Back to Journals » International Journal of General Medicine » Volume 15
Association of Sleep, Body Weight and Physical Exercise with Plasma BDNF Levels in Healthy Male Saudi Smokers
Authors Al-Mshari A, AlSheikh MH , Latif R , Mumtaz S, Albaker W, Al-Hariri M
Received 8 June 2022
Accepted for publication 8 August 2022
Published 17 August 2022 Volume 2022:15 Pages 6603—6610
DOI https://doi.org/10.2147/IJGM.S377744
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Arwa Al-Mshari,1 Mona Hmoud AlSheikh,1 Rabia Latif,1 Sadaf Mumtaz,2 Waleed Albaker,3 Mohammed Al-Hariri1
1Physiology Department, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2Department of Physiology, Dental College, HITEC-Institute of Medical Sciences Taxilla Rawalpindi, Rawalpindi, Pakistan; 3Department of Internal Medicine, College of Medicine, Imam Abdulrahman Bin Faisal, Dammam, Saudi Arabia
Correspondence: Mohammed Al-Hariri, Email [email protected]
Introduction: Brain-derived neurotrophic factor (BDNF) has been shown to impact neural function and development. The BDNF plasma levels may be affected by a smoker’s behavior. Thus, the aim of this study was to investigate the association between sleep, body weight and physical exercise with brain-derived neurotrophic factor (BDNF) in healthy male Saudi smokers.
Methods: A cross-sectional study, with a convenience sample, was conducted during personal visits to the Anti-Smoking Clinic and Family and Community Medical Center of Imam Abdurrahman Bin Faisal University (IAU) in Dammam at the end of 2018. Blood samples were taken from participants to measure the BDNF plasma levels. Multiple linear regression analysis was used to examine the relationship between plasma BDNF levels and participants’ background characteristics, such as smoking index, physical activity, body mass index (BMI) and Pittsburgh sleep quality index (PSQI).
Results: A sample of 73 (31 smokers and 42 non-smokers) males took part in the study. The results demonstrated a significant relationship between plasma BDNF levels with physical activity, smoking age, smoking index, PSQI and BMI 25– 29.9 (overweight). However, the results showed no significant relationship between plasma BDNF levels and BMI (healthy weight) and obesity.
Conclusion: This study shows that physical activity and sleeping quality can provide a positive impact against smoking-associated variation of the BDNF plasma levels, which may affect the health of Saudi males. Further investigation is needed to understand what other potential background characteristics are best predictive or correlated with BDNF plasma levels.
Keywords: smokers, BDNF, PSQI, IPAQ, smoking index, physical activity, body mass index
Introduction
The brain-derived neurotrophic factor (BDNF) is a small dimeric protein and a member of the neurotrophin family of growth factors.1 It is one of the neurotrophins family that plays a critical role in survival and differentiation of neurons throughout their development.2 Another main function of BDNF is to sustain high levels of repair in adults’ brains.3 Evidence has suggested that BDNF regulating the synaptic plasticity and survival as well as cell proliferation.4,5 In addition, BDNF also plays an essential role in the cellular model of memory and learning, which includes both long-term potentiation (LTP) and late-phase LTP in hippocampal neurons.2
The BDNF plasma levels may also be affected by smoking and heavy abuse of nicotine.6 Furthermore, BDNF upregulation might be related to the duration and amount of smoking.7
Cigarette smoking imposes a huge health and economic burden. It kills around seven million people every year.8 The number of deaths is expected to reach 8.3 million by 2030. The prevalence of cigarette smoking remains high worldwide, as 20% of the world population are tobacco smokers. In Saudi Arabia, the prevalence of tobacco smokers among adults (≥15 years) in 2013 was 16%. According to the World Health Organization (WHO) global report on the trends of tobacco smoking in 2015, “the prevalence of tobacco smoking in Saudi Arabia is projected to increase to 24% by 2025”.9
Smoking has many hazardous compounds that are known to be highly toxic to the nervous system, where smoking primarily acts in the mesolimbic system (dopaminergic neurons) leading to release of dopamine, which is responsible for pleasure and euphoria feelings as well as considered the principal factor of addiction.10 In the same line, smoking may induce cognitive impairment through impairing other body systems.11
The exact relationship between smoking status to plasma BDNF levels remains controversial.12 According to published evidence, a functional variant of the BDNF human genome (polymorphism modifying) is highly related to smoking behavior13 and the age of smoking initiation.14
Furthermore, most studies that screened plasma BDNF and smoking were conducted on middle-aged and/or elderly participants and are compounded by the comorbidities of these subjects; therefore, there is a lack of studies conducted on young individuals to examine this relationship. More importantly, documented data confirm the diversity in BDNF levels among populations.15,16
To the best of our knowledge, very few studies have evaluated the influential effect of lifestyle factors on the plasma BDNF levels in healthy young smokers, especially in Saudi Arabia. In addition, since smoking is more common in males than females in Saudi Arabia and due to differences in smoking behaviors, as well as cyclic changes of BDNF levels in females.17 Thus, it would be interesting to explore the association between sleep, body weight and physical exercise with plasma BDNF levels in healthy young male Saudi smokers.
Materials and Methods
Participants
A cross-sectional study, with a convenience sample, was conducted during personal visits to the Anti-Smoking Clinic and Family and Community Medical Center of Imam Abdurrahman Bin Faisal University (IAU) in Dammam, Saudi Arabia at the end of 2018. The subjects were intentionally selected as young smokers to avoid any confounding effects on sleep due to aging.
Inclusion criteria were young healthy male subjects with a previous history of smoking at least one or more cigarettes per day over the previous six months. The study excluded participants with chronic and psychiatric disorders, or electronic cigarette users, along with alcoholics and those who had previously used drugs, such as heroin, cocaine and cannabis; they were excluded through structured survey items that elicited the health status of participants.
The nonsmokers were recruited from the Family and Community Medicine University Center in Dammam, Saudi Arabia and were matched for age and gender.
All participants filled out three questionnaires: “self-made questionnaire (includes questions related to smoking, health and socioeconomic status of the participant), Pittsburgh Sleep Quality Index (PSQI) and the short form of International Physical Activity Questionnaire. (IPAQ)”.
Dependent Variable (Outcome)
Plasma BDNF Measurements
Blood samples were collected early morning between 10 and 12 a.m. from all participants. Measurements of plasma BDNF concentrations were carried out in the biochemistry lab at IAU college of medicine, by using human BDNF sandwich ELISA kits (Aviva systems biology, OKBB00127, ELISA kits, USA), according to the manufacturer’s instructions. This assay has high sensitivity (<15 pg/mL) and an excellent specificity (<11.3 pg/mL) for detection of plasma BDNF.
Explanatory (Independent) Variables in the Study
Smoking Index
Smoking index is a parameter that measures the cumulative exposure to smoking.18 In other words, smoking index is the average number of cigarettes smoked during a day.
Physical Activity
The purpose of using this questionnaire was to measure the amount of physical activity of the participants as it can influence plasma BDNF level.19 IPAQ has been developed and tested for use in adults aged 15–69 years. The reliability of the IPAQ short, self-administered version is 0.75, and the validity is 0.30.20
IPAQ total score is determined by summing up the scores of the three types of physical activity, which were calculated by using the following formulae: Walking MET-minutes/week = 3.3 * walking minutes * walking days; moderate MET-minutes/week = 4.0 * moderate-intensity activity minutes * moderate days; vigorous MET-minutes/week = 8.0 * vigorous-intensity activity minutes * vigorous-intensity days.
Pittsburgh Sleep Quality Index (PSQI)
PSQI is an instrument that measures the pattern and quality of sleep-in elderly people. In general, PSQI differentiates between bad and good sleepers through measuring seven dimensions: habitual sleep efficiency, sleep duration, subjective sleep quality, sleep latency, daytime dysfunction, use of sleep medications and sleep disturbances. PSQI total score is determined by summing up the 7 components’ scores to get a global score that ranges from 0 to 21, with higher scores denoting poorer sleep quality. The original authors set up a cutoff of >5 for the global score to distinguish poor sleepers (>5) from good sleepers (<5). PSQI consists of 19 self-rated questions.21
Body Mass Index (BMI)
The role BMI is to measure individuals’ weights adjusted for height and age. BMI is regarded as an indicator of the fat present in the body. In other words, BMI is an alternative measure of the fat in the body and excess weight. All participants were classified according to their BMI to “underweight (BMI < 18.5), normal (BMI = 18.5–24.9), overweight (BMI = 25–29.9), or obese (BMI ≥ 30)”.22
Ethical Considerations
The study protocol has been approved by the local ethical committee in IAU (IRB-PGS-2018-01-033) and complies with the Declaration of Helsinki. All participants have signed an informed consent provided with an introductory letter that has taken into account the confidentiality of data prior to the study.
Statistical Analysis
The collected data were entered to Statistical Package for Social Sciences version (26) SPSS. Cross-tabulation and frequency tables were used to explore the data in terms of missing values and outliers. The correlation among the independent variables was conducted to examine multicollinearity. The results found no collinearity, and all variables were entered to the model. The normal distribution of the outcome variable was tested using the one-sample Kolmogorov–Smirnov test and Q-Q plots, and the results showed the outcome variable was normally distributed since the p-value is greater than 0.05 (p=0.072>0.05).
Multiple linear regression was employed in this empirical study to develop a predictive model for plasma BDNF level among smokers and non-smokers. Multiple linear regression is widely used in assessing relationships between single outcome variable (plasma BDNF levels) and many explanatory variables (independent variables). This type of inferential statistical methods establishes the relative contribution of each independent variable in the regression model and its effect on the dependent variable.
Dummy Variables
Simple and multiple linear regressions allow researchers to include categorical variables (predictors) in the model, but these variables should be transformed to dummy variables that take “1” and “0” values. The value “1” shows that the attribute of the category is present, while the value of “0” shows that the value of attribute of the category is absent. In this study, six categorical variables were transformed into dummy variables. For example, the variable “smoking age 12–17 year” was given the value “0” and “smoking age 18–24 years” was given the value “1”. In the multiple regression equation, the dummy variable coefficient indicated how the “smoking age 18–24” with value “1” affects the plasma BDNF levels (dependent variable) in reference to “smoking age 12–17 year” was given the value “0”.
Results
Features of Participants
A sample of 73 participants (31 smokers and 42 non-smokers) were involved in the present study (Figure 1). The sample size was calculated using G-power 3.34 software. The calculation was based on three components: effect size, level of significance (0.05) and power (0.90). The effect size used was 0.3, where the effect size measures the distance between the null hypothesis (H0) and alternative hypothesis (H1).
 |
Figure 1 Distribution of participants. |
Table 1 presents the features characteristics and plasma BDNF levels among smokers and non-smokers who participated in the study. The mean age of smokers was significantly higher (24.7±4.1 years) compared to the non-smokers (20.9 ±2.7 years). The results demonstrate significant differences between smokers and non-smokers in relation to plasma BDNF levels (t=2.011, p=0.048<0.05). Nonetheless, the results showed that no significant differences between smokers and non-smokers in relation to BMI (mean = 26.71 and 24.55, respectively), physical activity (2749 and 2039, respectively) and PSQI (5.77 and 4.88, respectively) (p > 0.05).
 |
Table 1 Baseline Features of the Study Sample According to Smoking Status |
The smoking history of participants is shown in Figure 2. The mean age of smoking initiation was 17.2±4 along with 1.13±0.2 for smoking index. The mean duration of smoking was 7.3±5 years, and the mean number of cigarettes/days was 14.8 ± 9.2.
 |
Figure 2 Number of cigarettes/days, smoking starting age, smoking index and duration of smoking (years) among the smokers group. |
In order to investigate the association between sleep, body weight and physical exercise with plasma BDNF levels among the smoker’s group, a multiple regression model analysis was run. The overall model fit was (F(10) < 2.6, p < 0.002)), with an R2 of 0.75 (Table 2), and the results show that participants whose smoking age began between 18 and 24 years had higher plasma levels of BDNF than participants whose starting age of smoking was 12–17 years (0.606+0.208=0.814, t = 5.526, p=0.000). Regarding smoking age, the results demonstrated a significant relationship with plasma BDNF levels (0.606+0.081=0.686, t = 2.129, p=0.047).
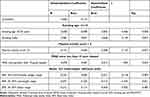 |
Table 2 Relationship Between Participants’ Background Characteristics and BDNF Plasma Levels |
Regarding physical activity, the results indicate that participants who walk more than 4 MET-minutes (<4) per week (moderate intensity) had higher BDNF levels than their counterparts (the reference category) who walk less 4 MET-minutes per week (0.606+0.131=0.737, t = 2.127, p=0.03) as presented in Table 2.
Furthermore, our results show that participants with good sleepers (less than 5 PSQI) had higher plasma BDNF levels than their counterparts whose sleep is poor (more than 5 PSQI) (0.606+0.078=0.684, t = 1.992, p=0.043).
The results also indicate a negative insignificant relationship between BMI and plasma BDNF levels in general and underweight (below 18.5 pg/mL) participants have BDNF (B = 0.606). Nonetheless, the results demonstrate weak significant negative association between overweight (25–29.9 pg/mL) participants and plasma BDNF levels (0.606–0.071=0.535, t=−2.375, p=0.021). This result suggests that the increase in BMI leads to a decrease in plasma BDNF levels (Table 2).
Discussion
The current study demonstrated significant differences between smokers and non-smokers in relation to plasma BDNF levels, since these levels were found higher in smokers than in non-smokers. These results are in line with other studies that argued that plasma BDNF levels were higher in smokers than in non-smokers.13,23 Higher plasma levels of BDNF in smokers are proportional to the number of cigarettes consumed. In other words, usage of cigarettes leads to increase the plasma levels of BDNF. This, in fact, is attributed to what is so called the stimulus dependence scenario and contributes to rearrangement of mesolimbic synaptic connections used in retaining the habit of smoking.6 Furthermore, de Arbol et al argued that high levels of cortisol among heavy smokers contributed to increased levels of BDNF.24 Additionally, Zhang et al argued that negative symptoms in smokers correlate with nicotine-induced upregulation of BDNF.14
Importantly, there are other influential factors that may affect the plasma BDNF levels in smokers that should be accounted. In relation to physical activity, the results of this study showed a significant association between the plasma BDNF levels and practicing physical activities in smokers. These results are in line with another report that demonstrated a significant correlation between plasma BDNF and physical activity.25 There are several studies that emphasize these results which argued that physical activity is beneficial for cognitive functioning (ie, functional recovery and physical health in general).26,27 In general, plasma BDNF level is sensitive to exercise mode and duration. A 30-minute open-skills exercise stimulates relatively more BDNF production. This finding implies that exercise mode might be a modality factor for the relationship between exercise and plasma BDNF levels among smokers. In contrast, another study found no significant relationship between plasma BDNF levels and physical activity and BMI.15 This may explain the fact of gene variations among populations.16
Our data showed that participants classified as good sleepers have higher plasma levels of BDNF than participants who were classified as “poor sleepers”. Biologically, plasma BDNF levels are associated with the number of sleeping hours because BDNF is affected by brain tissues, which are regarded as the main contributor of circulating BDNF.28 Furthermore, reported evidence showed that plasma BDNF levels were found to be significantly related to sleep patterns on weekends.29 BDNF levels were found to be negatively correlated with severity of insomnia. This correlation might be explained by the hypothesis that chronic insomnia might induce over activation of systemic inflammation and hypothalamus pituitary axis, which in the long-term decreases BDNF levels.30 Furthermore, chronic activation of the hypothalamus pituitary axis leads to increased secretion of glucocorticoid, which also affect the BDNF function.31 Along these lines, systemic inflammation could induce a significant decrease in the expression of brain BDNF.32 Therefore, BDNF was suggested to be a biomarker for insomnia.33
As mentioned in the results section, the results of multiple regression demonstrated a non-significant negative relationship between plasma levels of BDNF and BMI. These results suggest that BMI is not a good predictor of plasma BDNF levels. These results are consistent with the previous meta-analysis and systematic review conducted by Sandrini et al, who found no significant association between plasma BDNF levels and obesity.34
Limitation
First, the present study was a small cross-sectional. Second, we could not determine a causal relationship. These limit the generalizability of our findings.
Conclusions
This study model implies that physical activity and sleeping quality can provide a positive impact against smoking-associated variation of BDNF plasma levels, which may affect the health of Saudi males. Moreover, a large-scale longitudinal study targeting female participants may be required to illustrate the mechanisms responsible for the elevation of BDNF, as well as to understand what other potential background characteristics are best predictive or correlated with BDNF levels.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Acknowledgment
The authors are thankful to the participants in this research and the Deanship of Scientific Research, who supported this work.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work and that there is no conflict of interest regarding the publication of this article.
References
1. Neves CDC, Lacerda ACR, Lima LP, et al. Different levels of brain-derived neurotrophic factor and cortisol in healthy heavy smokers. Braz J Med Biol Res. 2017;50(12). doi:10.1590/1414-431x20176424
2. Colucci-D’Amato L, Speranza L, Volpicelli F. Neurotrophic factor BDNF, physiological functions and therapeutic potential in depression, neurodegeneration and brain cancer. Int J Mol Sci. 2020;21(20):7777. doi:10.3390/ijms21207777
3. Tyler WJ, Perrett SP, Pozzo-Miller LD. The role of neurotrophins in neurotransmitter release. Neuroscientist. 2002;8(6):524–531. doi:10.1177/1073858402238511
4. Vilar M, Mira H. Regulation of neurogenesis by neurotrophins during adulthood: expected and unexpected roles. Front Neurosci. 2016;9(10):26.
5. Garraway SM, Huie JR. Spinal plasticity and behavior: BDNF-induced neuromodulation in uninjured and injured spinal cord. Neural Plast. 2016;2016:9857201. doi:10.1155/2016/9857201
6. Kenny PJ, File SE, Rattray M. Acute nicotine decreases, and chronic nicotine increases the expression of brain-derived neurotrophic factor mRNA in rat hippocampus. Brain Res Mol Brain Res. 2000;85(1–2):234–238. doi:10.1016/S0169-328X(00)00246-1
7. Beuten J, Ma JZ, Payne TJ, et al. Significant association of BDNF haplotypes in European-American male smokers but not in European-American female or African-American smokers. Am J Med Genet B Neuropsychiatr Genet. 2005;139(1):73–80. doi:10.1002/ajmg.b.30231
8. World Health Organization. Tobacco [internet]; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/tobacco.
9. World Health Organization. WHO Global Report on Trends in Prevalence of Tobacco Use 2000–2025.
10. Pomerleau CS, Pomerleau OF. Euphoriant effects of nicotine in smokers. Psychopharmacology. 1992;108(4):460–465. doi:10.1007/BF02247422
11. Emery CF, Finkel D, Pedersen NL. Pulmonary function as a cause of cognitive aging. Psychol Sci. 2012;23(9):1024–1032. doi:10.1177/0956797612439422
12. Bhang SY, Choi SW, Ahn JH. Changes in plasma brain-derived neurotrophic factor levels in smokers after smoking cessation. Neurosci Lett. 2010;468(1):7–11. doi:10.1016/j.neulet.2009.10.046
13. Breetvelt EJ, Numans ME, Aukes MF, et al. The association of the alpha-5 subunit of the nicotinic acetylcholine receptor gene and the brain-derived neurotrophic factor gene with different aspects of smoking behavior. Psychiatr Genet. 2012;22(2):96–98. doi:10.1097/YPG.0b013e32834c0c75
14. Zhang XY, Xiu MH, Chen DC, et al. Nicotine dependence and serum BDNF levels in male patients with schizophrenia. Psychopharmacology. 2010;212(3):301–307. doi:10.1007/s00213-010-1956-y
15. Fonseca-Portilla R, Krell-Roesch J, Shaibi GQ, et al. Brain-derived neurotrophic factor and its associations with metabolism and physical activity in a latino sample. Metab Syndr Relat Disord. 2019;17(2):75–80. doi:10.1089/met.2018.0028
16. Petryshen TL, Sabeti PC, Aldinger KA, et al. Population genetic study of the brain-derived neurotrophic factor (BDNF) gene. Mol Psychiatry. 2010;15(8):810–815. doi:10.1038/mp.2009.24
17. Alotaibi SA, Alsuliman MA, Durgampudi PK. Smoking tobacco prevalence among college students in the Kingdom of Saudi Arabia: systematic review and meta-analysis. Tob Induc Dis. 2019;17. doi:10.18332/tid/105843
18. Jindal SK, Malik SK. Smoking index-a measure to quantify cumulative smoking exposure. Lung India. 1988;6(4):195–196.
19. Steves CJ, Mehta MM, Jackson SHD, Spector TD. Kicking back cognitive ageing: leg power predicts cognitive ageing after ten years in older female twins. GER. 2016;62(2):138–149.
20. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi:10.1249/01.MSS.0000078924.61453.FB
21. Farah NM, Saw Yee T, Mohd Rasdi HF. Self-reported sleep quality using the Malay version of the Pittsburgh Sleep Quality Index (PSQI-M) in Malaysian Adults. Int J Environ Res Public Health. 2019;16(23):E4750. doi:10.3390/ijerph16234750
22. Albaker W, El-Ashker S, Baraka MA, El-Tanahi N, Ahsan M, Al-Hariri M. Adiposity and cardiometabolic risk assessment among University Students in Saudi Arabia. Sci Prog. 2021;104(1):36850421998532. doi:10.1177/0036850421998532
23. Kim TS, Kim DJ, Lee H, Kim YK. Increased plasma brain-derived neurotrophic factor levels in chronic smokers following unaided smoking cessation. Neurosci Lett. 2007;423(1):53–57. doi:10.1016/j.neulet.2007.05.064
24. Del Arbol JL, Muñoz JR, Ojeda L, et al. Plasma concentrations of beta-endorphin in smokers who consume different numbers of cigarettes per day. Pharmacol Biochem Behav. 2000;67(1):25–28. doi:10.1016/S0091-3057(00)00291-4
25. Aas M, Djurovic S, Ueland T, et al. The relationship between physical activity, clinical and cognitive characteristics and BDNF mRNA levels in patients with severe mental disorders. World J Biol Psychiatry. 2019;20(7):567–576. doi:10.1080/15622975.2018.1557345
26. Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45(7):1343–1361. doi:10.1017/S0033291714003110
27. Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77:42–51. doi:10.1016/j.jpsychires.2016.02.023
28. Nishichi R, Nufuji Y, Washio M, Kumagai S. Serum brain-derived neurotrophic factor levels are associated with dyssomnia in females, but not males, among Japanese workers. J Clin Sleep Med. 2013;9(7):649–654. doi:10.5664/jcsm.2828
29. Saitoh K, Furihata R, Kaneko Y, Suzuki M, Takahashi S, Uchiyama M. Association of serum BDNF levels and the BDNF Val66Met polymorphism with the sleep pattern in healthy young adults. PLoS One. 2018;13(6):e0199765. doi:10.1371/journal.pone.0199765
30. Schmitt K, Holsboer-Trachsler E, Eckert A. BDNF in sleep, insomnia, and sleep deprivation. Ann Med. 2016;48(1–2):42–51. doi:10.3109/07853890.2015.1131327
31. Vgontzas AN, Bixler EO, Lin HM, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001;86(8):3787–3794. doi:10.1210/jcem.86.8.7778
32. Fernandez-Mendoza J, Baker JH, Vgontzas AN, Gaines J, Liao D, Bixler EO. Insomnia symptoms with objective short sleep duration are associated with systemic inflammation in adolescents. Brain Behav Immun. 2017;61:110–116. doi:10.1016/j.bbi.2016.12.026
33. Giese M, Unternährer E, Hüttig H, et al. BDNF: an indicator of insomnia? Mol Psychiatry. 2014;19(2):151–152. doi:10.1038/mp.2013.10
34. Sandrini L, Di Minno A, Amadio P, Ieraci A, Tremoli E, Barbieri SS. Association between obesity and circulating Brain-Derived Neurotrophic Factor (BDNF) levels: systematic review of literature and meta-analysis. Int J Mol Sci. 2018;19(8):2281. doi:10.3390/ijms19082281
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
