Back to Journals » Risk Management and Healthcare Policy » Volume 16
Availability, Price and Affordability of Psychotropic Medicines in Addis Ababa, Ethiopia
Authors Habte F, Shifa M, Berhanu H
Received 24 February 2023
Accepted for publication 12 May 2023
Published 22 May 2023 Volume 2023:16 Pages 957—970
DOI https://doi.org/10.2147/RMHP.S409929
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Fikreselam Habte,1 Mekdes Shifa,2 Hana Berhanu2
1Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Pharmacy, Universal Medical and Business College, Addis Ababa, Ethiopia
Correspondence: Fikreselam Habte, Tel +251 913 39 40 44, Email [email protected]; [email protected]
Background: Access to affordable, quality-assured essential medicines is crucial to reduce the burden of disease. However, one third of the world’s population lacks regular access to essential medicines. The purpose of this study was to assess the availability, price, and affordability of medicines for mental disorders in Addis Ababa, Ethiopia.
Methods: A cross-sectional study was done in selected pharmacies after modification of a WHO/HAI methodology developed questionnaire. Data on the availability and price of 28 lowest priced generics and originator brand essential psychotropic medicines were collected from seven public sectors, five private sectors, and seven other sectors (five Kenema Public Community Pharmacies and two Red Cross Pharmacies) in Addis Ababa between May 9 and May 31, 2022. The data were analyzed using the developed WHO/HAI workbook part I Excel sheet. Descriptive results were reported in text and table format.
Results: The overall availability of lowest-priced generics medication was 41.69%. The availability of lowest-priced generics and originator brand medication was 54.68% and 1.7% in the public pharmacies; 24.14% and 0.0% in private pharmacies; 43% and 0.0% in Red Cross Pharmacies; and 42% and 3.2% in Kenema Public Community Pharmacies. The median price ratio in the public, private, Red Cross, and Kenema Public Community pharmacies was 1.26, 3.72, 1.65, and 1.59, respectively. Most of the medications were unaffordable. A patient could be required to pay up to 73 days wages to purchase a standard treatment for 1 month.
Conclusion: The availability of psychotropic medicines was lower than the WHO target for non-communicable diseases and most of the available medicines were unaffordable.
Keywords: access to medicine, low income country, mental disorder, Ethiopia
Introduction
“Access to health care is a fundamental human right. However, the fundamental right to health cannot be realized without fair access to necessary medicines”.1 Access to affordable, quality-assured Essential Medicines is crucial to reduce the burden of disease. However, one third of the world’s population lacks regular access to essential medicines, The situation is significantly worse in Africa and Asia’s poorest countries; where up to 50% of the population lacks such access.2
Mental disorders are associated with a significant disease burden. Mental and substance use disorders are the leading cause of years of life lost due to disability (YLDs) worldwide.3,4 The burden of mental and substance use disorders have increased between 1990 and 2019.4 Globally mental disorder is among the top ten leading cause of burden.4 In Eastern Sub-Saharan Africa, mental and behavioral illnesses account for almost 19% of all YLD. Severe depression is the second largest cause of YLD globally and in the Eastern Sub-Saharan Africa sub-region.3
In Ethiopia, mental disorder is the leading cause of burden among all non-communicable disorders.5 The prevalence of common mental disease in the general population is 21.58% and was 36.43% in those with co-morbid illness.6 The prevalence was even higher in college students (51.9%) being 2-fold higher in students chewing Khat.7 At national level, current alcohol and khat use was 40.7% and 15.8%, respectively.5 The prevalence of schizophrenia, bipolar disorder, and major depression is 0.5%, 0.6%, and 6.8%, respectively.5 In Addis Ababa, 90% of street homeless adults had mental or substance use disorder.8 Among the street adults, 41%, 60%, and 14.8% had psychosis, alcohol dependence, and suicide attempt, respectively; despite this, only 10% of psychotic patients received treatment.8 Mental illness greatly affects the patients’ overall health, economic situation, and social integration.9
Medication treatment is the primary therapeutic option for people with severe mental disorder. One of the most crucial parts of providing good mental health treatment is a regular and adequate supply of effective, safe, and affordable medication.9 Essential medications have always been in short supply for the treatment of mental diseases. In Ethiopia, most psychotropic medications are not available in primary health care units which is one of the challenges for integrating mental health care in primary health facilities.5,10 Due to a lack of adequate medications, many patients are undertreated.10,11 An interrupted supply of psychotropic medicines results in relapse of the disease, furthermore deterioration of the disease condition.12 Most serious mental illness onset is in adolescence and early adulthood, resulting in significantly increased medication consumption and expenditure.13
WHO has established a framework to assist policymakers in improving access to essential medications for universal health coverage by 2030.14 To ensure that medications are inexpensive, national policies, medicine pricing, and procurement strategies are crucial. One of the most significant barriers to access is high medicine pricing.15 To develop strategies and policies there should be adequate study into the real situation of the problems. The purpose of this study was to assess the availability, pricing, and affordability of psychotropic medicines in Addis Ababa, Ethiopia.
Materials and Methods
Study Area and Selection Procedures
In Addis Ababa there are 13 public hospitals, among them six hospitals are owned by the Federal Ministry of Health the other seven hospitals are owned by Addis Ababa City Administration.
The study was conducted at five public hospitals (Amanuel Mental Specialized Hospital (AMSH), EkaKotebe General Hospital, Zewditu Memorial Hospital, Yekatit 12 Hospital, and Menelik Referral Hospital) and five private and seven other sector pharmacies (Red Cross and Kenema public pharmacies) around those selected hospitals. The selection was based on the WHO/HAI methodology for measuring medication price, availability, and affordability.15 Based on WHO/HAI methodology, public hospital medicine outlets are used to anchor the samples, with other medicine outlets selected based on their proximity to the public hospitals.15 Two of the federal hospitals were selected conveniently since they provide psychiatric treatment services at inpatient, emergency, and outpatient departments for people with mental illness. The two hospitals also provide services for patients referred from all corners of the country. The other three hospitals were selected from Addis Ababa City administration hospitals which provide psychiatric services for many patients in the city on an outpatient basis.5 Five private pharmacies around the hospitals were selected randomly after listing all private retail pharmacies around those hospitals. Also five Kenema public community Pharmacies and two Red Cross Pharmacies near to the selected hospitals were selected conveniently for the study.
AMSH is the oldest and only mental specialized hospital in Ethiopia, established in 1937.5 The hospital is playing a pivotal role as a training institute for psychiatric professionals so as to expand psychiatry services to the primary health care system of the country. AMSH has around 268 beds for admitted patients.5
EkaKotebe General Hospital was established in 2017 as an expansion of AMSH and mental health services in the country. It is five-floor building that provides services for mental health treatment with 150 beds and general medical services with 200 beds. In addition to outpatient pharmacies there is a special community pharmacy within both mental hospitals, which are also included in the study.
In Addis Ababa, there are around 300 private retail pharmacies; 40 Kenema Public community pharmacies, and three Red Cross pharmacies.
The Ethiopian Pharmaceuticals Supply Service (EPSS) was also included in the study. EPSS is a public procurement agency for pharmaceuticals in Ethiopia.
Study Design and Period
A cross-sectional study design was used to conduct availability price and affordability of psychotropic medications.
The study was conducted from May 9 to May 31, 2022 in Addis Ababa, Ethiopia.
Study Population
All medications used for treatment of mental disorder from the Essential Medicine list of Ethiopia (EML)16 were included in the study, Additionally two medicines used in the hospitals but not in the EML were included in the study.
Sample Size Determination
Based on WHO/HAI standardized sampling methodology to assess for one region in a country, at least five public hospital outpatient pharmacy outlet and nearby medicine outlets from other type of pharmacies are selected.15 Five outpatient pharmacies in the public hospital; two special community pharmacies within the public mental hospitals; five private retail pharmacies around the selected hospitals; Five Kenema Public Community Pharmacy around the hospitals; and two Red Cross Pharmacies near to the hospitals were included in the study for a total of 19 pharmacy outlets. The two special community pharmacies within the two mental hospitals were included in the public sector. For this study, 28 psychotropic medicines (26 from the EML and two not found in the EML) were included in the study. The central EPSS was also included in the sample as a public procurement agency.
Data Collection
A standardized data collection questionnaire was developed after necessary modification of WHO/HAI methodology workbook part I for measuring medicine price, availability, and affordability.15 The data was collected by four pharmacy students after providing adequate training on the data collection. The data regarding price and availability medicines for mental disorder were collected from each selected pharmacy. Price of the medication was also collected from EPSS.
Study Variables
The availability, price, and affordability of psychotropic medicine were study variables.
Data Processing and Analysis
After data collection, data was entered and analyzed using WHO/HAI Medicine Pricing Workbook part I Excel sheet v 15.0, and the results were summarized and presented in tables.
Data Quality Management
Pre-testing was carried out at one private pharmacy to guarantee the clarity of the questionnaire and the data obtained. The supervisor at the end of each data collection date check the data collected for completeness. After data collection was completed, a random check was done by the supervisor on 20% of the outlets in order to assure the quality of the data collected. The supervisor went back to four randomly chosen pharmacies to collect the same data in order to verify the accuracy of the data gathered previously. The pharmacists entered the data twice and cross-checked it to prevent errors (double entry). The workbook’s data-checker feature was utilized to highlight data that should be validated.
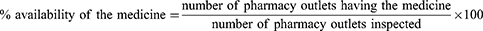
Availability
The availability of survey medicines was assessed by inspecting the lowest priced generic (LPG) and originator brand (OB) medicine in the pharmacy outlet. Medicine availability was calculated as percent availability of individual and mean percent (%) availability across a group of medicines. It was calculated as outlets with the medication divided by the number of the outlets included in the sector. Percent availability was calculated as:
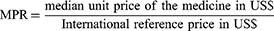
Price
In Ethiopia most patients acquire medicine by purchasing out of pocket. There are a few patients who have a letter stating they cannot afford the medicines, and for such patients’ medicines are free.
The price of the medicine was obtained from the price list in the pharmacy outlet. Pharmacies in private mostly write the local price on the medicine package. The local price was changed to US dollars using the exchange rate on the first day of the data collection. On the first day of data collection 1US$=51.52 ETB. Median price ratio (MPR) of the medicine was calculated as the median price of the medicine in each sector divided by the International reference price of the medicine. Median Price Ratio was calculated as:
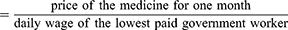
Affordability
Affordability was calculated as the number of working days necessary for the lowest-paid unskilled government employee to purchase the specific medication for a 1 month course of therapy. The daily wage of the lowest paid government worker of Ethiopia was about 32.4 birr.17 Affordability was calculated as:
Ethics Approval and Consent to Participate
The study protocol was reviewed and approved by the Institutional Research Review Committee of Universal Medical and Business College with reference number [IRRC/UMBC/454/14/2022]. The owners of drug outlets were informed about the aims of the study prior to participation, and verbal consent was obtained from each drug outlet owner after explaining his/her right not to participate in the study. Confidentiality of the outlet was kept.
Operational Definition
- Affordability: calculated as price of the medication for a month period divided by the lowest paid government worker wage. If the result is less than 1 it is affordable, if greater than 1 it is unaffordable.10
- Other sector 1: in this study was Red Cross Pharmacies.
- Other sector 2: in this study was Kenema Public Community Pharmacies.
Results
Availability of Psychotropic Medication
The overall availability of LPG in all sectors was found to be 41.69%. The availability of LPGs and OBs was 54.68% and 1.7% in the public sector; 42.07% and 3.2% in other sector 2, respectively. There were no OBs in private and other sector 1 pharmacies. LPGs availability was 24.14% and 43% in private and other sector 1 pharmacies, respectively (Table 1).
 |
Table 1 Overall Percentage Availability of LPG Psychotropic Medicines at Public, Private, and Other Sector in Addis Ababa, Ethiopia, 2022 |
The overall availability of WHO LPG psychotropic medicines was 55.42% (Table 1). It was 63.63% in the public sector; 38.18% in the private sector; and 64% and 56.36% in other sectors 1 and 2, respectively.
Among antidepressants, Amitriptyline 25 mg was the most available (86.4%) and sertraline 50 mg was the least available (10.7%). Sodium Valproate 200 mg was the most available (95%) and Lithium carbonate 300 mg was the least available (7.1%) tablet in the category of mood stabilizer. Among antipsychotics, Risperidone 2 mg tablet was the most available (96.4%) and Trifluoperazine 1 mg tablet was the least available (12.1%). Among anxiolytic, Diazepam 5 mg tab had availability of 66.4% and Clonazepam was not available in any strength. Also Trifluoperazine 5 mg and Fluphenazinedecanoate 25 mg/mL injection were not available in any outlet (Table 1).
There are two long acting injectable antipsychotics registered and used in Ethiopia, Fluphenazine decanoate 25 mg/mL and Haloperidol decanoate 50 mg/mL, but only Haloperidol decanoate was available in 3.5% of the outlets. Clozapine was available in only one Kenema public community pharmacy (Table 1).
There was no medication available for the treatment of substance use dependence or for attention deficit disorder, even though there are medicines listed in the Essential drug list of Ethiopia for those disorders. In Ethiopia, Benzodiazepines are commonly used in alcohol abuse withdrawal symptom treatment.
The overall availability of clozapine, clomipramine, Diazepam, Haloperidol, Lamotrigine, Lithium carbonate, Trifluoperazine, and Sertraline was very low in all sectors (Table 1).
Availability of OBs products in all sectors was low. Haloperidol 1.5 mg was the only OB medicine available in the public sector (71.4%).
Psychotropic Medication’s Prices
Public Sector Patient Prices
The median MPR for LPG in the public sector was 1.26, and the minimum and maximum MPR was 0.16 and 11.7, respectively. Also the 25th and 75th quartile was 0.51 and 1.3, respectively. The interquartile range was narrower, indicating there was less variation in the MPR (Table 2).
 |
Table 2 Median Price Ratio of Psychotropic Medicines in Public, Private, and Other Sector in Addis Ababa, Ethiopia, 2022 |
Private Sector Patient Prices
The median MPR for LPG medicine in the private sector was 3.72, and the minimum and maximum MPR was 1.22 and 81.07, respectively. The 25th and 75th percent quartile was 1.96 and 8.41, respectively. The range was very wide; there was one extreme value (Diazepam 5 mg/mL injection) (Table 2).
Other Sector 1 (Red Cross Pharmacy Patient Prices)
The median MPR for LPG medicine in the private sector was 1.65 and the minimum and maximum MPR were 0.19 and 5.04, respectively. The 25th and 75th percent quartiles were 0.92 and 2.9, respectively. The interquartile range was narrow relative to the range, which indicates there were no extreme values (Table 2).
Other Sector 2 (Kenema Public Community Pharmacy Patient Prices)
The median MPR for LPG medicine in the private sector was 1.59, and the minimum and maximum MPR were 0.63 and 6.3, respectively. The 25th and 75th percent quartiles were 0.82 and 1.93, respectively. The interquartile range was narrow, indicating there were no extremely different prices in the range (Table 2).
Affordability of Standard Treatment Regimens
All the available medications surveyed were unaffordable, except for Diazepam 5 mg tablets in all sectors (Table 3). A patient with major depression disorder treated with Amitriptyline 25 mg tablets requires 1.6 days wage in the public sector and other sector 2 (Kenema Public Community Pharmacy); 10.4 and 2.1 days wage in the private and other sector 1 (Red Cross Pharmacy), respectively. Treatment of bipolar disorder and epilepsy with Sodium valproate 200 mg tablet required more than 2 months wage to purchase 1 month of medicine.
 |
Table 3 Number of Days’ of Wages of the Lowest-Paid Government Worker Needed to Purchase Standard Treatments in Addis Ababa, Ethiopia, 2022 |
Except Diazepam 5 mg tablets, all the medicines which achieved a WHO target of 80% availability were unaffordable in any sector. The number of days’ wage needed to purchase medicine used for a month was higher in the private sector. Medicine cost in the public sector was mostly less than all other sectors (Table 3).
Discussion
Psychotropic medicines are the cornerstone of treatment for severe mental disorder. If patients with serious mental illness abruptly discontinue medication treatment because of access, it may result in: relapse of the disease; decreased response and resistance in subsequent treatment; deterioration of the patient condition; increased treatment cost; and finally may result in early death.18,19
The results of the current study showed that the overall availability of LPG medicine for mental illness was 41.69%. Overall, the availability of psychotropic medicines falls short of the WHO’s target of 80% availability of the necessary medicines to treat non-communicable disease.20 According to WHO, essential medicines are the minimum medicines needed for basic health systems to function and the medicines should be available at all times.21 The study was conducted in the capital city where many of the psychiatry health facilities in the country are situated and also many patients from regions are commonly referred to those studied hospitals for better management,5 however most of the drug outlets do not have most of the essential medications needed. This study was also similar with the systematic review noting the availability of essential psychotropic medicines in many low- and middle-income countries is less than 50%.22 There are many reasons for the unavailability of the medicines: the current civil war in Ethiopia stopped the production of one of the largest pharmaceutical manufacturing company (Addis Pharmaceuticals manufacturing); higher inflation rate; inadequate foreign currency for importation of medications; inadequate information on the real prevalence of the disease; number of patients attending health facilities, and associated poor quantification of medication needed; poorly organized supply chain management system may be some of the reason for unavailability of the essential psychotropic medicines. Despite this, the overall availability of psychotropic medicines was higher than Gambia findings (30%)23 and Mozambique.24
The overall availability of LPG psychotropic medicines in the WHO essential list was 55.42%, which was higher than the average availability in the WHO six regions of the world.22
The availability of psychotropic medicines at public sector outlets of the LPGs and OBs was 54.68% and 1.7%, respectively. Similarly, the availability in private sector outlets of LPGs and OBs was 24.14% and 0.0%, respectively, while availability in other sectors was 42% and 3.2% for Kenema Public Pharmacies; 43% and 0.0% for Red Cross Pharmacies for LPGs and OBs, respectively. The results showed that psychotropic medicines were more available in the public sector. Also Kenema public pharmacy had more availability than the private sector. Availability of LPG psychotropic medications in the public sector was higher than the average available in low income (44.1%), lower-middle income (34.3%), and upper middle income (46.7%) countries.20 The result was also higher than other recent global studies which indicate that the availability of LPG is less than 50% in the public sector.22 The availability in the public sector was also better than other countries in the public sector for LPG medicines.23,24 Unlike this study other studies indicated that there was better availability in the private sector than in the public sector.2,20,22,23 The reason for better availability in the public sector in this study may be, in Ethiopia most LPG medicines are supplied by a government procurement agency. The agency distributes the medication primarily to public health facilities. The private sector are not as such involved in the supply of psychotropic medications, this could be because private companies do not have adequate data on the real need of those medications. There is no clear source of information, especially for private suppliers, on the actual amount of the medicines needed in the country. If a private company feels the medication is not used by many patients they prefer not to supply such medications. Inadequate availability of foreign currencies for private suppliers could be the other main reason for the low availability in the private sector. Unlike the private sector, other sectors are allowed to purchase medicines from government procurement agencies, leading to better availability in other sectors. The findings of the current study also indicate that generic versions of the drugs are more available than originator brands.
The availability of OB psychotropic medicine was very low. Similarly to this study, most low income countries and WHO regions of Africa and Europe do not have OB medicines in the public sector.20,22 The availability of OB medicine is better in the private sector than in the public sector in most countries.20,22 Private suppliers in Ethiopia are not involved in the supply of psychotropic medicines and the government supply agency provides primarily LPG medicines, which may be the reason for the lower availability of OB medicines in Ethiopia.
Among LPG antidepressants, antipsychotics, mood stabilizers, and anxiolytics studied, at least one medication in each group had high availability [>80%], reaching the WHO target for NCD medicines.20 Amitriptyline 25 mg, risperidone 2 mg, risperidone 4 mg, sodium valproate 200 mg, and carbamazepine 200 mg had overall availability of 86.4%, 96.4%, 90%, 95%, and 82.8%, respectively. This was higher than the average availability of all WHO regions of the world22 and also higher than the average availability in each different income level categorized countries,22 and in Gambia,23 and Mozambique.24 The problem arises when there is a need to switch medication in each group, since the availability of the second chosen medicine was mostly very low. The availability of Amitriptyline 25 mg tablet and Diazepam 5 mg tablet was higher than seven low and lower-middle income countries,25 and also other countries like Gambia23 and China.26–28
The overall availability of LPG fluoxetine 20 mg capsules was 53.2%, with 42.9% in the public sector and 80% in the private sector. This was higher than the availability in most countries.22 Even though the overall and public sector availability is lower than the WHO target for NCD, it was higher than the average availability in the six regions of WHO and also higher than the average in all levels of income based categorized countries.22 This may be because fluoxetine is produced in Ethiopia and is most commonly used as a selective serotonine reuptake inhibitor in Ethiopia.
Lithium carbonate is considered as the medicine of choice in the long-term maintenance phase of bipolar disorder; also it is among WHO EML for mood disorder,21 but the drug was available only in 7.1% of the outlets in this study. The safety issue and associated need for monitoring lithium level in the blood may lead physicians to defer lithium for treatment of bipolar disorder in Ethiopia. But still there are cases in which lithium carbonate is the most effective treatment than all other mood stabilizers. Availability should consider patients which has a good response to lithium. The availability of lithium was also lower than the availability in Iran (50% in public sector and 90% in private sector).29 Lithium was not available in Mozambique and Gambia surveys.23,24
In Ethiopia up to half of the psychotic patients are non-adherent to their medication.19 Fluphenazine decanoate 25 mg/mL injection is commonly used for patients who are non-adherent to oral medication, but it was not available in any outlet. Fluphenazine decanoate 25 mg/mL injection is also among the few WHO EML for schizophrenia treatment.15 There is no registered second generation long-acting antipsychotic in Ethiopia. So patients may be left without an option when treatment change is required. The availability of LPG fluphenazine decanoate injection was 35.3% in low income countries22 and 16.7% in Mozambique.24
In the natural history of the disease one third of the patients with schizophrenia are treatment resistant. Clozapine is the drug of choice for management of treatment resistant schizophrenia, however this medication was not available in any of the public sectors. Patients who had good progress with Clozapine may relapse the full blown disease symptom when the medication is supplied interruptedly. Clozapine is among the essential drug list both in WHO and Ethiopian EML.30 However, only a quarter of countries in low and lower middle income had clozapine in the national medicine list.22 It is difficult to imagine how treatment resistant cases are treated in those countries without clozapine. Iran had better availability of clozapine.29
In Ethiopia there are only four hospitals providing treatment for substance use related problems. In Addis Ababa AMSH and Zewditu hospitals, which are included in this study, provide most treatment and rehabilitation for substance use disorders in the country. In both hospitals there was no medication for the treatment of common substance abuse in the country (Alcohol, cigarette, khat, Opioids) like disulfiram, acamprosate, naltrexone, nicotine replacement therapy, bupropion, varenicline, or methadone. Until now those medications are not available in Ethiopia, even though the medications are included in the national essential list.
There are many patients with attention deficit and hyperactive disorders but there was no medication for treatment of such disorder until now in Ethiopia. Also those medications are available in Gambia.31 In Ethiopia there are only two hospitals providing child psychiatry,5 and the limited expansion of the service, and inadequate information about the prevalence of those diseases and the required medication could be the reason for the unavailability of those medications.
Similarly to low income countries like Ethiopia, psychotropic medicines were also least available in lower-middle and upper-middle income countries.20 The lower availability psychotropic medications in Ethiopia may be a result of different factors, including: less prioritization given to those mental disorders; insufficient health financing; inadequate skilled manpower; poor information generation and use on the disease and medicines; poor drug supply management; stigma from the disease; and poor patients treatment seeking.5
Addis Ababa is the capital city of Ethiopia, where many of the mental health facilities and specialized health service are provided.5 Also many patients are sent to Addis Ababa for better management from all corners of the country. If at least essential psychotropic medicines are not adequately available, the patients may not have other options to access the medication anywhere in the country. In Ethiopia many patients have poor treatment-seeking behavior;32 poor medicine availability may increase the poor treatment-seeking behavior of patients. Mental health services are mostly accessible in urban areas in Ethiopia5 and also other LMIC.33 For many patients, AMSH is the first and last resort for accessing psychotropic medicines in the country.
In this study the median price of psychotropic medication in the private sector was three times higher than in the public sector. This is also the case at global level, the price of medicine in the private sector is almost always higher than the public sector.22 Median MPR in the other sector was similar with the public sector.
When medications are not available in public hospitals, patients commonly purchase the medication from the nearby private pharmacy; Diazepam 5 mg/mL injection is commonly used in the emergency department but the availability was low (42.9%) and MPR was 11.2 and 81.07 in the public and private sector, respectively. When diazepam injection was not available in the public sector, the patient may be forced to pay more than 7-times (81.07 divided by 11.2) more in the private sector. Amitriptyline is a commonly prescribed antidepressant, with a MPR of 2.13 and 8.41 in the public and private sectors, respectively. When Amitriptyline was not available in public hospital, the patient is required to pay more than 4-times more in the private sector. Some of the reasons for the variation between public and private sectors could be: Ethiopia has a policy on margin of price for medication, especially for public sectors, but this is not adequately implemented especially in the private sector;34 running costs for private pharmacies are higher than in public and other sectors. For example, a private sector has to rent the pharmacy house at a higher price but mostly public pharmacies uses the hospital building without rent; private sector pharmacies are primarily established for profit generation but public and other sector pharmacies are established to serve the population with a lower profit margin.
The MPR of LPG amitriptyline, fluoxetine, and diazepam tablets in both public and private sectors was lower than the average MPR in global and all income level categorized countries,22 however it was higher than the average Eastern Mediterranean and South East Asian WHO regions MPR.22 The MPR was also higher than studies conducted in China,28 Rwanda,35 and Indonesia.36 This could be because there are different companies which produce generic products in those regions. Ethiopia import 85% of the medications needed in the country. Most of the medications are imported from China and South East Asia countries like India. Cost for logistics are added to the Ethiopian price relative to those countries.
The study also assessed the affordability of psychotropic medications in public, private, and other sectors (Kenema and Red Cross Pharmacies) in Addis Ababa, Ethiopia. Affordability was measured by the number of days’ wages the lowest-paid unskilled government employee needs to purchase a 1 month course of treatment with a standard dose of the medicine. To say a medication is not affordable, the medication is more than 1 days’ wage. Unlike most other studies, psychotropic medications assessed in this study were unaffordable.28,29,35,37–39 Diazepam tablets was the only affordable medication in all sectors. Sodium valproate 200 mg tablets are commonly used as mood stabilizers and anticonvulsants, being the most available medication, however a patient required more than 2 months wage to purchase 1 month of medicine. Except for a few medications the unaffordability was much higher in the private sector than in public and other sectors. The unaffordability was increased even more when a combination of medication was used for a specific disease, which is commonly seen in psychiatric treatment services.40 This is also the case in many countries, where purchasing psychotropic medicines in lower-middle income countries require at least 1.4 days’ wages,20 however other LPG medications for non-communicable disease do not require more than 1 days’ wage in each therapeutic group.20 This indicates psychotropic medicines were more unaffordable than other groups of medications. The unaffordability in this study was much higher than in another study.20 This may be because of the higher inflation rate seen recently in Ethiopia, without increasing the wage of employees. Recently after the emergence of the COVID-19 pandemic and civil war in Ethiopia the price of many pharmaceuticals have increased at an alarming rate. However, according to WHO essential list those medications should be available at a price that the community and individuals are able to afford.21 Income level of house hold is mostly determinant for catastrophic health expenditure (CHE).41 CHE is higher in LMIC than high income countries.41 In Ethiopia the daily income of the lowest paid government worker is less than one US dollar and most patients access health services through out of pocket expenditure, so many patients are exposed to CHE. Recently youth’s unemployed rate is high, in addition to lower daily wages; this high unemployment rate may result in an increased rate of CHE. In LMIC common mental illnesses are associated with poverty, poverty is also a risk factor for mental disorders.5,42 CHE from severe mental illness is much higher than from other infectious diseases.41 In Ethiopia there are many different barriers that hinder patients from using mental health services, these include socioeconomic issues, cultural factors, negative attitude to mental illness, fear, and unfamiliarity with the service.43 Socioeconomic factors may affect the other aspects. Many patients using those medications have higher disability and difficulty of involvement in income generation activities,44 which might increase the economic burden of the patient and the families caring for those patients. In Ethiopia patients with mental illness had decreased health seeking behavior.32 Unaffordability and out of pocket payment for health services may be reasons for abandoning health services from the patients and care giver side.45,46 One study also showed increased coverage of mental health services, reimbursement of direct and indirect cost of treatment was one mechanism to increase patients seeking treatment and to increase mental health service coverage in primary health care unit in Ethiopia.45,46 In Ethiopia severe mental illness results in catastrophic out of pocket expenditure and consequent poverty.47,48 Severe mental illness also leads to severe food insecurity in families.5 Health insurance should be a decisive priority. Public health insurance system is also a promising program for universal health coverage in Ethiopia and sub-Saharan Africa.49 Publicly financed treatment of mental disorder had the advantage of increasing patient productivity, progressive health benefit, and could help to resolve concerns related with equity in accessing mental health services.50 Accessing mental health services and medication at a lower level primary health care unit in LMIC has the benefit of decreasing indirect and direct economic burden on the patients.51 Unavailability and unaffordability of psychotropic medicines were the biggest challenge in psychiatric disease treatment in other low income countries also.23
In Ethiopia the PRogramme for Improving Mental healthcarE [PRIME] project supporting delivery of mental healthcare integrated into primary care helps to improve the availability, accessibility, and affordability of treatment.46 By availing mental health services in a primary health care unit, indirect costs associated with treatment of mental illness definitely decrease, and its role for decreasing direct costs like purchasing of the medicines may be minimal. Such a program should also work on improving accessibility and affordability of medicines for mental illness. The WHO slogan “No health without mental health” also shows the decisive importance of adequate access to the necessary psychotropic medicine for treatment of mental illness.
A limitation in this study was it was difficult to get full data from the Public procurement agency, so it was excluded from the analysis.
Conclusion
The availability of most psychotropic medicine was low in all sectors in comparison to the WHO target. Public pharmacies had relatively better availability for LPG than Private sector pharmacies. The patient price of psychotropic medicines was not as such different from international reference price, however when the income of a patient is considered, most of the medications were unaffordable.
Abbreviations
DALYs, disability-adjusted life-years; Cap, Capsule; EML, Essential Medicine List; ETB, Ethiopian birr; HAI, Health action international; LMICs, low- and middle-income countries; LPGs, lowest-priced generics; MPR, Median price rationale; MSH, Management Science for Health; NGOs, non-governmental organization; OB, Originator brands; Tab, Tablet; USD, United States dollars; WHO, World Health Organization; WHO/HAI, World Health Organization/Health Action International.
Supporting Document
All data are found in the manuscript, if additional is needed it can be accessed from the corresponding author on request.
Acknowledgments
We would like to thank data collection site professionals, Addis Ababa University and Universal Medical and Business College for giving us this opportunity to undertake this study.
Funding
The author received no funding for this study.
Disclosure
The authors report no conflict of interest in this work.
References
1. McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Aff. 2017;36(5):808–818. doi:10.1377/hlthaff.2016.1650
2. Sisay M, Amare F, Hagos B, Edessa D. Availability, pricing and affordability of essential medicines in Eastern Ethiopia: a comprehensive analysis using WHO/HAI methodology. J Pharma Policy Pract. 2021;14(1):1–20. doi:10.1186/s40545-021-00339-2
3. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi:10.1016/S0140-6736(13)61611-6
4. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–150. doi:10.1016/S2215-0366(21)00395-3
5. Minister of Health. National Mental Health Strategy 2020–2025 (2013–2017 EFY). Addis Ababa, Ethiopia: Minister of Health; 2020.
6. Kassa GM, Abajobir AA. Prevalence of common mental illnesses in Ethiopia: a systematic review and meta-analysis. Neurol Psychiatry Brain Res. 2018;30:74–85. doi:10.1016/j.npbr.2018.06.001
7. Mekuriaw B, Zegeye A, Molla A, Hussen R, Yimer S, Belayneh Z. Prevalence of common mental disorder and its association with khat chewing among Ethiopian college students: a systematic review and meta-analysis. Psychiatry J. 2020;2020:1–8. doi:10.1155/2020/1462141
8. Fekadu A, Hanlon C, Gebre-Eyesus E, et al. Burden of mental disorders and unmet needs among street homeless people in Addis Ababa, Ethiopia. BMC Med. 2014;12(1):1–2. doi:10.1186/s12916-014-0138-x
9. Haak H. Improving Access and Use of Psychotropic Medicines. World Health Organization; 2005.
10. Hanlon C, Luitel NP, Kathree T, et al. Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five low-and middle-income countries. PLoS One. 2014;9(2):e88437. doi:10.1371/journal.pone.0088437
11. Iseselo MK, Ambikile JS. Medication challenges for patients with severe mental illness: experience and views of patients, caregivers and mental health care workers in Dar es Salaam, Tanzania. Int J Ment Health Syst. 2017;11(1):1–2. doi:10.1186/s13033-017-0126-6
12. Alene M, Wiese MD, Angamo MT, Bajorek BV, Yesuf EA, Wabe NT. Adherence to medication for the treatment of psychosis: rates and risk factors in an Ethiopian population. BMC Clin Pharmacol. 2012;12(1):1–9. doi:10.1186/1472-6904-12-10
13. Kebede D, Alem A, Shibre T, et al. Onset and clinical course of schizophrenia in Butajira-Ethiopia. Soc Psychiatry Psychiatr Epidemiol. 2003;38(11):625–631. doi:10.1007/s00127-003-0678-4
14. World Health Organization. Towards Access 2030: WHO Essential Medicines and Health Products Strategic Framework 2016–2030. World Health Organization; 2017.
15. World Health Organization. Measuring Medicine Prices, Availability, Affordability and Price Components. World Health Organization; 2008.
16. Minister of health/Ethiopian Food and Drug Authority. Ethiopian Essential Medicines List.
17. Ministers of Council. Federal civil servants position rating, grading and salary scale council of ministers regulation number 455/2019. Federal Negarit Gazette. 2019;11862:11863.
18. Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013;13(1):1–8. doi:10.1186/1471-244X-13-50
19. Wei Shan G, Makmor-Bakry M, Salihah Omar M. Long term use of lithium and factors associated with treatment response among patients with bipolar disorder. PsychiatriaDanubina. 2016;28(2):146–153.
20. Ewen M, Zweekhorst M, Regeer B, Laing R. Baseline assessment of WHO’s target for both availability and affordability of essential medicines to treat non-communicable diseases. PLoS One. 2017;12(2):e0171284. doi:10.1371/journal.pone.0171284
21. World Health Organization. Improving Access to and Appropriate Use of Medicines for Mental Disorders. World Health Organization; 2017.
22. Todesco B, Ostuzzi G, Barbui C. Mapping the selection, availability, price and affordability of essential medicines for mental health conditions at a global level. Epidemiol Psychiatr Sci. 2022;31. doi:10.1017/S2045796022000087
23. Samba D. Availability of Psychotropic Medications in Primary Health Care Facilities in the Gambia (Doctoral dissertation); 2017.
24. Wagenaar BH, Stergachis A, Rao D, et al. The availability of essential medicines for mental healthcare in Sofala, Mozambique. Glob Health Action. 2015;8(1):27942. doi:10.3402/gha.v8.27942
25. Rahman MA, Babaye Y, Bhat A, Collins PY, Kemp CG. Availability of two essential medicines for mental health in Bangladesh, the Democratic Republic of Congo, Haiti, Nepal, Malawi, Senegal, and Tanzania: evidence from nationally representative samples of 7958 health facilities. J Glob Health. 2022;12. doi:10.7189/jogh.12.04063
26. Wang X, He X, Ren Y, et al. Evaluating the price, availability, and affordability of essential medicines in primary healthcare institutions: a mixed longitudinal and cross-sectional study in Jiangsu, China. Front Public Health. 2022;10:245.
27. Xi X, Li W, Li J, et al. A survey of the availability, prices and affordability of essential medicines in Jiangsu Province, China. BMC Health Serv Res. 2015;15(1):1–7. doi:10.1186/s12913-015-1008-8
28. Xu R, Li S, Lv X, Xie X. Prices, availability, and affordability of national essential medicines in public primary hospitals: a cross‐sectional survey in poverty‐stricken rural areas in China. Int J Health Plann Manage. 2020;35(2):545–557. doi:10.1002/hpm.2963
29. Karam R. Prices, availability, affordability and price components of medicines to treat non-communicable diseases in Iran Report of a survey undertaken in 2014 by the Ministry of Health. 2015.
30. World Health Organization. World Health Organization Model List of Essential Medicines: 22nd List (2021). World Health Organization; 2021.
31. Thome J, Marenah E, Moraru D, Höppner J, Nyan O. Availability of psychiatric medication in an urban area of The Gambia/West Africa. World J Biolog Psychiatry. 2011;12(sup1):114–117. doi:10.3109/15622975.2011.601925
32. Teshager S, Kerebih H, Hailesilassie H, Abera M. Pathways to psychiatric care and factors associated with delayed help-seeking among patients with mental illness in Northern Ethiopia: a cross-sectional study. BMJ open. 2020;10(7):e033928. doi:10.1136/bmjopen-2019-033928
33. Rathod S, Pinninti N, Irfan M, et al. Mental health service provision in low-and middle-income countries. Health Services Insights. 2017;10:1178632917694350. doi:10.1177/1178632917694350
34. World Health Organization. Assessment of the Pharmaceutical Sector in Ethiopia. Addis Ababa, Ethiopia: Ministry of Health; 2017.
35. Bizimana T, Kayumba PC, Heide L. Prices, availability and affordability of medicines in Rwanda. PLoS One. 2020;15(8):e0236411. doi:10.1371/journal.pone.0236411
36. Kristina SA, Aditama HA, Endarti D, Widayanti AW. Evaluating accessibility of essential medicines in Indonesia: a survey on availability and prices in public and private health sectors. Int J Pharm Res. 2020;12(2):692–699.
37. Alefan Q, Amairi R, Tawalbeh S. Availability, prices and affordability of selected essential medicines in Jordan: a national survey. BMC Health Serv Res. 2018;18(1):1–2. doi:10.1186/s12913-018-3593-9
38. Saeed A, Saeed H, Saleem Z, Fang Y, Babar ZU. Evaluation of prices, availability and affordability of essential medicines in Lahore Division, Pakistan: a cross-sectional survey using WHO/HAI methodology. PLoS One. 2019;14(4):e0216122. doi:10.1371/journal.pone.0216122
39. Kasonde L, Tordrup D, Naheed A, Zeng W, Ahmed S, Babar ZU. Evaluating medicine prices, availability and affordability in Bangladesh using World Health Organisation and Health Action International methodology. BMC Health Serv Res. 2019;19(1):1–2. doi:10.1186/s12913-019-4221-z
40. Tesfaye S, Debencho N, Kisi T, Tareke M. Prevalence of antipsychotic polypharmacy and associated factors among outpatients with schizophrenia attending Amanuel mental specialized hospital, Addis Ababa, Ethiopia. Psychiatry J. 2016;2016. doi:10.1155/2016/6191074
41. Mouhoumed HM, Mollahaliloğlu S. Catastrophic health expenditures on accessing different healthcare services in Ethiopia and Kenya. Med Res Rep. 2020;3(2):39–44.
42. Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. 2010;71(3):517–528. doi:10.1016/j.socscimed.2010.04.027
43. Hughes TL, Quinn C, Tiberi A, Zeleke WA. Developing a framework to increase access to mental health services for children with special needs in Ethiopia. Front Sociol. 2020;5:583931. doi:10.3389/fsoc.2020.583931
44. Hailemichael Y, Hanlon C, Tirfessa K, et al. Mental health problems and socioeconomic disadvantage: a controlled household study in rural Ethiopia. Int J Equity Health. 2019;18(1):1–2. doi:10.1186/s12939-019-1020-4
45. Hailemariam M, Fekadu A, Medhin G, Prince M, Hanlon C. Equitable access to mental healthcare integrated in primary care for people with severe mental disorders in rural Ethiopia: a community-based cross-sectional study. Int J Ment Health Syst. 2019;13(1):1. doi:10.1186/s13033-019-0332-5
46. Hailemariam M, Fekadu A, Selamu M, Medhin G, Prince M, Hanlon C. Equitable access to integrated primary mental healthcare for people with severe mental disorders in Ethiopia: a formative study. Int J Equity Health. 2016;15(1):1. doi:10.1186/s12939-016-0410-0
47. Hailemichael Y, Hailemariam D, Tirfessa K, et al. Catastrophic out-of-pocket payments for households of people with severe mental disorder: a comparative study in rural Ethiopia. Int J Ment Health Syst. 2019;13(1):1–3. doi:10.1186/s13033-019-0294-7
48. Hailemichael Y, Hanlon C, Tirfessa K, et al. Catastrophic health expenditure and impoverishment in households of persons with depression: a cross-sectional, comparative study in rural Ethiopia. BMC Public Health. 2019;19(1):1–3. doi:10.1186/s12889-019-7239-6
49. Hanlon C, Alem A, Lund C, et al. Moving towards universal health coverage for mental disorders in Ethiopia. Int J Ment Health Syst. 2019;13(1):1–6. doi:10.1186/s13033-019-0268-9
50. Johansson KA, Strand KB, Fekadu A, Chisholm D. Health gains and financial protection provided by the Ethiopian mental health strategy: an extended cost-effectiveness analysis. Health Policy Plan. 2017;32(3):376–383. doi:10.1093/heapol/czw134
51. Khan MM, Khan MM. Economic burden of mental illnesses in Pakistan. J Ment Health Policy Econ. 2016;19(3):155.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.