infection (78.2%) or increases susceptibility to HIV transmission if the same medical equipment, including instruments and other materials, is used (69%). Only 49.5% of all students correctly disagreed with the statement that FGM/C is a legal practice (Table 3).
  | Table 3 FGM/C-related knowledge among medical students in Egypt |
Table 4 shows that the MPS for knowledge about the hazards of FGM/C was significantly higher in female than in male students (P<0.001), in those from Lower Egypt than from Upper Egypt (P<0.001), and in non-circumcised than in circumcised female students (P<0.001). These findings remained significant after adjusting for potential confounders (Table 5).
  | Table 5 Predictors of female genital mutilation/cutting among the female medical students |
Attitude toward FGM
The MPS for the overall attitude toward discontinuation of FGM/C was 76.29±17.93, reflecting neutrality overall. Notably, discontinuation was favored more in female than in male students (83.13% versus 68.47%, t=10.629, P<0.001). The majority of all students (58.7%) favored discontinuation of FGM/C, and there was a significant sex difference in favor of female students (75.9% versus 38.9%, χ2=111.73, degree of freedom =2, P<0.001) (Table 2).
Only two-thirds of all students agreed that FGM/C is harmful for girls and women, and many disagreed with statements that FGM/C is a religious requirement (61.0%) or a positive tradition (68.6%). The majority of students (76%) disagreed with statements that FGM/C is a prerequisite for a trustworthy marriage, and over one-half of all students (57.7%) disagreed with statements that men prefer to marry a circumcised female (Table 6).
Table 4 shows that the MPS was significantly higher (P<0.001 in all cases) in females than in males, in non-circumcised than in circumcised females, in those of urban than in those of rural origin, in those living in Lower than those living in Upper Egypt, and those enrolled in the clinical than in the educational phase. These findings remained significant after adjustment by logistic regression analysis (Table 5).
Figure 1 shows that non-circumcised female students had a significantly higher MPS for both knowledge (P=0.001) and attitude (P<0.001) than their counterparts among the circumcised students.
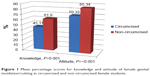  | Figure 1 Mean percentage scores for knowledge and attitude of female genital mutilation/cutting in circumcised and non-circumcised female students. |
Personal experience/opinion with circumcision status
The overall prevalence of circumcision among female students was 14.7%, and this prevalence was significantly higher among female students of rural versus non-rural origin (25% versus 10.8%, P=0.001) and those residing in Upper versus Lower Egypt (20.6% versus 8.7%, P=0.003) (Figure 2).
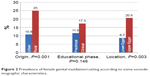  | Figure 2 Prevalence of female genital mutilation/cutting according to some sociodemographic characteristics. |
Responses from female participants regarding their experiences of circumcision revealed that 42.6% of the circumcised females had previously been teased about their circumcision status, compared to only 11.7% of their non-circumcised peers about their status (Table 7). When circumcised students were asked if they had experienced any benefits from being circumcised, around one-third (38.3%) did not think they experienced any benefit and about half (51.1%) did not know. Nearly 10% of respondents reported that they believed the circumcision had some benefits; however, information on these perceived benefits was not investigated in the present study. With regard to the effect of circumcision status on future marriage prospects, nearly half of the circumcised students (44.7%) did not think that circumcision would be advantageous. The majority (71.1%) of uncircumcised individuals did not think their circumcision status would have a negative effect. Approximately half (46.8%) of circumcised students do not plan on having their daughters circumcised, and the majority of circumcised students were unsure whether it would have been better if they had not been circumcised (46.8%). Almost 60% of the circumcised females reported that they had not been harmed from being circumcised, a figure that may reflect the negative attitude toward discontinuation of the practice, and only 25.5% reported that they experienced a certain level of harm due to their circumcision status (Table 7).
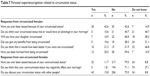  | Table 7 Personal experience/opinion related to circumcision status |
Discussion
Previous studies have demonstrated that FGM/C occurs in females across all social strata: rich and poor, undereducated and highly educated, city dwellers and countryside dwellers.25 Studies on FGM/C in the general population in Egypt have reported that almost all Egyptian women (97%) have been subjected to FGM/C.26,27 In our study, in which only medical students were included, only 14.7% of female students had been circumcised. The prevalence of FGM/C observed in the current study is comparable to that in Ghana (14%) for a similar age group,28 but is lower than that reported in Kurdistan (23%).29 However, the paucity of studies on FGM/C and its correlates and determinants in the Arab world, as well the diversity in the methodology and statistical analysis of the available studies, affect the validity of such a comparison.
Previous studies on the attitudes and practices of FGM/C have concluded that the development and implementation of legislation as a sole strategy against FGM/C is not an effective way to reduce its prevalence, and that educational interventions that emphasize the negative consequences of FGM/C are also needed to support a change in attitude.26,30,31 However, we found only a modest level of knowledge in our study group, which represents the future leaders of such educational interventions. Moreover, the students’ knowledge of some of the negative health consequences of FGM/C was poor: only one-third correctly answered that FGM/C could lead to difficulty with urination, for example.
Tolerant attitudes toward FGM/C could play a significant role in the persistence of this practice in Egypt. In our study, the overall attitude toward FGM/C was neutral (MPS 76.29±17.93), and 40% of the participants had a positive attitude toward the discontinuation of FGM/C, as compared with a previous study that found that 82% of the Egyptian women surveyed supported its continuation.32 Both studies show there was still a majority in favor of continuing FGM/C. In our study, almost half (46.8%) of circumcised female students were unwilling to have their daughters circumcised. This finding provides more optimism for a change in attitude toward FGM/C than does a recent study in pregnant females from Nigeria, in which only 24.2% said they would be unwilling to have their daughters circumcised.33
Understanding attitudes to the discontinuation of FGM/C and its predictors is imperative in understanding how to drive behavioral changes.34 In our survey, 46.8% of circumcised females were unsure whether it would have been better if they had not been circumcised. This ambivalence might reflect the findings in a study by Afifi34 in Egypt, which reported that only 12.4% of the study population intended to discontinue the practice. A recent study moreover concluded that nonsupportive attitudes of women and their husbands toward the continuation of FGM/C were associated with their decision to not subject their daughters to this practice.35 Despite some indication of changes in attitude toward discontinuation of FGM/C, those who continue to support this practice do so for reasons including preservation of group identity, perceived enhancement of femininity, supposed maintenance of female purity, maintenance of cleanliness, and assurance of a woman’s marriageability.36–38
In the present study, residency in Upper Egypt and/or rural areas was a significant predictor of favoring the continuation of FGM/C, and this finding was in agreement with the findings of other studies.32 Egypt is a traditional society, especially in Upper Egypt and rural areas: in these regions, even those who believe that FGM/C should be stopped are often forced to make their own daughters undergo the procedure, owing to pressure from their family and society. The belief that the practice of FGM/C is religiously significant has been used as justification for the continuation of FGM/C, although the highest religious authority in Egypt, Al-Azhar, has spoken against it. In our study, fewer than two-thirds of all students disagreed with the statement that FGM/C is a religious requirement. This suggests that dissemination of this ruling is not reaching people, so there is a need for education that this practice contradicts religion, and this would result in discontinuation of the practice.39
A woman’s attitude toward FGM/C is closely related to her status as a woman within her community.40 In our study, female students had significantly higher scores in favor of discontinuing FGM/C practice than did male students. This finding could be explained by the fact that men are usually excluded from women’s reproductive health education and programs, and men’s attitudes toward women’s reproductive health are therefore not informed directly by health professionals.29 In recognition of this, the WHO has made recommendations for the provision of information and services related to FGM/C that target boys, youths, and men within the home, community, and work settings.41–44 One report suggests that male involvement in reproductive health be incorporated in all major thrusts of the strategic framework, and declares that men of all ages must be educated about responsible sexual behavior.41
The results from the current study support the notion that a woman’s attitude toward FGM/C is related to her circumcision status. Uncircumcised female students had a significantly higher MPS for attitude against FGM/C than did circumcised students, even after adjusting for other confounders. Moreover, the majority of uncircumcised participants (71.1%) did not think that their uncircumcised status would negatively affect their marriage. Some parents insist that their daughters are circumcised because they fear that they otherwise may never marry,45 and only 57.7% of all students in our study disagreed that men prefer to marry a circumcised female. Notably, this figure is higher than the 29.3% reported in a previous study.33 The majority of students (76%) disagreed that FGM/C is a prerequisite for a trustworthy marriage. An Egyptian study reported that women who were circumcised had less sexual desire, fewer orgasms, and greater vaginal dryness during sex.46 Conversely, in another study, Sudanese women believed that non-circumcised women were less able to please their husbands sexually.47 This may reflect the notion that sexuality is a purely culture-related issue.
Students in the clinical phase of medical education, in the present study, had a significantly higher MPS for a positive attitude against the continuation of FGM/C. This finding could be explained by the fact that students in the clinical phase may have had greater exposure to information about the negative health consequences of this practice during their medical education than their colleagues who are in the preclinical phase of education.
The WHO is clear in its position that health professionals should not perform FGM/C in any setting.48,49 Despite the Egyptian High Court banning FGM in 1997, fewer than half (49.5%) of the students in the current study were aware that FGM/C is an illegal practice. This finding was similar to the results of a study on Nigerian antenatal patients, in which 63% supported the enactment of legislation against FGM/C.50 While countries may pass laws to ban FGM/C, legal rulings alone cannot end the practice owing to the strong and deeply rooted traditions and beliefs in the societies that conduct FGM/C.51
Study limitations
There were several limitations of this study. First, the study is subjected to selection bias, simply because the nonresponders may actually differ from the responders who completed the questionnaire online, hence the conclusion may not be representative of all members of IFMSA-Egypt. Also, there was no randomization in the selection of the participants, hence the conclusion may not be representative of medical students in Egypt. Rather, it applies to the medical students surveyed. Second, as causality and/or temporal association could not be established using the cross-sectional design, we could not be sure whether some students with certain beliefs or opinions would perpetuate the practice in their daughters. A third limitation is the possibility of recall bias or reporting bias; for example, self-reporting of FGM/C could represent a source of reporting bias. It is possible that some students had forgotten about or were unaware of undergoing FGM/C, especially considering that a traditional birth attendant performs most FGM/Cs at home when the girl is young. Finally, some girls are not aware that they have been circumcised until they get married or have been examined, and some are not willing to provide accurate information about their FGM/C status. Moreover, female participants may be unwilling to report their real FGM/C status due to the illegal situation for the practice in Egypt. Collectively, these factors could lead to misclassification bias.
Conclusion and recommendations
The findings of this study revealed that medical students in Egypt – the future leaders of programs to support the discontinuation of FGM/C in their region – have a low level of knowledge about this practice. Residency in Upper Egypt or in rural areas, where traditions are strongly respected, was a predictor of attitude to continuation of FGM/C. The involvement of religious leaders could therefore be critical to drive discontinuation of the practice of FGM/C.52 Education on FGM/C is seen as a source of empowerment for women because it can promote their abilities to gather and assimilate information.53 Our finding that male students were less likely than their female peers to support discontinuation of the practice of FGM/C supports the stance of the WHO, which has emphasized that males should be empowered through targeted reproductive health education and services. Collectively, the results of this study support and confirm that better communication and education on FGM/C, rather than passive learning alone, is needed to change attitudes in both men and women toward the discontinuation of this harmful practice. These young advocates of health should be the target group to start with, being the future leaders of these programs.
Acknowledgments
The authors would like to thank Mr Mahmoud Salam, the research coordinator at King Abdullah International Medical Research Center, King Saud Bin-Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, for his help in formatting the references. The IFMSA-Egypt Research Team includes: National Research Team Coordinator Ahmed Z Ebrahim (medical student, Alexandria Faculty of Medicine); FGM Peer Education Project Coordinators Mennat-Allah El Beheiry (MB-BCh, Kasr El Einy Faculty of Medicine, President of IFMSA-Egypt 2012–2013) and Maysoun Mohammed (MB-BCh, Mansoura Faculty of Medicine); Research Editorial Assistant Usman Suleiman (medical student, Alexandria University Faculty of Medicine); Research Data Manager Yehia Soliman (MB-BCh, Mansoura Faculty of Medicine); Research Proofreading Coordinator Pushpa Hossain (medical student, Kasr El Einy Faculty of Medicine); and Research Ethical Guidelines Coordinator Kholoud Afifi (medical student, Alexandria Faculty of Medicine).
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Eliminating Female Genital Mutilation: An Inter-agency Statement. Geneva: WHO, OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO; 2008. | ||
UNICEF. Female Genital Mutilation/Cutting: A Statistical Overview and Exploration of the Dynamics of Change. UNICEF; 2013. Available from: Wikiprogress.org. Accessed June 2, 2014. | ||
Nour NM. Female genital cutting: clinical and cultural guidelines. Obstet Gynecol Surv. 2004;59(4):272–279. | ||
Sundby J. Female genital mutilation. Lancet. 2003;362 Suppl:s26–s27. | ||
WHO study group on female genital mutilation and obstetric outcome, Banks E, Meirik O, et al. Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet. 2006;367(9525):1835–1841. | ||
Amnesty International. Female Genital Mutilation: A Human Rights Information Pack. London: Amnesty International; 1998. | ||
Almroth L, Elmusharaf S, El Hadi N et al. Primary infertility after genital mutilation in girlhood in Sudan: a case-control study. Lancet. 2005;366(9483):385–391. | ||
Aziz FA. Gynecologic and obstetric complications of female circumcision. Int J Gynaecol Obstet. 1980;17(6):560–563. | ||
Agugua NE, Egwuatu VE. Female circumcision: management of urinary complications. J Trop Pediatr. 1982;28(5):248–252. | ||
MacLeod T. Female genital mutilation. J Soc Gynaecol Can. 1995;17:333–342. | ||
Yoder PS, Khan S. Numbers of Women Circumcised in Africa: The Production of a Total. 2008. | ||
Nour N, Lalonde A, Mutilation ATFoFCFG, Obstetricians ACo, Physicians GWsHC. Female Genital Cutting: Clinical Management of Circumcised Women: American College of Obstetricians and Gynecologists. Women’s Health Care Physicians; 2007. | ||
von der Osten-Sacken T, Uwer T. Is female genital mutilation an Islamic problem? Middle East Quarterly. 2007. | ||
Dellenborg L. A reflection on the cultural meanings of female circumcision. Re-thinking Sexualities in Africa. 2004;79. | ||
El-Damanhoury I. The Jewish and Christian view on female genital mutilation. Afr J Urol. 2013;19(3):127–129. | ||
El-Zanaty F, Way A. Egypt Demographic and Health Survey 2008. Cairo: Ministry of Health, El-Zanaty and Associates, and Macro International; 2012. | ||
el Salam SA. A comprehensive approach for communication about female genital mutilation in Egypt. Male and Female Circumcision. 1999;317–330. | ||
Smolowe J. A rite of passage – or mutilation? Time. 1994 Sept 26. | ||
Michael M. Egypt officials ban female circumcision. The Associated Press. 2007 June 29. | ||
Toubia N. Female circumcision as a public health issue. N Engl J Med. 1994;331(11):712–716. | ||
World Health Organization. Female Genital Mutilation: The Prevention and the Management of the Health Complications: Policy Guidelines for Nurses and Midwives. Geneva: WHO; 2001. | ||
Toubia NA. A Practical Manual for Health Care Providers Caring for Women with Circumcision. New York:RAINBO Publication; 1999. | ||
International Federation of Medical Students’ Associations. Policy Statement on Female Genital Mutilation. Baltimore; 2013. Date of expiry 2016. | ||
Gele AA, Johansen EB, Sundby J. When female circumcision comes to the West: attitudes toward the practice among Somali immigrants in Oslo. BMC Public Health. 2012;12:697. | ||
World Health Organization. Female genital mutilation [webpage on the Internet]. Geneva: WHO [updated February 2014]. Available from: http://www.who.int/mediacentre/factsheets/fs241/en/. Accessed August 9, 2013. | ||
Yount KM. Like mother, like daughter? Female genital cutting in Minia, Egypt. J Health Soc Behav. 2002;43:336–358. | ||
El-Zanaty FH, Way AA. Egypt Interim Demographic and Health Survey, 2003. Ministry of Health and Population; 2004. | ||
Oduro A, Ansah P, Hodgson A, et al. Trends in the prevalence of female genital mutilation and its effect on delivery outcomes in the kassena-nankana district of northern Ghana. Ghana Med J. 2006;40(3):87–92. | ||
Saleem RA, Othman N, Fattah FH, Hazim L, Adnan B. Female genital mutilation in Iraqi Kurdistan: description and associated factors. Women Health. 2013;53(6):537–551. | ||
Omer-Hashi KH. Female genital mutilation: perspectives from a Somalian midwife. Birth. 1994;21(4):224–226. | ||
Barstow DG. Female genital mutilation: the penultimate gender abuse. Child Abuse Negl. 1999;23(5):501–510. | ||
Dalal K, Lawoko S, Jansson B. Women’s attitudes towards discontinuation of female genital mutilation in Egypt. J Inj Violence Res. 2010;2(1):41–45. | ||
Omolase CO, Akinsanya OO, Omotayo RS, Omolase BO. Attitudes towards female genital cutting among pregnant women in Owo, Nigeria. S Afr Fam Pract. 2012;54(4):363–366. | ||
Afifi M. Egyptian ever-married women’s attitude toward discontinuation of female genital cutting. Singapore Med J. 2010;51(1):15–20. | ||
Al-Khulaidi GA, Nakamura K, Seino K, Kizuki M. Decline of supportive attitudes among husbands toward female genital mutilation and its association to those practices in Yemen. PLoS One. 2013;8(12):e83140. | ||
Allam MF, de Irala-Estévez J, Fernández-Crehuet Navajas R, et al. Factors associated with the condoning of female genital mutilation among university students. Public Health. 2001;115(5):350–355. | ||
Almroth L, Almroth-Berggren V, Hassanein OM, et al. A community based study on the change of practice of female genital mutilation in a Sudanese village. Int J Gynaecol Obstet. 2001;74(2):179–185. | ||
Toubia NF, Sharief EH. Female genital mutilation: have we made progress? Int J Gynaecol Obstet. 2003;82(3):251–261. | ||
Yount KM. Symbolic gender politics, religious group identity, and the decline in female genital cutting in Minya, Egypt. Social Forces. 2004;82(3):1063–1090. | ||
Moore K, Randolph K, Toubia N, Kirberger E. The synergistic relationship between health and human rights: a case study using female genital mutilation. Health Hum Rights. 1997;2:137–146. | ||
Maja TM, Litt D. Men’s Involvement in Promoting Reproductive health. Women and Health Learning Package. Available from: http://www.the-networktufh org/sites/default/files/attachments/basic_pages/WHLP% 20Men. 2013;9. | ||
Al-Shawafi N. Clinical-Based Investigation of Female Genital Mutilation in Selected Areas in Yemen. Ministry of Public Health and Population; 1999:13. | ||
Rahman A, Toubia N. Female Genital Mutilation: A Practical Guide to Worldwide Laws and Policies. London: Zed Books; 2000. | ||
Wegner MN, Landry E, Wilkinson D, Tzanis J. Men as partners in reproductive health: from issues to action. Int Fam Plan Perspect. 1998;24:38–42. | ||
Nour NM. Female genital cutting: a persisting practice. Rev Obstet Gynecol. 2008;1(3):135–139. | ||
el-Defrawi MH, Lotfy G, Dandash KF, Refaat AH, Eyada M. Female genital mutilation and its psychosexual impact. J Sex Marital Ther. 2001;27(5):465–473. | ||
Gruenbaum E. Sexuality issues in the movement to abolish female genital cutting in Sudan. Med Anthropol Q. 2006;20(1):121–138. | ||
World Health Organization. Female Genital Mutilation: The Prevention and the Management of the Health Complications: Policy Guidelines for Nurses and Midwives. Geneva: WHO; 2001. | ||
UNICEF (United Nations Children’s Fund). Infant and Young Child Feeding Programme Review. Case Study: Benin. New York, NY: UNICEF; 2009. | ||
Ezenyeaku C, Okeke T, Chigbu C, Ikeako L. Survey of women’s opinions on female genital mutilation (FGM) in Southeast Nigeria: study of patients attending antenatal clinic. Ann Med Health Sci Res. 2011;1(1):15–20. | ||
Ali AS. The Role of Policymakers in Ending Female Genital Mutilation: An African Perspective. 2010. | ||
Gage AJ, Van Rossem R. Attitudes toward the discontinuation of female genital cutting among men and women in Guinea. Int J Gynaecol Obstet. 2006;92(1):92–96. | ||
UNICEF. Female Genital Mutilation/Cutting: A Statistical Exploration 2005. UNICEF; 2005. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



