Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 15
Association of CYP7A1 and CYP2E1 Polymorphisms with Type 2 Diabetes in the Chinese Han Populations
Authors Zhang L, Tang J, Wang Y, Wang X, Wang F
Received 24 March 2022
Accepted for publication 30 August 2022
Published 21 September 2022 Volume 2022:15 Pages 843—855
DOI https://doi.org/10.2147/PGPM.S367806
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Lihong Zhang, Jingjing Tang, Yindi Wang, Xiang Wang, Fang Wang
Department of Endocrinology, Xi’an Central Hospital Affiliated to Xi’an Jiaotong University, Xi’an, 710003, People’s Republic of China
Correspondence: Fang Wang, Department of Endocrinology, Xi’an central hospital affiliated to Xi’an Jiaotong University, No. 185, Houzaimen, Xincheng District, Xi’an, Shaanxi Province, People’s Republic of China, Tel/Fax +86 18681809668, Email [email protected]
Background: Type 2 diabetes mellitus (T2DM) is caused by diverse environmental and genetic risk factors. Previous studies have reported that cytochrome P450 (CYP) is a promising gene for T2DM. Therefore, we aimed to determine the effects of CYP7A1 and CYP2E1 polymorphisms on T2DM susceptibility among the Chinese Han population.
Methods: A case-control study was conducted to assess the potential relationship of four polymorphisms (rs8192879, rs12542233, rs2070672 and rs2515641) with T2DM susceptibility in the Chinese population, involving 512 T2DM patients and 515 age- and gender-matched healthy individuals. We used the Agena MassARRAY platform to detect CYP7A1 and CYP2E1 polymorphisms. The relationship between genetic polymorphisms and T2DM risk was evaluated using odds ratios (ORs) and 95% confidence intervals (CIs) in various genetic models.
Results: After adjusting for age and gender, rs12542233 in the CYP7A1 gene was significantly associated with decreased T2DM risk (recessive: OR = 0.67, 95% CI = 0.49– 0.91, p = 0.012; after FDR correction, p = 0.048). The CYP7A1 rs12542233 was associated with a reduced risk of T2DM in people over 59 years of age (p = 0.010). In the population with BMI ≤ 24 kg/m2, CYP7A1 rs12542233 was associated with an increased risk of T2DM (p < 0.05). In the population with BMI > 24 kg/m2, CYP2E1 rs2515641 can significantly reduce the risk of T2DM (p < 0.05). And rs8192879, rs2070672 and rs2515641 could significantly increase the risk of diabetes retinopathy in T2DM patients (p < 0.05). Furthermore, the Trs8192879Crs12542233 haplotype was significantly associated with T2DM (p = 0.019).
Conclusion: CYP7A1 and CYP2E1 polymorphisms may contribute to T2DM susceptibility in the Chinese Han population, especially in stratified analysis.
Keywords: diabetes mellitus, type 2, gene polymorphisms, case-control study, CYP7A1, CYP2E1
Background
Diabetes mellitus (DM) is a complex metabolic disease characterized by hyperglycemia, which is caused by deficiencies in insulin secretion and function. According to the International Diabetes Federation (IDF), there were about 463 million people with diabetes worldwide in 2019 (diabetes prevalence was 9.3%). It is estimated that the number of diabetes patients in the world will reach 578 million (diabetes prevalence is 10.2%) by 2030, and will increase to 700 million (diabetes prevalence is 10.9%) by 2045.1 Type 2 diabetes mellitus (T2DM) accounts for approximately 90% of patients with diabetes.2 Diabetes complications are the main cause of death in diabetes patients, including diabetes retinopathy, renal failure, diabetes foot and cardiovascular disease. One-third of diabetes patients will have diabetes retinopathy, which is related to the risk of systemic vascular complications.3 It is well known that genetic factors, lifestyle and environmental factors have an important impact on susceptibility to diabetes. Numerous studies have demonstrated that the significance of genetic polymorphisms in cytochromes P450 (CYP) in the pathogenesis of T2DM, such as CYP2C9, CYP2C19, CYP2D6, CYP3A4, and CYP2J2.4–6 Cholesterol 7 α-hydroxylase (cytochrome P450 7A1, CYP7A1), a member of the CYP family, plays an essential role in regulating the homeostasis of cholesterol and bile acids. It has been reported that bile acids are signaling molecules, which can activate bile acid receptors to regulate bile acid synthesis and glucose metabolism.7 Some studies have demonstrated that the bile acid pool and excretion increase in diabetic human patients and diabetic animals.8 Gerhard et al have found that diabetic patients have significantly higher serum bile acid levels than healthy controls.9 In addition, Prawitt et al showed that the administration of a bile acid sequestrant decreased plasma glucose and HbA1c concentrations.10 Moreover, previous studies indicated that insulin inhibits the expression of CYP7A1 in rat hepatocytes, the key enzyme in bile acid synthesis pathways.11 These findings suggested that CYP7A1 may be involved in the development of T2DM through bile acid synthesis pathways. CYP7A1 polymorphisms have been associated with the susceptibility of coronary heart disease, gall bladder stone disease and cancers.12–15 However, the relationship between CYP7A1 and T2DM is unclear.
Cytochrome P450 2E1 (CYP2E1) is another member of the CYP superfamily and is responsible for the metabolic activation of many low-molecular weight compounds, including ethanol, benzene, vinyl chloride, and N- nitrosamines.16 The overexpressed CYP2E1 exhibits a high capacity of produce free radicals that probably cause liver damage and lipid peroxidation in obese T2DM patients.17 It has been shown that there is elevated activity of CYP2E1 in the liver of obese patients with T2DM.18 Previous studies also have shown that T2DM could induce increased levels of CYP2E1 protein and increase the activities of liver-related enzymes. Moreover, T2DM enhances the toxicity and/or carcinogenic effects of chemicals in the liver by inducing CYP2E1-dependent drug-metabolizing enzymes.19 This evidence suggests that CYP2E1 plays a crucial role in T2DM development. In addition, a large body of literature has demonstrated that CYP2E1 polymorphisms are correlated with the risk of cancer and other diseases.20,21 However, no studies have focused on the association of CYP2E1 polymorphisms with susceptibility to T2DM.
To explore the relationship of CYP7A1 and CYP2E1 polymorphisms with T2DM risk in the Chinese Han populations, we designed this case-control study and focused on the correlations between four polymorphisms (CYP7A1: rs8192879 and rs12542233; CYP2E1: rs2070672 and rs2515641) and T2DM susceptibility.
Methods
Study Populations
A total of 512 diabetic patients and 515 healthy controls were enrolled from the First affiliated hospital of Xi’an Jiaotong University in China. All patients were diagnosed based on the 2022 American Diabetes Association (ADA) diagnostic criteria for diabetes. Criteria for the diagnosis of diabetes: 1) fasting blood glucose (FBG) ≥7.0 mmol/L, 2) 2-h plasma glucose (2-h PG) ≥200 mg/dL (11.1 mmol/L) during oral glucose tolerance test (OGTT), 3) A1C ≥6.5% (48 mmol/mol), 4) In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L).22 A person who accord with one of these criteria is diagnosed diabetes. Patients suffering from type 1 diabetes, gestational diabetes, inflammation, malignancy, renal dysfunction, other chronic or endocrine disease, and who have receiving any drugs like antidiabetics were excluded. The controls were age- and gender-matched healthy population and had no history of diabetes, metabolic disorders or severe diseases. The demographic and clinical characteristics of the study population, such as age, gender, body mass index (BMI), smoking status, drinking status, Complication, Antidiabetes drug, Insulin, diabetic retinopathy, Fasting blood glucose (FBG), hemoglobin A1C (HbA1C), total cholesterol (TC), Triglycerides (TG), Low-density lipoprotein (LDL), High-density lipoprotein (HDL), Urea, Creatinine, Cystatin C, glomerular filtration rate (GFR) were required from their medical records (Table 1). The study was approved by the ethical committee of the First affiliated hospital of Xi’an Jiaotong University, and informed consent forms were signed by all individuals before the study according to the Helsinki Declaration.
 |
Table 1 Demographic and Clinical Characteristics of Participants |
Genotyping
Genomic DNA was isolated using GoldMag–Mini Purification Kit (GoldMag Co. Ltd. Xi’an, China) and stored at −80°C until analysis. The genetic variations of CYP7A1 and CYP2E1 were obtained through Ensembl (http://grch37.ensembl.org/Homo_sapiens/Tools/VcftoPed) database.23 Using Haploview software, we selected tagSNPs based on Hardy-Weinberg equilibrium (HWE) > 0.01, minor allele frequency (MAF) > 0.05, Minimum genotype (Min Genotype) > 75%, and Tagger r2 >0.8. Combined MassARRAY, HWE > 0.05, MAF > 0.05 and the call rate > 95% in our study population, four candidate SNPs (rs8192879, rs12542233, rs2070672 and rs2515641) were randomly selected in order to study their potential role in T2DM risk (Table 2). We applied the Agena MassARRAY Assay Design 3.0 software (Agena Bioscience, San Diego, California, USA) to design PCR and extension primers of each SNP (Table 3). All SNPs were genotyped by the MassARRAY iPLEX platform. Then, we performed data management and analysis using the Agena Typer 4.0 Software. HaploReg v4.1 (https://pubs.broadinstitute.org/mammals/haploreg /haploreg.php)24 was conducted to predict the potential functions of the candidate variants.
 |
Table 2 Primary Information of CYP7A1 and CYP2E1 Polymorphisms |
 |
Table 3 Primer Sequence of CYP7A1 and CYP2E1 SNPs for PCR and UEP Used in This Study |
Data Analysis
Data analysis was performed using SPSS version 20.0 software (SPSS, Chicago, IL, USA). The differences in demographic variables and genotype distribution were assessed by the chi-square test and student’s t test between diabetes patients and healthy controls. We used Fisher’s exact test to evaluate the HWE of each SNP in controls. The association of diabetes risk and genetic polymorphisms was assessed using odds ratios (ORs) and 95% confidential intervals (95% CI) using logistic regression adjusted by sex and age. In addition, linkage disequilibrium (LD) and haplotype analysis were analyzed by Haploview software (version 4.0) and PLINK software.25,26 Multifactor dimensionality reduction (MDR) analysis was used to identify the best SNP–SNP interaction model. The p values <0.05 were considered significant in our study.
Results
Characteristics of Participants
The demographic and clinical characteristics of study participants are shown in Table 1. The mean age was 59.23 ± 9.59 years and 59.27 ± 10.97 years in cases and controls, respectively. No significant differences were observed in the distributions of age, gender BMI and other characteristics of subjects. However, there were significant differences in FBG, HbA1c, TC, TG, urea, GFR and other clinical indicators between the T2DM patients and the healthy control.
Association of CYP7A1 and CYP2E1 Polymorphisms with Diabetes Risk
In Table 2, the primary information of CYP7A1 and CYP2E1 polymorphisms are presented. The results of stratified analysis by age, gender, BMI, etc. are listed in Supplemental Table 1. All genetic polymorphisms were in accordance with HWE (P> 0.05). HaploReg showed that candidate polymorphisms were associated with the regulation of promoter and/or enhancer histone, DNase, motifs changed, GRASP QTLhits and selected eQTL hits.
The genotypes frequencies of diabetes patients are shown in Table 4. CYP7A1 rs12542233 was significantly related to T2DM risk in recessive model (p = 0.012, OR = 0.67, 95% CI = 0.49–0.91; after FDR correction, p = 0.048). In addition, in order to further explore the relationship between these four variants genotypes and T2DM susceptibility, we performed subgroup analysis stratification on age, sex, BMI, etc. (Supplemental Table 2).
 |
Table 4 The Association of CYP7A1 and CYP2E1 Genotypes with Susceptibility of Diabetes |
Stratification Analysis by Age and BMI
The relationship between genotypes of four variants and T2DM susceptibility stratified by age and BMI are shown in Table 5. The CYP7A1 rs12542233 Recessive model was associated with a reduced risk of T2DM in people over 59 years of age (p = 0.010, OR = 0.55, 95% CI = 0.35–0.87). In the population with BMI ≤ 24 kg/m2, CYP7A1 rs12542233 Heterozygou (p = 0.023, OR = 2.08, 95% CI = 1.11–3.90) and Dominant (p = 0.026, OR = 1.94, 95% CI = 1.08–3.49) models were associated with an increased risk of T2DM. In the population with BMI > 24 kg/m2, CYP2E1 rs2515641 Homozygous (p = 0.038, OR = 0.10, 95% CI = 0.01–0.89) and Recursive (p = 0.038, OR = 0.10, 95% CI = 0.01–0.88) models can significantly reduce the risk of T2DM.
 |
Table 5 Stratification Analyses of the Association of CYP7A1 and CYP2E1 Polymorphisms with Susceptibility of Diabetes |
The Association of CYP7A1 and CYP2E1 Polymorphisms with Susceptibility of Diabetic Retinopathy
We stratified the T2DM patients according to diabetes retinopathy (Table 6). The results showed that rs8192879 Heterozygou (p = 0.032, OR = 1.65, 95% CI = 1.05–2.60) and Dominant (p = 0.033, OR = 1.61, 95% CI = 1.04–2.48) models, rs2070672 Heterozygou (p = 0.028, OR = 1.75, 95% CI = 1.06–2.87), Dominant (p = 0.027, OR = 1.71, 95% CI = 1.06–2.75) and Additive (p = 0.046, OR = 1.53, 95% CI = 1.01–2.32) models, rs2515641 Dominant (p = 0.045, OR = 1.64, 95% CI = 1.01–2.67) and Additive (p = 0.042, OR = 1.61, 95% CI = 1.02–2.55) models could significantly increase the risk of diabetes retinopathy in T2DM patients.
 |
Table 6 The Association of CYP7A1 and CYP2E1 Polymorphisms with Susceptibility of Diabetic Retinopathy |
Haplotype Analysis
Then, we conducted LD and haplotype analyses on the polymorphisms of CYP7A1 and CYP2E1. These analyses revealed one block in CYP7A1, including rs8192879 and rs12542233 (Figure 1). Haplotype frequencies and their association with T2DM risk are listed in Table 7. We found that Crs8192879Trs12542233 was markedly related to lower risk of diabetes (p = 0.019, OR = 0.75, 95% CI = 0.59–0.95). The results of hierarchical analysis are listed in Supplemental Table 3.
 |
Table 7 Haplotype Frequencies and the Association with the Risk of Diabetes |
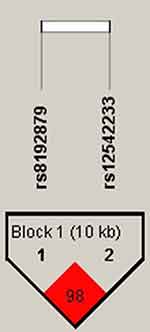 |
Figure 1 Haplotype block map for the SNPs of CYP7A1. Block includes rs8192879 and rs12542233. The LD between two SNPs is standardized by D′. |
MDR Analysis
MDR was used to analyze the interactions of these four SNPs. The results of the MDR model analysis of the SNP-SNP interactions are demonstrated in Table 8. The results showed that rs12542233 was the best single-locus model to predict trait anxiety (cross-validation consistency, 9/10; testing accuracy, 0.5010; p = 0.011). The best multi-loci model was the three-locus model, a combination of rs12542233, rs2070672 and rs2515641, with cross-validation consistency (7/10), the testing accuracy (0.4902) and p = 0.001.
 |
Table 8 SNP–SNP Interaction Models of the CYP7A1 and CYP2E1 Genes for T2DM Predisposition |
Association of CYP7A1 and CYP2E1 Polymorphisms with Clinical Characteristics Among T2DM Patients
Among the T2DM patients, the different genotypes of CYP7A1 rs819287 were significantly correlated with the levels of total cholesterol (TC, p = 0.036) and low-density lipoprotein (LDL, p = 0.031). And, TC level also was related to CYP2E1 rs2070672 genotypes (p= 0.040, Table 9).
 |
Table 9 Clinical Characteristics of Diabetes Patients Based on CYP7A1 and CYP2E1 Polymorphisms |
Discussion
In this study, we assessed the influence of four SNPs in CYP7A1 and CYP2E1 on susceptibility to T2DM. Our results showed that CYP7A1 rs12542233 was significantly associated with T2DM risk in the Chinese Han populations. Stratified analysis revealed that rs12542233 was associated with the reduced risk of T2DM patients without diabetic retinopathy. CYP7A1 rs12542233 had strong relationship with diabetes risk in the subgroups of age >59 years and BMI ≤ 24 kg/m2. Additionally, haplotype analysis showed Crs8192879Trs12542233 was associated with lower risk of T2DM.
In recent years, studies generally believed that genetic variation is one of the genetic factors of cancer and other diseases. And SNPs are important genetic variation. Several studies have found that genetic polymorphisms are associated with the risk of diabetes in Iranian population. Genome-wide association studies indicated that HHET rs1111875G/A and rs5015480C/T variants significantly increased the risk of T2DM.27 Hamidreza Galavi et al found the SREBF-2 gene rs2267439C/T polymorphism increased T2DM susceptibility.28 IGF2BP2 rs11705701 and rs1470579 gene polymorphisms may be associated with T2DM.29 Case-control study showed that functional miR-143/145 variants may affect the risk of T2DM.30 In addition, the SIRT1 functional variants rs12778366 significantly increased the risk of T2DM, and the rs3758391 was associated with a reduced risk of T2DM.31 SLC30A8 gene rs2466293 and rs2466294 variants are associated with increased risk of T2DM, and different genetic models of rs13266634 are associated with decreased risk of T2DM.32 In T2DM patients, the mean levels of HbA1c were significantly different between CC and TT genotype carriers of the rs28514894 polymorphism.33 HOTAIR rs920778 C/T, rs12826786 C/T, rs4759314 A/G polymorphisms were positively correlated with T2DM, while rs1899663 G/T was negatively correlated with T2DM susceptibility.34 In our study, the levels of TC and LDL were significantly different in rs8192879TT, TC and CC genotypes in T2DM patients. Genome-wide association studies revealed that CYP7A1 rs2081687 is an SNP associated with lipids in African Americans.35 However, there are no studies on the role of rs8192879 and rs12542233 in T2DM development. In our study, we found CYP7A1 rs125422333 significantly decreased T2DM risk in recessive model. More studies are required to confirm this result in a larger and well-designed study. The prevalence of diabetes was varied in factors, such as age, sex, and BMI. Sex and age are major risk variables in epidemiology of multiple diseases. The incidence, prevalence or mortality of non-insulin-dependent T2DM increases steeply with age.36,37 Diabetes is particularly prevalent in adults who are thin at birth but have a high BMI later in life.38,39 LeRoith et al showed that T2DM is becoming more and more common in people, especially in individuals over 65 years old.40 Our results showed that rs12542233 and rs2515641 could protect individuals from T2DM among the elderly Chinese population (age >59 years). Rs12542233 and rs2515641 also had strong relationships with diabetes risk in the individuals with different BMI. Meanwhile, the exact mechanism of the genetic variants in development of T2DM needs to be further studied.
Inevitably, this study has several limitations. First, the sample size is limited, so future large-scale studies are needed to verify our findings. Secondly, data on the potential function of these SNPs were predicted in silico only; thus, further functional assay is necessary to explore the underlying functions and mechanisms of these polymorphisms. Third, our study did not conduct cell or animal experiments, so we can supplement this part of the study in the future to make the relationship between CYP7A1 and CYP2E1 and diabetes more definite.
Conclusion
In summary, our study firstly evaluated the association of CYP7A1 and CYP2E1 polymorphisms with T2DM risk in a Chinese population. We have found that CYP7A1 and CYP2E1 gene polymorphisms were significantly associated with the risk of T2DM, especially in stratified analysis. It provides evidence that CYP7A1 and CYP2E1 may be associated with diabetes susceptibility, and suggests a vital role for CYP7A1 and CYP2E1 in the progression of diabetes.
Abbreviations
T2DM, type 2 diabetes mellitus; CYP, cytochrome P450; ORs, odds ratios; CIs, confidence intervals; DM, diabetes mellitus; CYP7A1, cytochrome P450 7A1; CYP2E1, cytochrome P450 2E1; BMI, body mass index; CHB, the Han Chinese in Beijing; CHS, Southern Han Chinese; HWE, Hardy-Weinberg equilibrium; MAF, minor allele frequency; LD, linkage disequilibrium; MDR, multifactor dimensionality reduction; LDL, low-density lipoprotein.
Data Sharing Statement
All the data regarding the findings are available within the manuscript. Anyone who is interested in the information should contact the corresponding author.
Ethics Approval and Informed Consent
The study was approved by the ethical committee of the First affiliated hospital of Xi’an Jiaotong University, and informed consent forms were signed by all individuals before the study according to the Helsinki Declaration.
Consent for Publication
All authors agree to publish.
Acknowledgment
We sincerely thank all participators in this study. Specially, we thank First affiliated hospital of Xi’an Jiaotong University for providing samples.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Shaanxi key research and development plan (2017SF-080).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
2. Tang K, Li X, Xing Q, et al. Genetic polymorphism analysis of cytochrome P4502E1 (CYP2E1) in Chinese Han populations from four different geographic areas of Mainland China. Genomics. 2010;95(4):0–229.
3. Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124–136. doi:10.1016/S0140-6736(09)62124-3
4. Semiz S, Dujic T, Ostanek B, et al. Analysis of CYP2C9*2, CYP2C19*2, and CYP2D6*4 polymorphisms in patients with type 2 diabetes mellitus. Bosn J Basic Med Sci. 2010;10(4):287–291. doi:10.17305/bjbms.2010.2662
5. Yamada Y, Matsuo H, Watanabe S, et al. Association of a polymorphism of CYP3A4 with type 2 diabetes mellitus. Int J Mol Med. 2007;20(5):703–707.
6. Wang CP, Hung W-C, Yu T-H, et al. Genetic variation in the G-50T polymorphism of the cytochrome P450 epoxygenase CYP2J2 gene and the risk of younger onset type 2 diabetes among Chinese population: potential interaction with body mass index and family history. Exp Clin Endocrinol Diabetes. 2010;118(6):346–352. doi:10.1055/s-0029-1243604
7. Chiang JY. Bile acid regulation of hepatic physiology: III. Bile acids and nuclear receptors. Am J Physiol Gastrointest Liver Physiol. 2003;284(3):G349–56. doi:10.1152/ajpgi.00417.2002
8. Li T, Kong X, Owsley E, et al. Insulin regulation of cholesterol 7alpha-hydroxylase expression in human hepatocytes: roles of forkhead box O1 and sterol regulatory element-binding protein 1c. J Biol Chem. 2006;281(39):28745–28754. doi:10.1074/jbc.M605815200
9. Gerhard GS, Styer AM, Wood GC, et al. A role for fibroblast growth factor 19 and bile acids in diabetes remission after Roux-en-Y gastric bypass. Diabetes Care. 2013;36(7):1859–1864. doi:10.2337/dc12-2255
10. Hansen M, Sonne DP, Knop FK. Bile acid sequestrants: glucose-lowering mechanisms and efficacy in type 2 diabetes. Curr Diab Rep. 2014;14(5):482. doi:10.1007/s11892-014-0482-4
11. Lefebvre P, Cariou B, Lien F, et al. Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev. 2009;89(1):147–191. doi:10.1152/physrev.00010.2008
12. Hofman MK, Princen H, Zwinderman A, et al. Genetic variation in the rate-limiting enzyme in cholesterol catabolism (cholesterol 7α-hydroxylase) influences the progression of atherosclerosis and risk of new clinical events. Clin Sci. 2005;108(6):539–545. doi:10.1042/CS20040339
13. Jiang ZY, Han TQ, Suo GJ, et al. Polymorphisms at cholesterol 7α-hydroxylase, apolipoproteins B and E and low density lipoprotein receptor genes in patients with gallbladder stone disease. World J Gastroenterol. 2004;10(10):1508–1512. doi:10.3748/wjg.v10.i10.1508
14. Hagiwara T, Kono S, Yin G. Genetic polymorphism in cytochrome P 450 7A1 and risk of colorectal cancer: the Fukuoka colorectal cancer study. Cancer Res. 2005;65(7):2979–2982. doi:10.1158/0008-5472.CAN-04-3872
15. Ueda N, Maehara Y, Tajima O, et al. Genetic polymorphisms of cyclooxygenase-2 and colorectal adenoma risk: the self defense forces health study. Cancer Sci. 2010;99(3):576–581.
16. Arin E, Arslan Ş, Bozcaarmutlu A, et al. Effects of diabetes on rabbit kidney and lung CYP2E1 and CYP2B4 expression and drug metabolism and potentiation of carcinogenic activity of N-nitrosodimethylamine in kidney and lung. Food Chem Toxicol. 45(1):0–118. doi:10.2341/19-251-L
17. Doroshyenko O, Fuhr U, Kunz D, et al. in vivo role of cytochrome P450 2E1 and glutathione-s-transferase activity for acrylamide toxicokinetics in humans. Cancer Epidemiol Biomarkers Prev. 2009;18(2):433–443. doi:10.1158/1055-9965.EPI-08-0832
18. Wang Z, Hall SD, Maya JF, et al. Diabetes mellitus increases the in vivo activity of cytochrome P450 2E1 in humans. Br J Clin Pharmacol. 2003;55(1):77–85. doi:10.1046/j.1365-2125.2003.01731.x
19. Arinç E, Arslan S, Adali O. Differential effects of diabetes on CYP2E1 and CYP2B4 proteins and associated drug metabolizing enzyme activities in rabbit liver. Arch Toxicol. 2005;79(8):427–433. doi:10.1007/s00204-005-0654-8
20. Barry KH, Zhang Y, Lan Q, et al. Genetic variation in metabolic genes, occupational solvent exposure, and risk of non-Hodgkin lymphoma. Am J Epidemiol. 2011;173(4):404–413. doi:10.1093/aje/kwq360
21. Huo R, Tang K, Wei Z, et al. Genetic polymorphisms in CYP2E1: association with schizophrenia susceptibility and risperidone response in the Chinese Han population. PLoS One. 2012;7(5):e34809. doi:10.1371/journal.pone.0034809
22. American Diabetes Association. 2. classification and diagnosis of diabetes: standards of medical care in Diabetes—2022. Diabetes Care. 2022;45(Suppl Supplement_1):S17–s38. doi:10.2337/dc22-S002
23. Yates A, Akanni W, Amode MR, et al. Ensembl 2016. Nucleic Acids Res. 2016;44(D1):D710–6. doi:10.1093/nar/gkv1157
24. Jin T, Wang L, He X, et al. Association between DIO2 polymorphism and the risk of Kashin–Beck disease in the Tibetan population. J Gene Med. 2019;21(10):e3123. doi:10.1002/jgm.3123
25. Dai ZJ, Liu X-H, Ma Y-F, et al. Association between single nucleotide polymorphisms in DNA polymerase kappa gene and breast cancer risk in Chinese Han population: a STROBE-compliant observational study. Medicine. 2016;95(2):e2466. doi:10.1097/MD.0000000000002466
26. Ren HT, Li Y-M, Wang X-J, et al. PD-1 rs2227982 polymorphism is associated with the decreased risk of breast cancer in northwest Chinese women. Medicine. 2016;95(21):e3760. doi:10.1097/MD.0000000000003760
27. Galavi H, Mollashahee‐Kohkan F, Saravani R, et al. HHEX gene polymorphisms and type 2 diabetes mellitus: a case-control report from Iran. J Cell Biochem. 2019;120(10):16445–16451. doi:10.1002/jcb.28788
28. Galavi H, Noorzehi N, Saravani R, et al. Association study of SREBF-2 gene polymorphisms and the risk of type 2 diabetes in a sample of Iranian population. Gene. 2018;660:145–150. doi:10.1016/j.gene.2018.03.080
29. Sargazi S, Heidari Nia M, Saravani R, et al. IGF2BP2 polymorphisms as genetic biomarkers for either schizophrenia or type 2 diabetes mellitus: a case-control study. Gene Rep. 2020;20:100680. doi:10.1016/j.genrep.2020.100680
30. Jahantigh D, Mirani Sargazi F, Sargazi S, et al. Relationship between functional miR-143/145 cluster variants and susceptibility to type 2 diabetes mellitus: a preliminary case-control study and bioinformatics analyses. Endocr Res. 2021;46(3):129–139. doi:10.1080/07435800.2021.1914079
31. Sadeghi MB, Nakhaee A, Saravani R, et al. SIRT1 functional polymorphisms (rs12778366, rs3758391) as genetic biomarkers of susceptibility to type 2 diabetes mellitus in Iranians: a case-control study and computational analysis. Int J Diabetes Dev Ctries. 2021;41(3):447–455. doi:10.1007/s13410-020-00898-1
32. Sargazi S, Heidari Nia M, Sargazi FM, et al. SNPs in the 3’-untranslated region of SLC30A8 confer risk of type 2 diabetes mellitus in a south-east Iranian population: evidences from case-control and bioinformatics studies. J Diabetes Metab Disord. 2020;19(2):979–988. doi:10.1007/s40200-020-00590-5
33. Sadeghi MB, Nakhaee A, Saravani R, et al. Significant association of LXRβ (NR1H2) polymorphisms (rs28514894, rs2303044) with type 2 diabetes mellitus and laboratory characteristics. J Diabetes Metab Disord. 2021;20(1):261–270. doi:10.1007/s40200-021-00740-3
34. Sargazi S, Ravanbakhsh M, Nia MH, et al. Association of polymorphisms within HOX transcript antisense RNA (HOTAIR) with type 2 diabetes mellitus and laboratory characteristics: a preliminary case-control study. Dis Markers. 2022;2022:4327342. doi:10.1155/2022/4327342
35. Adeyemo A, Bentley AR, Meilleur KG, et al. Transferability and fine mapping of genome-wide associated loci for lipids in African Americans. BMC Med Genet. 2012;13(1):88. doi:10.1186/1471-2350-13-88
36. King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. Diabetes Care. 1993;16(1):157–177. doi:10.2337/diacare.16.1.157
37. Nagai M, Sakata K, Yanagawa H, et al. [Prevalence estimates for non-insulin dependent diabetes mellitus (NIDDM) in Japan from National Survey of Circulatory Disorders 1990 data]. Nihon Koshu Eisei Zasshi. 1994;41(8):720. Japanese.
38. Eriksson JG, Forsén T, Tuomilehto J, et al. Early adiposity rebound in childhood and risk of type 2 diabetes in adult life. Diabetologia. 2003;46(2):190–194. doi:10.1007/s00125-002-1012-5
39. Sachdev HS, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort. Am J Clin Nutr. 2005;82(2):456–466.
40. LeRoith D, Biessels GJ, Braithwaite SS, et al. Treatment of diabetes in older adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2019;104(5):1520–1574. doi:10.1210/jc.2019-00198
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
