Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Association of the Coronavirus Disease 2019 Outbreak on the Diabetes Self-Management in Chinese Patients: An Analytical Cross-Sectional Study
Authors Huang L, Zhang L, Jiang S, Liang B, Xu N, Li J, Zhang X, Zhang Z
Received 8 February 2022
Accepted for publication 20 April 2022
Published 6 May 2022 Volume 2022:15 Pages 1413—1422
DOI https://doi.org/10.2147/DMSO.S351823
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Linyan Huang1 *, Li Zhang1,2 *, Shuiping Jiang,1 Baozhu Liang,1 Ningning Xu,1 Jingxin Li,1 Xiaoyan Zhang,1,3 Zhen Zhang1
1Department of Endocrinology, Zhujiang Hospital, Southern Medical University, Guangzhou, People’s Republic of China; 2Department of Endocrinology, People’s Hospital of Dehong, Yunnan, People’s Republic of China; 3Department of Pediatrics, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, People’s Republic of China
* These authors contributed equally to this work
Correspondence: Zhen Zhang, Department of Endocrinology, Zhujiang Hospital, Southern Medical University, 253 Industrial Avenue, Guangzhou, Guangdong, 510282, People’s Republic of China, Tel +86-15913162742, Email [email protected]
Background: The coronavirus disease 2019 (COVID-19) outbreak has seriously affected people’s lives, especially those with chronic diseases. Diabetes self-management, which plays an important role in glycaemic control and reducing the risk of acute and long-term complications, may be discouraged by social distancing.
Purpose: To evaluate the level of self-management activities in Chinese patients with type 2 diabetes mellitus (T2DM) during the COVID-19 pandemic.
Patients and Methods: A survey of with 872 patients with T2DM in the inpatient and outpatient departments through face-to-face interviews was conducted from 1 July, 2020 to 30 September, 2020. The main outcome measures were glycaemic control status and level of self-management activities during the pandemic.
Results: In terms of glycaemic control, the data showed that patients with fasting plasma glucose (FPG) < 7.0 mmol/L (36.4%), postprandial plasma glucose (PPG) < 10.0 mmol/L (26.3%), or glycosylated haemoglobin (HbA1c) < 7.0% (18.6%) in our investigation has well-controlled blood glucose level, and 11.9% of patients experienced blood glucose < 3.9 mmol/L during the outbreak. The diabetes self-management of Chinese patients decreased and the final diabetes self-management score of the Chinese patients was 3.4 ± 1.45. Patients with higher education, diabetes education, comorbidities, and online consultations had higher diabetes self-management scores (P < 0.05). Adherence to diabetes self-management in the normal glycaemic control group was higher than that in the substandard glycaemic control group (P< 0.05). Among all participants, 72.1% of the patients reduced the frequency of hospital visits, and 44.8% considered that they had diabetes-related stress during the pandemic. The mean anxiety level score rated by 286 patients was 5.3± 2.8.
Conclusion: The COVID-19 pandemic has affected diabetes self-management, including substandard glycemic control, increased diabetes-related stress, limited exercise range and medical visits. Therefore, future interventions should focus on the online management of chronic diseases and support online consultation’ development and promotion, which can overcome physical distance and provide personalized services conveniently.
Keywords: coronavirus disease 2019, diabetes self-management, online consultation, type 2 diabetes mellitus
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has affected countries across the globe and taken tens of thousands of lives, caused by a contagious coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. In the early stage of the outbreak, COVID-19 spread rapidly in all parts of China, causing different degrees of illness.1 A retrospective cohort study suggested that nearly half of the patients who suffered from the COVID-19 have comorbidity at the same time, including diabetes.2
Diabetes is a chronic disease, resulting from an impairment in insulin action or insulin secretion, and its prevalence is going up. Diagnosed according to the American Diabetes Association (ADA) criteria, the prevalence of diabetes among Chinese adults has risen to 12.8%.3 It has been reported that people with diabetes are more likely to be infected4 and reach the composite end-points5,6 because patients with diabetes have the problem of immunity decline,7 acting on phagocytosis, chemotaxis, the bactericidal activity of neutrophils and macrophages.8 However well-controlled blood glucose can improve the prognosis.6 According to the latest diabetes prevention and treatment guidelines issued by the National Diabetes Association, self-management education for patients with diabetes is the key to reducing the risk of acute and long-term complications.9 Self-management consists of adherence behaviors such as dietary changes, exercise, self-monitoring of blood glucose, regular self-medication and follow-up. Diabetes self-management in Chinese patients with T2DM is suboptimal. Studies have shown that the average score of diabetes self-management in Chinese people with T2DM was nearly half of the total possible score.10 With the spread of novel coronavirus continuously and rapidly, China has instituted some measures to achieve social distancing, which may lead to more unsatisfactory diabetes self-management. A study from Spain found that consumption of sugary foods and snacks increased and physical activity dropped significantly during the COVID-19 lockdown.11 But nearly half of all respondents from a Polish study stated that their diabetes self-management had significantly improved.12
The current situation of self-management of patients with diabetes during the pandemic lacks a relevant data and sufficient evidence in China. Therefore, we designed a questionnaire to determine how Chinese patients with diabetes coped and adjusted during the pandemic period.
Materials and Methods
Participants
The survey was conducted between in South China between July and September 2020. Trained interviewers in the clinic interviewed individual participants face-to-face. The inclusion criterion was that type 2 diabetes mellitus (T2DM) duration of not < 3 months. The exclusion criteria included psychiatric disorders with psychotic phenomena, language barriers, and a significant lack of vision or hearing. In addition, we evaluated the glycaemic control of patients based on the standards of medical care in diabetes.13,14 If the patient’s fasting plasma glucose (FPG) ranged from 3.9 to 7.0 mmol/L, postprandial plasma glucose (PPG) < 10.0 mmol/L and glycosylated haemoglobin (HbA1c) < 7%, we think that blood glucose level was well controlled. Moreover, hypoglycemia was defined as symptomatic or asymptomatic plasma glucose ≤ 3.9 mmol/L according to the ADA criteria.
The study protocol was approved by the Ethics Committee of Zhujiang Hospital, Southern Medical University, China. The survey was going on following the Declaration of Helsinki. All the participants provided informed consent.
Questionnaires
Questionnaires including demographic information, glycaemic control status, diabetes education, and the Summary of Diabetes Self-Care Activities (SDSCA) 15 were used. The SDSCA is a self-report questionnaire developed by Toobert et al to measure diabetes self-management behaviour. According to the actual situation of the Chinese people, we chose some questions from the SDSCA, translated them into Chinese, and used them to assess diabetes management during novel coronavirus outbreak. The demographic characteristics included age, gender, education level, and body mass index (BMI). Glycaemic control status was based on the HbA1c, FPG, and PPG levels. Medical records included the duration of diabetes, treatment regimen, complications, comorbidities, and blood pressure. Participants were asked if they experienced diabetes-related stress during the pandemic. If the answer is yes, the patient should rate the degree on a scale of 1 (slightly anxious) to 10 (strongly anxious).
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) software (version 26.0) was used to analyse the data. We used frequencies and percentages to summarise categorical variables. Continuous variables were described as mean and standard deviation (SD) or median and interquartile range, as appropriate. We divided patients into two groups based on their self-assessment of diabetes self-management. Chi-square test and independent samples t-test were used to test for significance. Single-factor analysis was used to compare the mean values of each group and evaluate whether there were significant differences.
Results
In total, 872 patients were eligible and agreed to participate in the study. The content validation index of the questionnaire was 0.748, and Cronbach’s alpha index was 0.708.
Demographic Characteristics
The demographic information of the participants is presented in Table 1. The median age of the participants was 58.0 years (interquartile range, 50–67 years), and 43.9% were female. Normal BMI was observed in 47.7% of the study cohort, overweight (33.6%), obesity (11.4%), and underweight (4.1%). Most patients had less than 12 years of education, and 130 patients (14.9%) had a university degree or above.
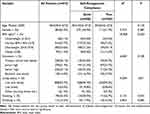 |
Table 1 The Demographic Information of the Study Patients |
Health and Diabetes-Related Variables of Study Participants
The median duration of diabetes mellitus was 7.0 years (interquartile range, 3.0 to 12.0) (Table 2). More than half (65.4%) of the participants reported that they already had complications from diabetes. Comorbidities such as hypertension, coronary heart disease, abnormal lipid metabolism, and gout were present in 73.5% of the respondents. Over half of the participants were giving a positive answer when asked whether their diabetes self-management had been ongoing at this particular time.
 |
Table 2 Health and Diabetes-Related Variables of Participants (n = 872) |
For glucose monitoring, approximately 85.0%, 62.7%, and 53.8% of the patients had FPG, PPG, and HbA1c records, respectively (Table 3). In terms of glycaemic control, the data showed that patients with FPG < 7.0 mmol/L (36.4%), PPG < 10.0 mmol/L (26.3%), or HbA1c < 7.0% (18.6%) in our investigation has well-controlled blood glucose level, and 11.9% of patients reported that they experienced blood glucose < 3.9 mmol/L during the outbreak. We believe that these patients had hypoglycemia. The remaining patients did not have their blood glucose recorded or not measured.
 |
Table 3 The Glycemic Control Status of Participants During the COVID-19 Pandemic. (n = 872) |
Impact of the COVID-19 Pandemic on Diabetes Self-Management
All participants reported four aspects of diabetes self-management within 7 days, including exercise, medication adherence, monitoring of complications, and blood glucose monitoring (Table 4). The final mean of diabetes self-management was 3.4 ± 1.3 per week. Medication adherence, which they did the best, was calculated with a mean score of 6.3 ± 1.7 per week. However, the mean score of self-examinations of diabetes-related complications was 1.6 ± 2.2 only.
 |
Table 4 Impact of Covid-19 Pandemic on Diabetic Self-Management (n=872) |
The COVID-19 pandemic has caused them to visit their physicians for routine clinical follow-ups. The majority of the patients (72.1%) reduced the frequency of hospital visits, while the remaining patients did not report any changes. In addition, 45.8% of the participants reported that they had consulted online, while 69.7% had consulted offline. Nearly half the participants (44.8%) considered that they had diabetes-related stress during the pandemic (Table 4). A total of 286 patients rated their anxiety levels on a scale of 1 (slightly anxious) to 10 (strongly anxious), and the mean score was 5.3 ± 2.8. Patients who self-perceived not having self-management during the outbreak had higher anxiety levels than those with self-management (6.0 versus 5.1).
Comparison of Diabetes Self-Management Between Different Variables
The effects of demographic factors and health risks on diabetes self-management are shown in Table 5. Patients with higher education levels had higher diabetes self-management scores than those with lower education levels (P < 0.001). Patients who received diabetes education and insisted on self-management had higher diabetes self-management scores than those who did not. The self-management scores of patients with comorbidities differed significantly from those without comorbidities (P < 0.05). Adherence to diabetes self-management was higher in the normal glycaemic control group than in the not-well glycemic control group (P < 0.05). Patients who had consulted online performed well in diabetes self-management (P < 0.05). No significant differences in BMI, complications, diabetes-related stress, or comorbidities were found.
 |
Table 5 Comparison of Self-Management Data Among Different Variables |
Discussion
This study was conducted to investigate diabetes self-management in patients with T2DM whose diabetes duration was no less than 3 months in China during the pandemic, demonstrating that the pandemic had a major impact on diabetes self-management. To reduce the risk of infection and transmission of COVID-19, social distancing, travel restrictions, stay-at-home guidance, and quarantine practices are required, which may worsen glycaemic control, reduce the frequency of exercise, change routine clinical follow-ups, and increase diabetes-related stress. A previous study interviewed 12 patients with T2DM during isolation in Wuhan, China, and found that they had barriers to diabetes self-management, including lack of resources and knowledge.16 The average score of diabetes self-management in Chinese people with T2DM during the pandemic was lower than before.10
According to this study, we found that glucose control was generally substandard during the COVID-19 pandemic. More than half of the patients’ FPG, PPG, and HbA1c were not up to the standard, which is similar to previous reports in Wuhan.17 It was well-known that glucose control was associated with diabetes management.18 Compared with patients with few self-management scores, patients with more self-management scores had better glycaemic control. However, among the 872 participants in this study, most had less overall practice in diabetes self-management, especially in complications and blood glucose monitoring, which is similar to previous studies.19
Owing to these official control measures for COVID-19, some patients with T2DM have experienced difficulty in diabetes self-management. Social quarantine and lockdowns had limited physical activity. This study showed that the mean score of the exercise was 3.4 ± 2.5 on a scale of 0 to 7 during the pandemic, which means exercise was inadequate and may lead to deterioration in glycaemic control. It is known that regular physical activity has significant physical and psychological benefits.20 More people reported that they preferred to take a walk near their home or exercise at home because of the limitation of activity scope. A brief survey published in a Polish study showed a statistically significant increase in the number of walks taken by patients with diabetes during this period.12 Therefore, during the outbreak, we can guide people with diabetes to perform appropriate exercises at home, such as walking and doing housework, or promote some simple and suitable exercise gymnastics that do not require too much space.
Adults with diabetes have reported significant changes in their healthcare. The number of patients with diabetes outpatient visits decreased in response to social distance guidance. Most of participants said they had reduced the number of visits to hospitals for fear of cross-infection, which would result in the hypoglycaemic regimen for patients with substandard glycaemic control not being adjusted in a timely manner. However, the shift in the medium of clinical consultation from face-to-face to online communication is surprising.
With smartphones prevailing in most households, online consultation has emerged which can help patients keep in contact with their routine physicians via mobile applications and web pages. As a result, care provided by diabetes-related professionals can be accessed more easily than face-to-face contact.21 Our study demonstrated that some of the respondents (45.8%) consulted online via WeChat Subscription, Doctor Ant, Baidu, Home of Diabetes, and other online platforms. Online consultations can help make it easier to access care without being exposed to the infection. First, online consultation can guide patients with diabetes to properly monitor their condition to emphasise the correct diet, exercise, and drugs. It can also help patients avoid fluctuations in blood glucose levels and prevent hypoglycaemia. A substantial number of patients lack education about the appropriate response to hyperglycaemia or hypoglycaemia. Previous studies have shown that diabetes apps can improve patients’ understanding of the disease and their ability to self-manage.22,23 Consistent with this finding, patients who consulted online had better glycaemic control and self-care behaviours in our study. In addition, mobile app-based consultation can reduce healthcare costs when patients care away from healthcare organizations.24 More importantly, online consultation provided comfort and peace of mind to anxious patients in this outbreak because the questions that make them anxious and helpless can be answered in time.
Although online consultation can overcome physical distance and provide timely physician care, it is still in its infancy and faces numerous challenges,25 including technological difficulties and lack of access to lab reports. The participants who refused to consult online in our survey explained that they were inexperienced in using the online platform and got used for traditional in-person visits. Therefore, broader access to digital health, and patient training, and simplifying procedures are the next priorities. Otherwise, the tool meant to bring convenience, will also become another burden.26 At the same time, although there are various applications for diabetes self-management, they have not been designed perfectly and tested rigorously; thus, both patients and clinicians do not have direct evidence to guide them in their choice. More importantly, device manufacturers are reluctant to interoperate with third-party devices because they do not want to risk losing their exclusivity.21
Previous studies have shown a significant increase in common and diabetes-related stress in adults with T2DM compared with pre-pandemic levels,27 associated with the emergence of the pandemic and not knowing how to make appropriate adjustments in time. The results of our study revealed that 44.8% of the participants reported the presence of diabetes-related stress during the pandemic. Similar to this study, diabetes-related stress may be related to the change in diabetes management in previous studies, affecting blood glucose control.28 It was reported that higher levels of depression are associated with decreased quality of life, unhealthy diets, and lack of physical activity.29 These aspects are also the influence by the novel coronavirus pandemic in our lives. Several reports have suggested that aggressive interventions should be undertaken, including increasing online consultation and establishing connections with the healthcare community.30
It is difficult to deny that something like the novel coronavirus will happen again. Furthermore, with the rise of diabetes prevalence, the diabetes community will increasingly face public health challenges in the following days,31 impacting the traditional diagnosis and treatment mode and chronic disease management model, such as the 2009 H1N1 pandemic32 and 2003 severe acute respiratory syndrome epidemic.33 Because of the new dawn that the diagnosis and treatment line has brought to chronic disease management during the pandemic, we think it is necessary to develop online consultation.
This study had some limitations that must be acknowledged. First, the sample size in the survey was large but only covered South China. In addition, no non-diabetes comparison group and adults with type 1 diabetes mellitus (T1DM) were included. As a result, it is not known whether patients with T2DM, T1DM, or patients without diabetes respond similarly to the pandemic. Another limitation was that this study was retrospective, therefore, some respondents could not recall the information they had to provide completely or accurately.
Conclusion
The novel COVID-2019 pandemic has impacted the self-management of patients with T2DM, including substandard glycemic control, limited exercise range and medical visits, and increased anxiety. We should not only adapt to it, but also seek a new management model. Online consultation can overcome distance limitations, increase physician-patient interaction, provide patients with health information, timely advice on improving health behaviors, and social and psychological support. Therefore, attention should be paid to the online management of chronic diseases and to support the development and promotion of online consultation.
Abbreviations
COVID-19, the coronavirus disease 2019; T2DM, type 2 diabetes mellitus; FPG, fasting plasma glucose; PPG, postprandial plasma glucose; HbA1c, glycosylated haemoglobin; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ADA, American Diabetes Association; SDSCA, summary of diabetes self-care activities; BMI, body mass index; SD, standard deviation; OAD, oral antidiabetic drug; GLP-1, glucagon-like peptide 1; BP, blood pressure.
Ethics Approval
Waiving to sign the informed consent will not adversely affect the rights and health of the participants. The privacy and personal information of the participants were protected. In this study, all patients were anonymised. The risk of the study to the participants was not greater than the minimum risk. The research protocol was approved by the Ethics Committee of Zhujiang Hospital, Southern Medical University, China (approval no. 2021-KY-177-01). The survey was in accordance with the Declaration of Helsinki. All the participants provided informed consent.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant NO: 81770804).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Guan WJ, Ni Z-Y, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi:10.1056/NEJMoa2002032
2. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi:10.1016/S0140-6736(20)30566-3
3. Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi:10.1136/bmj.m997
4. Kumar NP, Babu S. Influence of diabetes mellitus on immunity to human tuberculosis. Immunology. 2017;152:13–24. doi:10.1111/imm.12762
5. Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi:10.1183/13993003.00547-2020
6. Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–1077.e3. doi:10.1016/j.cmet.2020.04.021
7. Erener S. Diabetes, infection risk and COVID-19. Mol Metab. 2020;39:101044. doi:10.1016/j.molmet.2020.101044
8. Valerius NH, Eff C, Hansen NE, et al. Neutrophil and lymphocyte function in patients with diabetes mellitus. Acta Med Scand. 1982;211:463–467. doi:10.1111/j.0954-6820.1982.tb01983.x
9. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S13–S28. doi:10.2337/dc19-S002
10. Lin K, Park C, Li M, et al. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2017;131:179–186. doi:10.1016/j.diabres.2017.03.013
11. Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, et al. COVID-19 Lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020;12:2327. doi:10.3390/nu12082327
12. Grabia M, Markiewicz-Zukowska R, Puscion-Jakubik A, et al. The nutritional and health effects of the COVID-19 pandemic on patients with diabetes mellitus. Nutrients. 2020;12:3013. doi:10.3390/nu12103013
13. American Diabetes Association. Standards of medical care in diabetes-2020 abridged for primary care providers. Clin Diabetes. 2020;38(38):10–38. doi:10.2337/cd20-as01
14. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S14–S31. doi:10.2337/dc20-S002
15. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi:10.2337/diacare.23.7.943
16. Shi C, Zhu H, Liu J, Zhou J, Tang W. Barriers to self-management of type 2 diabetes during COVID-19 medical isolation: a qualitative study. Diabetes Metab Syndr Obes. 2020;13:3713–3725. doi:10.2147/DMSO.S268481
17. Zhou J, Tan J. Diabetes patients with COVID-19 need better blood glucose management in Wuhan, China. Metabolism. 2020;107:154216. doi:10.1016/j.metabol.2020.154216
18. Tao J, Gao L, Liu Q, et al. Factors contributing to glycemic control in diabetes mellitus patients complying with home quarantine during the coronavirus disease 2019 (COVID-19) epidemic. Diabetes Res Clin Pract. 2020;170:108514. doi:10.1016/j.diabres.2020.108514
19. AlQahtani AH, Alzahrani AS, Alzahrani SH, Alqahtani SM, AlOtaibi AF, Khan AA. Levels of practice and determinants of diabetes self-care in primary health care in Jeddah City, Saudi Arabia. Cureus. 2020;12:e8816. doi:10.7759/cureus.8816
20. Matias T, Dominski FH, Marks DF. Human needs in COVID-19 isolation. J Health Psychol. 2020;25:871–882. doi:10.1177/1359105320925149
21. Cafazzo JA. A digital-first model of diabetes care. Diabetes Technol Ther. 2019;21:S252–S258. doi:10.1089/dia.2019.0058
22. Kebede MM, Liedtke TP, Mollers T, Pischke CR. Characterizing active ingredients of ehealth interventions targeting persons with poorly controlled type 2 diabetes mellitus using the behavior change techniques taxonomy: scoping review. J Med Internet Res. 2017;19:e348. doi:10.2196/jmir.7135
23. Kebede MM, Pischke CR. Popular diabetes apps and the impact of diabetes app use on self-care behaviour: a survey among the digital community of persons with diabetes on social media. Front Endocrinol. 2019;10:135. doi:10.3389/fendo.2019.00135
24. Kitsiou S, Pare G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLoS One. 2017;12:e0173160. doi:10.1371/journal.pone.0173160
25. Iyengar V, Wolf A, Brown A, Close K. Challenges in diabetes care: can digital health help address them? Clin Diabetes. 2016;34:133–141. doi:10.2337/diaclin.34.3.133
26. Krebs P, Duncan DT. Health app use among us mobile phone owners: a national survey. JMIR Mhealth Uhealth. 2015;3:e101. doi:10.2196/mhealth.4924
27. Fisher L, Polonsky W, Asuni A, Jolly Y, Hessler D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: a national cohort study. J Diabetes Compl. 2020;34:107748. doi:10.1016/j.jdiacomp.2020.107748
28. Pandit AU, Bailey SC, Curtis LM, et al. Disease-related distress, self-care and clinical outcomes among low-income patients with diabetes. J Epidemiol Community Health. 2014;68:557–564. doi:10.1136/jech-2013-203063
29. Joensen LE, Tapager I, Willaing I. Diabetes distress in Type 1 diabetes–a new measurement fit for purpose. Diabet Med. 2013;30:1132–1139. doi:10.1111/dme.12241
30. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–357. doi:10.1037/hea0000875
31. Hill MA, Mantzoros C, Sowers JR. Commentary: COVID-19 in patients with diabetes. Metabolism. 2020;107:154217. doi:10.1016/j.metabol.2020.154217
32. Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care. 2010;33:1491–1493. doi:10.2337/dc09-2215
33. Yang JK, Feng Y, Yuan MY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006;23:623–628. doi:10.1111/j.1464-5491.2006.01861.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
