Back to Journals » Journal of Multidisciplinary Healthcare » Volume 9
Australians with osteoarthritis: satisfaction with health care providers and the perceived helpfulness of treatments and information sources
Authors Basedow M, Hibbert P, Hooper T, Runciman W, Esterman A
Received 17 April 2016
Accepted for publication 1 June 2016
Published 22 August 2016 Volume 2016:9 Pages 387—394
DOI https://doi.org/10.2147/JMDH.S110751
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Martin Basedow,1 Peter Hibbert,1 Tamara Hooper,1 William Runciman,1 Adrian Esterman,2
1School of Psychology, Social Work and Social Policy, 2School of Nursing and Midwifery, University of South Australia, Adelaide, SA, Australia
Objective: The aim of this study was to evaluate the satisfaction of Australian patients who suffer from osteoarthritis (OA) with their health care providers and the perceived helpfulness of treatments and information sources.
Methods: A self-administered questionnaire was conducted with a sample of 560 Australian patients who suffer from OA with questions about satisfaction with health care providers and the helpfulness of different treatment options and information sources. Logistic regression models were used to assess potential predictors of satisfaction. Thematic analysis was undertaken for attitudinal factors associated with satisfaction.
Results: A total of 435 participants returned questionnaires (response rate 78%). Most respondents were highly satisfied with the care provided by their general practitioner (GP) (84%), communication with their GP (88%), time spent with their GP (84%), and their ability to talk freely with their GP about their medical problem (93%), but less satisfied with their ability to talk freely about associated emotional problems (77%). Satisfaction with pharmacists (80%), rheumatologists (76%), and orthopedic surgeons (72%) was high. Joint replacement surgery (91%), prescription anti-inflammatory medications (66%), aids and assistive devices (65%), intra-articular injections (63%), and prescription painkiller medications (62%) were perceived as effective treatments. Less highly rated treatments were exercise (48%), physiotherapy (43%), and complementary medicines (29%). A majority of patients were satisfied with the information to manage their OA (65%). From the multivariable logistic regression analysis, four GP satisfaction factors were found to be predictors of overall satisfaction with GP care: the amount of time that the GP spends with the patient (P=0.005), the information the GP provides about what to expect (P<0.001), the communication between patient and GP (P=0.001), and the information that the GP provides about medications (P=0.042).
Conclusion: The study showed that although patients with OA were generally satisfied with their health care providers, there was notable variation in the perceived helpfulness of therapeutic options. The importance to patients of having access to good quality information about their condition was emphasized.
Keywords: multidisciplinary care, beliefs, attitudes, patient preference
Introduction
Health care that is responsive to individual patient preferences, needs, and values is now the dominant paradigm in health service delivery.1 Within this framework, patient satisfaction has emerged as a key indicator of the quality of health care. Donabedian regards patient satisfaction as a “patient’s judgement on the quality of care in all its aspects, but particularly as concerns the interpersonal process”.2 Satisfied patients are more likely to benefit from their health care and have improved quality of life.3 Satisfaction with care has particular relevance to chronic conditions, such as osteoarthritis (OA), which are largely self-managed, and where adherence to recommended treatments is critical for successful health outcomes.4
OA is a highly prevalent and costly condition, causing pain and disability for 1.9 million Australians.5 Approximately half the population aged over 65 years have radiological evidence of OA, and it is expected that the prevalence of this condition will increase as the population ages and becomes increasingly obese.6 While OA is incurable, there is a range of therapeutic options for symptomatic relief, including pharmacological and nonpharmacological treatments.
For many patients, however, effective interventions appear not to have been adopted. Many factors have been proposed as contributing to nonadherence, including a patient’s personal characteristics,7 social factors,8 the doctor–patient relationship,9 and cognitive factors, including beliefs, attitudes, and perceptions.10 Yet, there have been few studies in Australia that have investigated patients’ views about the management of their OA.
The aim of this study was to evaluate in Australian patients with OA their satisfaction with their health care providers, the determinants of that satisfaction, and the perceived helpfulness of treatments and information sources. An understanding of these perceptions may provide an insight into aspects of care that could be targeted for intervention with the objective of improving OA care.
Methods
Recruitment
A survey was conducted of 560 participants (293 in New South Wales, 267 in South Australia) who self-identified as having OA. These participants were sourced from the CareTrack Australia (CTA) study.11 The CTA was a study conducted in 2009–2010 to assess the appropriateness of health care delivery in Australia. The study examined compliance with quality indicators for 22 common conditions, including OA, in a population-based sample. The quality indicators were taken from a previous US study12 and other sources, and modified after review by expert panels. For recruitment into the CTA study, residential telephone numbers in selected areas in New South Wales and South Australia were randomly selected from the online White Pages. Trained staff then conducted computer-assisted telephone interviews to recruit participants and obtain the required information. Full details of the recruitment method have been described elsewhere.13
Survey instrument
A 19-page self-administered questionnaire comprising three parts was developed (see Supplementary material). A full description of the development and contents of the questionnaire has been previously published;13 however, in brief, the first section was based on Stanford University’s Health Assessment Questionnaire,14 the second section on the Patient Knowledge Questionnaire for Osteoarthritis,15 and the final section explored the participants’ attitudes toward OA and its management. The questionnaire items for this latter section were developed by the authors and assessed for validity by sending the questionnaire to three experts in the field of OA who were asked to judge each question for validity. Reliability of the questions was assessed using a test–retest study. Responses to this final section formed the basis of this paper. Here, participants were given options to respond to yes/no questions, open-ended text, and 5-, 6-, and 10-point Likert scales about satisfaction with aspects of their general practitioner (GP) care, helpfulness of other health professionals in dealing with their OA, effectiveness of different treatment options, including complementary and alternative medicine (CAM), and knowledge and satisfaction with sources of information to manage OA.
Statistical considerations and analysis
The sample size was predetermined as this study was part of CTA. The total number of 435 respondents was sufficient to provide prevalence estimates to, at worst, ±5% accuracy with 95% confidence.
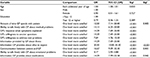
Initial analysis indicated that the majority of patients were satisfied or very satisfied with their GP, and so the question was dichotomized to 1= satisfied or very satisfied, or 0= not satisfied. Logistic regression models were used to assess a number of potential predictors of satisfaction. These included age, sex, level of education, and a number of GP-related questions, which can be found in Table 1. Those variables found to predict satisfaction at the P≤0.05 level were then entered into a multivariable model using backwards elimination. Descriptive results provided in Tables 2–4 are shown as percentages with 95% confidence intervals (CIs). All statistical analyses were undertaken using the Statistical Package for Social Scientists, version 21 (IBM Corporation, Armonk, NY, USA).
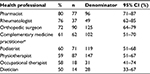  | Table 2 Respondent satisfaction with other health professionals Note: aFor example, chiropractor, osteopath, homeopath, naturopath, or masseur. Abbreviation: CI, confidence interval. |
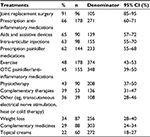  | Table 3 Helpfulness of OA treatments Abbreviations: CI, confidence interval; OA, osteoarthritis; OTC, over-the-counter. |
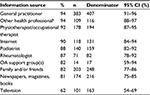  | Table 4 Helpfulness of information sources Note: aFor example, chiropractor, osteopath, homeopath, naturopath, or masseur. Abbreviations: CI, confidence interval; OA, osteoarthritis. |
Simple thematic analysis was applied to the open-ended responses to further illuminate factors related to respondent satisfaction with their health care provider and treatment and information sources, and a number of relevant quotations from this source were included in the results.
Ethical considerations
The study was approved by the Human Research Ethics Committee of the University of South Australia. All participants provided written informed consent.
Results
Study population
A total of 435 questionnaires were returned out of 560 sent, representing a response rate of 78%. The mean (standard deviation) age of the patients was 69 (10) years, and 308/435 (71%) were female. Approximately half the respondents (208/432; 48%) had some form of tertiary education, and the majority (309/435; 71%) was retired from the workforce.
Respondent satisfaction with their GP in managing their OA
In general, respondents were highly satisfied with the level of care provided by their GPs, with 356/426 (84%, 95% CI 80%–87%) reporting that they were satisfied or very satisfied. Similarly, 373/426 (88%, 95% CI 84%–90%) of respondents stated that they were satisfied or very satisfied with the communication with their GP. Eighty-four percent of respondents were highly satisfied with the time spent with their GPs and 93% reported high satisfaction with their ability to talk freely to their GP about their medical problems.
Respondents were slightly less satisfied with their ability to talk freely to their GPs about any emotional problems associated with their condition, with 325/423 (77%, 95% CI 73%–81%) stating that they were either satisfied or very satisfied with this aspect. The tendency of GPs to trivialize OA was the source of some frustration. A typical comment was “I dislike his tendency to put new symptoms down to getting older.” [Female, 50 years old]
Respondents were asked to rate the information provided to them by their GP. Responses were generally positive, with the proportion satisfied or very satisfied being 360/425 (85%, 95% CI 81%–88%) for information about their condition; 337/426 (79%, 95% CI 75%–83%) for information about their prognosis; and 368/427 (86%, 95% CI 83%–87%) for information about their medications.
We explored those factors associated with participants being satisfied or very satisfied with their GP care, and the results are presented in Table 1.
In the univariate model, patients who were older and, not unexpectedly, those who were satisfied with each component of GP care were more likely to express overall satisfaction with care. When all statistically significant variables from the univariate model were entered into the multivariable model, four GP satisfaction factors remained: the amount of time that the GP spends with the patient (P=0.005), the information the GP provides about what to expect (P<0.001), the communication between patient and GP (P=0.001), and the information that the GP provides about medications (P=0.042). Nagelkerke’s R-squared for the multivariable model was 0.734.
Notably, adherence with GP advice was extremely high with 408/425 (96%, 95% CI 94%–98%) of respondents always or usually following the guidance given. Where the GP’s advice was not followed, it was often related to anxiety about taking medications. In some instances, the condition itself limited adherence with GP advice: “I can’t do much exercise, my legs and my neck hurt too much”. [Female, 64 years old]
Respondent satisfaction with other health professionals
Respondents were asked to rate how helpful other health professionals were in dealing with their OA (Table 2). Satisfaction ratings for these other professionals rated less than that for their GP. The highest ranked professionals, with responses of either “very helpful” or “extremely helpful”, were pharmacists, rheumatologists, and orthopedic surgeons, while satisfaction ratings of less than 60% were reported for physiotherapists, occupational therapists, and dieticians.
Helpfulness of OA treatment
Of the common treatments for reducing pain and disability associated with OA, the most helpful (ratings of “helpful” and “extremely helpful”) were joint replacement surgery and prescription anti-inflammatory medications (Table 3). The least helpful therapies reported were weight loss, complementary medicines, and topical creams.
Some respondents expressed concern about the potential adverse effects of drugs with comments, such as the following, from a patient regarding non-steroidal anti-inflammatory drugs [NSAIDs]):
My GP prescribed Mobic (meloxicam) which I took daily. It helped quite a bit, but in retrospect I realized that I shouldn’t have taken it every day for two years. I became very ill with a bleeding stomach ulcer which went undiagnosed for several months despite 5 or 6 visits to 2 separate doctors. [Female, 66 years old]
Information sources
A majority of respondents were satisfied with the information to manage their OA, with 65% (274/420; 95% CI 61%–70%) reporting high overall satisfaction (“very satisfied” or “satisfied”). Ratings for the information sources that helped them to manage their condition were high for health professionals with responses of “helped a bit” to “extremely helpful” for GPs, rheumatologists, physiotherapists, and/or occupational therapists, podiatrists, and other health professionals (Table 4). Family and/or friends were also considered a helpful source of information.
Only a very small number of respondents reported using OA support groups. Several respondents expressed a lack of awareness about support services. Newspapers, magazines and books, and the Internet were helpful for most respondents, while television was the least helpful information source.
Despite general satisfaction with available sources of information, respondents still expressed a need for further material on their condition, with a considerable number wanting to know more about proven treatments. Many respondents expressed despondency about the inaccessibility of reliable information:
I do not know what is available and what information is worth taking notice of or is just rubbish or not scientifically accredited and can be more dangerous than helpful. [Female, 61 years]
Others found the format confusing.
A recurring theme for respondents was their concern about the adverse impact of medications and the need to know more about them, with comments, such as:
I find NSAIDs very helpful, but I do worry about long-term side effects. My husband was hospitalised a few years ago with a duodenal ulcer from taking Voltaren (diclofenac). He needed several blood transfusions because of internal bleeding and has now been advised to never again take anti-inflammatory medication. [Female, 64 years old]
Discussion
Most respondents were highly satisfied with the care provided by their GP, but less so with that provided by allied health professionals. The main predictors of satisfaction with their GP were the time spent with the patient, information provided about what to expect, communication with the patient, and information about medications. The treatment considered to be most helpful was joint replacement surgery. The GP, other health professionals, and the Internet were perceived as the most helpful sources of information.
OA is common and may cause considerable pain, discomfort, and disability. As it cannot be cured, optimizing the available treatments is important. This study sought to better understand patient satisfaction with their care provider and the management of their condition.
Satisfaction with GPs and other health care providers
GPs are the primary providers of care for patients with OA and so it is important that patient satisfaction is measured and evaluated as this has been linked to improved adherence to clinical recommendations, continuity of care, and clinical outcomes.4 Despite this, little has been known about satisfaction with GP care for OA in Australia, as most studies have focused on satisfaction with primary care in general.16–18 The mostly high patient satisfaction ratings reported in our study are consistent with more general research concerning primary care.
As reported elsewhere,16 we found that patient satisfaction increased with the amount of time spent with their GP. While relieving the time pressures that many Australian GPs experience19 may not be a viable option, the recent recommendation made by Arthritis Australia in support of specialist OA practice nurses warrants further exploration,20 as they are the health care professionals most likely to provide self-management support for patients with chronic disease.21
The effectiveness of communication between GP and patient and the information provided by GPs about what to expect were shown in our study to be significant predictors of overall patient satisfaction. Numerous other studies of primary care have made similar findings.22–24 The educational need for enhanced GP skills in lifestyle counseling for patients with OA, identified as an issue for Australian GPs over 10 years ago,25 still needs to be addressed.
Although our study found that nearly all patients reported following the advice given by their GP, it is plausible that the actual rate of adherence may be lower than the rate reported. Other studies have suggested nonadherence among patients with OA represents an important and widespread issue,26,27 and it is possible that respondents to our survey understated their actual behavior.
Helpfulness of OA treatment
Several studies have investigated patient satisfaction with treatments for OA with consistently high satisfaction being reported for joint replacement surgery and prescribed medications. Given that an estimated 80%–90% experience pain relief and functional improvement with joint replacement surgery,28 it is not surprising that this intervention was also rated highly by over 90% of our study participants. Other studies have reported similar satisfaction ratings.29,30
Our finding that nearly two-thirds of patients perceived prescription analgesics and prescription anti-inflammatories to be effective was similar to other studies that reported 50%–70% satisfaction with these medications.30,31 Many respondents expressed an awareness of the risks associated with NSAID use, but for some, as has been suggested by other authors, their potential seriousness may be underestimated.32
Less than half the respondents considered over-the-counter medications, such as paracetamol (acetaminophen) and some NSAIDs, to be very or extremely helpful. Despite their accepted efficacy, patients may have viewed them as less credible, as they were not medically prescribed.33 It has also been reported that patients are not always aware of the place that long-term regular paracetamol plays in the management of OA.34 This was also reflected in our study, so better patient education by their GPs may be warranted. Intra-articular injections can provide rapid short-term relief of OA; however, not all GPs offer this treatment, possibly due to time limitations and/or having not been exposed to this approach during their medical training.
The finding that only 43% of respondents found physiotherapy helpful contrasted with other studies of satisfaction with physiotherapy for musculoskeletal conditions.35,36 It has been reported elsewhere that patients appear to evaluate care and outcome separately and for many, satisfaction with outcome is more important.37 If this is so, low satisfaction with physiotherapy may be attributable to unrealistic expectations of treatment outcomes (eg, restoration of mobility).
CAM use among OA sufferers is widespread13 notwithstanding a paucity of evidence for effectiveness,38 and this is affirmed by the low number of respondents in our survey who found CAM to be helpful. Previous studies have reported that CAM use is not attributable to dissatisfaction with conventional medicine per se, but rather to congruence with the user’s values, beliefs, and philosophical orientation toward health and life.39
Information about OA
Studies have found that patients who are well informed about therapeutic options are more likely to adhere to recommended treatments,40 which is particularly pertinent to OA because of its high sensitivity to patient preferences at all stages of severity.41 Our finding that many respondents expressed a strong desire for improved information about OA, particularly about what to expect as their condition progressed, was consistent with the results reported by Mann and Gooberman-Hill.42
Notably, many respondents in our study expressed a need to know more about the effectiveness of different treatments. However, providing information alone cannot ensure better health outcomes, and this has been recognized by studies which found self-management programs that combined behavioral modification with information provision are more effective than information alone.43
A majority of respondents in our study chose the GP as their preferred information source for managing OA, consistent with findings from a Canadian survey of patients with arthritic conditions.44 Many respondents obtained information from family and friends, although the reliability of this source has been questioned.45
Of the media sources of information, the Internet was considered the most valuable. The unregulated nature of the Internet, however, means that much of the information may be unreliable and potentially biased. A literature review of OA websites reported that accurate and trustworthy information was more commonly found on government or education institution sponsored sites,46 but the issue remains that patients may not have the experience, knowledge, or education to properly assess the credibility of available information.47
There were several limitations to our study. First, we had limited information about health provider practices (practice size, age profile, number of practice nurses employed for clinical work, etc). We also had no clinical information on respondents, such as severity of OA, joints affected, duration of symptoms, and comorbidities. This made it difficult to contextualize the results.
Second, although the response rate was high, there was a possibility of selection bias. For example, those in the target population with OA of the hand may have found the physical completion of the questionnaire difficult, and so may not have responded to the survey. Similarly, those in the target population with cognitive impairment may also have had difficulty completing the survey.
In our study, OA was self-reported rather than diagnosed by a medical professional, which may impact on the findings. Finally, as with all self-reported questionnaires, there is a risk of social desirability bias. For example, patients may have overstated adherence to GP advice, because they did not wish to appear lazy or noncompliant.
Conclusion
The study showed that although patients with OA were generally satisfied with the management of their condition, there was notable variation in the perceived helpfulness of different therapeutic options. Given that better health outcomes in OA can be achieved if treatment recommendations are followed, future research should consider the relationship between adherence and perception of treatment. It would also be informative to further explore the influence of OA information on satisfaction with care.
Acknowledgments
We thank all participants who generously gave their time. This study was funded by a National Health and Medical Research Council Program Grant (number 568612).
Author contributions
MB conceived and performed the study, designed the questionnaire, analyzed and interpreted the data, and drafted the manuscript. TH coordinated the mail out and receipt of questionnaires and data entry, and critically revised the manuscript. TH, WR, PH, and AE analyzed and interpreted the data and critically revised the manuscript. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. | ||
Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260(12):1743–1748. | ||
Chow A, Mayer EK, Darzi AW, Athanasiou T. Patient-reported outcome measures: the importance of patient satisfaction in surgery. Surgery. 2009;146(3):435–443. | ||
Donovan JL. Patient decision making. The missing ingredient in compliance research. Int J Technol Assess Health Care. 1995;11(3):443–455. | ||
Arthritis and Osteoporosis Victoria. A Problem Worth Solving. Melbourne: Arthritis and Osteoporosis Victoria; 2013. | ||
March LM, Bagga H. Epidemiology of osteoarthritis in Australia. Med J Aust. 2004;180(5 suppl):S6–S10. | ||
Aggarwal B, Mosca L. Lifestyle and psychosocial risk factors predict non-adherence to medication. Ann Behav Med. 2010;40(2):228–233. | ||
Molloy GJ, Perkins-Porras L, Bhattacharyya MR, Strike PC, Steptoe A. Practical support predicts medication adherence and attendance at cardiac rehabilitation following acute coronary syndrome. J Psychosom Res. 2008;65(6):581–586. | ||
Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. | ||
Foster JM, Smith L, Bosnic-Anticevich SZ, et al. Identifying patient-specific beliefs and behaviours for conversations about adherence in asthma. Intern Med J. 2012;42(6):e136–e144. | ||
Runciman WB, Hunt TD, Hannaford NA, et al. CareTrack: assessing the appropriateness of health care delivery in Australia. Med J Aust. 2012;197(10):100–105. | ||
McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. | ||
Basedow M, Runciman W, March L, Esterman A. Australians with osteoarthritis; the use of and beliefs about complementary and alternative medicines. Complement Ther Clin Pract. 2014;20(4):237–242. | ||
Fries JF, Cella D, Rose M, Krishnan E, Bruce B. Progress in assessing physical function in arthritis: PROMIS short forms and computerized adaptive testing. J Rheumatol. 2009;36(9):2061–2066. | ||
Hill J, Bird H. Patient knowledge and misconceptions of osteoarthritis assessed by a validated self-completed knowledge questionnaire (PKQ-OA). Rheumatology (Oxford). 2007;46(5):796–800. | ||
Potiriadis M, Chondros P, Gilchrist G, Hegarty K, Blashki G, Gunn JM. How do Australian patients rate their general practitioner? A descriptive study using the General Practice Assessment Questionnaire. Med J Aust. 2008;189(4):215–219. | ||
Allan J, Schattner P, Stocks N, Ramsay E. Does patient satisfaction of general practice change over a decade? BMC Fam Pract. 2009;10:13. | ||
Young AF, Byles JE, Dobson AJ. Women’s satisfaction with general practice consultations. Med J Aust. 1998;168(8):386–389. | ||
Joyce CM, Schurer S, Scott A, Humphreys J, Kalb G. Australian doctors’ satisfaction with their work: results from the MABEL longitudinal survey of doctors. Med J Aust. 2011;194(1):30–33. | ||
Arthritis Australia Models of Care Steering Group. Time to Move: Osteoarthritis. A National Strategy to Reduce a Costly Burden. Sydney: Arthritis Australia; 2014. | ||
Dziedzic KS, Healey E, Main CJ. Implementing the NICE Osteoarthritis Guidelines in primary care: a role for practice nurses. Musculoskeletal Care. 2013;11(1):1–2. | ||
Little P, Everitt H, Williamson I, et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. Br Med J. 2001;322(7284):468–472. | ||
Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002;15(1):25–38. | ||
Robertson R, Dixon A, Le Grand J. Patient choice in general practice: the implications of patient satisfaction surveys. J Health Serv Res Policy. 2008;13(2):67–72. | ||
Saltman DC, O’Dea NA, Sambrook PN. Managing osteoarthritis in general practice: a long-term approach. Med J Aust. 2001;175:(Suppl):S92–S96. | ||
Marks R. Knee osteoarthritis and exercise adherence: a review. Curr Aging Sci. 2012;5(1):72–83. | ||
Laba T-L, Brien J-a, Fransen M, Jan S. Patient preferences for adherence to treatment for osteoarthritis: the MEdication Decisions in Osteoarthritis Study (MEDOS). BMC Musculoskelet Disord. 2013;14:160. | ||
Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113–1121. | ||
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. | ||
Juby AG, Skeith K, Davis P. Patients’ awareness, utilization, and satisfaction with treatment modalities for the management of their osteoarthritis. Clin Rheumatol. 2005;24(5):535–538. | ||
Tallon D, Chard J, Dieppe P. Exploring the priorities of patients with osteoarthritis of the knee. Arthritis Care Res. 2000;13(5):312–319. | ||
Milder TY, Williams KM, Ritchie JE, Lipworth WL, Day RO. Use of NSAIDs for osteoarthritis amongst older-aged primary care patients: engagement with information and perceptions of risk. Age Ageing. 2011;40(2):254–259. | ||
Nunes V, Neilson J, O’Flynn N, et al. Clinical Guidelines and Evidence Review for Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence. London: National Collaborating Centre for Primary Care and Royal College of General Practitioners; 2009. | ||
Barozzi N, Tett SE. Perceived barriers to paracetamol (acetaminophen) prescribing, especially following rofecoxib withdrawal from the market. Clin Rheumatol. 2009; 28(5):509–519. | ||
Hush J, Yung V, Mackey M, et al. Patient satisfaction with musculoskeletal physiotherapy care in Australia: an international comparison. J Man Manip Ther. 2012;20(4):201–208. | ||
Casserley-Feeney SN, Phelan M, Duffy F, Roush S, Cairns MC, Hurley DA. Patient satisfaction with private physiotherapy for musculoskeletal pain. BMC Musculoskelet Disord. 2008;9:50. | ||
Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine. 2000;25(24):3167–3177. | ||
De Silva V, El-Metwally A, Ernst E, Lewith G, Macfarlane GJ. Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review. Rheumatology. 2011;50:911–920. | ||
Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. | ||
Levesque A, Li HZ, Pahal JS. Factors related to patients’ adherence to medication and lifestyle change recommendations: data from Canada. Int J Psychol Stud. 2012;4(2):42–55. | ||
Rivero-Santana A, Perestelo-Perez L, Perez-Ramos J, Gonzalez-Lorenzo M, Serrano-Aguilar P. Treatment preferences in patients with knee or hip osteoarthritis: an overview. In: Chen Q, editor. Osteoarthritis – Diagnosis, Treatment and Surgery. Rijeka: In Tech; 2012. Available from: http://cdn.intechopen.com/pdfs-wm/30691.pdf. Accessed October 1, 2015. | ||
Mann C, Gooberman-Hill R. Health care provision for osteoarthritis: concordance between what patients would like and what health professionals think they should have. Arthritis Care Res. 2011;63(7):963–972. | ||
Riemsma RP, Taal E, Kirwan JR, Rasker JJ. Systematic review of rheumatoid arthritis patient education. Arthritis Rheum. 2004;51(6):1045–1059. | ||
Neville C, Fortin PR, Fitzcharles MA, et al. The needs of patients with arthritis: the patient’s perspective. Arthritis Care Res. 1999;12(2):85–95. | ||
Bower KN, Frail D, Twohig PL, Putnam W. What influences seniors’ choice of medications for osteoarthritis? Can Fam Physician. 2006;52:342–343. | ||
Pietrzak E, Cotea C, Pullman S. Can the Internet Improve Health Outcomes in Osteoarthritis Patients and Provide Reliable Information about the Disease? Brisbane: Centre for Military and Veterans Health; 2012. | ||
Weber BA, Derrico DJ, Yoon SL, Sherwill-Navarro P. Educating patients to evaluate web-based health care information: the GATOR approach to healthy surfing. J Clin Nurs. 2010;19(9–10):1371–1377. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.