Back to Journals » Risk Management and Healthcare Policy » Volume 15
Association Between the Severity of Early Acute Kidney Injury and Subsequent in-Hospital Complications and 90-Day Mortality in Geriatric Patients Receiving Invasive Mechanical Ventilation
Authors Li Q, Cai X, Li G , Ju H , Li D, Zhou F
Received 8 February 2022
Accepted for publication 5 April 2022
Published 26 April 2022 Volume 2022:15 Pages 793—804
DOI https://doi.org/10.2147/RMHP.S361598
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Qinglin Li,1,* Xiaoyan Cai,2,* Guanggang Li,3 Hongyan Ju,3 Dawei Li,4 Feihu Zhou1,5
1Department of Critical Care Medicine, the First Medical Center, Chinese PLA General Hospital, Beijing, 100853, People’s Republic of China; 2Department of Nephrology, the Second Medical Center, Chinese PLA General Hospital, Beijing, 100853, People’s Republic of China; 3Department of Critical Care Medicine, the Seventh Medical Center, Chinese PLA General Hospital, Beijing, 100700, People’s Republic of China; 4Department of Critical Care Medicine, the Sixth Medical Center, Chinese PLA General Hospital, Beijing, 100048, People’s Republic of China; 5Chinese PLA General Hospital National Clinical Research Center for Geriatric Diseases, Beijing, 100853, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Feihu Zhou, Department of Critical Care Medicine, the First Medical Center, Chinese PLA General Hospital, Beijing, 100853, People’s Republic of China, Tel +86– 10– 66938148, Fax +86– 10– 88219862, Email [email protected]
Purpose: Acute kidney injury (AKI) in elderly patients is associated with higher hospital mortality. However, the relationship between AKI and peri-intubation complications is unclear.
Methods: This retrospective, observational, multicenter cohort study enrolled 3271 consecutive elderly patients (≥ 75 years) who received invasive mechanical ventilation (MV) in four medical centers of Chinese PLA General Hospital from 2008 to 2020. AKI was diagnosed according to the 2012 KDIGO criteria by an absolute increase in serum creatinine of ≥ 26.5 μmol/L within the first 48 hours of MV. We recorded subsequent in-hospital complications, including incident gastrointestinal bleeding, new-onset electrolyte imbalances, severe hypoxemia, hypoalbuminemia, cardiovascular instability and all-cause 90-day mortality.
Results: A total of 1292 patients were included in the final evaluation, with 29.1% presenting AKI (stage 1: 31.4%, stage 2: 35.1%, stage 3: 33.5%). Multiple regression analyses show that more advanced AKI increased the risk of MAP < 65 mmHg (stage 1: OR=1.833, P=0.002; stage 2: OR= 4.653, P< 0.001; stage 3: OR=4.834, P< 0.001) and SBP < 90 mmHg (stage 1: OR=1.644, P=0.014; stage 2: OR=3.701, P< 0.001; stage 3: OR=5.750, P< 0.001), a new need for or requiring an increased dose of vasopressors (stage 1: OR=1.623, P=0.014; stage 2: OR=3.250, P< 0.001; stage 3: OR=12.132, P< 0.001), gastrointestinal bleeding (stage 1: OR=1.102, P=0.669; stage 2: OR=1.471, P=0.060; stage 3: OR=2.377, P< 0.001), severe hypoxia (stage 1: OR=1.213, P=0.399; stage 2: OR=1.449, P=0.077; stage 3: OR=2.214, P< 0.001) and all-cause 90-day mortality (stage 1: OR =0.935; P=0.741; stage 2: OR=1.888; P=0.001; stage 3: OR=12.584; P< 0.001).
Conclusion: Our study suggests that the presence of AKI within the first 48 hours of MV in geriatric patients is associated with a higher risk for postintubation complications and 90-day mortality. Moreover, the risk of complications was greater for patients with more severe AKI.
Keywords: mechanical ventilation, aged, complications, acute kidney injury, electrolyte imbalance
Introduction
Invasive mechanical ventilation (MV) is one of the most commonly performed and high-risk interventions in the care of critically ill patients.1,2 Unfortunately, this lifesaving tool also carries a high risk of complications.3,4 Russotto V reported that up to 45.2% of critically ill patients experience a life-threatening complication after tracheal intubation, including cardiovascular instability in 42.6% of patients and severe hypoxemia in 9.3% of patients.5 However, the above study analyzed only major adverse peri-intubation events within 30 minutes from the start of the intubation procedure, and additional organ complications, such as the development of acute kidney injury (AKI), may have been missed due to such a short study time window.6,7
AKI is a complex and severe kidney disease characterized by a sudden decline in renal function with a consequent increase in nitrogenous products and hydroelectrolytic and acid-base disorders.8 Aging kidneys undergoing structural and functional changes that adversely affect the autoregulatory capacity, systemic vasculature, and immunological system increase susceptibility to AKI in the elderly population.9 Van den Akker et al previously showed in a meta-analysis that invasive MV is associated with a threefold increase in the risk of AKI.10 The clinical data indicated that hypoxemia, hypercapnia, high PEEP value, and high tidal volume are risk factors for AKI development in patients with MV.6,11 Previous studies mostly examined the incidence, risk factors, and all-cause mortality or renal prognosis of AKI in elderly patients.12–14 However, few studies have investigated whether AKI increases the risk of cardiovascular instability, incident gastrointestinal bleeding, severe hypoxemia, and new-onset electrolyte imbalances in critically elderly patients undergoing MV.5,15
Thus, understanding whether accompanying AKI is a bystander phenomenon or an important marker of disease severity and a negative prognostic factor for subsequent complications is important for clinical management. Therefore, the aim of this study was to investigate the relationship of AKI severity in geriatric inpatients with subsequent complications over the first 48 hours under MV and all-cause 90-day mortality.
Methods
Study Design, Setting, and Population
This retrospective, observational, multicenter cohort study enrolled 3271 consecutive elderly patients (≥ 75 years) who received invasive MV in any of four medical centers of the Chinese PLA General Hospital from January 2008 to December 2020. Investigators included all consecutive critically ill elderly patients with life-threatening impairment of the cardiovascular, respiratory, or neurological system requiring in-hospital intubation during the study period at each center. Only patients ventilated for ≥ 48 hours with at least two Scr examinations within the first 48 hours of MV were included in the study. The study design was approved by the Clinical Ethics Committee of the Chinese PLA General Hospital (number: S2017–054–01). The requirement to obtain written informed consent from each patient was waived because this was an observational retrospective study. The patients’ information was anonymous and deidentified. This study was conducted in accordance with the Declaration of Helsinki.
Definitions
No definition for the diagnosis of AKI with MV is currently available; therefore, we used the current 2012 Kidney Disease Improving Global Outcomes (KDIGO) definition as the major screening criterion:16 AKI was diagnosed with reference (exclusively) to the patient’s Scr level, specifically, by an Scr increase of ≥26.5 µmol/L within 48 h after MV. Day 0 was the day of MV initiation, with Day 1 beginning at 8:00 a.m. on the next calendar day. The difference in Scr was calculated as the maximum variation in any Scr value on Days 0, 1, or 2.17 The baseline Scr level was defined as the most recent measurement in the previous 3 months.18 When no prior Scr records were available, we used the lowest Scr determination during hospitalization as the baseline Scr level.7 Sepsis was defined according to the Sepsis–3 criteria.19 For patients with multiple hospitalizations, we included only the first hospitalization in the analysis set.
Data Collection
Clinical data were noted, including demographic profiles (age, sex, and body mass index [BMI]) and comorbidities (history of coronary disease, hypertension, cerebrovascular diseases, chronic obstructive pulmonary disease [COPD], chronic kidney disease (CKD)20 and diabetes mellitus), the need for renal replacement therapy, the mean arterial pressure and the reason for MV.
Exclusion Criteria
The exclusion criteria were a history of CKD stages 4–5, renal replacement therapy before MV, nephrectomy, kidney transplantation, no Scr or only one Scr examination, a missing or incomplete medical history, hospital stay < 48 h and postoperative MV for the purposes of general anesthesia. As the aim of the study was to investigate the relationship of early AKI severity with subsequent complications (AKI developed within the first 48 hours of MV), patients with AKI before MV were also excluded to avoid the inclusion of patients with ongoing kidney failure.
Outcome Measures
The primary outcome of the study was the incidence and profile of major adverse peri-intubation complications defined by the occurrence of at least 1 of the following conditions within 48 hours from the start of the intubation procedure, including incident gastrointestinal bleeding, new-onset electrolyte imbalances, severe hypoxemia, hypoalbuminemia, any cardiovascular instability and all-cause 90-day mortality. (1) Cardiovascular instability was defined by a mean arterial pressure <65 mmHg recorded at least once, systolic blood pressure <90 mmHg for >30 minutes or a new requirement for or a need for an increased dose of vasopressors. (2) Any episode of incident gastrointestinal bleeding was monitored within the first 48 hours of MV. We included macroscopic bleeding episodes and clinically suspicious bleeding episodes, which were confirmed by a positive stool occult blood assay. (3) Severe hypoxemia was defined by an oxygen saturation measured by pulse oximetry SpO2 <80%. (4) Hypoalbuminemia was defined by an albumin was normal at Day 0 but <30g/L within the first 48 hours of MV. (5) A new-onset electrolyte imbalance was documented if any electrolyte was normal at Day 0 but became abnormal within the first 48 hours of MV or if a patient progressed from hypokalemia/hyperkalemia to hyperkalemia/hypokalemia, hyponatremia/hypernatremia to hypernatremia/hyponatremia, hypocalcemia/hypercalcemia to hypercalcemia/hypocalcemia, hypophosphatemia/hyperphosphatemia to hyperphosphatemia/hypophosphatemia, or hypomagnesemia/hypermagnesemia to hypermagnesemia/hypomagnesemia, respectively. The serum biochemistry panel and electrolyte profile (potassium, sodium, calcium, phosphate, magnesium and albumin) were routinely evaluated 1 or 2 times per day after MV by the attending physician. Dyskalemia, dysnatremia, dyscalcemia, dysphosphatemia, and dysmagnesemia were each defined as follows: dyskalemia as hypokalemia (K<3.5 mmol/L) or hyperkalemia (K>5.5 mmol/L), dysnatremia as hyponatremia (Na<135 mmol/L) or hypernatremia (Na>145 mmol/L), dyscalcemia as hypocalcemia (calcium< 2.1 mmol/L) or hypercalcemia (calcium>2.6 mmol/L), dysphosphatemia as hypophosphatemia (phosphate<0.8 mmol/L) or hyperphosphatemia (phosphate>1.5 mmol/L), and dysmagnesemia as hypomagnesemia (magnesium<0.7 mmol/L) or hypermagnesemia (magnesium>1.1 mmol/L).
Statistical Analysis
Continuous parametric variables are expressed as the means ± standard deviations (SDs), and continuous nonparametric variables are presented as the medians with interquartile ranges (25th and 75th percentiles). Categorical variables are given as numbers (n) or percentages (%). Between-group comparisons of continuous variables were performed using Student’s t-test or the Mann–Whitney U-test, and Pearson’s chi-squared or Fisher’s exact test was used to compare categorical variables. Three-group comparisons were conducted using one-way ANOVA or the Kruskal–Wallis H-test for continuous variables and Pearson’s chi-square or Fisher’s exact test for categorical variables. Logistic regression analyses and a forward stepwise selection method were performed to identify the effect of AKI on peri-intubation complications. Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) Version 17.0 for Windows (SPSS Inc., Chicago, IL, USA). A P–value<0.05 was considered indicative of statistical significance.
Results
General Characteristics of Patients Included in the Study
Between January 2008 and December 2020, a total of 3271 very elderly patients received invasive MV. Among these patients, 737 were excluded due to incomplete medical data, 554 for having fewer than two Scr examinations, 267 due to hospital stays < 48 hours, 171 for having CKD stages 4–5, 164 for having AKI before MV, 69 for undergoing renal replacement therapy before MV and 17 due to nephrectomy or kidney transplantation, resulting in 1292 patients with MV who were suitable for analysis. The study flow chart is shown in Figure 1. The 1292 study patients had a median age of 89 (85–92) years, and most patients (1171, 90.6%) were male. The causes of MV were sepsis (38.5%), pneumonia (21.4%), COPD with acute exacerbation (9.6%), acute heart failure (7.9%), acute coronary syndrome (5.5%), cardiac arrest (2.6%), emergency or urgent procedures (6.2%), airway obstruction (4.8%) and neuromuscular disease (3.6%). The most common comorbid conditions were hypertension (72.4%), coronary disease (71.1%), cerebrovascular diseases (53.6%), COPD (48.7%), diabetes mellitus (40.0%) and CKD (24.1%). The baseline characteristics and outcomes of the study population are summarized in Table 1. The all-cause 90-day mortality rate was 45.2%.
 |
Table 1 Baseline and Clinical Characteristics of Elderly Patients with AKI and without AKI |
 |
Figure 1 Flowchart of the patient inclusion and exclusion process. |
Characteristics Associated with AKI and Non-AKI
Three hundred seventy-six patients (29.1%) fulfilled the KDIGO diagnostic criteria according to their absolute increase in Scr over the first 48 hours under MV. Among these 376 patients, 118 (31.4%) had stage 1 AKI, 132 (35.1%) had stage 2 AKI, 126 (33.5%) had stage 3 AKI, and renal replacement therapy was required in only 8.8% (33/1292) of the AKI patients.
As shown in Table 1, the comparisons of elderly patients with and without AKI and of those with different stages of AKI indicated no significant differences in age, sex or BMI, but significant differences were found in baseline Scr (P<0.001), Scr (P<0.001) on Day 0, Scr at AKI diagnosis (P<0.001), and peak Scr (P<0.001). Patients with AKI were significantly more likely to have COPD (P<0.001) and CKD (P<0.001). Among patients with different stages of AKI, no significant differences in the presence of comorbidities were found. As shown in Table 1, the reason for MV (pneumonia P=0.020, acute coronary syndrome P<0.001, emergency or urgent procedure P=0.034, airway obstruction P=0.018) significantly differed between the AKI and non-AKI groups. Among patients with different stages of AKI, patients with more advanced AKI were less likely to require MV for emergency or urgent procedures (P=0.023) or due to airway obstruction (P=0.004) but had significantly higher Scr at AKI diagnosis (P<0.001) and peak Scr (P<0.001) levels.
Clinical Courses and Outcomes
The overall 90-day mortality rate was 45.2%; the non-AKI group had a 38.9% mortality rate, while the AKI group had a 60.6% mortality rate on average. The mortality rate increased significantly with AKI stage (37.3% for stage 1, 54.5% for stage 2, and 88.9% for stage 3; P<0.001) (Figure 2).
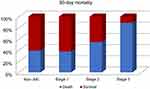 |
Figure 2 Ninety-day mortality of geriatric patients without AKI and with AKI stage 1, 2, and 3. |
As shown in Table 2, The most common complications were any electrolyte imbalance (52.2%), cardiovascular instability including a new requirement for or a need for an increased dose of vasopressors (48.5%), MAP<65 mmHg (39.5%), SBP<90 mmHg for >30 min (36.9%), gastrointestinal bleeding (25.5%), severe hypoxia (23.8%), and hypoalbuminemia (17.0%). The incidence of any cardiovascular instability (all P<0.001), gastrointestinal bleeding (P<0.001), and severe hypoxia (P=0.001) were significantly higher in the AKI group than in the non-AKI group, but the rate of incident electrolyte imbalances (dyskalemia, dysnatremia, dyscalcemia, dysphosphatemia and dysmagnesemia) was similar (all P>0.05). Furthermore, elderly individuals with more severe AKI were also more likely to develop MAP<65 mmHg (stage 1 vs 2 vs 3, 44.9% vs 67.4% vs 68.3%, P<0.001), SBP<90 mmHg (stage 1 vs 2 vs 3, 39.8% vs 59.8% vs 69.8%, P<0.001), a new requirement for or a need for an increased dose of vasopressors (stage 1 vs 2 vs 3, 51.7% vs 68.2% vs 88.9%, P<0.001), and gastrointestinal bleeding (stage 1 vs 2 vs 3, 24.6% vs 30.3% vs 41.3%, P=0.013).
 |
Table 2 Complications of Elderly Patients with and without Acute Kidney Injury |
Table 2 also shows dysphosphatemia was the most common electrolyte imbalance (23.1%), followed by dysnatremia (16.7%), dyscalcemia (14.6%), dyskalemia (9.6%), and dysmagnesemia (9.2%). Among patients with different stages of AKI, no significant difference was identified between the 3 cohorts in terms of electrolyte imbalances.
Next, we used multiple regression analyses to determine the significant predictors of complications. The results showed that more advanced AKI increased the risk of MAP< 65 mmHg (stage 1: OR=1.833, 95% CI=1.242–2.705, P=0.002; stage 2: OR= 4.653, 95% CI=3.150–6.874, P<0.001; stage 3: OR=4.834, 95% CI=3.239–7.214, P<0.001) and SBP< 90 mmHg (stage 1: OR=1.644, 95% CI=1.107–2.441, P=0.014; stage 2: OR=3.701, 95% CI=2.540–5.392, P<0.001; stage 3: OR=5.750, 95% CI=3.829–8.634, P<0.001), a new requirement for or a need for an increased dose of vasopressors (stage 1: OR=1.623, 95% CI=1.105–2.384, P=0.014; stage 2: OR=3.250, 95% CI=2.201–4.797, P<0.001; stage 3: OR=12.132, 95% CI=6.853–21.477, P<0.001), gastrointestinal bleeding (stage 1: OR=1.102, 95% CI=0.705–1.723, P=0.669; stage 2: OR=1.471, 95% CI=0.984–2.199, P=0.060; stage 3: OR=2.377, 95% CI=1.615–3.500, P<0.001), severe hypoxia (stage 1: OR=1.213, 95% CI=0.775–1.898, P=0.399; stage 2: OR=1.449, 95% CI=0.960–2.188, P=0.077; stage 3: OR=2.214, 95% CI=1.493–3.284, P<0.001), and all-cause 90-day mortality (stage 1: OR =0.935, 95% CI=0.629–1.390, P=0.741; stage 2: OR=1.888, 95% CI=1.307–2.726, P=0.001; stage 3: OR=12.584, 95% CI=7.108–22.280, P<0.001) Table 3, Figure 3.
 |
Table 3 Multiple Regression Analyses of Elderly Patients with and without AKI, with Complications as the Dependent Variables |
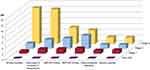 |
Figure 3 Risk of incident in-hospital complications in geriatric patients without AKI and with AKI stage 1, 2, and 3. |
Discussion
The results of this study indicate that elderly patients with invasive MV had a greater risk of developing subsequent complications, including AKI, gastrointestinal bleeding, new-onset electrolyte imbalances, severe hypoxemia, cardiovascular instability and all-cause 90-day mortality. The risk of developing subsequent complications increased with the initial severity of AKI. In addition, subanalyses indicated that more severe initial AKI significantly increased the risk of such complications. These findings are the first of their kind and suggest that AKI has an important impact on peri-intubation complications in addition to its established effect on 90-day mortality.
The incidence of AKI in the elderly population is typically higher than that in the general population because elderly individuals are more likely to have renal structural declines and multiple comorbidities. Previous studies reported that the incidence of AKI among patients over the first 48 hours under MV ranged from 15.5 to 17.1%, with most patients having stage 1 disease.17,21 We found that nearly 30% of geriatric patients had AKI at rates higher than those reported in previous studies. In addition, the pathophysiology of AKI in MV patients is related to nonspecific mechanisms, such as septic shock, hypovolemia and subsequent prerenal AKI, nephrotoxic drugs, and injurious MV strategies. The fundamental pathophysiology of sepsis in critically ill patients is impaired gas exchange and severe hypoxemia, which have been recognized as factors associated with AKI. Injurious MV strategies may affect the kidney by causing hemodynamic abnormalities and can cause hypotension and fluid reactive shock, affecting renal perfusion by decreasing the GFR by reducing cardiac output and stimulating hormonal and sympathetic pathways. MV with permissive hypercapnia or permissive hypoxemia can lead to renal hypoperfusion, a decreased GFR, and functional renal insufficiency.7 In this aspect, hemodynamic changes directly determined by MV may also be related to AKI development. This aspect may contribute to the COPD patients showing an increased risk of early AKI in the study since these patients are particularly prone to the deleterious effects of MV, such as lung hyperinflation associated with autoPEEP. Kidneys are responsible for maintaining water homeostasis, and AKI can augment the effect of in-hospital complications on the clinical consequences.
Hospitalized patients have a higher risk of developing in-hospital complications, but the exact incidence varies according to complication definitions and the reasons for hospitalization. In the elderly population, the incidence of in-hospital complications is expected to be higher because of diminished organ function, decreased physiologic reserves, frailty, and the higher prevalence of disability and functional impairment.22–24 Indeed, several reports have indicated that elderly patients have a 20 to 30% greater incidence of hospital complications after surgery. This number would be even greater if the complication definitions extend beyond those related to surgery. For example, a prospective observational study by Chao CT et al enrolled 163 elderly (≥65 years) patients admitted to general medical wards with a mean age of 80.3 ± 8.1 years. They defined AKI according to the Scr criteria of the KDIGO classification. The authors reported that the overall rate of in-hospital complications was 77%, including incident gastrointestinal bleeding at rates of 53% in non-AKI patients and 45% in AKI patients and any incident electrolyte imbalance at rates of 39% in non-AKI patients and 81% in AKI patients. They found that dyskalemia was the most common electrolyte imbalance (43%), followed by dysnatremia (31%), indicating that more severe initial AKI significantly increased the risk of new-onset electrolyte imbalances (especially sodium, potassium, calcium, and phosphate imbalances).
AKI is widely recognized to be associated with prolonged hospitalization and poorer outcomes, but few studies have examined the association between AKI and in-hospital complications. Available reports often consider AKI to be a type of hospital complication rather than a preceding or precipitating event. A large-scale study indicated that patients with AKI had a 1.9-fold higher risk of gastrointestinal bleeding during hospitalization, and another study reported that episodes of postoperative AKI increase the risk of nosocomial infections. In the present study, we found that AKI increases the risk of in-hospital complications in the elderly population, particularly cardiovascular instability. In support of this finding, these risks increased incrementally with higher AKI stages. These relationships potentially shed light on the elusive relationship between initial AKI early during intubation and subsequent adverse in-hospital events. However, we did not detect statistically significant associations between AKI stage and subsequent incident electrolyte imbalances. These negative findings could partially result from nearly all AKI stages, the definitions of electrolyte imbalance that we used in this study, or our study window.
We have no satisfactory explanation for the finding of no significant difference between the AKI stages in terms of incident electrolyte imbalances; however, some reasons may include (1) the population studied and the definition of AKI or electrolyte disorders; (2) our measurement of the electrolyte level at the time of AKI onset and not during the entire hospitalization period and AKI staging calculated according to the entire course of the disease, resulting in a time difference between the two; and (3) our inclusion of only elderly people, most of whom are hospitalized for a long time. Clinicians focus more on electrolyte levels and frequently supplement them, including fluid resuscitation after tracheal intubation, which improves electrolyte levels. Therefore, the incidence of electrolyte disturbance is not high.
Postintubation hypotension is common in critically ill patients, with reported incidence rates ranging between 20–52%. We report a similar experience with an incidence ranging from 37% to 40%. Hypotension in critically ill patients is associated with an increased risk of mortality and the development of AKI. One multicenter retrospective study by Maheshwari et al evaluating 8782 septic patients found that for every unit increase in the time-weighted average of MAP <65 mmHg, the odds of in-hospital mortality increased 11.4%, and the odds of AKI increased 7.0%.25 The presentation of lower SBP and MAP in elderly patients with AKI is interesting, which we suggest may be related to the reasons for tracheal intubation. Airway management in critically ill patients differs significantly from tracheal intubation carried out for routine surgical procedures in operating rooms. In operating rooms, elective intubation is performed in stable patients with good physiological reserves by skilled anesthesiologists, and tracheal intubation is associated with very low rates of complications.
Elderly patients with invasive MV have a high risk of suffer from AKI, which is usually an indicator of more severe disease and multiorgan dysfunction. So kidney function protection should be an important part of clinical treatment. However, one notable factor in the burden of AKI is the very high nonrecognition rate of AKI by the physicians in charge. A nationwide survey in China demonstrated that Chinese nonnephrologists still had poor general knowledge of AKI. The missed diagnosis rate of AKI was as high as 53–74%;26–28 even in the ICU, 73% of AKI patients were missed.29 We assume that one possible explanation may be the definition and diagnostic criteria of AKI, which is neither uniformly known nor applied in nonkidneydepartments. Much attention has been focused on cardiovascular or pulmonary complications, while little attention has been given to renal function.
Limitations
First, the study excluded patients who were intubated in the operating room or for the purposes of general anesthesia; thus, the results may not be generalizable to other patients. Second, the diagnosis of AKI depends on an increase in Scr and/or a decrease in urine volume. We lacked data on urine output, the exclusion of 737 patients with incomplete medical information (22.5%) and 554 (16.9%) with less than two Scr measurements, and we screened and evaluated AKI using only the 48-hour diagnostic window within the first 48 hours of MV, which may have led to underestimation of the true incidence of AKI. Third, the multicenter design of the study could bias the results because most patients were elderly males, with fewer females treated in our hospital. Fourth, some important information was lacking in the database, such as arterial blood gas values (pH and HCO3), daily fluid balance, fluid management or the type of fluid, the length of hospital stay, MV time, sequential organ failure assessment or Acute Physiologic and Chronic Health Evaluation II score and lactate levels.
Conclusion
In this study, the presence of AKI within the first 48 hours of MV in geriatric patients was associated with a higher risk for postintubation complications, especially cardiovascular instability, hypoalbuminemia and 90-day mortality. Moreover, the risk of complications was greater for patients with more severe AKI. Intensivists should focus more on postintubation complications, and larger populations must be studied to confirm our findings.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
This study has been approved by the Ethics Committee of the Chinese PLA General Hospital (Number: S2017–054–01).
Informed Consent
The requirement for written informed consent was waived by the ethics committee of the designated hospital because this was an observational retrospective study.
Consent for Publication
The manuscript has been read and its submission approved by all coauthors.
Acknowledgments
This manuscript was edited for English language by American Journal Experts (AJE).
Funding
This study was funded by grants from the Special Scientific Research Project of Military Health Care (grant 20BJZ27 to Dr FHZ) and National Natural Science Foundation of China (grant 81871581 to Dr FHZ).
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188(2):220–230. doi:10.1164/rccm.201212-2169OC
2. Walter JM, Corbridge TC, Singer BD. Invasive mechanical ventilation. South Med J. 2018;111(12):746–753. doi:10.14423/SMJ.0000000000000905
3. Husain-Syed F, Slutsky AS, Ronco C. Lung-kidney cross-talk in the critically ill patient. Am J Respir Crit Care Med. 2016;194(4):402–414. doi:10.1164/rccm.201602-0420CP
4. Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287(3):345–355. doi:10.1001/jama.287.3.345
5. Russotto V, Myatra SN, Laffey JG, et al. Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA. 2021;325(12):1164–1172. doi:10.1001/jama.2021.1727
6. Koyner JL, Murray PT. Mechanical ventilation and the kidney. Blood Purif. 2010;29(1):52–68. doi:10.1159/000259585
7. Li Q, Zhang T, Li F, et al. Acute kidney injury can predict in-hospital mortality in elderly patients with COVID-19 in the ICU: a Single-Center Study. Clin Interv Aging. 2020;15:2095–2107. doi:10.2147/CIA.S273720
8. Kellum JA, Romagnani P, Ashuntantang G, et al. Acute kidney injury. Nat Rev Dis Primers. 2021;7(1):52. doi:10.1038/s41572-021-00284-z
9. Denic A, Glassock RJ, Rule AD. Structural and functional changes with the aging kidney. Adv Chronic Kidney Dis. 2016;23(1):19–28. doi:10.1053/j.ackd.2015.08.004
10. van den Akker JP, Egal M, Groeneveld AB. Invasive mechanical ventilation as a risk factor for acute kidney injury in the critically ill: a systematic review and meta-analysis. Crit Care. 2013;17(3):R98. doi:10.1186/cc12743
11. Koyner JL, Murray PT. Mechanical ventilation and lung-kidney interactions. Clin J Am Soc Nephrol. 2008;3(2):562–570. doi:10.2215/CJN.03090707
12. Li Q, Zhao M, Zhou F. Hospital-acquired acute kidney injury in very elderly men: clinical characteristics and short-term outcomes. Aging Clin Exp Res. 2020;32(6):1121–1128. doi:10.1007/s40520-019-01196-5
13. Li Q, Zhao M, Wang X. The impact of transient and persistent acute kidney injury on short-term outcomes in very elderly patients. Clin Interv Aging. 2017;12:1013–1020. doi:10.2147/CIA.S135241
14. Li Q, Zhao M, Du J, et al. Outcomes of renal function in elderly patients with acute kidney injury. Clin Interv Aging. 2017;12:153–160. doi:10.2147/CIA.S121823
15. Smischney NJ, Kashyap R, Khanna AK, et al. Risk factors for and prediction of post-intubation hypotension in critically ill adults: a multicenter prospective cohort study. PLoS One. 2020;15(8):e0233852. doi:10.1371/journal.pone.0233852
16. Joannidis M, Forni LG, Klein SJ, et al. Lung-kidney interactions in critically ill patients: consensus report of the Acute Disease Quality Initiative (ADQI) 21 Workgroup. Intensive Care Med. 2020;46(4):654–672. doi:10.1007/s00134-019-05869-7
17. Lombardi R, Nin N, Lorente JA, et al. An assessment of the Acute Kidney Injury Network creatinine-based criteria in patients submitted to mechanical ventilation. Clin J Am Soc Nephrol. 2011;6(7):1547–1555. doi:10.2215/CJN.09531010
18. Wang Y, Wang J, Su T, et al. Community-acquired acute kidney injury: a Nationwide Survey in China. Am J Kidney Dis. 2017;69(5):647–657. doi:10.1053/j.ajkd.2016.10.034
19. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
20. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
21. Lombardi R, Nin N, Penuelas O, et al. Acute kidney injury in mechanically ventilated patients: the risk factor profile depends on the timing of aki onset. Shock. 2017;48(4):411–417. doi:10.1097/SHK.0000000000000871
22. Abdel-Kader K, Girard TD, Brummel NE, et al. Acute kidney injury and subsequent frailty status in survivors of critical illness: a secondary analysis. Crit Care Med. 2018;46(5):e380–e388. doi:10.1097/CCM.0000000000003003
23. Baek SH, Lee SW, Kim SW, et al. Frailty as a predictor of acute kidney injury in hospitalized elderly patients: a Single Center, Retrospective Cohort Study. PLoS One. 2016;11(6):e0156444. doi:10.1371/journal.pone.0156444
24. Muscedere J, Waters B, Varambally A, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–1122. doi:10.1007/s00134-017-4867-0
25. Maheshwari K, Nathanson BH, Munson SH, et al. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018;44(6):857–867. doi:10.1007/s00134-018-5218-5
26. Yang C, Yang B. Acute kidney injury in China: a neglected truth and perspective. Asian J Urol. 2016;3(1):4–5. doi:10.1016/j.ajur.2015.11.001
27. Yang L, Xing G, Wang L, et al. Acute kidney injury in China: a cross-sectional survey. Lancet. 2015;386(10002):1465–1471. doi:10.1016/S0140-6736(15)00344-X
28. Cheng X, Wu B, Liu Y, et al. Incidence and diagnosis of Acute kidney injury in hospitalized adult patients: a retrospective observational study in a tertiary teaching Hospital in Southeast China. BMC Nephrol. 2017;18(1):203. doi:10.1186/s12882-017-0622-6
29. Tang X, Chen D, Yu S, et al. Acute kidney injury burden in different clinical units: data from nationwide survey in China. PLoS One. 2017;12(2):e0171202. doi:10.1371/journal.pone.0171202
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
