Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Association of Serum Fibroblast Growth Factor 23 Levels with the Presence and Severity of Hepatic Steatosis Is Independent of Sleep Duration in Patients with Diabetes
Authors Hu X, Yang L, Yu W, Pan W, Chen X, Li Q, Zhou J, Gu X
Received 6 December 2019
Accepted for publication 1 February 2020
Published 16 April 2020 Volume 2020:13 Pages 1171—1178
DOI https://doi.org/10.2147/DMSO.S241348
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ming-Hui Zou
Xiang Hu, Lijuan Yang, Weihui Yu, Wei Pan, Xueqin Chen, Qianqian Li, Jingzong Zhou, Xuejiang Gu
Department of Endocrine and Metabolic Diseases, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China
Correspondence: Xuejiang Gu
Department of Endocrine and Metabolic Diseases, The First Affiliated Hospital of Wenzhou Medical University, Ouhai District, Wenzhou 325000, Zhejiang Province, People’s Republic of China
Tel/Fax +86 577 5557 9381
Email [email protected]
Purpose: Fibroblast growth factor (FGF) 23 is currently recognized to be involved in the occurrence and development of metabolic diseases. The present study aimed to investigate the association between serum FGF23 levels and hepatic steatosis, as well as the influence of sleep duration.
Patients and Methods: The present study population was selected from patients with diagnosed diabetes hospitalized during February 2018 to April 2019. Serum FGF23 levels were assessed by two-side sandwich enzyme-linked immunosorbent assay. The presence and severity of hepatic steatosis were determined by controlled attenuation parameter (CAP). Hepatic steatosis was determined as CAP≥ 302 dB/m.
Results: Serum FGF23 levels were significantly higher in individuals with hepatic steatosis than in those without hepatic steatosis (P=0.004). The present study population was divided into Q1–Q4 according to serum FGF23 quartiles. The risks of hepatic steatosis were increased more than 3 folds in Q2–Q4 (all P< 0.01) compared to Q1. CAP showed an uptrend from Q1 to Q4 (P=0.005), even after adjustment for gender and age (P=0.001). Multivariate variance analyses showed significant differences in CAP among Q1–Q4 (P=0.008) and between individuals with short and long sleep duration (P=0.023), which were independent of each other. Serum FGF23 levels were positively associated with CAP independent of gender, age, total metabolic traits, and sleep duration (P=0.042).
Conclusion: Serum FGF23 levels were independently and positively associated with the severity of hepatic steatosis. The associations of serum FGF23 levels and sleep duration with hepatic steatosis were independent of each other.
Keywords: fibroblast growth factor 23, hepatic steatosis, controlled attenuation parameter, sleep duration
Introduction
Non-alcoholic fatty liver disease (NAFLD), emerging as the most common chronic liver disease, is present in nearly a quarter of the population worldwide. In China, the prevalence of NAFLD has been on a rising trend in the past two decades, leading to a threat to citizens’ health and a health burden to society.1 As an adverse outcome of ectopic fat deposition in the liver, NAFLD is always concomitant with metabolic and cardiovascular diseases, such as obesity, diabetes, hyperlipidemia, hypertension, and atherosclerosis, and even contributes to the onset and progression of these diseases.2,3 The complex interplay between multiple environmental factors, metabolic “hits”, and genetic predispositions leads to the development of necroinflammation and fibrosis in the liver, which progressed to NAFLD.4
Fibroblast growth factor (FGF) 23, mainly expressed in osteocytes and osteoblasts in bone, binds to FGF receptors with the cofactor, αklotho, to initiate downstream signaling events and thus functions as a circulating endocrine factor.5 When klotho is absent, although with low affinity, it is possible to activate FGF receptors in the presence of high FGF23 levels.6 Traditionally regarded as a link between bone and the kidney to regulate mineral homeostasis, FGF23 is currently recognized to play an important role in the occurrence and development of metabolic and cardiovascular diseases, including obesity, diabetes, and atherosclerosis.6–8 Previous basic animal research suggested that FGF23 could be involved in insulin resistance, oxidative stress, apoptosis, inflammatory reaction, and ectopic fat deposition in the liver through the inflammatory pathways.9,10 Additionally, clinical studies reported that FGF23 was associated with not only the visceral fat accumulation,11 but also the presence and severity of NAFLD.12
NAFLD encompasses a wide range of liver diseases, usually progressing from fairly benign forms such as isolated steatosis to steatosis with inflammation and necrosis, and eventually cirrhosis and/or hepatocellular carcinoma.13 The presence of diabetes, a key factor for the development of NAFLD, has been associated with a faster progression of NAFLD and advanced fibrosis. Diabetes predisposes individuals to develop NAFLD with faster progression and more severe forms.13 Controlled attenuation parameter (CAP), a novel non-invasive parameter to assess hepatic steatosis quantitatively, is established based on the properties of ultrasonic signals acquired by the vibration-controlled transient elastography device (Fibroscan). Being able to detect and quantify hepatic steatosis accurately, CAP can identify NAFLD in the earlier stage with higher sensitivity.14–16 Therefore, the present study recruited patients with diabetes and used CAP to evaluate hepatic steatosis, aiming to investigate the association between serum FGF23 levels and hepatic steatosis. Furthermore, in consideration that circadian misalignment would induce unbalanced activity of the sympathetic–parasympathetic branches between organs, which provides the conditions for the development and progression of NAFLD, the present study further explored the influence of sleep duration on the association between NAFLD and serum FGF23 levels.
Materials and Methods
Subjects
The present study population was selected from patients with diagnosed diabetes hospitalized in the Department of Endocrine and Metabolic Diseases, the First Affiliated Hospital of Wenzhou Medical University, during February 2018 to April 2019. Candidate subjects were excluded before enrollment if they had acute or chronic viral hepatitis, drug-induced liver diseases, alcoholism (a total of ≥140 g per week by a male adult or a total of ≥70 g per week by a female17), autoimmune liver disease, liver cirrhosis, renal failure, thyroid dysfunction, acute infection, severe cardiovascular diseases, severe cerebrovascular diseases, malignant tumor, psychiatric disease, and current treatment with systemic corticosteroids.
The participants finished a standardized questionnaire to gather information on their disease history, medication usage, family history, and living habits.
The present study was carried out in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the First Affiliated Hospital of Wenzhou Medical University. All subjects provided written informed consent before their participation in the study.
Anthropometric Measurements
Every participant underwent a physical examination adhering to the standard protocols by trained physicians, which included anthropometric measurements (body height, weight, waist and hip circumferences) and blood pressure (BP). Body weight and height are measured to calculate body mass index (BMI) as follows: BMI=weight (kg)/height2 (m2). Waist circumference was measured at the horizontal plane between the lowest rib and the iliac crest on the midaxillary line. Waist–hip ratio (WHR) was calculated as waist circumference divided by hip circumference. Systolic BP (SBP) and diastolic BP (DBP) were assessed with a mercury sphygmomanometer in triplicate with a 3-min interval after 10 min of rest. Mean arterial pressure (MAP) was calculated as follows: MAP=DBP+1/3(SBP–DBP).
Laboratory Measurements
Standard laboratory measurements were performed. Venous blood was drawn in the morning after a 10-h overnight fast and used to measure fasting plasma glucose (FPG), glycated hemoglobin A1c (HbA1c), triglyceride (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), and serum FGF23 levels. Serum FGF23 levels were determined by two-side sandwich enzyme-linked immunosorbent assay using the Kainos kit (Kainos Laboratories Inc., Tokyo, Japan). The inter- and intra-assay coefficients of variations were 2.1–3.8% and 2.0–3.0%, respectively.
Fibroscan Examination
CAP measurements were detected by transient elastography device (Fibroscan: Echosens, Paris, France), conducted by experienced technicians. The assessments were carried out on the right lobe of the liver through the intercostal space on patients lying in the dorsal decubitus position with the right arm in maximal abduction. Ten successful acquisitions were obtained from each patient with the 3.5-MHz standard M probe at a depth of 25–65 mm, of which the median value was used for analysis. Details of the measurements have been previously described.18 Hepatic steatosis was determined as CAP≥302 dB/m.19
Statistical Analysis
The statistical analyses were performed with the statistical software package version 16.0 (SPSS Inc., Chicago, IL, USA). The normality of data distribution was determined by one-sample Kolmogorov–Smirnov test. Continuous variables were expressed as mean±standard deviation or median with interquartile range according to their distribution (normal or skewed). Comparison between the two groups was conducted by an unpaired Student’s t-test and Mann–Whitney U-test. Variance analyses were carried out to explore the correlation between the serum FGF23 quartiles and CAP, as well as the influence of sleep duration. Logistic regression analyses were performed to determine the association between serum FGF23 quartiles and the presence of hepatic steatosis. Multiple stepwise linear regression analyses were conducted to determine the association between serum FGF23 levels and CAP. All reported Pvalues were two-tailed, and P<0.05 was considered statistically significant.
Results
Clinical Characteristics of the Study Participants
A total of 296 individuals with an average age of 54.63±10.97 years (age range: 22.98–74.97 years) were enrolled in the present study, including 209 individuals without hepatic steatosis and 87 individuals with hepatic steatosis. Serum FGF23 levels were significantly higher in individuals with hepatic steatosis than in those without hepatic steatosis (41.60 [35.73–55.09] pg/mL versus 38.08 [30.20–51.16] pg/mL, P=0.004). In addition, compared to those without hepatic steatosis, participants with hepatic steatosis exhibited higher levels of BMI, WHR, SBP, DBP, MAP, and TG, but lower levels of HDL-c (all P<0.001, except P=0.001 for DBP). Other variables did not differ between these two groups (all P>0.05; Table 1).
 |
Table 1 Characteristics of the Study Participants |
The Presence and Severity of Hepatic Steatosis Among Serum FGF23 Quartiles
The present study population was further divided into four subgroups according to serum FGF23 quartiles (serum FGF23 levels: Q1: ≤32.05 pg/mL, Q2: 32.06–39.68 pg/mL, Q3: 39.67–51.72 pg/mL, Q4: >51.72 pg/mL). Adjusted for gender and age, the risks of hepatic steatosis were increased more than 3 folds in Q2 (odds ratio [OR]=3.462, P=0.003), Q3 (OR=3.716, P=0.002), and Q4 (OR=3.431, P=0.003) compared to Q1. CAP differed significantly among these subgroups (P=0.005), showing an uptrend from Q1 to Q4. Pairwise comparisons between subgroups uncovered significant increases in Q2 (P=0.008), Q3 (P=0.003), and Q4 (P=0.001) when compared to Q1. After adjustment for gender and age, the difference in CAP remained among Q1–Q4 (P=0.001). Pairwise comparisons obtained similar results with Q1 as the reference (all P<0.01, Table 2).
 |
Table 2 Comparisons of CAP Among Serum FGF23 Quartiles |
Interaction of CAP Between Serum FGF23 Levels and Sleep Duration
On the basis of upper quartile values of sleep duration (9 h), the present study population was stratified as individuals with short sleep duration and long sleep duration. Multivariate variance analyses took into consideration the influence of serum FGF23 levels and sleep duration on CAP. As a result, there were significant differences in CAP among Q1–Q4 (P=0.008) and between individuals with short and long sleep duration (P=0.023). The associations of serum FGF23 levels and sleep duration with CAP were independent of each other (Figure 1).
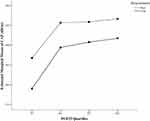 |
Figure 1 Interaction of CAP between serum FGF23 levels and sleep duration. Note: The associations of serum FGF23 levels and sleep duration with CAP were independent of each other (both P<0.05). |
Multiple Stepwise Linear Regression of CAP
Multiple stepwise linear regression defined CAP as the dependent variable, and serum FGF23 levels, age, gender, and total metabolic traits (BMI, MAP, HbA1c, TG, HDL-c, and LDL-c) as independent variables. The results showed that in addition to BMI, MAP, TG, and HDL-c, serum FGF23 levels were independently and positively associated with CAP (standardized β=0.117, P=0.031). Further adjustment for sleep duration showed serum FGF23 levels were still an independent and positive factor of CAP (standardized β= 0.112, P=0.042, Table 3).
 |
Table 3 Linear Regression Analysis of CAP |
Discussion
The present study revealed that individuals with hepatic steatosis exhibited higher serum FGF23 levels. CAP increased with the FGF23 quartiles. After adjustment for gender, age, and total metabolic traits, serum FGF23 levels were associated with CAP positively and independently. Longer sleep duration could attenuate the extent of hepatic steatosis, but did not interfere in the association between serum FGF23 levels and CAP.
There was growing evidence supporting bone involvement in the regulation of homeostasis, including the energy balance and metabolism of adipose. Interacting through bone-derived factor and adipocytokine, bone and adipose tissue established a feedback system of homeostasis.20 As a factor mainly produced and secreted by osteoblasts/osteocytes, FGF23 was suggested to play a role in the regulation of fat accumulation and distribution. Clinical research revealed that FGF23 was correlated with not only overall obesity, but also central obesity. To be precise, FGF23 explained 2% of the variations in total fat mass and 3% of the variations in trunk fat mass. It was suggested that circulating FGF23 was related to increased fat mass and the occurrence and development of the metabolic syndrome and its components.11 Our previous study also demonstrated that serum FGF23 levels were associated with visceral fat accumulation independently.21 NAFLD is recognized as the hepatic manifestation of the metabolic syndrome.13 So far, however, there have been rare clinical studies investigating the relationship between serum FGF23 levels and NAFLD. Chinese researchers conducted a clinical study in patients with type 2 diabetes, with a diagnosis of NAFLD by hepatic ultrasound and evaluation of hepatic steatosis according to the fatty liver index. The results showed an independent and positive association of serum FGF23 levels with the presence and severity of NAFLD.12 Without the influence of inflammation, fibrosis, and etiology, CAP obtained by Fibroscan was more accurate in the assessment of hepatic steatosis than ultrasound. Additionally, CAP was highly sensitive to mild hepatic steatosis when the fat depositions were more than 10%.14 Several studies with liver biopsy as gold standard indicated that CAP effectively quantified the severity of hepatic steatosis.15,16 Therefore, the present study used Fibroscan instead of traditional ultrasound to detect and assess hepatic steatosis with CAP. The results suggested that hepatic steatosis is aggravated with the increase in serum FGF23 levels. Serum FGF23 levels stood out as a positive factor for hepatic steatosis independent of metabolic traits, in line with the previous studies.
Over the past century, the average duration of sleep for adults in the world has been descending.22 Inadequate sleep duration results in a series of adverse health outcomes, leading to remarkable changes in endocrine, metabolism, stress, and immune pathways. Especially, sleep deprivation exerts negative impacts on metabolic disorders, such as obesity, diabetes, hypertension, and metabolic syndrome.23 Epidemiological studies revealed the association between sleep duration and NAFLD, of which the results, nevertheless, did not reach a consensus.22–25 A meta-analysis found an increased risk of NAFLD among individuals with short sleep duration.22 A study from China revealed the correlation between short sleep duration and an increased risk of prevalent NAFLD among middle-aged and elderly Chinese populations. Spanish researchers discovered that sleep disruption might contribute to the pathogenesis of NAFLD, and the alteration of the liver, in turn, might influence sleep patterns.24 However, Kim et al provided evidence supporting the relationship between longer sleep duration and incidence of NAFLD.25 Consistent with most of the previous studies, the present study uncovered that hepatic steatosis was attenuated in individuals with longer sleep duration. In addition, the associations of sleep duration and serum FGF23 levels with NAFLD were independent of each other. Therefore, for the high-risk population with higher serum FGF23 levels, longer sleep duration might contribute to the prevention of NAFLD.
The mechanism behind the association between FGF23 and NAFLD remained unclear. Ectopic overexpression of FGF23 by hepatocytes was observed in 2 infants with end-stage liver disease.26 Additionally, serum FGF23 levels and the mRNA expression of FGF23 in the liver were significantly increased following the administration of lipopolysaccharides.27 Basic research uncovered that FGF23 played a direct regulatory role in expression of Fetuin-A, an anti–inflammatory protein synthesized by the liver, which suggested a potential regulatory effect of FGF23 on inflammatory cytokines via the tumor necrosis factor-α/nuclear factor-kappa B pathway.28 Additionally, FGF receptor 1c, a potential receptor for FGF23, was found to be abundantly expressed in macrophages,27 of which the resident hepatic form, known as Kupffer cells, could lead to increased hepatic steatosis via increased activity of diacylglycerol transferase when polarized to the M1 phenotype.4 There is emerging evidence that FGF23 directly interacts with macrophages through binding of FGF receptor/α-Kl receptors.29 Xu et al discovered that FGF receptor inhibitor could increase the serum FGF23 levels to activate the phosphorylation of janus kinase 2, while anti-FGF23 could suppress it.10 The activation of janus kinase/activators of transcription pathway was involved in TG accumulation, insulin resistance, and fat deposition in the liver. Shi et al found that hepatocyte-specific deletion of janus kinase 2 could protect against diet-induced hepatic steatosis.9 Furthermore, interferon-α exerts an impact on memory CD8 cells and cytotoxic CD8 cells, and further promotes the recruitment and activation of macrophages in adipose tissue, contributing to ectopic fat storage and utilization, such as hepatic steatosis.30 Therefore, these findings suggested a role of FGF23 in the process of ectopic fat deposition, inflammation, and fibrosis in the liver via inflammatory pathways, including tumor necrosis factor-α/nuclear factor-kappa B and janus kinase/activators of transcription pathways. Additionally, FGF21 belongs to the same FGF subfamily (FGF19 subfamily) as FGF23, which promotes insulin sensitivity but causes bone loss.31 Systemic FGF21 levels were correlated positively with hepatic fat content, suggesting that the function of FGF21 is impaired in NAFLD. Mechanistically, the elevation of circulating FGF21 levels might result from dysfunctional peroxisome proliferator-activated receptor-α signaling, which provided the potential mechanism for the association of FGF23 and NAFLD.32
There were some limitations to the present study. Firstly, because of the cross-sectional nature of the present study, the chronological and causal sequences of changes in the serum FGF23 levels and the occurrence and development of hepatic steatosis were hard to determine. Secondly, the present study population was restricted to patients with diabetes, and the sample size was relatively small. In the future, research studies are necessary to confirm and generalize the findings in larger cohorts with different characteristics.
Conclusion
Serum FGF23 levels were independently and positively associated with the severity of hepatic steatosis. The associations of serum FGF23 levels and sleep duration with hepatic steatosis were independent of each other. It was suggested that for individuals with diabetes, serum FGF23 levels were expected to be a target for monitoring, controlling, and treating NAFLD in patients with diabetes. Additionally, as a lifestyle Intervention, prolonging sleep duration might bring some additional benefits.
Acknowledgments
This research was funded by grants from Wenzhou Science & Technology Bureau, grant number Y20190126 and Y20170047; The Project Supported by Zhejiang Provincial Natural Science Foundation of China, grant number LY20H070003; National Key R&D Program of China, grant number 2016YFC1305202; and National Natural Science Foundation of China, grant number 81900737.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67:862–873. doi:10.1016/j.jhep.2017.06.003
2. Adams LA, Waters OR, Knuiman MW, et al. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol. 2009;104:861–867. doi:10.1038/ajg.2009.67
3. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212–1218. doi:10.2337/dc06-2247
4. Manne V, Handa P, Kowdley KV. Pathophysiology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Clin Liver Dis. 2018;22:23–37. doi:10.1016/j.cld.2017.08.007
5. Urakawa I, Yamazaki Y, Shimada T, et al. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature. 2006;444:770–774. doi:10.1038/nature05315
6. Martin A, David V, Quarles LD. Regulation and function of the FGF23/klotho endocrine pathways. Physiol Rev. 2012;92:131–155. doi:10.1152/physrev.00002.2011
7. Grethen E, Hill KM, Jones R, et al. Serum leptin, parathyroid hormone, 1,25-dihydroxyvitamin D, fibroblast growth factor 23, bone alkaline phosphatase, and sclerostin relationships in obesity. J Clin Endocrinol Metab. 2012;97:1655–1662. doi:10.1210/jc.2011-2280
8. Silswal N, Touchberry CD, Daniel DR, et al. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am J Physiol Endocrinol Metab. 2014;307:E426–436. doi:10.1152/ajpendo.00264.2014
9. Shi SY, Martin RG, Duncan RE, et al. Hepatocyte-specific deletion of Janus kinase 2 (JAK2) protects against diet-induced steatohepatitis and glucose intolerance. J Biol Chem. 2012;287:10277–10288. doi:10.1074/jbc.M111.317453
10. Xu L, Zhang L, Zhang H, et al. The participation of fibroblast growth factor 23 (FGF23) in the progression of osteoporosis via JAK/STAT pathway. J Cell Biochem. 2018;119:3819–3828. doi:10.1002/jcb.26332
11. Mirza MA, Alsiö J, Hammarstedt A, et al. Circulating fibroblast growth factor-23 is associated with fat mass and dyslipidemia in two independent cohorts of elderly individuals. Arterioscler Thromb Vasc Biol. 2011;31:219–227. doi:10.1161/ATVBAHA.110.214619
12. He X, Shen Y, Ma X, et al. The association of serum FGF23 and non-alcoholic fatty liver disease is independent of vitamin D in type 2 diabetes patients. Clin Exp Pharmacol Physiol. 2018;45:668–674. doi:10.1111/1440-1681.12933
13. Bril F, Cusi K. Nonalcoholic fatty liver disease: the new complication of type 2 diabetes mellitus. Endocrinol Metab Clin North Am. 2016;45:765–781. doi:10.1016/j.ecl.2016.06.005
14. de Lédinghen V, Vergniol J, Foucher J, et al. Non-invasive diagnosis of liver steatosis using controlled attenuation parameter (CAP) and transient elastography. Liver Int. 2012;32:911–918. doi:10.1111/j.1478-3231.2012.02820.x
15. Kumar M, Rastogi A, Singh T, et al. Controlled attenuation parameter for non-invasive assessment of hepatic steatosis: does etiology affect performance? J Gastroenterol Hepatol. 2013;28:1194–1201. doi:10.1111/jgh.12134
16. Chon YE, Jung KS, Kim SU, et al. Controlled attenuation parameter (CAP) for detection of hepatic steatosis in patients with chronic liver diseases: a prospective study of a native Korean population. Liver Int. 2014;34:102–109. doi:10.1111/liv.12282
17. Jian-Gao F; Chinese Liver Disease Association. Guidelines for management of nonalcoholic fatty liver disease: an updated and revised edition. Zhonghua Gan Zang Bing Za Zhi. 2010;18:163–166.
18. Cai YJ, Dong JJ, Wang XD, et al. A diagnostic algorithm for assessment of liver fibrosis by liver stiffness measurement in patients with chronic hepatitis B. J Viral Hepat. 2017;24:1005–1015. doi:10.1111/jvh.12715
19. Eddowes PJ, Sasso M, Allison M, et al. Accuracy of Fibroscan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1717–1730. doi:10.1053/j.gastro.2019.01.042
20. Greco EA, Lenzi A, Migliaccio S. The obesity of bone. Ther Adv Endocrinol Metab. 2015;6:273–286. doi:10.1177/2042018815611004
21. Hu X, Ma X, Luo Y, et al. Associations of serum fibroblast growth factor 23 levels with obesity and visceral fat accumulation. Clin Nutr. 2018;37:223–228. doi:10.1016/j.clnu.2016.12.010
22. Wijarnpreecha K, Thongprayoon C, Panjawatanan P, et al. Short sleep duration and risk of nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;31:1802–1807. doi:10.1111/jgh.13391
23. Peng K, Lin L, Wang Z, et al. Short sleep duration and longer daytime napping are associated with nonalcoholic fatty liver disease in chinese adults. J Diabetes. 2017;9:827–836. doi:10.1111/1753-0407.12489
24. Marin-Alejandre BA, Abete I, Cantero I, et al. Association between sleep disturbances and liver status in obese subjects with nonalcoholic fatty liver disease: a comparison with healthy controls. Nutrients. 2019;11:322. doi:10.3390/nu11020322
25. Kim JH, Jung DH, Kwon YJ, et al. The impact of the sleep duration on NAFLD score in Korean middle-aged adults: a community-based cohort study. Sleep Med. 2019;57:144–150. doi:10.1016/j.sleep.2019.02.012
26. Wasserman H, Ikomi C, Hafberg ET, et al. Two case reports of FGF23-induced hypophosphatemia in childhood biliary atresia. Pediatrics. 2016;138:e20154453. doi:10.1542/peds.2015-4453
27. Masuda Y, Ohta H, Morita Y, et al. Expression of Fgf23 in activated dendritic cells and macrophages in response to immunological stimuli in mice. Biol Pharm Bull. 2015;38:687–693. doi:10.1248/bpb.b14-00276
28. Mattinzoli D, Ikehata M, Tsugawa K, et al. FGF23 and fetuin-A interaction in the liver and in the circulation. Int J Biol Sci. 2018;14:586–598. doi:10.7150/ijbs.23256
29. Fitzpatrick EA, Han X, Xiao Z, et al. Role of fibroblast growth factor-23 in innate immune responses. Front Endocrinol (Lausanne). 2018;9:320. doi:10.3389/fendo.2018.00320
30. Tarantino G, Costantini S, Citro V, et al. Interferon-alpha 2 but not Interferon-gamma serum levels are associated with intramuscular fat in obese patients with nonalcoholic fatty liver disease. J Transl Med. 2019;17:8. doi:10.1186/s12967-018-1754-6
31. Wang X, Wei W, Krzeszinski JY, et al. A liver-bone endocrine relay by IGFBP1 promotes osteoclastogenesis and mediates FGF21-induced bone resorption. Cell Metab. 2015;22:811–824. doi:10.1016/j.cmet.2015.09.010
32. Tucker B, Li H, Long X, et al. Fibroblast growth factor 21 in non-alcoholic fatty liver disease. Metabolism. 2019;101:153994. doi:10.1016/j.metabol.2019.153994
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
