Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 15
Association of Patient Anthropometric Measurements and Dental Implant Treatment
Authors Al-Radha ASD
Received 27 January 2023
Accepted for publication 29 March 2023
Published 6 April 2023 Volume 2023:15 Pages 51—61
DOI https://doi.org/10.2147/CCIDE.S406119
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Afya Sahib Diab Al-Radha
Oral Surgery and Periodontology Department, College of Dentistry, Mustansiriyah University, Baghdad, Iraq
Correspondence: Afya Sahib Diab Al-Radha, Oral Surgery and Periodontology Department, College of Dentistry, Mustansiriyah University, Central Baghdad Post Office, Post Box (P.O.) 55388, Baghdad, Iraq, Tel +9647816883387, Email [email protected]; [email protected]
Background: Dental implants are currently one of the most preferred treatment modalities for replacing missing teeth, as they are the most comparable to natural teeth. Even so, satisfaction with such treatment may differ depending on patient nature. The aim of this article was to examine the relationships between different anthropometric measurements on dental implant patient’s satisfaction.
Methods and Material: Self-administered questionnaire (structured questions) were given to patients who had dental implant treatment to evaluate their satisfaction level with dental-implant treatment. Different anthropometric measurements were taken: body height; weight; body mass index (BMI); body composition; waist/hip ratio; and circumferences at the waist, hip, and neck.
Results: The overall BMI was 28.9± 4.7 kg/m2, there was a highly-significant difference in patient satisfaction among the different BMI groups (P< 0.000). The significant difference in most of those groups was between the obese group and the other groups. For neck circumference and waist/hip ratio, a significance difference between the normal weight and obese groups (P< 0.000) was found, while for percentage of muscle, the differences were between the overweight and obese groups (P< 0.000). According to BMI groups a highly significant difference in many patient satisfaction domains were found (P< 0.000). These significant differences were between the obese group and non-obese groups for most aspects of patient satisfaction. For patient satisfaction with final appearance, the normal BMI group differed significantly from the overweight BMI group (P=0.013). Additionally, for patient satisfaction with dentist performance and communication, the overweight BMI group showed significantly higher satisfaction than the normal BMI group (P=0.019). Body measurements were correlated negatively with overall patient satisfaction, and positively with satisfaction with prosthesis.
Conclusion: The obese group patients had the lowest rate of patient satisfaction. BMI and other body measurements can be used to predict patient satisfaction with the outcome of dental implant treatment.
Keywords: dental implant, obesity, body mass index, anthropometry
Introduction
A dental implant is a synthetic tooth root that is implanted into the jaw to replace a missing tooth or teeth that have been lost due to dental disease, tumors, trauma or developmental abnormalities.1 Dental implants are currently one of the most preferred treatment modalities for replacing missing teeth, as they are the most comparable to natural teeth.2
Although dental implant treatment is a somewhat new treatment modality in dentistry, it has undergone substantial progress and advancement,3 Whether by creating new procedures to solve certain problems4,5 or by implication of new surgical technology tool in dental treatment options.6 However, its cost and relatively long treatment time are still considered limitations. Patients anticipate high-standard dental services and excellent treatment outcome as a return for the high costs and time consumed during dental implant therapy.7
A previous study stated that dentists should “meet the mind of the patient before meeting the mouth of the patient”.8 In spite of a good diagnosis and an excellent treatment with significant clinical quality, some patients will remain dissatisfied,9 and anxious.10 Thus patient satisfaction is a multifactorial concept and comprises numerous facets.9
Most of the studies on dental satisfaction have addressed general dental treatment. However, satisfaction may differ depending on patient nature and the type of dental treatment implemented.11 Some previous studies have assessed satisfaction with dental implant treatment.12
In recent years, a series of discoveries have radically altered the view of adipose tissue, and it is now considered an endocrine organ, not simply storage cells. Adipose tissue has a major role in lipid and glucose metabolism and also contributes to signaling in homeostasis. There are two main types of adipose tissue: visceral fat, which is located within the mediastinum and abdominal cavity, and subcutaneous fat, which is located in the hypodermis.13
However, Body mass index (BMI) has been linked to many dental conditions as well as to the number of decayed, missing and filled teeth (DMFT).14 Additionally, obesity has been associated with chronic periodontitis and with poor outcomes following periodontal treatment,15 as well as with increase the chance of complications post implant surgery.16 Similarly, a fatty diet showed to affect osseointegration, resulting in a weak outcome of dental implant therapy.17
BMI, high waist circumference, waist/hip ratio (WHR) and body fat have been associated with periodontitis.18 Patients with obesity have even been shown to have a different microbiome, as Socransky & Haffajee found a high amount of T. forsythia in those with a high BMI (> 35 kg/m2).19 Furthermore, alveolar bone loss has been correlated to obesity (BMI> 30 kg/m2) in patients younger than 40 years of age.20
Knowing the risk factors that associated with disease development and progression is important.21 Adipose tissue has been found to be a source of stem and progenitor cells,22 in which they showed the effect of these mediators on periodontal condition as Currò et al in their study on mRNA transcripts in the gingival tissues suggest that “transglutaminase gene expression” could be modified in the damaged gingival.23 Similar, results had been shown by Isola et al on their study on microRNA (miRNAs) in patients with periodontitis, and they found an increase of miRNAs in the gingival crevicular fluid of the periodontitis group in comparison to healthy controls group.24 Also, Poteser et al, in their study reported the expression of a “subpopulation of CD133+ adipose tissue-resident” stem cells,25 which had been shown later to be significantly lower “(CD133+/KDR+ levels)” in patients with periodontitis compared to healthy patients.26
In the same direction, Azab et al showed a significant increase in the production of “DKK1 mRNA” in chronic periodontitis.27 In the same direction, Some glycoprotein (RANKL/OPG ratio) that regulates bone metabolism had been also linked with the severity of periodontal disease conditions.28 As it had been showed improvement in periodontal condition and reduced DKK1 serum levels after in response to effective nonsurgical periodontal treatment.27
However, a balanced and healthy diet has a protective action on periodontal health. Therefore, adopting an accurate lifestyle and healthy diet is essential for healthy periodontal disease.29 Adding to this, patient education regarding the importance of good oral hygiene practices and using of fluoridated toothpaste is important.30
Achievement of patient satisfactions is one of the essential parts of dental implant treatment. Patient satisfaction varies according to the condition of the patient being served, and it is essential to identify the precise treatment plan for each patients.31
Patient satisfaction is a multifactorial concept.9 It is important to understand the elements that affect patient satisfaction among dental implant patients to ensure a good dental treatment.3,7 Dentists should know the treatment modality for each patient situation32 and should put in mind that the patient’s satisfaction could be jeopardies if he could not perform the correct treatment modality.33 Therefore, assessing the factors that may influence patient satisfaction can provide a clue regarding the best dental treatment.
However, few studies address the impact of anthropometric factors on patient satisfaction.
Our null hypothesis was that patients with a high BMI would be highly satisfied with their dental implant treatment.
This article was aimed to examine if different anthropometric measurements of dental implant patients had an effect on patient satisfaction.
The objective of this study was to (a) to analyse patient’s satisfaction with dental implant treatment, and (b) explore if the patient anthropometric measurements had effect on patients satisfaction.
Materials and Methods
This cross-sectional analytical study was conducted in accordance with the “World Medical Association Declaration of Helsinki”. Approval from “the scientific and ethical committee of the Oral Surgery and Periodontology Department, College of Dentistry, Al-Mustansiriyah University” was obtained for research “including consent procedure”.
Patients attending a dental implant clinic for routine check-up at the “College of Dentistry, Al- Mustansiriyah University, and AL-Karkh General Hospital” were asked to involve in this study.
Inclusion criteria of this study included healthy patients, at least 18 years of age (Age ≥ 18 years), with no active periodontal disease or systemic disease, who had previously implant treatment that still in function. Exclusion criteria: patients had severe periodontitis, systemic diseases, history of chemotherapy, head and neck radiotherapy, smoking history.
The study aim was explained to the patients, and only the patients who participate and gave their consent were included in the study. A questionnaire (structured questions) had been given to patients to fill, those questioners were focused on satisfaction with implant treatment in terms of overall satisfaction and satisfaction with the doctor, with function, aesthetics and phonetics, and with improvement in personal life, psychology makeup and confidence; these aspects were included to cover patient perceptions and to identify the exact nature of dissatisfaction. Moreover, patient “age, gender, and their education level” were also reported. The responses had been recorded on a “5-point Likert scale, with 5=excellent, 4=very good, 3=good, 2=fair and 1=poor”.
Anthropometric Measurements
All measurements were performed by the investigator. Patient weight and height were measured with patients in light clothing and bare feet while standing upright with relaxed shoulders. An electronic scale (Beurer GmbH, Sȍfinger, Germany) was used to measure body weight to the nearest 100 g.
The BMI (kg per meter squared) was calculated for each patient by dividing the weight [in kg] by the square of height [in meters].34
Patients’ waist, hip and neck circumferences were measured using plastic tapes. “Waist circumference was measured midway between the lowest rib and the iliac crest” (after the end of a smooth exhalation) when the patient is standing, and hip circumference was measured at the largest horizontal location.35 Neck circumference was measured “perpendicular to the long axis of the neck” above the cricothyroid cartilage, immediately below the laryngeal prominence.36
Body fat was calculated using a specific formula that included the patient’s height and waist, hip and neck circumferences: http://www.calculator.net/body-fat-calculator.html.
Percentages of body water and muscle were measured using a “special diagnostic scale designed to measure body composition (Beurer GmbH, Sȍfinger, Germany)” after entering each patient’s weight, height, age and gender. A specific chart [guidance for interpretation of body fat (www.beurer.com)] was used to interpret the results of the percentage of fat increase, which was calculated according to each age and gender category.
Statistical analyses were conducted using Excel (Microsoft) and IBM® SPSS® Statistics Version 20. Descriptive statistics (means and standard deviations) were used to analyze and interpret the results.
Analysis of variance (ANOVA) was used to assess any significant differences between the selected groups. To test multiple comparisons (post hoc multiple comparisons), the least significant difference (LSD) was used to find the precise differences between groups. The probability value “(P-value) was considered significant at P< 0.05 and highly significant at P< 0.01”.
Results
Twenty-five patients who had previously received dental implant therapy were enrolled in the study. Patient data were categorized into four groups according to their BMI value: “BMI< 18.5 kg/m2 (underweight), 18.5–24.99 kg/m2 (normal), 25–29.99 kg/m2 (overweight) and ≥ 30 kg/m2 (obese)” based on previously reported cutoffs.37 However, no patients were categorized as being underweight.
77.1% of the patients were female, and 22.9% were male. Additionally, 20% of the patients were categorized as having normal BMI; 44%, as being overweight; and 36%, as being obese.
Highly significant differences between these groups in all body measurements except patient height were found. For neck circumference and waist/hip ratio, a significance difference was observed between the normal weight and obese groups only (P< 0.000), while for percentage of muscle, the differences were apparent between the overweight and obese groups (P< 0.000) (Table 1).
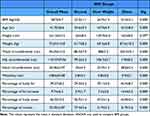 |
Table 1 Average of Different Patients’ Anthropometric Measurements, Body Composition and Age. For All Patients and for Each BMI Group with P values for Differences Between Group Means |
Overall, patient satisfaction was high, with 74% of the patients evaluating their overall implant treatment as excellent and very good, and the rest (26%) providing scores of “good”; none of the patients gave a score of “fair” or “weak”.
The obese patient group showed the lowest value for all aspects of patient satisfaction, as seen in Figure 1, which presents the percentage of excellent and very good response options for the patient satisfaction constructs.
 |
Figure 1 Percentages of excellent and very good scores for different aspects of patient satisfaction for each BMI group. |
The means of all aspects of patient satisfaction according to BMI groups can be seen in Table 2. ANOVA of the three groups revealed a highly significant difference in many patient satisfaction domains (P< 0.000). These significant differences were between the obese group and non-obese groups for most aspects of patient satisfaction, except for appearance, in which the normal BMI group differed significantly from the overweight BMI group (P=0.013). Additionally, for patient satisfaction with dentist performance and communication, the overweight BMI group showed significantly higher satisfaction than the normal BMI group (P=0.019).
 |
Table 2 Average of Different Patients’ Satisfaction Aspects for All Patients and for Each BMI Group with P value for Differences Between Group Means |
The overall correlations of anthropometric measurements with dental implant patient satisfaction can be seen in Table 3. Highly significant negative correlations can be seen between body measurements and many elements of patient satisfaction, particularly improvements in social life, self-confidence, phonetics, psychology, and chewing ability. In contrast, a significant positive correlation was found with satisfaction with prosthesis.
 |
Table 3 Correlation Values Showing the Relation Between Patient Satisfactions Aspects and Different Patient Anthropometric Measurements, Body Composition and Age |
Discussion
This study analysed patient’s satisfaction with dental implant treatment, and explore if the patient anthropometric measurements had effect on it. The results showed that the patient satisfaction with dental implant treatment was high, with 74% excellent and very good, 26% “good”.
However, the obese patient group showed the lowest value for all aspects of patient satisfaction with highly significant negative correlations were found between body measurements and many elements of patient satisfaction.
This study indicated that dental implant patients’ satisfaction was associated with body weight, BMI, and other anthropometric measures. Lower satisfaction values were found in the obese group than in the normal and overweight group.
Satisfaction with improvement in chewing ability was relatively low, as 65.6% of the patients gave scores of “excellent” and “very good”; however, when scores of “good” were included, the rate of satisfaction increased to 91.6%. This rate is in agreement with previous research,38 which they show that about 90% of the treated patients were satisfied and pleased with their masticatory function, and with Alam et al, who reported that 95.2% of their patients were satisfied with the function of their dental implants.2
Indeed, when we considered “excellent”, “very good” and “good” response options as indicating satisfaction, our results were nearly consistent with those of Pjetursson et al, as they found that 72% of patients stated that their implants resemble their teeth in masticatory function and that 92% and 83% were satisfied with the pronunciation and aesthetic aspects of satisfaction, respectively. These findings are in agreement with our results, in which 100% of patients were satisfied with their phonetic results (61.1% when considering only “excellent” and “very good” scores); 91.5% were satisfied with the aesthetics; and 92.1% stated that their dental implant was similar to their natural teeth.38 Similarly, Alam et al also found that all patients (100%) were satisfied with the appearance of their dental implants.2
Obesity is considered a “public health problem” and has been shown to have an adverse effect on wound healing; it has also been associated with adverse post-surgical results such as complications due to infection and delayed healing39 and increased occurrence of wound complications such as dehiscence, hematoma and pressure ulcers.40 These findings indicate that obese patients are more vulnerable and respond differently to trauma, and this sensitivity could explain their low satisfaction level with dental implants. Similar results were found by Wee et al, who also reported low levels of satisfaction with ambulatory care in obese patients compared to normal-weight patients.41
Obesity affects the immune response, causing more susceptibility to infections.42 Additionally, adipocytes release number of inflammatory mediators and initiate a general pro-inflammatory state.43 Obesity has been shown to have an effect on dental implants, and studies have identified greater concentrations of IL-1α and IL-1β, which are inflammatory cytokines, in peri-implantitis and even in the development of peri-implantitis than in healthy sites [IL-1β is considered a “gatekeeper of inflammation”].44 In addition, increases in central obesity are significantly correlated with a high level of IL-1β, which is a major proinflammatory cytokine in peri-implant sulcus fluid;45 this increase could explain the lower level of satisfaction with mastication in the obese group, as these patients may have subclinical inflammation induced by these proinflammatory cytokines that leads to their lower satisfaction.
Additionally, adipose tissue, particularly visceral adipose tissue, secretes adipocytokine substances such as tumor necrosis factor-a,46 which can directly affect periodontal tissue and mediates “endotoxin-induced injury” in many organs which periodontal tissue one of them; this effect may also enhance the degradation of periodontium.47 A previous study showed that the concentration of “tumor necrosis factor-a” in the gingival crevicular fluid positively correlated with BMI even in healthy periodontium,48 and many studies have addressed the relation between obesity and periodontics. These findings can also be applied to peri-implantitis, as peri-implantitis and periodontitis are comparable in etiology, microbial flora, diagnosis, and therapy.49
In our study, 92% of the patients were satisfied with their doctor’s performance and communication. Patients evaluated their dentist’s skills and quality of treatment according to their personal interactions, degree of comfort, and dentist’s post-treatment sympathy; these experiences included periods before, during and after treatment.50 Although dentist’s competence is important for patients51 but human communication is still appreciated.52
A relationship between obesity and adverse social communication, depression, body dissatisfaction, self-esteem, reduced levels of optimism and less satisfaction with life has been observed.53 These findings are in accordance with our results, which showed a significant difference between groups in satisfaction level with different psychological aspects (self-respect, social life and psychology).
However, highly significant differences were found between groups regarding satisfaction with improvement in chewing ability, and this finding could be explained by the fact that obese patients have a larger bite size, bite speed, and eating rate, which are positively correlated with obesity and greater body size.54 In addition, maximum occlusal bite is positively correlated with patient weight and height,55 and oral vestibules experience greater pressure on the chewing side than on the non-chewing side.56 These findings indicate that dental implants in obese patients may be subjected to a greater load, and as these patients are more susceptible to increased occurrence of pressure ulcers,40 they may be more vulnerable and susceptible to considerable discomfort in mastication with dental implants.
Additionally, Al-Omiri et al found greater maximum occlusal bite on the dental side with teeth than on the other side with a prosthesis supported by dental implant (P< 0.05); this finding could explain why most of the anthropometric measurements in the current study were correlated negatively with patient satisfaction in terms of occlusion and chewing ability, as these patients believed that their chewing ability would return to its previous strength, and they were less satisfied when they found that their occlusal force with implant-supported prosthesis was lower than when they had natural teeth.55 Although Said et al found a significant increase in patients’ satisfaction with prosthesis supported by dental implant than in prosthesis without implant support, and they also found improvement in masticatory activity and masseter muscle action, but this beneficial effect occurred only on the mandibulectomy side, not on the normal mandible side.57
Certain limitations are found in the current study in which the implant position in the oral cavity was not fixed for all patients neither the number of implants. Adding to this the relatively small number of patients.
Future research that address the limitation in the current study will be valuable for getting further information, the study could be designed as a standardize split mouth study that fix the implant position, number of implant and prosthesis type for each body mass group.
Conclusions
The obese group patients had the lowest rate of patient satisfaction. BMI and other body measurements can be used to predict patient satisfaction with the outcome of dental implant treatment.
Patients satisfaction about improvements in their social life, self-confidence, phonetics, psychology, and chewing ability, correlated negatively with body measurements.
Positive correlation was found between body measurements and satisfaction with prosthesis.
Obese patients need more attention regarding their treatment with dental implants, and critical analyses of their needs should be made before treatment to achieve the best satisfaction level.
Key Messages
Gaining patient satisfactions is an important part in successful dental implant treatment. Patient satisfaction differs depending on the nature of the patient being served, and it is important to know the specific management plan for each patient’s situation.
Acknowledgment
The Authors would like to thank Mustansiriyah University (www.uomustansiriyah.edu.iq), Baghdad, Iraq, for its support in the present work. Also, the Author thank Mrs. Hadhen Abd Al Wahed for her assistance and help.
Funding
The work was self-funded and the study did not receive any financial support from any company or organization.
Disclosure
The author has no conflict of interests.
References
1. Palmer R. Teeth and implants. Br Dent J. 1999;187(4):183–188. doi:10.1038/sj.bdj.4800236
2. Alam MK, Abdul Rahaman S, Basri R, Sing-Yi T, Si-Jie J, Saha S. Dental implants – perceiving patients’ satisfaction in relation to clinical and electromyography study on implant patients. PLoS One. 2015;14:e0143902. doi:10.1371/journal.pone.0143902
3. Strassburger C, Heydecke G, Kerschbaum T. Influence of prosthetic and implant therapy on satisfaction and quality of life: a systematic literature review. Part 1--characteristics of the studies. Int J Prosthodont. 2004;17:83–93.
4. Hindi AR, Bede S. The effect of osseodensification on implant stability and bone density: a prospective observational study. J Clin Exp Dent. 2020;12:e474–e478. doi:10.4317/jced.56727
5. Al-Noori NM, Al-Adili SS, Alnuaimi AS. Evaluation of related factors affecting stability and survival rate of dental implants (meta-analysis of retrospective study). Mustansiria Dent J. 2018;15:105–121.
6. Alattar AN, Bede SYH. Does mixed conventional/piezosurgery implant site preparation affect implant stability? J Craniofac Surg. 2018;29:e472–e475. doi:10.1097/SCS.0000000000004490
7. Strassburger C, Kerschbaum T, Heydecke G. Influence of implant and conventional prostheses on satisfaction and quality of life: a literature review. Part 2: qualitative analysis and evaluation of the studies. Int J Prosthodont. 2006;19:339–348.
8. De Van MM. Methods of procedure in a diagnostic service to the edentulous patient. J Am Dent Assoc. 1942;29:1981–1990. doi:10.14219/jada.archive.1942.0305
9. Sondell K, Soderfeldt B, Palmqvist S. The dentist’s communicative role in prosthodontic treatment. Int J Prosthodont. 2004;17:666–670.
10. Alwan AM, Mousa HA, Talib HJ, Jassim TK. Impact of air and manual scaling on dental anxiety and blood glucose level among diabetic patients. J Int Soc Prev Commun Dent. 2021;11:510–515. doi:10.4103/jispcd.JISPCD_411_20
11. Calnan M, Dickinson M, Manley G. The quality of general dental care: public and users’ perceptions. Qual Health Care. 1999;8:149–153. doi:10.1136/qshc.8.3.149
12. Khorshidi H, Lavaee F, Ghapanchi J, Golkari A, Kholousi S. The relation of preoperative stress and anxiety on patients’ satisfaction after implant placement. Dent Res J. 2017;14:351–355. doi:10.4103/1735-3327.215968
13. Küçük U, Küçük HO, Cüce F, Balta S. Relationship between neck circumference and epicardial fat thickness in a healthy male population. Arq Bras Cardiol. 2016;107:266–270. doi:10.5935/abc.20160112
14. Alswat K, Mohamed WS, Wahab MA, Aboelil AA. The association between body mass index and dental caries: cross-sectional study. J Clin Med Res. 2016;8:147–152. doi:10.14740/jocmr2433w
15. Suvan J, Petrie A, Moles DR, et al. Body mass index as a predictive factor of periodontal therapy outcomes. J Dent Res. 2014;93:49–54. doi:10.1177/0022034513511084
16. Hazem A, Bissada NF, Demko C, Paes A, Lang LA. Comparison of preprosthetic implant complications and failures between obese and non obese patients. Int J Oral Maxillofac Implants. 2016;5:1093–1099. doi:10.11607/jomi.4438
17. Keuroghlian A, Barroso AD, Kirikian G, et al. The effects of hyperlipidemia on implant osseointegration in the mouse femur. J Oral Implantol. 2015;41:e7–e11. doi:10.1563/AAID-JOI-D-13-00105
18. Saito T, Shimazaki Y, Sakamoto M. Obesity and periodontitis. N Engl J Med. 1998;339:482–483. doi:10.1056/NEJM199808133390717
19. Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol 2000. 2005;38:135–187. doi:10.1111/j.1600-0757.2005.00107.x
20. Alabdulkarim M, Bissada N, Al-Zahrani M, Ficara A, Siegel B. Alveolar bone loss in obese subjects. J Int Acad Periodontol. 2005;2:34–38.
21. Shaddox L, Walker CB. Treating chronic periodontitis: current status, challenges, and future directions. Clin Cosmet Investig Dent. 2010;2:79–91. doi:10.2147/CCIDE.S7712
22. Fraser JK, Wulur I, Alfonso Z, Hedrick MH. Fat tissue: an underappreciated source of stem cells for biotechnology. Trends Biotechnol. 2006;24(4):150–154. doi:10.1016/j.tibtech.2006.01.010
23. Currò M, Matarese G, Isola G, et al. Differential expression of transglutaminase genes in patients with chronic periodontitis. Oral Dis. 2014;20(6):616–623. doi:10.1111/odi.12180
24. Isola G, Santonocito S, Distefano A, et al. Impact of periodontitis on gingival crevicular fluid miRNAs profiles associated with cardiovascular disease risk. J Periodontal Res. 2023;58(1):165–174. doi:10.1111/jre.13078
25. Poteser M, Graziani A, Eder P, et al. Identification of a rare subset of adipose tissue-resident progenitor cells, which express CD133 and TRPC3 as a VEGF-regulated Ca2+ entry channel. FEBS Letter. 2008;582(18):2696–2702. doi:10.1016/j.febslet.2008.06.049
26. Kharaeva ZF, Mustafaev MS, Khazhmetov AV, et al. Anti-bacterial and anti-inflammatory effects of toothpaste with Swiss medicinal herbs towards patients suffering from gingivitis and initial stage of periodontitis: from clinical efficacy to mechanisms. Dent J. 2020;8(1):10. doi:10.3390/dj8010010
27. Azab E, Attia A, Yaghmoor W, Aldahlawi S, Youssef AR. The impact of nonsurgical periodontal therapy on serum levels of dickkopf-related protein-1 in smokers and nonsmokers with periodontitis: a prospective comparative study. Clin Cosmet Investig Dent. 2022;14:191–198. doi:10.2147/CCIDE.S362801
28. Ansari Moghadam S, Sarani S, Alijani E, Ansari Moghadam A. The effect of Phase 1 periodontal treatment on the salivary RANKL/OPG ratio in severe chronic periodontitis. Clin Cosmet Investig Dent. 2019;11:251–257. doi:10.2147/CCIDE.S199680
29. Santonocito S, Polizzi A, Palazzo G, Indelicato F, Isola G. Dietary factors affecting the prevalence and impact of periodontal disease. Clin Cosmet Investig Dent. 2021;13:283–292. doi:10.2147/CCIDE.S288137
30. Al-Zain AO, Fakhry LM, Tallab RA, Natto ZS. Attitude, practice, and knowledge regarding fluoridated toothpaste, brushing, and rinse usage among residents of Jeddah City in Saudi Arabia. Patient Prefer Adherence. 2023;17:23–39. doi:10.2147/PPA.S389413
31. Chaffin JG, Chaffin SD, Mangelsdorff AD, Finstuen K. Patient satisfaction with dental hygiene providers in US military clinics. J Dent Hyg. 2007;8:1–9.
32. AL-Noori NM, Abdulmunem MM, Ibraheem NS. Evaluation of the cause and pattern of teeth extraction in the college of dentistry, Mustansiriyah University. J Res Med Dent Sci. 2021;9:10–15.
33. Shrivastava R, Srivastava R, Shigli K, Prashanth MB, Kumaraswamy BN, Nethravathi TD. Assessment of dental anxiety and its correlation with denture satisfaction in edentulous patients. J Contemp Dent Pract. 2012;13:257. doi:10.5005/jp-journals-10024-1133
34. Akinbami BO, Didia BC. Analysis of body mass index, the mandible, and dental alveolar arch factors in prediction of mandibular third molar impaction: a pilot study. J Contemp Dent Pract. 2010;11:E041–E048. doi:10.5005/jcdp-11-6-41
35. Li HX, Zhang F, Zhao D, et al. Neck circumference as a measure of neck fat and abdominal visceral fat in Chinese adults. BMC Public Health. 2014;14:311. doi:10.1186/1471-2458-14-311
36. Yang GR, Yuan SY, Fu HJ, et al. Beijing Community Diabetes Study Group Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing Community Diabetes Study 4. Diabetes Care. 2010;33:2465–2467. doi:10.2337/dc10-0798
37. Chala S, El Aidouni M, Abouqal R, Abdallaoui F. U-shaped association between untreated caries and body mass index in adults at Rabat dental University hospital, Morocco: cross sectional study. BMC Res Notes. 2017;10:5. doi:10.1186/s13104-016-2356-0
38. Pjetursson BE, Karoussis I, Bürgin W, Brägger U, Lang NP. Patients’ satisfaction following implant therapy. Clin Oral Implants Res. 2005;16:185–193. doi:10.1111/j.1600-0501.2004.01094.x
39. Wilson JA, Clark JJ. Obesity: impediment to wound healing. Crit Care Nurs. 2003;26:119–132.
40. Wilson JA, Clark JJ. Obesity: impediment to postsurgical wound healing. Adv Skin Wound Care. 2004;17:426–435. doi:10.1097/00129334-200410000-00013
41. Wee C, Phillips R, Cook F, et al. Influence of body weight on patient’s satisfaction with ambulatory care. J Gen Intern Med. 2002;17:155–159. doi:10.1046/j.1525-1497.2002.00825.x
42. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6:438–446. doi:10.1016/S1473-3099(06)70523-0
43. Maury E, Brichard SM. Adipokine dysregulation, adipose tissue inflammation and metabolic syndrome. Mol Cell Endocrinol. 2010;314:1–16. doi:10.1016/j.mce.2009.07.031
44. Johnson RB, Serio FG. Leptin within healthy and diseased human gingiva. J Periodontol. 2001;72:1254–1257. doi:10.1902/jop.2000.72.9.1254
45. Elangovan S, Brogden KA, Dawson DV, et al. Body fat indices and biomarkers of inflammation: a cross-sectional study with implications for obesity and peri-implant oral health. Int J Oral Maxillofac Implants. 2014;29:1429–1434. doi:10.11607/jomi.3758
46. Shimomura I, Funahashi T, Takahashi M, et al. Enhanced expression of PAI-1 in visceral fat: possible contributor to vascular disease in obesity. Nat Med. 1996;2:800–803. doi:10.1038/nm0796-800
47. Gemmell E, Marshall RI, Seymour GJ. Cytokines and prostaglandins in immune homeostasis and tissue destruction in periodontal disease. Periodontol. 1997;14:112–143. doi:10.1111/j.1600-0757.1997.tb00194.x
48. Lundin M, Yucel-Lindberg T, Dahllof G, Marcus C, Modeer T. Correlation between TNFalpha in gingival crevicular fluid and body mass index in obese subjects. Acta Odontol Scand. 2004;62:273–277. doi:10.1080/00016350410000172
49. Heitz-Mayfield LJ, Lang NP. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol. 2010;53:167–181. doi:10.1111/j.1600-0757.2010.00348.x
50. Riley J, Gordan V, Rindal D, et al. Components of patient satisfaction with a dental restorative visit: results from The Dental Practice- Based Research Network. J Am Dent Assoc. 2012;143:1002–1010. doi:10.14219/jada.archive.2012.0329
51. Goedhart H, Eijkman MA, ter Horst G. Quality of dental care: the view of regular attenders. Community Dent Oral Epidemiol. 1996;24:28–31. doi:10.1111/j.1600-0528.1996.tb00808.x
52. Dewi FD, Sudjana G, Oesman YM. Patient satisfaction analysis on service quality of dental health care based on empathy and responsiveness. Dent Res J. 2011;8:172–177. doi:10.4103/1735-3327.86032
53. Horsten M, Mittleman MA, Wamala SP, Schenck-Gustafsson K, Orth-Gomér K. Social relations and the metabolic syndrome in middle-aged Swedish women. J Cardiovasc Risk. 1999;6:391–397. doi:10.1177/204748739900600606
54. Porter Starr K, Fischer JG, Johnson MA. Eating behaviors, mental health, and food intake are associated with obesity in older congregate meal participants. J Nutr Gerontol Geriatr. 2014;33:340–356. doi:10.1080/21551197.2014.965375
55. Al-Omiri MK, Sghaireen MG, Alhijawi MM, Alzoubi IA, Lynch CD, Lynch E. Maximum bite force following unilateral implant-supported prosthetic treatment: within-subject comparison to opposite dentate side. J Oral Rehabil. 2014;41:624–629. doi:10.1111/joor.12174
56. Nishiura M, Ono T, Yoshinaka M, Fujiwara S, Yoshinaka M, Maeda Y. Pressure production in oral vestibule during gum chewing. J Oral Rehabil. 2015;42:900–905. doi:10.1111/joor.12328
57. Said MM, Otomaru T, Sumita Y, Leung KC, Khan Z, Taniguchi H. Systematic review of literature: functional outcomes of implant-prosthetic treatment in patients with surgical resection for oral cavity tumors. J Investig Clin Dent. 2016;8. doi:10.1111/jicd.12207
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
