Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
Association of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio with Diabetic Kidney Disease in Chinese Patients with Type 2 Diabetes: A Cross-Sectional Study
Received 12 October 2022
Accepted for publication 14 December 2022
Published 28 December 2022 Volume 2022:18 Pages 1157—1166
DOI https://doi.org/10.2147/TCRM.S393135
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Lan Li,1 Qing Shen,1 Sijie Rao2
1Department of Nephrology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, 400016, People’s Republic of China; 2Department of Nephrology, The Yongchuan Hospital of Chongqing Medical University, Chongqing, 402160, People’s Republic of China
Correspondence: Qing Shen, Department of Nephrology, The First Affiliated Hospital of Chongqing Medical University, No. 1, Youyi Road, Chongqing, 400016, People’s Republic of China, Tel +86 13508304817, Fax +86 023 89012019, Email [email protected]
Purpose: The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have been extensively studied in a variety of diseases. However, research on their relationship with diabetic kidney disease (DKD) is limited. The aim of our study was to investigate the association between these two indicators and renal function in Chinese patients with type 2 diabetes and assess whether they can serve as predictors of DKD.
Methods: This cross-sectional study enrolled 655 Chinese patients with type 2 diabetes. Subjects were divided into three groups according to the urinary albumin-to-creatinine ratio (UACR). The differences in the NLR and PLR among the groups and their correlation with renal function were analyzed. Logistic regression analysis was used to analyze independent risk factors for DKD, and receiver operating characteristic (ROC) curves were used to assess the predictive values of the NLR and PLR for the disease.
Results: The NLR and PLR were significantly different among the three groups, and they increased with increasing levels of albuminuria. Pearson’s correlation analysis showed that the NLR and PLR were positively correlated with the UACR but negatively correlated with the estimated glomerular filtration rate (eGFR) (p< 0.001). Logistic regression analysis showed that these two indicators were independent risk factors for DKD (p< 0.001). The results of ROC curve analysis suggested that the NLR (AUC=0.794; 95% CI, 0.760– 0.827; p< 0.001) and PLR (AUC=0.665; 95% CI, 0.623– 0.706, p< 0.001) had important diagnostic value for DKD.
Conclusion: The NLR and PLR were closely associated with renal function among Chinese patients with type 2 diabetes, and high NLR and PLR values may serve as predictors of DKD.
Keywords: diabetic kidney disease, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, renal function, inflammation
Introduction
Diabetes is a chronic, systemic metabolic disease of global concern. As the number of people with diabetes increases worldwide, the prevalence of diabetic kidney disease (DKD) as its microvascular complication increases each year. Approximately one-third of patients with diabetes develop DKD, which has become the leading cause of end-stage renal disease.1 In addition to renal risk, DKD significantly increases the rate of infection and the incidence of cardiovascular events and decreases the quality of life,2 which emphasizes the necessity of early diagnosis and proper therapy. Therefore, considerable attention has been given to the search for biomarkers associated with the onset and progression of DKD.
The etiology of DKD is multifactorial, with chronic inflammation playing an important role in its onset and development.3,4 Metabolic disorders in patients with diabetes activate inflammatory signals in the body, and elevated levels of multiple inflammatory factors drive inflammation and are involved in kidney injury.5 Studies have shown that the pathogenesis of DKD is associated with altered levels of inflammatory cytokines, such as interleukins and tumor necrosis factor.6 However, they are not routinely measured due to the costs and technical difficulties in clinical application. The neutrophil-to-lymphocyte ratio (NLR), calculated by leukocyte count, is regarded as a cost-effective, readily measurable indicator of inflammatory status and is considered a predictor of inflammatory burden in diabetes mellitus, cardiac conditions, inflammatory bowel disease, thyroiditis, diabetic foot ulcers and SARS COV-2 infection.7–12 Similarly, the platelet-to-lymphocyte ratio (PLR) has been introduced as a novel hemogram-derived inflammatory indicator in various diseases, such as liver fibrosis, cancer, diabetes mellitus and COVID-19 infection.13–16
Although the NLR and PLR have been shown to be closely related to the progression and prognosis of a variety of diseases, research on their association with DKD is limited. Furthermore, their clinical significance in DKD has not yet been established. Therefore, the aim of our study was to investigate the association between these two indicators and renal function in Chinese patients with type 2 diabetes. In addition, we investigated whether they are independent risk factors for DKD and assessed their potential as predictors of this disease.
Patients and Methods
This cross-sectional study enrolled 655 adult patients with type 2 diabetes who were admitted to the First Affiliated Hospital of Chongqing Medical University from January 2018 to January 2021. The diagnosis of type 2 diabetes was in accordance with World Health Organization diagnostic criteria. The diagnosis of DKD was in accordance with KDIGO guidelines,17 that is, DKD was defined as a persistent urinary albumin-to-creatinine ratio (UACR) ≥30 mg/g and/or a persistent reduction in estimated glomerular filtration rate (eGFR) to below 60 mL/min/1.73m2 for more than three months.
For all these individuals, patients with acute complications of diabetes, acute or chronic infection, acute coronary artery disease, heart failure, cancer, hematologic disorders that affect blood cell counts (eg, leukemia), diseases that affect urinary protein excretion (eg, nephrotic syndrome), and autoimmune disorders were excluded. Patients taking drugs that affect blood counts (eg, steroids) were also excluded. The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (Approval Number: 2022-K391). Informed consent was obtained from each subject.
Information on sex, age, the duration of diabetes, medications (eg, antidiabetic drugs and lipid-lowering agents), height and weight was recorded from the case history, and body mass index (BMI) was calculated by dividing weight by the square of the height. Fasting venous blood was obtained on the second day after admission. Blood cell characteristics, including neutrophil, lymphocyte and platelet levels, were measured with SYSMEX XE-2100. The NLR and PLR were calculated. Glycated hemoglobin (HbA1c) levels were measured with Premier Hb9210. Biochemical parameters, including the levels of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), serum creatinine (Scr), blood urea nitrogen (BUN), serum uric acid (SUA) and fasting plasma glucose (FPG), were measured with Beckman AU5800. Morning urine samples were collected to measure the levels of urine albumin and creatinine, and the UACR was calculated. The eGFR was calculated using the equation of Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI).18
Subjects were divided into three groups according to the UACR as follows: normoalbuminuria (UACR<30 mg/g, 290 cases); microalbuminuria (UACR=30–300 mg/g, 190 cases); and macroalbuminuria (UACR ≥300 mg/g, 175 cases). According to the KDIGO guidelines, patients in the latter two groups were clinically diagnosed with DKD.
The Kolmogorov‒Smirnov test was used for normality analysis. Continuous variables conforming to a normal distribution were presented as the mean ± standard deviation, and group comparisons were performed via one-way analysis of variance (ANOVA). Categorical variables were presented as frequencies, and the chi-square test was used for comparisons among groups. Pearson’s correlation analysis was used to determine correlations among the NLR, PLR and renal function indexes. Independent risk factors for DKD were determined by logistic regression analysis. The results are presented as odds ratios (ORs) and 95% confidence intervals (CIs). Receiver operating characteristic (ROC) curve analysis was used to determine the optimum cutoff levels of the NLR and PLR to predict DKD. The results with a P value <0.05 were considered statistically significant. SPSS statistical software (SPSS for Windows, version 26.0) was used for data analysis.
Results
Characteristics of Subjects Categorized According to the UACR
A total of 655 patients were enrolled in our study. There were 351 men and 304 women, and their mean age was 59.94±10.63 years old. The distributions of the NLR and PLR among the three groups are shown in Figure 1A and B, respectively. The NLR and PLR values were significantly higher in those with microalbuminuria and those with macroalbuminuria than in those with normoalbuminuria (p<0.001). Table 1 summarizes the one-way ANOVA results. The duration of diabetes, white blood cell (WBC) count, neutrophil count, NLR, and PLR and the Scr, BUN, TG, LDL-C, FPG and HbA1c levels were higher and correlated with increased UACR. However, the lymphocyte count and eGFR were lower (all p<0.05). The proportion of patients taking angiotensin-converting-enzyme (ACE) inhibitors and angiotensin-receptor blockers (ARBs) were significantly higher in those with microalbuminuria and those with macroalbuminuria than in those with normoalbuminuria (p<0.001). However, no significant intergroup difference was observed regarding sex, age, BMI, blood pressure, platelet count or SUA, TC, HDL-C levels or in the proportion of patients taking statins and antidiabetic drugs.
 |
Table 1 Characteristics of Subjects Categorized by the UACR |
Relationships Among the NLR, PLR and Renal Function Indexes
We observed a positive correlation between the UACR and NLR (r=0.508, p<0.001), whereas there was a negative correlation between the eGFR and NLR (r=−0.386, p<0.001). We also observed a positive correlation between the PLR and the UACR and a negative correlation between the PLR and the eGFR (r=0.287 and r=−0.166, respectively, all p<0.001) (Table 2). We can draw the same conclusion as that resulting from the data in Figure 2.
 |
Table 2 Pearson’s Correlation Analysis Between NLR, PLR and Renal Function Indexes |
 |
Figure 2 Relationship between NLR, PLR and renal function indexes. Relationship between NLR and UACR (A), between NLR and eGFR (B), between PLR and UACR (C), between PLR and eGFR (D). |
Risk Factors for DKD in Patients with Type 2 Diabetes
Further logistic regression analysis of the factors with results of p<0.05 in Table 1 was performed to determine the risk factors for DKD in type 2 diabetes patients. The results showed that the independent risk factors included the duration of diabetes, NLR (OR, 3.137; 95% CI, 1.955–5.033; p<0.001), PLR (OR, 1.008; 95% CI, 1.000–1.015; p<0.001) and Scr, LDL-C and HbA1c levels (Table 3).
 |
Table 3 Risk Factors for DKD in Patients with Type 2 Diabetes |
Receiver Operating Characteristics Curve Analysis
Figure 3 shows the diagnostic ability of the NLR and PLR for DKD, as analyzed by the ROC curve. The areas under the ROC curves were 79.4% for the NLR and 66.5% for the PLR. The cutoff with the largest Youden index of the NLR was 2.46 (sensitivity of 76.2% and specificity of 70.7%), and the cutoff with the largest Youden index of the PLR was 125.04 (sensitivity of 51.5% and specificity of 75.5%).
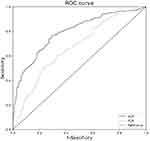 |
Figure 3 Receiver operating characteristic (ROC) curve analysis of NLR and PLR for DKD prediction. |
Discussion
DKD is a common diabetic microvascular complication with insidious early symptoms. Diagnosis is mainly based on albuminuria and a progressive decline in eGFR, which can be confirmed by renal biopsy. However, renal biopsy is an invasive operation. Additionally, urinary albumin excretion is affected by exercise, fever, urinary tract infection and other factors, and the eGFR changes relatively slowly. Therefore, it is important to identify related biomarkers to detect patients at risk for DKD at a relatively early stage.
Accumulated evidence has implicated that chronic inflammation plays a key role in DKD and that inflammatory indicators may contribute to the diagnosis and prognostic assessment of the disease. Novel predictors of inflammation, such as the C-reactive protein to serum albumin ratio and the fibrinogen to albumin ratio, are considered to be independent risk factors for the progression of DKD.19,20 In addition, some hemogram-derived inflammatory markers are thought to be associated with the development and progression of DKD. For example, the monocyte-to-lymphocyte ratio (MLR) is positively correlated with microalbuminuria in patients with type 2 diabetes and may serve as a predictor of renal injury.21 The NLR and PLR, also derived from hemogram, are considered cost-effective, readily measured predictors of inflammatory burden in various diseases. Recently, researchers have found that these two indicators are closely associated with type 2 diabetes and its microvascular complications.22,23 Our study provides a new perspective that the NLR and PLR are closely associated with renal function and that both have predictive value for the development of DKD.
White blood cells and their subtypes (eg, neutrophils and lymphocytes) are recognized indicators of inflammation. The NLR integrates two different types of leukocytes and is more stable than a single indicator. Ciray et al24 reported that the NLR was positively correlated with microalbuminuria but negatively correlated with the eGFR in type 2 diabetes patients, suggesting that the NLR was associated with a progressive decline in renal function. The results of a cross-sectional survey including more than 4000 adult patients with diabetes showed that a higher NLR level was associated with an increased prevalence of DKD.25 A study by Huang et al26 showed that increased NLR levels were associated with DKD and that high NLR values were a predictor of early DKD. Similarly, PLR was considered to be a predictor of diabetic microvascular complications.27 In a follow-up study of 167 patients with biopsy-proven DKD, the PLR was found to be an independent risk factor for renal progression and was associated with the prognosis of DKD.28 Our study exhibited similar results: the NLR and PLR increased with increasing albuminuria in patients with type 2 diabetes, and their levels were correlated with renal function indexes. Moreover, novel findings in this study were that the NLR and PLR were independent risk factors for DKD in Chinese patients with type 2 diabetes, and the DKD odds ratio increased by a factor of 3.137 (95% CI, 1.955–5.033) for every one unit increase in the NLR. In addition, the ROC curve showed that these two inflammatory markers had diagnostic value for DKD. At an NLR ≥2.46 or a PLR ≥125.04, it should be considered that patients with type 2 diabetes may develop DKD. It appears that these metrics could serve as predictors of the risk for DKD, and the predictive value of the NLR was greater than that of the PLR in terms of the area under the curve. The best cutoff values are valuable in getting patients to more tests to clarify the diagnosis. Dynamic monitoring of the NLR and PLR as early warning factors and clinical predictors of DKD facilitates the early identification and timely diagnosis and treatment of patients with type 2 diabetes at renal risk by physicians. They are particularly suitable for use in primary hospitals and outpatient clinics due to the affordability, simplicity and reproducibility.
The mechanism leading to increased NLR and PLR in DKD patients is still being explored. We assume that this finding may be related to the inflammatory state present in DKD. Studies have demonstrated that both systemic inflammation and renal inflammation are closely related to the pathological process of DKD.5 Several inflammatory cytokines (eg, interleukins and tumor necrosis factors) and the NLRP3 inflammasome lead to pathological changes in kidney structure via multiple inflammatory pathways. They aggravate glomerular sclerosis, renal fibrosis and tubular damage and increase urinary albumin excretion.4,29 Neutrophils are traditional indicators of inflammation and are an important component of the innate immune response.30 In the early stage of diabetes, renal cellular stress caused by persistent hyperglycemia initiates an innate immune response and recruits leukocytes to the kidney. This causes renal damage and promotes the development of DKD. As DKD continues to progress, patients are prone to renal ischemia. This exacerbates endothelial cell dysfunction and facilitates the renal infiltration of neutrophils, which accelerates renal damage.31 Neutrophils are involved in the onset and development of DKD, and therefore, a high NLR is closely associated with this disease.
Platelets are the blood cell component involved in thrombosis and hemostasis, and recent studies have demonstrated that platelets are involved in inflammation by releasing proinflammatory factors that recruit and activate leukocytes.32 In patients with systemic lupus erythematosus and rheumatoid arthritis, the PLR is strongly correlated with the severity of systemic inflammation and disease activity.33,34 In addition, recent studies have indicated that platelet microparticles, which are vesicles released by platelets, are associated with the regulation of vascular function. Experiments on animal models of DKD illustrated that platelet microparticles mediate renal endothelial injury by inducing reactive oxygen species.35 Due to the hyperactivity of platelets in patients with diabetes,36 we assume that activated platelets may cause renal damage by promoting inflammatory responses and mediating endothelial injury. Thus, the PLR is closely associated with DKD as a marker reflecting inflammation.
Current treatments for DKD include lifestyle interventions, appropriate control of blood glucose and blood pressure, and reduction of albuminuria. ACE inhibitors and ARBs are renin-angiotensin system blockers that can exert renoprotective effects by reducing albuminuria and lowering blood pressure and are recommended by the KDIGO guidelines for the treatment of type 2 diabetes patients with microalbuminuria or macroalbuminuria. More than half of patients with albuminuria in this study were taking these two classes of drugs. Approximately 60% of patients in this study were taking metformin, consistent with its use as a first-line treatment for type 2 diabetes. Recent studies have shown that in addition to lowering blood glucose and attenuating chronic inflammation caused by hyperglycemia, metformin activates AMPK and inhibits the mTOR pathway, exerting a direct anti-inflammatory effect.37 Sodium-glucose cotransporter 2 (SGLT2) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors are antidiabetic agents that reduce albuminuria and have protective effects on the kidney. In addition, recent studies have found that SGLT2 inhibitors can attenuate kidney inflammation by reducing the levels of inflammatory cytokines.38 GLP-1 receptor agonists and DPP-4 inhibitors have also been shown to have renoprotective effects that may be partially related to the reduction of inflammation.39 However, the anti-inflammatory effects and mechanisms of the above drugs still need further study, and the relationship between antidiabetic drugs and the NLR and PLR needs further follow-up studies. These could become new directions for research.
In addition, our results suggested that the duration of diabetes and LDL-C and HbA1c levels are independent risk factors for DKD, indicating that early diagnosis and treatment and proper control of blood glucose and cholesterol levels can reduce DKD risk.
The limitations of the present study should be considered. First, as a cross-sectional study, our study provides a new perspective that high NLR and high PLR can be used as predictors of DKD in patients with type 2 diabetes, however, the conclusion still needs to be confirmed in prospective studies. Therefore, follow-up studies with large sample sizes are needed to observe the group differences between the high NLR and low NLR groups in the development of type 2 diabetes to DKD, as well as the differences between the high PLR and low PLR groups. This could confirm the current findings and investigate the causal relationship between high NLR, high PLR and DKD. Second, the patients enrolled in this study were not diagnosed pathologically, and there may be a small number of patients with nondiabetic kidney disease, that is, renal dysfunction is not a consequence of the diabetes mellitus. Future studies may need to enroll patients with DKD diagnosed by renal biopsy. Last, our study provides new evidence that DKD is associated with inflammatory markers, but the specific mechanism still needs more research.
In conclusion, the NLR and PLR are cost-effective, readily measured inflammatory markers that are closely associated with renal function in Chinese patients with type 2 diabetes and can be used as predictors of DKD. Clinicians should pay attention to the levels and dynamics of these markers and consider them as warning factors. This could aid in the early assessment of renal risk in patients with type 2 diabetes. These metrics can be used as adjunctive tests in combination with the UACR and eGFR to clarify the clinical diagnosis of DKD. The conclusions of this study still need to be confirmed in prospective studies, and the relationship between these two inflammatory markers and the prognosis of DKD still requires follow-up studies with large sample sizes.
Abbreviations
ACE, angiotensin-converting-enzyme; ARB, angiotensin-receptor blocker; BMI, body mass index; BUN, blood urea nitrogen; CI, confidence interval; DKD, diabetic kidney disease; DPP-4, dipeptidyl peptidase-4; eGFR, estimated glomerular filtration rate; FPG, fasting plasma glucose; GLP-1, glucagon-like peptide 1; HbA1c, hemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; MLR, monocyte-to-lymphocyte ratio; NLR, neutrophil-to-lymphocyte ratio; OR, odds ratio; PLR, platelet-to-lymphocyte ratio; ROC, receiver operating characteristic; Scr, serum creatinine; SGLT2, sodium-glucose cotransporter 2; SUA, serum uric acid; TC, total cholesterol; TG, triglyceride; UACR, urinary albumin-to-creatinine ratio; WBC, white blood cell.
Data Sharing Statement
All data are available from the corresponding author on reasonable request.
Ethical Approval
The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (Approval Number: 2022-K391). Informed consent was obtained from each subject.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report for this study.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12(12):2032–2045. doi:10.2215/CJN.11491116
2. Pálsson R, Patel UD. Cardiovascular complications of diabetic kidney disease. Adv Chronic Kidney Dis. 2014;21(3):273–280. doi:10.1053/j.ackd.2014.03.003
3. Wada J, Makino H. Inflammation and the pathogenesis of diabetic nephropathy. Clin Sci. 2013;124(3):139–152. doi:10.1042/CS20120198
4. Yaribeygi H, Atkin SL, Sahebkar A. Interleukin-18 and diabetic nephropathy: a review. J Cell Physiol. 2019;234(5):5674–5682. doi:10.1002/jcp.27427
5. Matoba K, Takeda Y, Nagai Y, Kawanami D, Utsunomiya K, Nishimura R. Unraveling the role of inflammation in the pathogenesis of diabetic kidney disease. Int J Mol Sci. 2019;20(14):3393. doi:10.3390/ijms20143393
6. Jung SW, Moon JY. The role of inflammation in diabetic kidney disease. Korean J Intern Med. 2021;36(4):753–766. doi:10.3904/kjim.2021.174
7. Bilgin S, Aktas G, Zahid Kocak M, et al. Association between novel inflammatory markers derived from hemogram indices and metabolic parameters in type 2 diabetic men. Aging Male. 2020;23(5):923–927. doi:10.1080/13685538.2019.1632283
8. Boralkar KA, Kobayashi Y, Amsallem M, et al. Value of neutrophil to lymphocyte ratio and its trajectory in patients hospitalized with acute heart failure and preserved ejection fraction. Am J Cardiol. 2020;125(2):229–235. doi:10.1016/j.amjcard.2019.10.020
9. Chen W, Chen K, Xu Z, et al. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio predict mortality in patients with diabetic foot ulcers undergoing amputations. Diabetes Metab Syndr Obes. 2021;14:821–829. doi:10.2147/DMSO.S284583
10. Jeong Y, Jeon SR, Kim HG, et al. The role of platelet to lymphocyte ratio and neutrophil to lymphocyte ratio in ulcerative colitis. Intest Res. 2021;19(1):62–70. doi:10.5217/ir.2019.09156
11. Khalid A, Ali Jaffar M, Khan T, et al. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematology. 2021;26(1):529–542. doi:10.1080/16078454.2021.1950898
12. Onalan E, Dönder E. Neutrophil and platelet to lymphocyte ratio in patients with hypothyroid Hashimoto’s thyroiditis. Acta Biomed. 2020;91(2):310–314. doi:10.23750/abm.v91i2.8592
13. Aktas G. Hematological predictors of novel Coronavirus infection. Rev Assoc Med Bras. 2021;67(Suppl 1):1–2. doi:10.1590/1806-9282.67.suppl1.20200678
14. Atak B, Aktas G, Duman TT, Erkus E, Kocak MZ, Savli H. Diabetes control could through platelet-to-lymphocyte ratio in hemograms. Rev Assoc Med Bras. 2019;65(1):38–42. doi:10.1590/1806-9282.65.1.38
15. Hirahara T, Arigami T, Yanagita S, et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer. BMC Cancer. 2019;19(1):672. doi:10.1186/s12885-019-5903-y
16. Kosekli MA. Mean platelet volume and platelet to lymphocyte count ratio are associated with hepatitis B-related liver fibrosis. Eur J Gastroenterol Hepatol. 2022;34(3):324–327. doi:10.1097/MEG.0000000000002219
17. Caramori ML, Chan JC, Heerspink HJ. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4s):S1–S115. doi:10.1016/j.kint.2020.06.019
18. Sudchada P, Laehn S. Comparisons of GFR estimation using the CKD Epidemiology Collaboration (CKD-EPI) equation and other creatinine-based equations in Asian population: a systematic review. Int Urol Nephrol. 2016;48(9):1511–1517. doi:10.1007/s11255-016-1357-1
19. Bilgin S, Kurtkulagi O, Atak Tel BM, et al. Does C-reactive protein to serum Albumin Ratio correlate with diabEtic nephropathy in patients with Type 2 dIabetes MEllitus? The CARE TIME study. Prim Care Diabetes. 2021;15(6):1071–1074. doi:10.1016/j.pcd.2021.08.015
20. Wang K, Xu W, Zha B, Shi J, Wu G, Ding H. Fibrinogen to albumin ratio as an independent risk factor for type 2 diabetic kidney disease. Diabetes Metab Syndr Obes. 2021;14:4557–4567. doi:10.2147/DMSO.S337986
21. Kocak MZ, Aktas G, Duman TT, et al. Monocyte lymphocyte ratio as a predictor of diabetic kidney injury in type 2 diabetes mellitus; The MADKID Study. J Diabetes Metab Disord. 2020;19(2):997–1002. doi:10.1007/s40200-020-00595-0
22. Wang JR, Chen Z, Yang K, et al. Association between neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and diabetic retinopathy among diabetic patients without a related family history. Diabetol Metab Syndr. 2020;12:55. doi:10.1186/s13098-020-00562-y
23. Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy. 2021;122(7):474–488. doi:10.4149/BLL_2021_078
24. Ciray H, Aksoy AH, Ulu N, Cizmecioglu A, Gaipov A, Solak Y. Nephropathy, but not angiographically proven retinopathy, is associated with neutrophil to lymphocyte ratio in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes. 2015;123(5):267–271. doi:10.1055/s-0035-1547257
25. Wan H, Wang Y, Fang S, et al. Associations between the neutrophil-to-lymphocyte ratio and diabetic complications in adults with diabetes: a cross-sectional study. J Diabetes Res. 2020;2020:6219545. doi:10.1155/2020/6219545
26. Huang W, Huang J, Liu Q, et al. Neutrophil-lymphocyte ratio is a reliable predictive marker for early-stage diabetic nephropathy. Clin Endocrinol. 2015;82(2):229–233. doi:10.1111/cen.12576
27. Onalan E, Gozel N, Donder E. Can hematological parameters in type 2 diabetes predict microvascular complication development? Pak J Med Sci. 2019;35(6):1511–1515. doi:10.12669/pjms.35.6.1150
28. Duan S, Sun L, Zhang C, et al. Association of platelet-to-lymphocyte ratio with kidney clinicopathologic features and renal outcomes in patients with diabetic kidney disease. Int Immunopharmacol. 2021;93:107413. doi:10.1016/j.intimp.2021.107413
29. Milas O, Gadalean F, Vlad A, et al. Pro-inflammatory cytokines are associated with podocyte damage and proximal tubular dysfunction in the early stage of diabetic kidney disease in type 2 diabetes mellitus patients. J Diabetes Complications. 2020;34(2):107479. doi:10.1016/j.jdiacomp.2019.107479
30. Liew PX, Kubes P. The neutrophil’s role during health and disease. Physiol Rev. 2019;99(2):1223–1248. doi:10.1152/physrev.00012.2018
31. Tesch GH. Diabetic nephropathy - is this an immune disorder? Clin Sci. 2017;131(16):2183–2199. doi:10.1042/CS20160636
32. Repsold L, Joubert AM. Platelet function, role in thrombosis, inflammation, and consequences in chronic myeloproliferative disorders. Cells. 2021;10(11):3034. doi:10.3390/cells10113034
33. Qin B, Ma N, Tang Q, et al. Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were useful markers in assessment of inflammatory response and disease activity in SLE patients. Mod Rheumatol. 2016;26(3):372–376. doi:10.3109/14397595.2015.1091136
34. Targońska-Stępniak B, Zwolak R, Piotrowski M, Grzechnik K, Majdan M. The relationship between hematological markers of systemic inflammation (neutrophil-to-lymphocyte, platelet-to-lymphocyte, lymphocyte-to-monocyte ratios) and ultrasound disease activity parameters in patients with rheumatoid arthritis. J Clin Med. 2020;9(9):2760. doi:10.3390/jcm9092760
35. Zhang Y, Ma KL, Gong YX, et al. Platelet microparticles mediate glomerular endothelial injury in early diabetic nephropathy. J Am Soc Nephrol. 2018;29(11):2671–2695. doi:10.1681/ASN.2018040368
36. Kaur R, Kaur M, Singh J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol. 2018;17(1):121. doi:10.1186/s12933-018-0763-3
37. Bharath LP, Nikolajczyk BS. The intersection of metformin and inflammation. Am J Physiol Cell Physiol. 2021;320(5):C873–C879. doi:10.1152/ajpcell.00604.2020
38. Heerspink HJL, Perco P, Mulder S, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia. 2019;62(7):1154–1166. doi:10.1007/s00125-019-4859-4
39. Kawanami D, Matoba K, Sango K, Utsunomiya K. Incretin-based therapies for diabetic complications: basic mechanisms and clinical evidence. Int J Mol Sci. 2016;17(8):1223. doi:10.3390/ijms17081223
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

