Back to Journals » OncoTargets and Therapy » Volume 8
Association between the polymorphisms of urokinase plasminogen activation system and cancer risk: a meta-analysis
Authors Xu Z, Meng L, Lin J, Ling Y, Chen S, Lin N
Received 26 March 2015
Accepted for publication 4 July 2015
Published 9 September 2015 Volume 2015:8 Pages 2493—2502
DOI https://doi.org/10.2147/OTT.S85520
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Faris Farassati
Zhen Xu,1,* Li-Li Meng,2,* Jizong Lin,3 Yunbiao Ling,3 Shu-xian Chen,3 Nan Lin3
1Department of Infectious Diseases, The Third Affiliated Hospital, Sun Yat-sen University, 2Department of Gynecology and Obstetrics, Sun Yat-sen Memorial Hospital, 3Department of Hepatobiliary Surgery, The Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, People’s Republic of China
*These authors contributed equally to this study
Purpose: The present study aimed to investigate the potential association between the urokinase plasminogen activation (uPA) system polymorphisms (rs4065, rs2227564, and rs344781) and cancer risk.
Methods: An extensive search was performed to identify published case–control studies on the association between the uPA system polymorphisms and cancer risk. Odds ratios (ORs) with 95% confidence intervals (CIs) were used to evaluate the relationship between the uPA system polymorphisms and cancer risk.
Results: A total of 20 studies comprising 7,037 cancer cases and 10,094 controls were identified and included in the present meta-analysis. Overall, significantly increased cancer risk was associated with the uPA polymorphism rs4065 (T vs C: OR 1.50, 95% CI: 1.19–1.89; TT vs CC: OR 4.63, 95% CI: 3.10–6.91; dominant model: OR 1.93, 95% CI: 1.60–2.33; recessive model: OR 3.02, 95% CI: 1.26–7.25) and the uPA receptor polymorphism rs344781 (T vs C: OR 1.13, 95% CI: 1.04–1.23; TC vs CC: OR 1.26, 95% CI: 1.06–1.49; TT vs CC: OR 1.35, 95% CI: 1.13–1.63; dominant model: OR 1.29, 95% CI: 1.10–1.52). No significant association was found between the uPA polymorphism rs2227564 and cancer risk. Subgroup analysis suggests that the T allele of the rs4065 (T allele vs C allele: OR 1.50, 95% CI: 1.19–1.89) and rs344781 polymorphisms (T allele vs C allele: OR 1.13, 95% CI: 1.04–1.23) was associated with increased cancer risk in Asians.
Conclusion: Our results suggest that the uPA polymorphism rs4065 and the uPA receptor polymorphism rs344781 are associated with increased cancer risk.
Keywords: uPA system, polymorphisms, cancer, meta-analysis
Background
The urokinase plasminogen activation (uPA) system, including the ligand uPA, the urokinase plasminogen activation receptor (uPAR), and the plasminogen activator inhibitor-1 (PAI-1) and plasminogen activator inhibitor-2 (PAI-2), is a serine proteinase system involved in the degradation of extracellular matrix (ECM). The uPA system plays an important role in tumor invasion and metastasis, and is associated with poor prognosis of cancers.1–4 The uPA ligand binds to the uPAR receptor, a three-domain glycolipid-anchored cell surface protein. The binding of inactive precursor pro-uPA to uPAR-activated surface-bound plasminogen results in the formation of plasmin and matrix metalloproteinase, which enhances the degradation of most components of ECM and the basement membranes.5–7 It has been reported that the levels of uPA components were associated with poor prognosis and high mortality of a wide range of malignancies1,2,8–10 due to their roles in metastasis. The effects of uPA/uPAR on plasminogen activation are regulated by their specific inhibitors PAI-1 and PAI-2.3,11–13
Epidemiological studies have evidenced that both environmental carcinogens and genetic factors contributed to cancer susceptibility. Given that single-nucleotide polymorphisms (SNPs) within the promoter or other regulatory regions of the genes encoding the uPA system may affect their expression and activities, SNP identification based on genotyping approaches is useful for investigating the association between these SNPs, cancer risk, and prognosis.14 In the past few decades, a large number of epidemiological studies have evaluated the association between the genetic variations of genes encoding the uPA system and the risk of breast cancer, prostate cancer, non-small-cell lung cancer, gastric cancer, endometrial cancer, hepatocellular carcinoma, and oral cancer; however, the results of these studies were conflicting.14–20 Interestingly, a meta-analysis has found an association between the PAI-1 4G/5G polymorphism (rs1799768) and increased cancer risk.21 In the present study, we conducted a meta-analysis to systemically evaluate the association between the uPA system polymorphisms and cancer risk.
Methods
Selection of published studies
Published studies, which have been published no later than November 13, 2014, were identified by searching the PubMed, Embase, and Web of Science databases using the following MeSH terms and keywords: uPA (PLAU), uPAR, urokinase plasminogen activation, urokinase plasminogen activation receptor, polymorphism, cancer, carcinoma, and neoplasms. The reference lists of retrieved studies were also searched to identify relative studies. Studies included in the present meta-analysis were as follows: 1) articles investigating the association between the uPA system polymorphisms rs4065, rs2227564, and rs344781 and cancer risk; 2) case–control studies; 3) studies providing genotype frequency for computing odds ratios (ORs) with 95% confidence intervals (CIs); and 4) studies with full text articles. The exclusion criteria were as follows: 1) only case population studies without comparison outcomes reported or not possible to determine comparison outcomes; 2) duplicated publications; and 3) benign tumors and/or precancerous lesions.
Data extraction
Two investigators independently screened the manuscript titles, abstracts, and full texts using a standardized extraction form. For conflicting evaluation, an agreement was reached based on consensus and discussion. For each study, the following data were extracted: the first author’s name, year of publication, country of origin, ethnicity, genotyping methods, source of control, cancer type, total numbers of cases and controls, and genotype distributions in cases and controls. We did not define a minimum number of patients in each study for the present meta-analysis.
Evaluation of study quality and validation of study
The quality of studies was assessed by quality scores using a standardized extraction form according to previous studies with minor modification (Table S1).22,23 The total quality score ranged from 0 (the lowest quality) to 20 (the highest quality). The analyses were stratified according to the study quality.
Statistical analyses
Statistical analyses were performed using STATA software (Version 11.0; StataCorp LP, College Station, TX, USA), and all tests were two-sided with a significant level of 0.05, unless stated otherwise. The Hardy–Weinberg equilibrium (HWE) in controls was assessed using chi-squared test, and a P-value <0.05 was considered as significant disequilibrium. If the HWE existed (P<0.05) or it was impossible to evaluate the HWE, sensitivity analysis was performed. The strength of the association between the uPA system polymorphisms and cancer risk was evaluated on the basis of ORs with 95% CIs. The Q-statistic was used to test heterogeneities among the studies included in the meta-analysis.24 When the Q-test P-value was not <0.1, fixed effect model with Mantel–Haenszel method was used to calculate the pooled ORs.25 Otherwise, a random effect model with inverse variance method was used. Taking the uPA polymorphism rs4065 as an example, pooled ORs were obtained from the combination of all studies by heterozygote comparison (TC vs CC), homozygote comparison (TT vs CC), dominant and recessive models (TT + TC vs CC and TT vs TC + CC), and allelic comparison (T vs C). Similarly, comparison of the results of other polymorphisms was also obtained. In addition, we also performed stratification analyses according to ethnicity and quality score: high-quality studies (quality score >15) vs low-quality studies (quality score <15). Begg’s and Egger’s tests were used to evaluate publication bias.26,27
Results
Characteristics of the studies
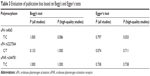
A total of 62 studies were included in this meta-analysis based on the search strategy using different combinations of keywords (Figure 1). Through reviewing the abstracts and full texts, 20 case–control studies from 13 articles met our inclusion criteria.14,17–20,28–35 A total of 7,037 cancer cases and 10,094 controls were included in the 20 case–control studies. The characteristics of these studies are listed in Table 1. Among them, seven studies including 1,233 cancer cases and 1,919 controls investigated the uPA polymorphism rs4065, six studies including 2,343 cancer cases and 2,780 controls studied the uPA polymorphism rs2227564, and seven studies including 2,265 cancer cases and 3,241 controls were about the uPAR polymorphism rs344781. The distribution of genotypes in the controls of all studies was consistent with HWE.
  | Figure 1 The inclusion and exclusion criteria used in the selection of published studies on the polymorphisms of uPA system and cancer risk. |
Meta-analysis
The significance of the association between uPA and uPAR polymorphisms and cancer risk is shown in Table 2. Overall, no significant association was found between the uPA polymorphism rs2227564 and cancer risk based on all genetic models (Table 2), whereas significantly increased cancer risk was associated with the uPA polymorphism rs4065 (T allele vs C allele: OR 1.50, 95% CI: 1.19–1.89; TT vs CC: OR 4.63, 95% CI: 3.10–6.91; dominant model: OR 1.93, 95% CI: 1.60–2.33; recessive model: OR 3.02, 95% CI: 1.26–7.25) (Figure 2) and the uPAR polymorphism rs344781 (T allele vs C allele: OR 1.13, 95% CI: 1.04–1.23; TC vs CC: OR 1.26, 95% CI: 1.06–1.49; TT vs CC: OR 1.35, 95% CI: 1.13–1.63; dominant model: OR 1.29, 95% CI: 1.10–1.52) (Figure 3), which was consistent with the results from studies of high quality (Table 2).
  | Figure 3 Forest plot of ORs of the uPAR polymorphism rs344781 (T vs C). |
When the cases were stratified according to ethnicity, we found that the uPA polymorphism rs4065 (T allele vs C allele: OR 1.48, 95% CI: 1.11–1.95; TT vs CC: OR 5.52, 95% CI: 3.46–8.81; dominant model: OR 2.02, 95% CI: 1.65–2.47; recessive model: OR 5.53, 95% CI: 3.50–8.75) and the uPAR polymorphism rs344781 (T allele vs C allele: OR 1.16, 95% CI: 1.03–1.29; TC vs CC: OR 1.25, 95% CI: 1.02–1.54; TT vs CC: OR 1.35, 95% CI: 1.08–1.70; dominant model: OR 1.28, 95% CI: 1.06–1.56) were associated with increased cancer risk in Asians, which was consistent with the results of analyses of high quality. No significant association between the uPA polymorphisms rs4065 and rs344781 and cancer risk was found in the Caucasian population.
Subgroup studies were performed according to different cancer types (digestive system cancers and nondigestive system cancers). For digestive system cancers, meta-analyses of all studies and studies of high quality demonstrated a significant association between the uPA polymorphism rs4065 and increased risk of digestive system cancers based on the dominant model (the former: OR 1.60, 95% CI: 1.16–2.22; the latter: OR 1.86, 95% CI: 1.29–2.68). However, no significant association was detected between the uPAR polymorphism rs344781 and increased risk of digestive system cancers. Regarding nondigestive system cancers, we found that the uPA polymorphism rs4065 (TT vs CC: OR 4.61, 95% CI: 3.05–6.96; dominant model: OR 2.12, 95% CI: 1.68–2.67) and the uPAR polymorphism rs344781 (T allele vs C allele: OR 1.17, 95% CI: 1.06–1.30; TT vs CC: OR 1.43, 95% CI: 1.14–1.79; dominant model: OR 1.30, 95% CI: 1.06–1.59; recessive model: OR 1.20, 95% CI: 1.04–1.37) were associated with increased risk of nondigestive system cancers, which was consistent with the results from studies of high quality.
Subgroup studies were also performed according to the source of control. We found that the uPA polymorphism rs4065 (T allele vs C allele: OR 1.50, 95% CI: 1.19–1.89; TT vs CC: OR 4.63, 95% CI: 3.10–6.91; dominant model: OR 1.93, 95% CI: 1.60–2.33; recessive model: OR 3.02, 95% CI: 1.26–7.25) and the uPAR polymorphism rs344781 (T allele vs C allele: OR 1.16, 95% CI: 1.03–1.29; TC vs CC: OR 1.25, 95% CI: 1.02–1.54; TT vs CC: OR 1.35, 95% CI: 1.08–1.70; dominant model: OR 1.28, 95% CI: 1.06–1.56) were associated with increased cancer risk in hospital-based control studies, which was consistent with the results from studies of high quality. No significant association between the uPAR polymorphism rs344781and cancer risk was detected in the studies from population-based control.
Sensitivity analyses and publication bias
When examining the genotype frequencies in the controls, no significant deviation from HWE was detected, suggesting that the final results of this meta-analysis were reliable and stable. Both Begg’s and Egger’s tests were conducted to assess the publication bias of literatures. No evidence of publication bias was observed in the allele genetic model in the present meta-analysis (Table 3).36 Similar results were also observed in analyses restricted to other genetic models (data not shown).
  | Table 3 Evaluation of publication bias based on Begg’s and Egger’s tests |
Discussion
The uPA system plays an essential role in the degradation and regeneration of basement membrane and ECM, as well as cancer metastasis.11,12 The biological function of the uPA system may be impaired by SNPs within genes encoding the uPA system, resulting in altered susceptibility to cancers. The effects of genetic variations of the uPA system in cancer development have been recognized in recent years; however, the results are contradictory.14,17–20 In the present study, we provided a comprehensive meta-analysis to evaluate the association of the uPA system polymorphisms and cancer risk. To the best of our knowledge, this is the first systematic meta-analysis addressing the association between the uPA system polymorphisms (not the PAI-1) and cancer risk.
Yoshimoto et al37 reported that the CC genotype exhibited the strongest uPA affinity for substrates and inhibitors, resulting in the formation of uPA/uPAR and uPA/PAI-1 complexes and the activation of the uPA system. Our meta-analysis suggests that the T allele in the uPA polymorphism rs4065 was associated with a high incidence of cancers. Therefore, we speculate that the activation of the uPA system may be interrupted by the lower affinity of the rs4065 variant with its substrates and inhibitors. Based on stratified analysis of ethnicity, significant association between uPA polymorphism rs4065 and cancer risk was found in Asians. However, lack of case–control studies limited our evaluation on the association between the uPA polymorphism rs4065 and cancer risk among other ethnicities. In the subgroup analysis of cancer types, a significant association was identified between the polymorphism rs4065 and increased risk of both digestive and nondigestive system cancers based on a dominant model, which was consistent with the results from high-quality studies.
Regarding the general analysis of the uPAR polymorphism, we showed that the presence of minor alleles significantly increased the risk of cancers than major alleles, suggesting that genetic variations significantly modify the host susceptibility to cancers. In the subgroup analysis of ethnicity, significant association was identified between the polymorphism rs344781 and increased cancer risk in Asians rather than Caucasians. The inconsistent results between these two ethnicities may be explained by distinct lifestyles and environmental factors of these two ethnic groups. In the subgroup analysis of cancer types, we detected an association between the polymorphism rs344781 and the risk of nondigestive system cancers, but not the digestive system cancers. This difference between digestive and nondigestive system cancers may be explained by the differential expression, function, and regulatory mechanisms of the uPA and uPAR systems in various tissues and tumors.38–42
General analysis of the uPA polymorphism rs2227564 showed no significant association between the uPA polymorphism rs2227564 and cancer risk. However, case–control studies of large scale are necessary to ascertain the accurate effects of the rs2227564 polymorphism on cancer development.
A number of limitations in the present meta-analysis should be addressed. First, lack of original data of the reviewed studies limited our evaluation of the potential effects of gene–gene and gene–environment interactions. Second, all case–control studies were from People’s Republic of China, Taiwan, Europe, the US, and India. These results may be applicable only to the relative ethnicities. Third, the meta-analysis study should provide a more accurate evaluation on the association between the uPA polymorphisms and cancer risk by considering classic cancer risk factors, such as smoking, age, sex, and diabetes. At last, future studies should evaluate the association between the PAI-1 and PAI-2 polymorphisms and cancer risk when the original data are available.
In summary, the present meta-analysis study suggests that the uPA polymorphism rs4065 and the uPAR polymorphism rs344781 were associated with increased cancer risk in Asian population. In addition, subgroup analysis of cancer types suggests that the uPAR polymorphism rs344781 was associated with increased risk of nondigestive system cancers, but not the digestive system cancers. However, it is important to include larger samples with detailed clinical data, standardized unbiased genotyping methods, homogeneous cancer patients, and well-matched controls to further understand the association between the uPA polymorphisms and cancer risk in the future.
Conclusion
This meta-analysis found that the uPA polymorphism rs4065 and the uPAR polymorphism rs344781, not the uPA polymorphism rs2227564, are associated with increased cancer risk. However, well-designed case–control studies with larger sample size and more ethnicities are necessary to validate our findings in the future.
Acknowledgments
This study was supported by Science and Technology Planning Project of Guangdong Province, People’s Republic of China (no 2011B061200005) and by Doctoral Fund of Ministry of Education for new teacher, People’s Republic of China (no 20110171120090).
Disclosure
The authors report no conflicts of interest in this work.
References
Andreasen PA, Kjoller L, Christensen L, Duffy MJ. The urokinase-type plasminogen activator system in cancer metastasis: a review. Int J Cancer. 1997;72(1):1–22. | ||
Berger DH. Plasmin/plasminogen system in colorectal cancer. World J Surg. 2002;26(7):767–771. | ||
Duffy MJ. The urokinase plasminogen activator system: role in malignancy. Curr Pharm Des. 2004;10(1):39–49. | ||
Sidenius N, Blasi F. The urokinase plasminogen activator system in cancer: recent advances and implication for prognosis and therapy. Cancer Metastasis Rev. 2003;22(2–3):205–222. | ||
Gondi CS, Rao JS. Therapeutic potential of siRNA-mediated targeting of urokinase plasminogen activator, its receptor, and matrix metalloproteinases. Methods Mol Biol. 2009;487:267–281. | ||
Yang SF, Hsieh YS, Lue KH, Chu SC, Chang IC, Lu KH. Effects of nonsteroidal anti-inflammatory drugs on the expression of urokinase plasminogen activator and inhibitor and gelatinases in the early osteoarthritic knee of humans. Clin Biochem. 2008;41(1–2):109–116. | ||
Yang SF, Wang PH, Lin LY, et al. A significant elevation of plasma level of matrix metalloproteinase-9 in patients with high-grade intraepithelial neoplasia and early squamous cell carcinoma of the uterine cervix. Reprod Sci. 2007;14(7):710–718. | ||
Duffy MJ, Maguire TM, McDermott EW, O’Higgins N. Urokinase plasminogen activator: a prognostic marker in multiple types of cancer. J Surg Oncol. 1999;71(2):130–135. | ||
Sakakibara T, Hibi K, Koike M, et al. Plasminogen activator inhibitor-1 as a potential marker for the malignancy of colorectal cancer. Br J Cancer. 2005;93(7):799–803. | ||
Yang JL, Seetoo D, Wang Y, et al. Urokinase-type plasminogen activator and its receptor in colorectal cancer: independent prognostic factors of metastasis and cancer-specific survival and potential therapeutic targets. Int J Cancer. 2000;89(5):431–439. | ||
Hildenbrand R, Allgayer H, Marx A, Stroebel P. Modulators of the urokinase-type plasminogen activation system for cancer. Expert Opin Investig Drugs. 2010;19(5):641–652. | ||
Kwaan HC, McMahon B. The role of plasminogen-plasmin system in cancer. Cancer Treat Res. 2009;148:43–66. | ||
Pepper MS. Role of the matrix metalloproteinase and plasminogen activator-plasmin systems in angiogenesis. Arterioscler Thromb Vasc Biol. 2001;21(7):1104–1117. | ||
Su CK, Yeh KT, Yeh CB, et al. Genetic polymorphism of the plasminogen activator inhibitor-1 is associated with an increased risk of endometrial cancer. J Surg Oncol. 2011;104(7):755–759. | ||
Castello R, Espana F, Vazquez C, et al. Plasminogen activator inhibitor-1 4G/5G polymorphism in breast cancer patients and its association with tissue PAI-1 levels and tumor severity. Thromb Res. 2006;117(5):487–492. | ||
Jorgenson E, Deitcher SR, Cicek M, et al. Plasminogen activator inhibitor type-1 (PAI-1) polymorphism 4G/5G is associated with prostate cancer among men with a positive family history. Prostate. 2007;67(2):172–177. | ||
Shih CM, Kuo WH, Lin CW, et al. Association of polymorphisms in the genes of the urokinase plasminogen activation system with susceptibility to and severity of non-small cell lung cancer. Clin Chim Acta. 2011;412(1–2):194–198. | ||
Weng CJ, Lin CW, Chung TT, Tsai CM, Chen MK, Yang SF. Impact of uPA system gene polymorphisms on the susceptibility of environmental factors to carcinogenesis and the development of clinicopathology of oral cancer. Ann Surg Oncol. 2011;18(3):805–812. | ||
Weng CJ, Tsai CM, Chen YC, et al. Evaluation of the association of urokinase plasminogen activator system gene polymorphisms with susceptibility and pathological development of hepatocellular carcinoma. Ann Surg Oncol. 2010;17(12):3394–3401. | ||
Wu CY, Wu MS, Chen YJ, et al. Clinicopathological significance of urokinase-type plasminogen activator genotypes in gastric cancer. Hepatogastroenterology. 2008;55(86–87):1890–1894. | ||
Wang S, Cao Q, Wang X, et al. PAI-1 4G/5G polymorphism contributes to cancer susceptibility: evidence from meta-analysis. PLoS One. 2013;8(2):e56797. | ||
Camargo MC, Mera R, Correa P, et al. Interleukin-1beta and interleukin-1 receptor antagonist gene polymorphisms and gastric cancer: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15(9):1674–1687. | ||
Gao LB, Pan XM, Li LJ, et al. RAD51 135G/C polymorphism and breast cancer risk: a meta-analysis from 21 studies. Breast Cancer Res Treat. 2011;125(3):827–835. | ||
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. | ||
Petitti DB. Meta-Analysis, Decision Analysis, and Cost-Effectiveness Analysis: Methods for Quantitative Synthesis in Medicine. Oxford University Press; Oxford. 1999. | ||
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. | ||
Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Bentov Y, Brown TJ, Akbari MR, et al. Polymorphic variation of genes in the fibrinolytic system and the risk of ovarian cancer. PLoS One. 2009;4(6):e5918. | ||
Forsti A, Lei H, Tavelin B, et al. Polymorphisms in the genes of the urokinase plasminogen activation system in relation to colorectal cancer. Ann Oncol. 2007;18(12):1990–1994. | ||
Lei H, Hemminki K, Johansson R, et al. PAI-1-675 4G/5G polymorphism as a prognostic biomarker in breast cancer. Breast Cancer Res Treat. 2008;109(1):165–175. | ||
Mittal RD, Srivastava DS, Mishra DK. Is urokinase gene 3′-UTR polymorphism associated with prostate cancer? Cancer Biomark. 2005;1(6):287–292. | ||
Przybylowska K, Smolarczyk K, Blasiak J, et al. A C/T polymorphism in the urokinase-type plasminogen activator gene in colorectal cancer. J Exp Clin Cancer Res. 2001;20(4):569–572. | ||
Tee YT, Wang PH, Tsai HT, et al. Genetic polymorphism of urokinase-type plasminogen activator is interacting with plasminogen activator inhibitor-1 to raise risk of cervical neoplasia. J Surg Oncol. 2012;106(2):204–208. | ||
Tsai MH, Chen WC, Chen HY, Tsai FJ. Urokinase gene 3′-UTR T/C polymorphism is associated with oral cancer. J Clin Lab Anal. 2004;18(5):276–279. | ||
Turkmen B, Schmitt M, Schmalfeldt B, et al. Mutational analysis of the genes encoding urokinase-type plasminogen activator (uPA) and its inhibitor PAI-1 in advanced ovarian cancer. Electrophoresis. 1997;18(5):686–689. | ||
Garza-Gonzalez E, Bosques-Padilla FJ, Mendoza-Ibarra SI, Flores-Gutierrez JP, Maldonado-Garza HJ, Perez-Perez GI. Assessment of the toll-like receptor 4 Asp299Gly, Thr399Ile and interleukin-8-251 polymorphisms in the risk for the development of distal gastric cancer. BMC Cancer. 2007;7:70. | ||
Yoshimoto M, Ushiyama Y, Sakai M, et al. Characterization of single chain urokinase-type plasminogen activator with a novel amino-acid substitution in the kringle structure. Biochim Biophys Acta. 1996;1293(1):83–89. | ||
Ahmad A, Kong D, Wang Z, Sarkar SH, Banerjee S, Sarkar FH. Down-regulation of uPA and uPAR by 3,3′-diindolylmethane contributes to the inhibition of cell growth and migration of breast cancer cells. J Cell Biochem. 2009;108(4):916–925. | ||
Almasi CE, Hoyer-Hansen G, Christensen IJ, Pappot H. Prognostic significance of urokinase plasminogen activator receptor and its cleaved forms in blood from patients with non-small cell lung cancer. APMIS. 2009;117(10):755–761. | ||
Illemann M, Bird N, Majeed A, et al. Two distinct expression patterns of urokinase, urokinase receptor and plasminogen activator inhibitor-1 in colon cancer liver metastases. Int J Cancer. 2009;124(8):1860–1870. | ||
Kogianni G, Walker MM, Waxman J, Sturge J. Endo180 expression with cofunctional partners MT1-MMP and uPAR-uPA is correlated with prostate cancer progression. Eur J Cancer. 2009;45(4):685–693. | ||
Thomas C, Wiesner C, Melchior SW, et al. Urokinase-plasminogen-activator receptor expression in disseminated tumour cells in the bone marrow and peripheral blood of patients with clinically localized prostate cancer. BJU Int. 2009;104(1):29–34. |
Supplementary material
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




