Back to Journals » International Journal of General Medicine » Volume 15
Association of Office and Ambulatory Blood Pressure with Left Ventricular Structure and Function in Hypertensive Patients
Authors Sang Z, Zeng X, Yuan X, Wang X, Fu L, Zhuang W
Received 13 January 2022
Accepted for publication 1 April 2022
Published 4 May 2022 Volume 2022:15 Pages 4649—4656
DOI https://doi.org/10.2147/IJGM.S357508
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zhuo Sang, Xianli Zeng, Xiaohui Yuan, Xiaolin Wang, Liancong Fu, Wenwen Zhuang
Department of General Practice, Huizhou Municipal Central Hospital, Huizhou, Guangdong, People’s Republic of China
Correspondence: Zhuo Sang, Department of General Practice, Huizhou Municipal Central Hospital, Huizhou, Guangdong, People’s Republic of China, Tel +86-752-2288288, Email [email protected]
Objective: The current study was to evaluate the association of office blood pressure (OBP) and 24h ambulatory blood pressure (ABP) with left ventricular (LV) structure and function in hypertensive patients. Whether the association was modified by sex was also evaluated.
Methods: A total of 694 hypertensive patients without cardiovascular disease were retrospectively included from the inpatient clinic. Regression analysis was performed to evaluate the association of OBP and 24h ABP parameters with LV mass index (LVMi), e’ velocity and left ventricular hypertrophy (LVH) with adjustment for covariates including age, obesity, diabetes mellitus, obstructive sleep apnea, estimated glomerular filtration rate and antihypertensive drugs.
Results: There was no difference in OBP by sex. Compared to women, men had a higher 24h (132.6 ± 11.3 vs 129.3 ± 10.0 mm Hg), daytime (136.6 ± 12.9 vs 132.8 ± 9.5 mm Hg) and nighttime (130.3 ± 9.2 vs 125.1 ± 6.6 mm Hg) SBP. The proportion of patients with non-dipping pattern and reverse dipper pattern was also higher in men. In the overall participants, 24h, daytime and nighttime SBP, non-dipping and reverse dipper pattern were associated with LVMi, e’ velocity and LVH, which were not observed in OBP. The magnitude of the association between 24h, daytime and nighttime SBP, non-dipping and reverse dipper pattern with LVMi, e’ velocity and LVH was stronger in men than in women (P-value for interaction < 0.05).
Conclusion: Twenty-four-hour ABP appears to be better than OBP in association with LV structural and functional alterations, and this association was modified by sex.
Keywords: office blood pressure, ambulatory blood pressure, sex, cardiac structure, cardiac function
Introduction
Hypertension is a major risk factor of cardiovascular morbidity and mortality in China and worldwide.1–3 According to the China Hypertension Survey,4 the number of adults with hypertension is nearly 245 million. Elevated blood pressure (BP) causes left ventricular (LV) structural and functional alteration, which predisposes hypertensive patients developing heart failure.5,6 Therefore, evaluating LV structure and function is important to predict the prognosis for hypertensive populations.
Prior studies have reported the relationship between BP and parameters of LV structure and function based on office BP (OBP).7–11 The association between 24h ambulatory blood pressure (ABP) and LV structure and function was less investigated. In addition, participants of these studies were almost White populations, and data on the Chinese population are remarkably limited. Numerous studies have reported racial and ethnic disparities in cardiac remodeling.12,13 Therefore, it is clinically relevant to evaluate the association between BP and LV structure and function in Chinese hypertensive patients, considering the increasing prevalence of hypertension and associated health complication in China.14,15
Several studies have reported the sex-differences in LV structural and functional alteration with elevated OBP.16–18 However, whether there were differences in the association between 24h ABP and LV structural and functional alteration by sex was undetermined. Herein, we conducted a retrospective study to evaluate the association of OBP and 24h ABP with LV structure and function in hypertensive patients without overt cardiovascular diseases. In addition, we evaluated whether the association was modified by sex.
Methods
Study Participants
The current study was approved by the Institution Review Board of the Huizhou Municipal Central Hospital. Since this was a retrospective study, no consent form was obtained, and the Ethnic Committee of Huizhou Municipal Central Hospital waived the consent form. Patient’s data were keeping confidentiality and all the performances were in accordance with the Declaration of Helsinki.19 Hypertensive patients in the inpatient clinic of our hospital between July 2019 and July 2021 were screened for the eligibility of the current study. The inclusion criteria were as follows: hypertensive patients who 1) were receiving antihypertensive drug; 2) had transthoracic echocardiographic examination in recent 1 month of index inpatient visit; and 3) had 24h ABP measurements in recent 1 month of index inpatient visit. The exclusion criteria were as follows: 1) documented secondary hypertension and 2) documented cardiovascular disease, including coronary heart disease, myocardial infarction, ischemic stroke, intracranial hemorrhage, heart failure, valvular heart disease, hypertrophy, dilated or restrictive cardiomyopathy, myocarditis, congenital heart disease, pulmonary hypertension, or pericardial disease.
Transthoracic Echocardiographic Parameters
Transthoracic echocardiographic parameters were extracted from electronic health record of inpatient clinic system. Parameters used in the current analysis included left atria diameter (LAd), LV end systolic and diastolic diameter (LVESd and LVEDd), LV mass index (LVMi), relative wall thickness (RWT), LV ejection fraction (LVEF), lateral mitral annular diastolic velocity e’, and E/e’ ratio. Specifically, RWT = (posterior wall thickness [PWT] + interventricular septal thickness [IVST])/LVEDd. LV mass (LVM)=0.8*[1.04 *([LVEDd + IVST + PWT] 3 – LVEDd3)] + 0.6 and LVMi=LVM/body surface area (BSA). LVMi ≥115 g/m2 for men and ≥95 g/m2 for women were defined as LV hypertrophy (LVH). Based on the value RWT of (≤0.42 or >0.42) and the presence of LVH, LV geometry was classified into normal (RWT ≤ 0.42 and LVH absence), concentric remodeling (RWT > 0.42 and LVH absence), concentric hypertrophy (RWT > 0.42 and LVH presence), and eccentric hypertrophy (RWT ≤ 0.42 and LVH presence), respectively.20
Office Blood Pressure and 24h Ambulatory Blood Pressure
BP parameters were extracted from medical health record in the clinic system. In brief, according to the China Hypertension Guideline, OBP was measured two times with 1-minute interval and the average value of these two BP readings was used. If the first two BP readings differed by more than 10 mm Hg, the third measurement was performed and the average of the three readings was used. Parameters of 24h ABP included daytime, nighttime and 24h systolic and diastolic BP (SBP and DBP). Patients with a nighttime-to-daytime ratio of SBP and/or DBP ≤0.90 were defined as having a dipping pattern, and those with a ratio >0.90 were defined as having a non-dipping pattern, and those with nighttime BP higher than daytime BP was defined as reverse dipper.21
Data Collection
Structured questionnaire was used to collect data at baseline. Data, which included demographics (age and sex), anthropometrics (body weight and height), comorbidities (smoking, obesity, dyslipidemia, diabetes mellitus and obstructive sleep apnea), laboratory and medications used, were collected by two independent investigators. Body mass index (BMI) was calculated as Weight/Height2, and BMI ≥28 kg/m2 was defined as obesity for Chinese populations,22 and BSA was calculated as (Weight 0.425 * Height 0.725) * 0.007184.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD) and between-group differences were assessed using Student t-test, and categorical variables were presented as number (percentage) and between-group differences were assessed by Chi-Square test or Fisher’s exact test. Linear regression analysis was performed to evaluate the association between per 1-SD change of OBP and 24h ABP with LVMi and e’ velocity with adjustment for potential covariates including age, obesity, diabetes mellitus, obstructive sleep apnea, estimated glomerular filtration rate (eGFR) and antihypertensive drugs. Multivariable regression analysis was performed to evaluate the association between per 1-SD change of OBP and 24h ABP with LVH, with adjustment for covariates including age, obesity, diabetes mellitus, obstructive sleep apnea, eGFR and antihypertensive drugs. These associations were also assessed by sex and a P-value for interaction was reported. All the statistical analyses were performed using SPSS 23.0 package and a two-sided P value <0.05 was considered as statistical significance.
Results
Baseline Characteristics
A total of 694 patients were enrolled for the current analysis (Figure 1). Baseline characteristics of all participants are presented in Table 1. The mean age was 62.9 years and women accounted for 36.3%. Compared to men, women were younger and less likely to smoke, had a higher triglyceride level, and were less likely to receive calcium channel blocker and more likely to receive beta-blocker.
 |
Table 1 Baseline Characteristics |
 |
Figure 1 Study flowchart. |
Echocardiographic Parameters
As presented in Table 2, 37.2% of the participants had LVH, and among these participants, 25.2% and 12.0% had concentric and eccentric LVH, respectively. Compared to men, women had a smaller LVESd and LVEDd and LVMi. In addition, women were less likely to have concentric LVH (8.3% vs 14.0%) while they had a higher e’ velocity (9.5 cm vs 9.0 cm).
 |
Table 2 Echocardiographic Parameters |
Parameters of OBP and 24h ABP
As shown in Table 3, there was no difference in office SBP and DBP between men and women. However, compared to women, men had a higher 24h (132.6 ± 11.3 vs 129.3 ± 10.0 mm Hg), daytime (136.6 ± 12.9 vs 132.8 ± 9.5 mm Hg) and nighttime (130.3 ± 9.2 vs 125.1 ± 6.6 mm Hg) SBP. There was no difference in 24h, daytime and nighttime DBP by sex. In addition, the proportion of patients with non-dipping (34.6% vs 29.0%) and reverse dipper pattern (16.7% vs 11.9%) was also higher in men than in women.
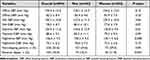 |
Table 3 Parameters of OBP and 24h ABP |
The Relationship Between OBP and 24h ABP with LVMi and e’ Velocity
In the overall participants, 24h, daytime and nighttime SBP, non-dipping and reverse dipper pattern were significantly associated with LVMi and e’ velocity, and no association was observed in OBP (Table 4). The magnitude of the association between 24h, daytime and nighttime SBP, non-dipping and reverse dipper pattern with LVMi was stronger in men than in women (P-value for interaction <0.05), as was e’ velocity (P-value for interaction <0.05). Notably, there was no association between 24h, daytime and nighttime DBP with LVMi and e’ velocity.
 |
Table 4 Association Between OBP and 24h ABP with LVMi and e’ Velocity |
The Relationship Between OBP and 24h ABP with LVH
In the overall participants, 24h, daytime and nighttime SBP, and non-dipping and reverse dipper pattern were significantly associated with LVH, and no association was observed in OBP (Table 5). The magnitude of the association between 24h, daytime and nighttime SBP, non-dipping and reverse dipper pattern with LVH was stronger in men than in women (P-value for interaction <0.05). However, there was no association between 24h, daytime and nighttime DBP with LVH.
 |
Table 5 Association Between OBP and 24h ABP with LVH |
Discussion
The current study, to the best of our knowledge, should be the first few studies to evaluate the association between 24h ABP and the LV structure and function in hypertensive patients without cardiovascular disease. There are three important findings. First, compared to OBP, 24h ABP appears to be more closely associated with LV structure and function. Second, among 24h ABP parameters, only 24h, daytime and nighttime SBP were associated with LV structure and function after adjusted for multiple covariates. Third, the magnitude of these associations was stronger in men than in women.
There are three potentially clinically important implications of the current study. First of all, compared to OBP, 24h ABP provided additional valuable information in assessing the association between elevated BP and LV structural and functional alterations, suggesting that 24h ABP parameters could provide additional information for prognostic assessment. It might be appropriate to apply 24h ABP for hypertensive patients with high cardiovascular risk in daily clinical practice. Second, SBP was better than DBP in terms of their correlations with LV structural and functional alterations. These findings demonstrate that ambulatory SBP might be more relevant than ambulatory DBP to assess the association between elevated ABP and LV structure and function. Third, elevated ambulatory SBP had stronger effects on LV structural and functional alteration in men than in women, indicating that men might require more intensive SBP lowering than their female counterparts to prevent LV structural and functional alteration.
Numerous studies have evaluated the association between elevated OBP with LV structure and function. For example, Lauer et al reported that in the Framingham Heart Study, 30-year average office DBP was correlated with LVM but to a lesser degree than office SBP.23 Savage et al reported that office SBP was associated with LVM in both sexes.24 Based on OBP, Cuspidi et al classified participants into normotension, prehypertension and hypertension. After 10 years’ follow-up, they found that the incidence of LVH increased progressively from the normotensive to prehypertension and hypertension group (9.0%, 23.2%, and 36.5%, respectively).25 Li et al recently evaluated the cardiac and vascular responses to elevated OBP in Chinese populations without cardiovascular disease.16 The results suggest that LV structural and functional alteration was stronger in women than in men. Cai et al evaluated the age-related LV structural and functional alteration by sex in different office SBP level.7 The results suggest that lower office SBP level attenuated the sex-difference in LV structural and functional alterations with age. These results demonstrate the effects of elevated OBP on LV structural and functional alteration.26
Compared to OBP, 24h ABP can provide additional information on BP assessment outside of office. For example, OBP only assesses BP in the clinic, while 24h ABP is useful to evaluate BP around the day. In addition, 24h ABP provides information on nighttime BP during sleep, and the daytime and nighttime BP ratio can be used to determine the BP pattern, which has been associated with prognosis.27–29 Despite these advantages, 24h ABP has not been routinely used for all hypertensive patients in daily clinical practice due to the cost and feasibility in many remote areas. In the current study, we retrospectively evaluated the association between OBP and 24h ABP with LV structure and function in hypertensive patients without cardiovascular diseases. Our results indicated that only 24h SBP was associated with LVMi and e’ velocity. In addition, daytime and nighttime SBP, non-dipping and reverse dipper pattern were associated with LVMi and e’ velocity. Notably, the β-coefficient was larger in 24h, daytime and nighttime SBP compared to office SBP, suggesting that 24h ABP might be more closely related to LV structural and functional alteration than OBP. In addition, when evaluating the association by sex, there was no significant interaction in office SBP. However, in 24h, daytime and nighttime SBP, the association with LVMi and e’ velocity was stronger in men than in women. We then evaluated the association between OBP and 24h ABP with LVH, and the findings were consistent with above results. Taken together, these findings demonstrate that 24h ABP provided additional value in evaluating the influence of elevated BP on LV structural and functional alteration in hypertensive patients. Further studies are needed to corroborate the current findings.
There are some limitations of the current study. First, this was a retrospective study, and the findings cannot be drawn any causal relationship and can only be used for hypothesis generation. Second, although we have adjusted for multiple covariates, some unmeasured and unknown covariates might exist and influence the findings. Third, the current findings might not be extrapolated to other racial and ethnic groups. Last but not the least, all participants in the current study were without cardiovascular disease and whether these findings can be extrapolated to those with cardiovascular disease is unknown.
Conclusion
In conclusion, the current study shows that in hypertensive patients without cardiovascular disease, 24h ABP appears to be better than OBP in reflecting the relationship between elevated BP and LV structural and functional alterations. In addition, there was difference in the association between 24h ABP and LV structural and functional alterations by sex.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liu LS, Wu ZS, Wang JG, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16(3):182–241. doi:10.11909/j.issn.1671-5411.2019.03.014
2. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi:10.1093/eurheartj/ehy339
3. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71(6):e13–e115. doi:10.1161/HYP.0000000000000065
4. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi:10.1161/CIRCULATIONAHA.117.032380
5. Sorrentino MJ. The evolution from hypertension to heart failure. Heart Fail Clin. 2019;15(4):447–453. doi:10.1016/j.hfc.2019.06.005
6. Slivnick J, Lampert BC. Hypertension and heart failure. Heart Fail Clin. 2019;15(4):531–541. doi:10.1016/j.hfc.2019.06.007
7. Cai A, Zhou D, Liu L, Zhou Y, Tang S, Feng Y. Age-related alterations in cardiac and arterial structure and function in hypertensive women and men. J Clin Hypertens. 2021;23(7):1322–1334. doi:10.1111/jch.14262
8. Soliman EZ, Byington RP, Bigger JT, et al. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with diabetes mellitus: action to control cardiovascular risk in diabetes blood pressure trial. Hypertension. 2015;66(6):1123–1129. doi:10.1161/HYPERTENSIONAHA.115.06236
9. von Jeinsen B, Vasan RS, McManus DD, Mitchell GF, Cheng S, Xanthakis V. Joint influences of obesity, diabetes, and hypertension on indices of ventricular remodeling: findings from the community-based Framingham Heart Study. PLoS One. 2020;15(12):e0243199. doi:10.1371/journal.pone.0243199
10. Upadhya B, Rocco MV, Pajewski NM, et al. Effect of intensive blood pressure reduction on left ventricular mass, structure, function, and fibrosis in the SPRINT-HEART. Hypertension. 2019;74(2):276–284. doi:10.1161/HYPERTENSIONAHA.119.13073
11. Cao X, Broughton ST, Waits GS, Nguyen T, Li Y, Soliman EZ. Interrelations between hypertension and electrocardiographic left ventricular hypertrophy and their associations with cardiovascular mortality. Am J Cardiol. 2019;123(2):274–283. doi:10.1016/j.amjcard.2018.10.006
12. Park CM, March K, Ghosh AK, et al. Left-ventricular structure in the Southall And Brent REvisited (SABRE) study: explaining ethnic differences. Hypertension. 2013;61(5):1014–1020. doi:10.1161/HYPERTENSIONAHA.111.00610
13. Poppe KK, Doughty RN, Gardin JM. Ethnic-Specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL Study. JACC Cardiovasc Imaging. 2015;8(6):656–665. doi:10.1016/j.jcmg.2015.02.014
14. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–2558. doi:10.1016/S0140-6736(17)32478-9
15. Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176(4):524–532. doi:10.1001/jamainternmed.2016.0190
16. Li Z, Liu J, Shen J, et al. Sex-specific cardiac and vascular responses to hypertension in Chinese populations without overt cardiovascular diseases. Postgrad Med. 2020;133(2):181–187. doi:10.1080/00325481.2020.1835037
17. Tadic M, Cuspidi C, Grassi G. The influence of sex on left ventricular remodeling in arterial hypertension. Heart Fail Rev. 2019;24(6):905–914. doi:10.1007/s10741-019-09803-3
18. Guzik P, Schneider A, Piskorski J, et al. Sex differences in excess and reservoir arterial blood pressures as markers of phenotype. J Hypertens. 2019;37(11):2159–2167. doi:10.1097/HJH.0000000000002135
19. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
20. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–270. doi:10.1093/ehjci/jev014
21. Cai A, Zhong Q, Liu C, et al. Associations of systolic and diastolic blood pressure night-to-day ratios with atherosclerotic cardiovascular diseases. Hypertens Res. 2016;39(12):874–878. doi:10.1038/hr.2016.82
22. Consultation WE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi:10.1016/S0140-6736(03)15268-3
23. Lauer MS, Anderson KM, Levy D. Influence of contemporary versus 30-year blood pressure levels on left ventricular mass and geometry: the Framingham Heart Study. J Am Coll Cardiol. 1991;18(5):1287–1294. doi:10.1016/0735-1097(91)90549-O
24. Savage DD, Levy D, Dannenberg AL, Garrison RJ, Castelli WP. Association of echocardiographic left ventricular mass with body size, blood pressure and physical activity (the Framingham Study). Am J Cardiol. 1990;65(5):371–376. doi:10.1016/0002-9149(90)90304-J
25. Cuspidi C, Facchetti R, Bombelli M, et al. High normal blood pressure and left ventricular hypertrophy echocardiographic findings from the PAMELA population. Hypertension. 2019;73(3):612–619. doi:10.1161/HYPERTENSIONAHA.118.12114
26. Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29(1):1–6. doi:10.1038/jhh.2014.36
27. Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73(5):e35–e66. doi:10.1161/HYP.0000000000000087
28. Huang QF, Yang WY, Asayama K, et al. Ambulatory blood pressure monitoring to diagnose and manage hypertension. Hypertension. 2021;77(2):254–264. doi:10.1161/HYPERTENSIONAHA.120.14591
29. Melville S, Byrd JB. Out-of-office blood pressure monitoring in 2018. JAMA. 2018;320(17):1805–1806. doi:10.1001/jama.2018.14865
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
