Back to Journals » Patient Preference and Adherence » Volume 13
Attitudes Of Chinese Cancer Patients Toward The Clinical Use Of Artificial Intelligence
Authors Yang K , Zeng Z , Peng H , Jiang Y
Received 4 August 2019
Accepted for publication 16 October 2019
Published 1 November 2019 Volume 2019:13 Pages 1867—1875
DOI https://doi.org/10.2147/PPA.S225952
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Keyi Yang, Zhi Zeng, Hu Peng, Yu Jiang
Department of Head and Neck Oncology, Cancer Center, West China Hospital, Sichuan University, Chengdu, Sichuan, People’s Republic of China
Correspondence: Yu Jiang
Department of Head and Neck Oncology, Cancer Center, West China Hospital, Sichuan University, No. 37, Guo Xue Lane, Chengdu, Sichuan 610041, People’s Republic of China
Tel/fax +86 28 85423278
Email [email protected]
Purpose: Artificial intelligence (AI) plays a substantial role in many domains, including medical fields. However, we still lack evidence to support whether or not cancer patients will accept the clinical use of AI. This research aims to assess the attitudes of Chinese cancer patients toward the clinical use of artificial intelligence in medicine (AIM), and to analyze the possible influencing factors.
Patients and methods: A questionnaire was delivered to 527 participants. Targeted people were Chinese cancer patients who were informed of their cancer diagnosis.
Results: The effective response rate was 76.3% (402/527). Most cancer patients trusted AIMs in both stages of diagnosis and treatment, and participants who had heard of AIMs were more likely to trust them in the diagnosis phase. When an AIM’s diagnosis diverged from a human doctor’ s, ethnic minorities, and those who had received traditional Chinese medicine (TCM), had never received chemotherapy, were more likely to choose “AIM”, and when an AIM’s therapeutic advice diverged from a human doctor’s, male participants, and those who had received TCM or surgery, were more likely to choose “AIM”.
Conclusion: Most Chinese cancer patients believed in the AIM to some extent. Nevertheless, most still thought that oncology physicians were more trustworthy when their opinions diverged. Participants’ gender, race, treatment received, and AIM related knowledge might influence their attitudes toward the AIM. Most participants thought AIM would assist oncology physicians in the future, while little really believed that oncology physicians would completely be replaced.
Keywords: artificial intelligence, attitude, cancer, cancer patient, clinical use, oncology
Introduction
After the digital revolution, also known as the third industrial revolution, which ended around the late 1970s with its continual impact up to the present day, we may be witnessing the fourth industrial revolution, namely artificial intelligence (AI).1 The phrase “AI” first appeared at a famous Dartmouth College conference in 1956.2 And the earliest work in medical AI dates back to the early 1970s, also known as the AI in medicine (AIM).3
A boom is now emerging in AI technology in many domains, and in healthcare, it can be epoch-making in the near future. Major disease areas use AI tools include cancer, neurology, and cardiology; mainly, the studies have been about neoplasms.4 For example, Shiraz et al developed a computational intelligence system for breast cancer detection.5 Arau´jo et al demonstrated that they could distinguish breast carcinoma from healthy tissues by histology images using convolutional neural networks (CNNs) with a sensitivity of 95.6%.6 Vandenberghe et al even set up a digital approach based on deep learning to automatically score the human epidermal growth factor receptor 2 (HER2), with a concordance of 83.0% with a pathologist.7 Treatment recommendations made by Watson for Oncology (WFO) were highly concordant compared with a multidisciplinary tumor board for breast cancer cases.8
The application of AIM in oncology is much beyond breast cancer. An increasing number of AIMs are invented and applied to the clinical decision support of many other types of tumors such as lung cancer.9 However, AI poses limitations and threats, but might be a boon, mainly due to the interpersonal and interventional intrinsic quality of medical activities.
In China, we may have the largest number of patients, so it is a general trend to apply AIMs to clinic. However, as we discuss the marvelous advances and limitations of the AIMs, the feelings of patients are naturally neglected. Whether patients will accept it or not is still a question, and our answer to that is little more than guesswork. Thus, it is crucial to investigate Chinese cancer patients’ attitudes toward the clinical use of artificial intelligence.
Materials And Methods
Subjects
Four oncology departments from two university hospitals were involved in this study. To be eligible for the study, subjects needed to be over 18 years old, with a pathological diagnosis of cancer and being informed of their cancer diagnosis, well enough to fill out a questionnaire independently and communicate with the interviewer. All researching activities held adhered to the principle of voluntary participation with written informed consent. Incomplete questionnaires for any reason were excluded.
Definition Of Principle Terms
To make the term “AIM” easier to understand for patients from different levels and cultures, we defined AIM in the questionnaire as “Computer systems or robots that perform clinical medical activities independently or as ancillaries of human physicians”.10
Questionnaire
A questionnaire was designed to investigate Chinese cancer patients’ attitudes toward AIM based on a cross-sectional study. Information collected by the questionnaire can be divided into four groups as following: (1) Demographic and characteristics of patients, including age, gender, ethnicity, marital status, educational level, occupation, religious beliefs, place of residence, and family income. (2) Clinical information, including tumor category, time since the initial diagnosis, Eastern Cooperative Oncology Group performance status (ECOG PS), and treatment received. (3) Knowledge reserve, where patients were to indicate whether they had ever heard of AIM and how much they knew about AIM. (4) Information about participants’ attitudes toward the clinical use of AI. The last part included 11 major questions that covered the following: (1) the reliability of a diagnostic, therapeutic, and prognostic advice given by an AIM independently; (2) when given different advice from AIMs and oncology physicians, which was more credible, and the most important reason for the choice; and (3) the advantages and disadvantages of AIMs, and the outlook of them. The complete questionnaire is listed in the online supplemental materials (Figure S1).
Study Procedures
Questionnaires were distributed to all eligible inpatients. Before administration, the questionnaire was pilot-tested for 30 cancer patients to make sure it was intelligible. All participants were asked not to share the information with others. Questionnaires were anonymously filled out by participants independently or with the help of the interviewer. This study was approved by the medical ethical committee of Cancer Center of Sichuan University, China (2015–152).
Statistical Analysis
All records were collected and input into a computer database. Descriptive statistics were carried out for the participants’ demographic characteristics, clinical information, knowledge reserve, and Information about participants’ attitudes toward the clinical use of AI. Fisher’s exact test was conducted when the Chi-squared test was inapplicable in the single-factor analysis. Chi-squared test, Fisher’s exact test, and univariate logistic regression analysis were used to filter out potential significant predictors of attitudes towards AIMs. Any factor with P < 0.1 in either single-factor analysis method would be further evaluated by multivariable logistic regression analysis, the result of which would be finally presented. We set the significance level at P < 0.05 when the multiple-factor analysis was done. All tests of statistical significance were two-tailed tests. SPSS (Version 25.0) was used for data analysis.
Results
The effective response rate was 76.3% (402/527). The two most common reasons for not participating were lack of time and physical discomfort. The demographic and clinical information of participants was summarized in Table 1. Of all the 402 patients, 259 (64.3%) had never heard of AIM before our contact (Table 2). Only 24 (6.0%) demonstrated that they were familiar with AIMs to some extent (Table 2). Patients with bachelor’s degrees and higher educational qualifications were more likely to hear about AIMs as compared with those without one (46.6% vs 27.0%; OR, 2.36; 95% CI, 1.43–3.91, P = 0.001; where OR stands for odds ratio and CI, confidence interval). Male patients (OR, 2.52; 95% CI, 1.03–6.18, P = 0.043) and those with bachelor’s degrees and higher educational qualifications (OR, 3.80; 95% CI, 1.30–11.16, P = 0.015) exhibited more familiarity with AIMs.
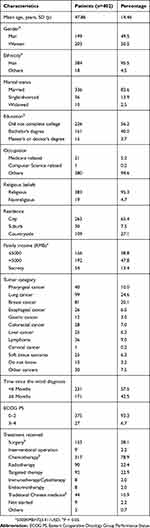 |
Table 1 Demographic Characteristics Of Patients |
 |
Table 2 AIM-Related Knowledge Reserve Of Patients |
Attitudes Toward AIMs In The Diagnosis Phase
Attitudes Toward The Question “Do You Believe In The Diagnosis Made By An AI Doctor Independently?”
Of 402, 362 (90.0%) participants reported that they believed to some extent in the diagnosis made by an AIM independently (Table 3). All 24 patients who had stated that they had a better understanding of AIM chose “Yes” to this question. Participants who had heard of AIM were more likely to choose “Yes” (OR, 2.38; 95% CI, 1.07–5.31, P = 0.035) (Table S1 of online supplemental materials).
 |
Table 3 Patients Attitudes Toward The Clinical Use Of AI |
Attitudes Toward The Question “Whose Suggestion Do You Prefer To Take When AIM’s Diagnosis Diverges From Human Doctor’s?”
Among 402, 45 (11.2%) participants reported that they believed in AIM’s diagnosis, while the majority of patients (88.8%) preferred to take human doctors’ diagnostic advice (Table 3). Patients who had received traditional Chinese medicine (TCM) (OR, 2.46; 95% CI, 1.07–5.66, P = 0.034), had never received chemotherapy (OR, 2.18; 95% CI, 1.10–4.30, P = 0.025), and minorities (OR, 4.43; 95% CI, 1.52–12.90, P = 0.006) were more likely to choose “AIM” (Table S1 of online supplemental materials). See the leading causes of choosing AIM in Tables S2 and S4 of online supplemental materials.
Attitudes Toward AIMs In Treatment Scheme Making
Attitudes Toward The Question “Do You Believe In The Therapeutic Advice Made By An AI Doctor Independently?”
The majority of patients (85.1%) believed in the therapeutic advice made by an AI doctor independently to some extent (Table 3). Patients who had heard of AIM were more likely to choose “Yes” than those who had never heard of AIM (89.5% vs 82.6%), but with no significant statistical difference.
Attitudes Toward The Question “Whose Suggestion Do You Prefer To Take When AIM’s Therapeutic Advice Diverges From Human Doctor’s?”
Only 35 out of 402 (8.7%) participants preferred to take AIM’s therapeutic advice, while the other 367 (91.3%) chose to take human doctor’s advice (Table 3). However, participants who had received TCM (OR, 2.91; 95% CI, 1.21–7.03, P = 0.018) or surgery (OR, 2.12; 95% CI, 1.02–4.42, P = 0.044), and male patients (OR, 2.99; 95% CI, 1.38–6.50, P = 0.006) were more likely to choose AIM (Table S1 of online supplemental materials). See the most important reasons for the choices in Tables S3 and S4 of online supplemental materials.
Attitudes Toward AIMs In A Follow-Up
Attitudes Toward The Question “To Whom Would You Like To Discuss The Effect Of The Therapy Or Prognosis Of The Disease After The Treatment?”
In our study, 355 patients (88.3%) preferred to report their physical condition to human doctors, while only 37 (9.2%) chose AIM, and another 10 (2.5%) reported their ideas as unwilling to receive follow-ups (Table 3). The answers to this question were not influenced by any demographic and clinical characteristics and knowledge reserve of patients.
Other Details
When asked the question, “Do you expect the presence of a human doctor in an AI clinic,” only four gave a negative answer (Table 3). Being more economical and convenient was regarded as an advantage of AIM by most people, and the lack of capability to deal with complicated disorders was considered a disadvantage of AIM by the majority ((Figures 1 and 2, and Table S4 of online supplemental materials). Only five participants thought that AIM in oncology would be eliminated; 228 thought AI equipment would assist oncology physicians, while 122 held the idea that oncology physicians would assist AIM in the future. Another 47 participants believed AIM would replace oncology physicians completely (Figure S2 of online supplemental materials).
Discussion
Since origin, AI has developed rapidly during the past several decades, and AI-related topics remain hot. We have developed various algorithms to try to put AI into clinical application,5–9 but we always have been ignoring the patients’ willingness to accept them. In our study, less than half of the participants had ever heard of AIMs (Table 2), which is less than that in the Central and Eastern Europe (CEE) population, according to the first local CEE study on AI conducted for IBM.11 Over three quarters expected the presence of a human doctor in an AI clinic (Table 3). A published report had also shown that a human-AI pair might perform better than an individual AI.12 Still, there were four participants who were unwilling to see a human doctor in an AI clinic, of whom two had been diagnosed of breast cancer, and another two had colorectal cancer. Unwillingness to disclose disorders of private parts could be one possible reason, which indicates that patients might reveal some details to AI doctors that were too private to tell human doctors.13
Auxiliary examination methods were important in tumor diagnosis, and AIMs have been extensively studied in those fields. The accuracy of an AIM is not necessarily poorer than human experts, which could give strong support to the vast majority of the participants who reported their trust in AIMs, either in our study (Table 3) or others’.11,14 Nam et al developed an algorithm that outperformed physicians in recognizing malignant pulmonary nodules on chest radiographs.9 A similar “AIM conquers human experts” case was discovered by Bejnordi et al, in whose study deep learning algorithms performed better in detecting lymph node metastases of breast cancer with time constraints.15 However, the AIMs were not always the better one. Hirasawa et al reported their application of AI in detecting gastric cancer in endoscopic images, in their study, 71 of 77 (92.2%) gastric cancer lesions were correctly detected by a CNN though, 161 non-cancerous stomach endoscopic images were also diagnosed as gastric cancer.16 As for decision-making for a treatment, in case of the most well-known AIM, WFO, which was used by hundreds of hospitals all over the world, many of the therapeutic recommendations were proved to be erroneous.8,17 AIMs might do better in some study with a certain diagnostic direction, but human experts could see more when given the same amount of information, and overturn the results of AIMs,18 like the algorithm mentioned previously, which was trained only for malignant lesions. Benign lung nodules, types of pneumonia, and interstitial lung disease were not considered in that research.9 It was no wonder that when divergence arose, most people tended to be convinced by human doctors (Table 3). Nonetheless, male participants, minorities, and those who had received TCM or surgery, or had never received chemotherapy were more likely to show more trust in AIMs than oncology physicians (Table S1 of online supplemental materials). Ethnic minority inpatients might carry their cultural views;19 thus, they showed less confidence in western medicine and doctors, and in turn, tended to believe in AIMs. Actually, in a study conducted by Hamilton et al, race/ethnicity did influence the caregivers’ attitude toward health app.20 According to our study, 77.8% of the ethnic minority patients who completed our questionnaires had bachelor’s degrees or higher educational qualifications, while this proportion was only 42.2% in the Han Chinese. Similarly, people with bachelor’s degrees and higher educational qualifications made up 54.6% of the patients who had received TCM, while the proportion was only 42.4% in those who had not. Moreover, according to our data, patients with higher education were more likely to hear about AIMs. As mentioned before, because patients who had heard of AIMs were more likely to trust them, this could be one possible reason why ethnic minority inpatients and those who had received TCM were more likely to trust in AIMs than oncology physicians. In addition, in our study, 42.5% of postoperative patients had heard of AIM, but only 31.3% of patients of the non-operated group had ever heard of AIM. This could explain why postoperative patients were more likely to show more trust in AIMs than oncology physicians. A course of chemotherapy often takes a significant amount of time, during which a patient’s trust in his doctor might increase,21 while, patients who had never received chemotherapy could show less. However, gender was not reported as an influencing factor for Chinese patients’ trust in physicians,21 the reason why male patients were more likely to trust AIMs might be that male patients knew more about AIMs, according to our data; another reason might be the different attitudes of men and women towards computer science, which still needs further research.
Although oncology physicians were more trustworthy than AIMs, statistical results demonstrated that participants who had heard of AIMs were still more likely to believe in the diagnosis made by an AIM independently (Table S1 of online supplemental materials). This result was not beyond our expectations. Santos et al also found in their research that more tech-savvy medical students tended to be more confident about the impact of computer science on medicine.22 In addition, a journalistic article in China reported that people who knew better about AI were more likely to accept them.23 To our surprise, knowledge reserve was not one of the factors influencing people’s trust in the therapeutic advice made by an AI doctor independently; this might be because the therapeutic capacities of AIMs still do not appear to be entirely proved. Since the establishment of initial trust is fairly important when a new technology is put to use,24 thus, to establish the initial trust by strengthening the education about AIMs is significant. However, as only a few participants demonstrated that they were familiar with AIMs, a larger sample size is needed to verify our findings further.
The most frequent reasons for believing in human doctors other than AIMs were mainly about their greater ability at complicated situations (Tables S2 and S3 of online supplemental materials). In fact, they were right in this respect. The AI techniques required scientific literature and electronic medical records to learn and mainly involved only one or one type of disease. Past medical records not necessarily covered all clinical cases, and scientific literature was often rigorously designed with strict inclusion and exclusion criteria which were far from realistic clinic. Therefore, the learning resource of AIM could never represent every possibility. Physicians could often provide the most proper advice considering the patients’ current comorbidities and complications, thus performing better in complicated situations.
At the end of the treatment comes the stage of follow-up. In our study, only 10 of 402 (2.5%) participants unequivocally stated their unwillingness to receive follow-ups (Table 3); however, when questioned further regarding their preference, most participants chose human doctors with no influencing factors. In our clinical practice, follow-up was supposed to be an integrated part of the treatment, which often started with the end of one phase of anti-tumor therapy. Comorbidities, complications, relapse, or progression of cancers, as well as the preferred treatment strategies after cancer relapse or progression might be more frequently considered in this medical stage by physicians. Because of the lack of capability of AIMs to deal with such situations, and additionally, follow-up is done automatically by a programmed AI, which could bring a sense of indifference, our participants’ choices were comprehensible.
It was demonstrated that AIMs had their superiority; nevertheless, limitations also existed. Both advantages and disadvantages are demonstrated in Figures 1 and 2, and Table S4 of online supplemental materials.
“Being more economical and convenient” got the most votes as an advantage of AIMs (Figure 1), which was generally consistent with another similar study conducted by Liu et al14. Many studies considered the shorter decision-making time as a major advantage of AIM, while few actually mentioned the cost it took to get advice from an AIM. Therefore, to satisfy patients, reducing costs, and improving the efficiency of an AIM application is necessary. “Help to accomplish therapy in plan” was only two votes behind (Figure 1). Long-term treatment is needed to fight cancer, and as a study conducted by Ali et al claimed, facing difficulty in maintaining adherence was thought to be a facilitating factor for patients taking oral anticancer medications using an app in healthcare,25 AIMs might be popular with a large number of patients in China who might not be able to maintain adherence to their medications due to a variety of reasons.
Only 157 thought AIMs could improve the accuracy of doctor’s advice, and 149 believed they could reduce the rate of missed diagnosis and misdiagnosis (Figure 1). Actually, when comparing the accuracy of an individual reader with a physician being assisted by an AIM given the thoracic computed tomography (CT) scans, the latter performed evidently better, in a study we mentioned previously.12 The application of AIM at primary hospitals could also be a substantial benefit, according to our results.
Two hundred and fifty thought the AIM’s lack of capability to deal with complicated disorders was a potential shortcoming of them (Figure 2), which was basically in accordance with their most frequent reason for choosing oncology physicians (Tables S2 and S3 of online supplemental materials). Further, it was interesting that while 210 regarded the lack of humane care as one defect of AI doctors (Figure 1), only three who trusted human’s diagnosis and two who trusted human’s treatment advice reported their most important reason for their choice as humane care related, which further demonstrated that most people regarded the accuracy of medical advice as more important and beneficial.
However, it was not that humane care was not important. In fact, the doctor-patient relationship was not only found to be the highest predictor of patients’ satisfaction, but also to influence the subjective symptom burden.26 A better doctor-patient relationship and a warm and empathic atmosphere during treatments might even increase the placebo response.27,28 Therefore, equipping the AIMs with humane care capability makes much sense.
Human doctors were still indispensable in most patients’ opinions (Figure S2 of online supplemental materials). Wen and his team also reached similar conclusions in their survey on Chinese medical students.29 Medicine was intrinsically complex and multi-disciplinary. For example, it was difficult for oncology physicians to diagnose fractures fast and accurately; however, researchers found increased sensitivity and specificity and reduced misinterpretation rate, with the assistance of a deep learning model when detecting fractures through X-ray imaging.30 Rubin et al also demonstrated that a computer-aided detection algorithm for pulmonary nodule detection on CT scans did better than a second reader when used as a complement to an individual reader.12 Therefore, different AIMs being used to assist physicians of different specialties might be in the foreseeable future as our participants expected.
Our study had several limitations. First, we distributed the questionnaire in only one region of China, though patients from nearly all over the country come to our hospitals. Second, we gave too broad and simple a definition of AIM. However, the education levels of cancer patients were varied, and the definition we gave was more likely to be understood by every participant. Third, we failed to provide some specific situations in which patients might exhibit different attitudes in our questionnaire. For example, this could happen that an AI doctor’s suggestion is closer to a patient’s expectation compared with that of a human physician. Fourth, we failed to provide an option about humane care for the questions, which may cause some bias. Fifth, only cancer patients were included in our research, while AIMs are also applied to other fields of healthcare like childhood cataracts.31
This is the first study assessing Chinses cancer patients’ attitudes toward AIMs through a questionnaire, also the first to analyze the possible influencing factors, as far as we know, and it has implications in guiding efforts to draft the interrelated policies and apply AIMs into clinical use as assistants to human doctors. We believe that the willingness of patients deserves a lot more attention, and we hope that studies concerning other diseases will spring up in the future.
Conclusion
This study found that most Chinese cancer patients believed in the AIMs to some extent. Nevertheless, most still thought that oncology physicians were more trustworthy when their opinions diverged. Participants’ gender, race, treatment received, and AIM related knowledge might influence their attitudes toward the AIM. Most participants thought AIM would assist oncology physicians in the future, while little really believed that oncology physicians would completely be replaced.
Acknowledgements
We thank all participants for their help. We also thank all the doctors and nurses who helped us in this study.
Author Contributions
Keyi Yang and Yu Jiang contributed to the conception and design of the study. Keyi Yang conducted the data acquisition with the help of Zhi Zeng and Hu Peng. Data analysis and interpretation and drafting of the manuscript was done by Keyi Yang. All authors revised the article critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Frueh SJ. The fourth industrial revolution: proceedings of a workshop-in brief. Paper presented at: Government-University-Industry Research Roundtable Meeting; Washington, DC, 25–26 October 2016. doi:10.17226/24699
2. McCarthy J, Minsky ML, Rochester N, Shannon CE. A Proposal for the Dartmouth Summer Research Project on Artificial Intelligence, August 31, 1955. AI Magazine. 2006;27(4):12–14. doi:10.1609/aimag.v27i4.1904
3. Patel VL, Shortliffe EH, Stefanelli M, et al. The coming of age of artificial intelligence in medicine. Artif Intell Med. 2009;46(1):5–17. doi:10.1016/j.artmed.2008.07.017
4. Jiang F, Jiang Y, Zhi H, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–243. doi:10.1136/svn-2017-000101
5. Zadeh Shirazi A, Seyyed Mahdavi Chabok SJ, Mohammadi Z. A novel and reliable computational intelligence system for breast cancer detection. Med Biol Eng Comput. 2018;56(5):721–732. doi:10.1007/s11517-017-1721-z
6. Araujo T, Aresta G, Castro E, et al. Classification of breast cancer histology images using convolutional neural networks. PLoS One. 2017;12(6):e0177544. doi:10.1371/journal.pone.0177544
7. Vandenberghe ME, Scott MLJ, Scorer PW, Söderberg M, Balcerzak D, Barker C. Relevance of deep learning to facilitate the diagnosis of HER2 status in breast cancer. Sci Rep. 2017;7:45938. doi:10.1038/srep45938
8. Somashekhar SP, Sepulveda MJ, Puglielli S, et al. Watson for Oncology and breast cancer treatment recommendations: agreement with an expert multidisciplinary tumor board. Ann Oncol. 2018;29(2):418–423. doi:10.1093/annonc/mdx781
9. Nam JG, Park S, Hwang EJ, et al. Development and validation of deep learning-based automatic detection algorithm for malignant pulmonary nodules on chest radiographs. Radiology. 2019;290(1):218–228. doi:10.1148/radiol.2018180237
10. Kaplan A, Haenlein M. Siri, Siri, in my hand: who’s the fairest in the land? On the interpretations, illustrations, and implications of artificial intelligence. Bus Horiz. 2019;62(1):15–25. doi:10.1016/j.bushor.2018.08.004
11. Stachera T. IBM survey: CEE citizens trust in artificial intelligence. Available from: https://www.linkedin.com/pulse/ibm-survey-cee-citizens-trust-artificial-intelligence-tomasz-stachera?articleId=6481877528502890496. Published 2018. Accessed September 28, 2019.
12. Rubin GD, Lyo JK, Paik DS, et al. Pulmonary nodules on multi-detector row CT scans: performance comparison of radiologists and computer-aided detection. Radiology. 2005;234(1):274–283. doi:10.1148/radiol.2341040589
13. Liu PL, Yeo TED. Breast health, risk factors, and cancer screening among lesbian, bisexual, and queer/questioning women in china. Health Care Women Int. 2019;1–15. doi:10.1080/07399332.2019.1571062
14. Liu L, He Y, Liu X. Investigation on patients’ cognition and trust in artificial intelligence medicine. Chin Med Ethics. 2019;32(8):986–990.
15. Ehteshami Bejnordi B, Veta M, Johannes van Diest P, et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA. 2017;318(22):2199–2210. doi:10.1001/jama.2017.14585
16. Hirasawa T, Aoyama K, Tanimoto T, et al. Application of artificial intelligence using a convolutional neural network for detecting gastric cancer in endoscopic images. Gastric Cancer. 2018;21(4):653–660. doi:10.1007/s10120-018-0793-2
17. Ross C, Swetlitz I IBM’s Watson supercomputer recommended “unsafe and incorrect” cancer treatments, internal documents show. 2018 July 25. Available from: https://www.statnews.com/2018/07/25/ibm-watson-recommended-unsafeincorrect-treatments/Updated.
18. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56. doi:10.1038/s41591-018-0300-7
19. Degrie L, Gastmans C, Mahieu L, Dierckx de Casterlé B, Denier Y. How do ethnic minority patients experience the intercultural care encounter in hospitals? A systematic review of qualitative research. BMC Med Ethics. 2017;18(1):2. doi:10.1186/s12910-016-0163-8
20. Hamilton EC, Saiyed F, Miller CC
21. Pan J, Zhao J, Hou Y. Analysis on current stiuation and effective factors of patients’ trust in physicians. Guangdong Med J. 2017;38(06):941–943.
22. Pinto Dos Santos D, Giese D, Brodehl S, et al. Medical students’ attitude towards artificial intelligence: a multicentre survey. Eur Radiol. 2019;29(4):1640–1646. doi:10.1007/s00330-018-5601-1
23. Hu Y, Zhu X. “The phantom public” of artificial intelligence – an empirical study on professional journalists. China Publishing J. 2018;19:15–21.
24. Zhu Z, Liu Y, Che X, Chen X. Moderating factors influencing adoption of a mobile chronic disease management system in China. Inform Health Soc Care. 2018;43(1):22–41. doi:10.1080/17538157.2016.1255631
25. Ali EE, Chan SSL, Leow JL, Chew L, Yap KY-L. User acceptance of an app-based adherence intervention: perspectives from patients taking oral anticancer medications. J Oncol Pharm Pract. 2019;25(2):390–397. doi:10.1177/1078155218778106
26. Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323(7318):908–911. doi:10.1136/bmj.323.7318.908
27. Kelley JM, Lembo AJ, Ablon JS, et al. Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosom Med. 2009;71(7):789–797. doi:10.1097/PSY.0b013e3181acee12
28. Riedl D, Schussler G. The influence of doctor-patient communication on health outcomes: a systematic review. Z Psychosom Med Psyc. 2017;63(2):131–150. doi:10.13109/zptm.2017.63.2.131
29. Wen L, Zhao X, He L. A survey on the medical students’ attitude towards artificial intelligence. Contin Med Educ. 2019;33(07):12–13.
30. Lindsey R, Daluiski A, Chopra S, et al. Deep neural network improves fracture detection by clinicians. Proc Natl Acad Sci U S A. 2018;115(45):11591–11596. doi:10.1073/pnas.1806905115
31. Lin H, Li R, Liu Z, et al. Diagnostic efficacy and therapeutic decision-making capacity of an artificial intelligence platform for childhood cataracts in eye clinics: a multicentre randomized controlled trial. EClinicalMedicine. 2019;9:52–59. doi:10.1016/j.eclinm.2019.03.001
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


