Back to Journals » Journal of Inflammation Research » Volume 15
Association of Procalcitonin to Albumin Ratio with the Presence and Severity of Sepsis in Neonates
Authors Li T, Li X, Liu X, Zhu Z, Zhang M, Xu Z, Wei Y, Feng Y, Qiao X, Yang J, Dong G
Received 24 January 2022
Accepted for publication 16 March 2022
Published 12 April 2022 Volume 2022:15 Pages 2313—2321
DOI https://doi.org/10.2147/JIR.S358067
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Tiewei Li,1,* Xiaojuan Li,1,* Xinrui Liu,1 Zhiwei Zhu,1 Min Zhang,1 Zhe Xu,1 Yulei Wei,1 Yichuang Feng,1 Xiaoliang Qiao,2 Junmei Yang,1 Geng Dong1
1Zhengzhou Key Laboratory of Children’s Infection and Immunity, Children’s Hospital Affiliated to Zhengzhou University, Henan Children’s Hospital, Zhengzhou Children’s Hospital, Zhengzhou, People’s Republic of China; 2Center of Laboratory Medicine, Women & Infants Hospital of Zhengzhou, Zhengzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junmei Yang; Geng Dong, Email [email protected]; [email protected]
Purpose: Previous studies have demonstrated that procalcitonin and albumin have a close correlation with sepsis. However, the role of procalcitonin (PCT) to albumin (ALB) ratio (PAR) in sepsis was still unclear, especially in neonates. Thus, this study aimed to investigate the association between PAR and neonatal sepsis.
Patients and Methods: A total of 1,196 neonates with suspected sepsis were included in this study. Neonates were divided into control group and sepsis group, according to whether they were diagnosed with sepsis. Neonates with sepsis were further divided into mild sepsis and severe sepsis group according to the severity of sepsis. PAR was calculated as serum PCT (ng/mL)/ALB (mg/mL). All statistical analyses were performed using the statistical package SPSS 24.0, as appropriate.
Results: Compared with the control group, neonates with sepsis had a higher PAR. PAR also showed a significant gradual increase in the control, mild sepsis, and severe sepsis groups (P< 0.001). Correlation analysis showed that there was a strong positive correlation between PAR and hsCRP, neonatal sequential organ failure assessment score (nSOFA), and prolonged length of hospital stay (P< 0.001). On multiple logistic regression, higher PAR was independently associated with the presence and severity of neonatal sepsis. According to the receiver operating characteristic curve analysis, a PAR ≥ 0.065 had 64% sensitivity and 72% specificity in predicting the presence of neonatal sepsis (area under curve (AUC)=0.72, 95% CI=0.69– 0.75, P< 0.001) and a PAR≥ 0.070 had 69% sensitivity and 63% specificity in predicting the presence of severe sepsis (AUC=0.71, 95% CI=0.68– 0.74, P< 0.001).
Conclusion: PAR is significantly higher in neonates with sepsis and correlated with the severity of the disease. Increased PAR is an independent predictor useful for identifying the presence and severity of neonatal sepsis.
Keywords: procalcitonin-to-albumin ratio, neonatal sepsis, severe sepsis, predictor
Introduction
Neonatal sepsis remains a leading cause of morbidity and mortality in infants worldwide.1–3 It is estimated there may be about 3 million cases of neonatal sepsis in the world.4 Compared with adults, the immune system of neonates is not yet mature. Therefore, neonates were more prone to be infected by pathogenic microorganisms and can further develop neonatal sepsis. Neonatal sepsis has been a common and fatal disease affecting neonates all over the world. Currently, the gold standard for diagnosis of neonatal sepsis is blood culture.5 However, the blood culture faces a low positive detection rate of pathogenic microorganisms, owing to the pre-hospital antimicrobial exposure, inadequate blood volume from neonates, and a low bacteremia.6 In addition, blood culture needs a long waiting time for the results. Meanwhile, neonatal sepsis can present with subtle signs but can rapidly progress to multisystem organ failure and meningitis.7 Therefore, the rapid identification of neonatal sepsis is the key to successful treatment in neonatal sepsis.
Procalcitonin (PCT) is a 116-amino acid peptide produced in the thyroid C-cells and adipose tissue in healthy individuals.8 Under normal physiological conditions, serum PCT was maintained at a low level (<0.05 ng/mL).9 However, in the case of systemic inflammation, especially bacterial infection, PCT is produced in large quantities by many tissues. Currently, multiple studies have demonstrated that PCT was a useful biomarker to assist the clinician in the diagnosis of sepsis in adults and children (including neonates).10–13 Albumin (ALB) is a protein synthesized by the liver hepatocytes and makes up 40~60% of the total proteins in the body.14 ALB is the main protein responsible for maintaining the colloid-osmotic pressure and can act as a transporter of several endogenous and exogenous compounds.14 In addition to being a nutritional indicator, ALB was closely related with the inflammation and hypoalbuminemia was frequently seen in patients with inflammatory diseases.15–18 Qian and Liu19 also found that the rates of hypoalbuminemia are common among children with sepsis and serum albumin level was negatively correlated with the prognosis.
PCT-to-ALB ratio (PAR), based on PCT and ALB levels, indicates not only the infection/inflammation, but also the body nutritional status. Studies have reported that PAR was an early diagnostic predictor in discriminating urosepsis from adult patients with febrile urinary tract infection20 and an independent predictor of the poor prognosis in adult patients with sepsis-induced acute kidney injury.21 However, to our knowledge, there are no published studies on the association between PAR and sepsis in neonates. Thus, this study aims to evaluate the relationship between PAR and sepsis in a relatively large neonatal population.
Materials and Methods
Clinical Definition
Neonatal sepsis is defined as systemic inflammatory response syndrome in the presence of or as a result of suspected or proven infection. Severe sepsis was defined as sepsis plus one of the following: cardiovascular organ dysfunction, acute respiratory distress syndrome, or two or more other organ dysfunctions (respiratory, renal, neurologic, hematologic, or hepatic), according to the published International Pediatric Sepsis Consensus.22 Infection was defined as a suspected or proven infection caused by any pathogen or clinical syndrome associated with a high probability of infection, including clinical exam, imaging, or laboratory tests. The diagnosis of clinical neonatal infection and sepsis was made by two study investigators as per the International Pediatric Sepsis Consensus.22 The severity of neonatal sepsis was assessed by using the neonatal sequential organ failure assessment (nSOFA) score that consisted of respiratory, cardiovascular, and hematological criteria.23 In this study, neonates with suspected sepsis (not diagnosed with sepsis) were used as the control group.
Study Population
This was a hospital-based observational retrospective study conducted in Henan Children’s Hospital (Zhengzhou, China). From January 2016 to December 2020, a total of 1,196 consecutive neonates with suspected sepsis were enrolled in this study. Inclusion criteria include 1) aged 1–28 days, and 2) neonates with symptoms of infection. Exclusion criteria include 1) incomplete clinical and laboratory data at admission, 2) congenital liver defects and previous liver related diseases, and 3) neonates with malignancies, haematological system diseases, or major congenital malformations. The study protocol complied with the Declaration of Helsinki and the approval of the hospital ethics review board was obtained.
Data Collection
The data of the first admission were collected from electronic medical records, including the following aspects: 1) demographic and admission status data, including age, gender, weight, body temperature, respiratory rate, heart rate, systolic blood pressure, and diastolic blood pressure; and 2) laboratory data at admission, including PCT, C-reactive protein (CRP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), total protein (TP), and ALB. The detection methods of those laboratory indexes were described in our previous published study.24 For our data, CRP levels <0.8 mg/L were assigned a value of 0.7 mg/L. PCT level >100 ng/mL or <0.02 ng/mL were assigned, 101 ng/mL and 0.01 ng/mL, respectively.
Statistical Analysis
Continuous variables are presented as mean±standard deviation (SD) for normally distributed variables, or medians (interquartile range) for non-normally distributed variables, and analyzed using independent t-tests or one-way analysis of variance (ANOVA) test. Categorical variables are expressed as numbers (percentage) and analyzed using Chi-square tests. The correlation between PAR and other clinical and laboratory indexes was analyzed by Spearman correlation coefficients. Multiple logistic regression analysis was used to evaluate whether PAR was an independent risk factor for the presence and severity of neonatal sepsis. Variables with a P-value <0.05 in the univariate logistic analysis were included in the multiple logistic regression analysis. All data statistical analyses were performed using IBM SPSS version 24.0 (SPSS Inc., Chicago, IL). A two-sided P-value of less than 0.05 was considered statistically significant.
Results
Study Population Characteristics
A total of 1,196 neonates suspected with sepsis were enrolled in this study. At present in Table 1, 758 neonates had a diagnosis of sepsis, and the remaining 438 neonates with infection served as controls. According to the severity of sepsis, neonates with sepsis were further divided into mild sepsis and severe sepsis groups.
 |
Table 1 Basic Characteristics of Study Subjects |
Characteristics of the study population are shown in Table 1. Compared with the control group, neonates with sepsis were older and had a higher body temperature, respiratory rate, and heart rate. Biochemical analysis revealed that the levels of PCT, CRP, and ALT were higher in neonates with sepsis. Meanwhile, the levels of TP and ALB were lower in neonates with sepsis. Further analysis showed that neonates with sepsis had a higher PAR and nSOFA score and a longer length of hospital stay. Among those variables, only PCT, CRP, TP, ALB, PAR, and the length of hospital stay showed a gradual increase or decrease with the severity of sepsis (P<0.05).
Associations Between PAR and the Presence and Severity of Neonatal Sepsis
According to the tertiles of PAR, neonates were divided into three groups: low PAR group (<0.043×10−4), intermediate PAR group ((0.043–0.134)×10−4), and high PAR group (>0.134×10−4). The clinical and laboratory data of the study patients based on tertiles of PAR are presented in Table 2. Neonates in the high PAR group had a higher level of CRP and longer length of hospital stay, compared with other groups. Further analysis showed that the prevalence of overall sepsis and severe sepsis showed a progressive increase from the low PAR group to the high PAR group, while the prevalence of control showed a progressive decrease from the low PAR group to the high PAR group (P<0.001).
 |
Table 2 The Presence and Severity of Neonatal Sepsis According to PAR Tertiles |
Correlation Between PAR and Clinical and Laboratory Indexes
As shown in Table 3, PAR was negatively correlated with age (r=−0.207, P<0.001) and weight (r=−0.097, P=0.001), and positively correlated with body temperature (r=0.163, P<0.001), respiratory rate (r=0.118, P<0.001), and heart rate (r=0.125, P<0.001). In the correlation analysis between PAR and biochemical indexes, our data showed that PCT was significantly correlated with CRP (r=0.437, P<0.001), AST (r=0.174, P<0.001), ALT (r=0.151, P<0.001), and TP (r=−0.308, P<0.001). In addition, PAR also showed a strong correlation with the nSOFA score (r=0.352, P<0.001) and the length of hospital stay (r=0.322, P<0.001).
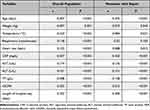 |
Table 3 Correlations Between PAR and Clinical Parameters |
Predictive Value of PAR for the Presence and Severity of Neonatal Sepsis
As present in Table 4, after adjusting age, temperature, heart rate, respiratory rate, CRP, AST, ALT, and TP, multivariable binary logistic regression analysis revealed that PAR was an independent risk factor for the presence of sepsis (OR=1.211, 95% CI=1.035–1.416, P<0.001) and severe sepsis (OR=1.080, 95% CI=1.037–1.125, P=0.001). Further analysis showed that PAR tertiles were also independently associated with an increased prevalence of neonatal sepsis.
 |
Table 4 Regression Analysis to Assess the Presence of Neonatal Sepsis and Severe Sepsis According to PAR Tertiles |
Diagnostic Value of PAR in Neonatal Sepsis
The ROC curve analysis was performed to evaluate the diagnostic value of the PAR in neonatal sepsis. As shown in Figure 1A, the AUC for the PAR in predicting overall neonatal sepsis was 0.72 (95% CI=0.69–0.75, P<0.001). The optimal cut-off value of PAR was 0.065×10−4, with 64% sensitivity and 72% specificity. Additionally, we further evaluated the ability of the PAR to predict severe sepsis. The AUC was 0.71 (95% CI=0.68–0.74, P<0.001), with a sensitivity and specificity of 69% and 62%, respectively, at a cut-off value of 0.076×10−4 (Figure 1B).
Discussion
Neonatal sepsis, characterized by systemic inflammatory response syndrome caused by infection, is a serious and life-threatening disease in newborns.25 Compared with adult, neonates were more susceptible to infection, and then develop into sepsis, severe sepsis, septic shock, and death.26 Based on a systematic review and meta-analysis of studies reporting population-based sepsis incidence in neonates, Fleischmann-Struzek et al4 reported that neonates had a high risk of sepsis and a higher mortality, between 11% and 19%. Early and accurate diagnosis of neonatal sepsis can reduce the development of sepsis and the occurrence of death events and decrease the overuse of antibiotics. Currently, blood culture, the gold diagnosis of neonatal sepsis, faces some challenges, such as pre-hospital antimicrobial therapy, inadequate volume of blood, and a long waiting time,5,6 which lead to the low positive rate of blood culture and the inability to give early clinical result feedback. Circulating blood biomarkers have advantages in terms of convenience, being economical, and rapid, which can provide important information in the early diagnosis of neonatal sepsis.
Procalcitonin (PCT), a marker of bacterial infection, exhibits greater specificity than other proinflammatory markers.27–29 Studies have demonstrated that PCT is a specific inflammatory marker of sepsis, and the efficiency of PCT in identifying early bacterial infection is better than CRP.30–32 A meta-analysis of 3,244 patients showed that the AUC of PCT in the diagnosis of sepsis was up to 0.85.13 In addition, PCT can also be used to guide the monitoring of the therapeutic effect of antibiotics, which can result in improved survival and lower antibiotic treatment duration.33,34 In terms of neonates, PCT level physiologically after birth and reaches a peak level at 24 hours, and then decreases gradually to normal at 48–72 hours, suggesting that PCT may not be a better early marker of neonatal sepsis.35,36 However, according to the physiological characteristics of serum PCT in early newborns, setting the PCT cut-off values of sepsis can improve the accuracy of neonatal sepsis diagnosis.37
ALB was the most abundant protein in blood produced by the liver. Traditionally, ALB is considered as a nutritional index, which can reflect the nutritional status of the body.17 However, some studies reported that ALB is a marker related to inflammation.15–17,38,39 In sepsis, pathogens, toxins, or inflammatory mediators can impair the ability of liver function to synthesize ALB, resulting in a significant decrease in ALB content.40 Godinez-Vidal et al41 reported that ALB could be a predictor of severity of abdominal sepsis in adult patients, while it was not a predictor of mortality. In neonates, Yang et al42 reported that a lower level of ALB was frequent among neonates with sepsis and associated with a poorer prognosis.
In recent years, to further improve the potential predictive value of each single marker, PCT and ALB were combined to generate a new index: PAR. PAR can both indicate the infection/inflammation and the nutritional status, which may enhance the predictive value. Studies have reported that PAR or ALB/PCT was an independent predictor of 28-day mortality in acute respiratory distress syndrome (ARDS) patients43 and could be used as a sensitive early diagnostic marker for nosocomial blood stream infection in patients with intra-cerebral hemorrhage.44 A low ALB/PCT ratio was associated with a high risk to experience shock in patients with intra-cerebral hemorrhage.44 Luo et al20 reported that PAR was an early diagnostic predictor that can discriminate between urosepsis and febrile urinary tract infection, and urosepsis patients with high PAR were more likely to experience uroseptic shock. However, in terms of the association between PAR and neonatal sepsis, there is no relevant research report at present.
In this study, we firstly explore the association between PAR and sepsis in a relatively large neonatal population and found that PAR was higher in neonates with sepsis and showed a gradual increase among control group, mild sepsis group, and severe sepsis group. According to PAR tertiles, neonates were divided into three groups, and our data showed that the prevalence of overall sepsis increased significantly from 41.3% in PAR tertile 1 to 83.4% in PAR tertile 3 (P<0.001). Additionally, the prevalence of severe sepsis also showed a gradual increase from 16.2% in PAR tertile 1 to 53.7% in PAR tertile 3. Multivariate analysis showed that PAR was an independent predictor for the presence of neonatal sepsis and severe sepsis. ROC curve analysis revealed that PAR had a well discriminatory power in predicting sepsis and severe sepsis. In addition, compared with PCT, ALB, and CRP, our data showed that CAR had a higher discriminatory power in predicting sepsis and severe sepsis (data not shown).
This study also has several limitations. First, neonatal sepsis was diagnosed by two independent doctors based on their clinical features and was not confirmed by positive blood culture. Therefore, the accurate incidence rate of neonatal sepsis may have bias. Second, this is a retrospective single center study, and the results may also differ from other centers. Third, owing to the measurement limits, CRP levels <0.8 mg/L were assigned a value of 0.7 mg/L, and PCT levels >100 ng/mL or <0.02 ng/mL were assigned, 101 ng/mL and 0.01 ng/mL. This definition may lead to bias. At last, PAR was only measured at admission and serial PAR measurement may be more useful in monitoring the association between PAR and neonatal sepsis.
Conclusions
In conclusion, our study demonstrated that PAR was an independent predictor for neonatal sepsis. Additionally, in neonates with sepsis, those with low PAR were more likely to have severe sepsis.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by he Hospital Ethics Review Board of Henan Children’s Hospital. We confirmed that all the data were anonymized and maintained with confidentiality; therefore, the requirement for informed consent has been waived because of the retrospective nature of the current study.
Acknowledgments
We gratefully thank Chong Ren for her important contribution in laboratory data processing. In addition, we also thank Bullet Edits for its linguistic assistance during the preparation of this manuscript. Tiewei Li and Xiaojuan Li are co-first authors for this study.
Funding
This work was supported by the Key Research, Development, and Promotion Projects of Henan Province (222102310171, 222102310328 and 222102310067), and Medical Science and Technology Project of Henan Province (LHGJ20200633, LHGJ20200666, LHGJ20210681, LHGJ20210637, LHGJ20210654, LHGJ20210665, LHGJ20210672 and LHGJ20210661).
Disclosure
The authors report no conflicts of interest.
References
1. Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of global incidence and mortality of hospital-treated sepsis. current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi:10.1164/rccm.201504-0781OC
2. Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42(3):625–631. doi:10.1097/CCM.0000000000000026
3. Berg D, Gerlach H. Recent advances in understanding and managing sepsis. F1000Res. 2018;7:1570. doi:10.12688/f1000research.15758.1
4. Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med. 2018;6(3):223–230. doi:10.1016/S2213-2600(18)30063-8
5. Ershad M, Mostafa A, Dela Cruz M, Vearrier D. Neonatal Sepsis. Neonatal Sepsis Curr Emerg Hosp Med Rep. 2019;7(3):83–90. doi:10.1007/s40138-019-00188-z
6. Iroh Tam PY, Bendel CM. Diagnostics for neonatal sepsis: current approaches and future directions. Pediatr Res. 2017;82(4):574–583. doi:10.1038/pr.2017.134
7. Kim F, Polin RA, Hooven TA. Neonatal sepsis. BMJ. 2020;371:m3672. doi:10.1136/bmj.m3672
8. Paudel R, Dogra P, Montgomery-Yates AA, Coz Yataco A. Procalcitonin: a promising tool or just another overhyped test? Int J Med Sci. 2020;17(3):332–337. doi:10.7150/ijms.39367
9. Lippi G, Sanchis-Gomar F. Procalcitonin in inflammatory bowel disease: drawbacks and opportunities. World J Gastroenterol. 2017;23(47):8283–8290. doi:10.3748/wjg.v23.i47.8283
10. Mohsen AH, Kamel BA. Predictive values for procalcitonin in the diagnosis of neonatal sepsis. Electron Physician. 2015;7(4):1190–1195. doi:10.14661/2015.1190-1195
11. Vouloumanou EK, Plessa E, Karageorgopoulos DE, Mantadakis E, Falagas ME. Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta-analysis. Intensive Care Med. 2011;37(5):747–762. doi:10.1007/s00134-011-2174-8
12. Vijayan AL, Ravindran S, Ravindran S, et al. Procalcitonin: a promising diagnostic marker for sepsis and antibiotic therapy. J Intensive Care. 2017;5:51. doi:10.1186/s40560-017-0246-8
13. Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(5):426–435. doi:10.1016/S1473-3099(12)70323-7
14. Fanali G, Di Masi A, Trezza V, Marino M, Fasano M, Ascenzi P. Human serum albumin: from bench to bedside. Mol Aspects Med. 2012;33(3):209–290. doi:10.1016/j.mam.2011.12.002
15. Eckart A, Struja T, Kutz A, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med. 2020;133(6):713–722 e7. doi:10.1016/j.amjmed.2019.10.031
16. Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr. 2019;43(2):181–193. doi:10.1002/jpen.1451
17. Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17(6):432–437. doi:10.1111/j.0894-0959.2004.17603.x
18. Arnau-Barres I, Guerri-Fernandez R, Luque S, Sorli L, Vazquez O, Miralles R. Serum albumin is a strong predictor of sepsis outcome in elderly patients. Eur J Clin Microbiol Infect Dis. 2019;38(4):743–746. doi:10.1007/s10096-019-03478-2
19. Qian SY, Liu J. [Relationship between serum albumin level and prognosis in children with sepsis, severe sepsis or septic shock]. Zhonghua Er Ke Za Zhi. 2012;50(3):184–187. Chinese.
20. Luo X, Yang X, Li J, et al. The procalcitonin/albumin ratio as an early diagnostic predictor in discriminating urosepsis from patients with febrile urinary tract infection. Medicine. 2018;97(28):e11078. doi:10.1097/MD.0000000000011078
21. Chen L, Wu X, Qin H, Zhu H. The PCT to albumin ratio predicts mortality in patients with acute kidney injury caused by abdominal infection-evoked sepsis. Front Nutr. 2021;8:584461. doi:10.3389/fnut.2021.584461
22. Goldstein B, Giroir B, Randolph A. International consensus conference on Pediatric S. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8. doi:10.1097/01.PCC.0000149131.72248.E6
23. Wynn JL, Polin RA. A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr Res. 2020;88(1):85–90. doi:10.1038/s41390-019-0517-2
24. Li T, Dong G, Zhang M, et al. Association of neutrophil-lymphocyte ratio and the presence of neonatal sepsis. J Immunol Res. 2020;2020:7650713. doi:10.1155/2020/7650713
25. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390(10104):1770–1780. doi:10.1016/s0140-6736(17)31002-4
26. Camacho-Gonzalez A, Spearman PW, Stoll BJ. Neonatal infectious diseases: evaluation of neonatal sepsis. Pediatr Clin North Am. 2013;60(2):367–389. doi:10.1016/j.pcl.2012.12.003
27. Yan ST, Sun LC, Jia HB, Gao W, Yang JP, Zhang GQ. Procalcitonin levels in bloodstream infections caused by different sources and species of bacteria. Am J Emerg Med. 2017;35(4):579–583. doi:10.1016/j.ajem.2016.12.017
28. Leli C, Ferranti M, Moretti A, Al Dhahab ZS, Cenci E, Mencacci A. Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections. Dis Markers. 2015;2015:701480. doi:10.1155/2015/701480
29. Oussalah A, Ferrand J, Filhine-Tresarrieu P, et al. Diagnostic accuracy of procalcitonin for predicting blood culture results in patients with suspected bloodstream infection: an observational study of 35,343 consecutive patients (A STROBE-compliant article). Medicine. 2015;94(44):e1774. doi:10.1097/MD.0000000000001774
30. Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev. 2015;(8):CD007577. doi:10.1002/14651858.CD007577.pub3
31. Schuetz P, Birkhahn R, Sherwin R, et al. Serial procalcitonin predicts mortality in severe sepsis patients: results from the multicenter procalcitonin MOnitoring SEpsis (MOSES) study. Crit Care Med. 2017;45(5):781–789. doi:10.1097/CCM.0000000000002321
32. Nargis W, Ibrahim M, Ahamed BU. Procalcitonin versus C-reactive protein: usefulness as biomarker of sepsis in ICU patient. Int J Crit Illn Inj Sci. 2014;4(3):195–199. doi:10.4103/2229-5151.141356
33. Wirz Y, Meier MA, Bouadma L, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care. 2018;22(1):191. doi:10.1186/s13054-018-2125-7
34. Schuetz P, Beishuizen A, Broyles M, et al. Procalcitonin (PCT)-guided antibiotic stewardship: an international experts consensus on optimized clinical use. Clin Chem Lab Med. 2019;57(9):1308–1318. doi:10.1515/cclm-2018-1181
35. Stocker M, Fontana M, El Helou S, Wegscheider K, Berger TM. Use of procalcitonin-guided decision-making to shorten antibiotic therapy in suspected neonatal early-onset sepsis: prospective randomized intervention trial. Neonatology. 2010;97(2):165–174. doi:10.1159/000241296
36. Chiesa C, Panero A, Rossi N, et al. Reliability of procalcitonin concentrations for the diagnosis of sepsis in critically ill neonates. Clin Infect Dis. 1998;26(3):664–672. doi:10.1086/514576
37. Pontrelli G, De Crescenzo F, Buzzetti R, et al. Accuracy of serum procalcitonin for the diagnosis of sepsis in neonates and children with systemic inflammatory syndrome: a meta-analysis. BMC Infect Dis. 2017;17(1):302. doi:10.1186/s12879-017-2396-7
38. Arroyo V, García-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. J Hepatol. 2014;61(2):396–407. doi:10.1016/j.jhep.2014.04.012
39. Kaysen GA. Biochemistry and biomarkers of inflamed patients: why look, what to assess. Clin J Am Soc Nephrol. 2009;4(Suppl 1):S56–63. doi:10.2215/CJN.03090509
40. Yan J, Li S, Li S. The role of the liver in sepsis. Int Rev Immunol. 2014;33(6):498–510. doi:10.3109/08830185.2014.889129
41. Godinez-Vidal AR, Correa-Montoya A, Enriquez-Santos D, Perez-Escobedo SU, Lopez-Romero SC, Gracida-Mancilla NI. Is albumin a predictor of severity and mortality in patients with abdominal sepsis? [inverted question markEs la albumina un predictor de gravedad y de mortalidad en pacientes con sepsis abdominal?]. Cir Cir. 2019;87(5):485–489. doi:10.24875/CIRU.180003903
42. Yang C, Liu Z, Tian M, et al. Relationship between serum albumin levels and infections in newborn late preterm infants. Med Sci Monit. 2016;22:92–98. doi:10.12659/msm.895435
43. Chen H, Liu Q, Wang L. An analysis of the 28-day mortality risk factors in acute respiratory distress syndrome patients and the establishment of prediction models. Am J Transl Res. 2021;13(6):6937–6944.
44. Deng S, Gao J, Zhao Z, Tian M, Li Y, Gong Y. Albumin/procalcitonin ratio is a sensitive early marker of nosocomial blood stream infection in patients with intra-cerebral hemorrhage. Surg Infect (Larchmt). 2019;20(8):643–649. doi:10.1089/sur.2018.260
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

