Back to Journals » Clinical Interventions in Aging » Volume 10
Association between resting heart rate and N-terminal pro-brain natriuretic peptide in a community-based population study in Beijing
Authors Cao R, Bai Y, Xu R, Ye P
Received 29 April 2014
Accepted for publication 9 October 2014
Published 18 December 2014 Volume 2015:10 Pages 55—60
DOI https://doi.org/10.2147/CIA.S66971
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Ruihua Cao, Yongyi Bai, Ruyi Xu, Ping Ye
Department of Geriatric Cardiology, Chinese PLA General Hospital, Beijing, People’s Republic of China
Background: N-terminal pro-brain natriuretic peptide (NT-proBNP) is associated with an increased risk of cardiac insufficiency, which possibly leads to heart failure. However, the relationship between resting heart rate and NT-proBNP is unclear.
Objective: This study focuses on this relativity between resting heart rate and plasma NT-proBNP levels in a surveyed community-based population.
Methods: We evaluated the relativity between resting heart rate and plasma levels of NT-proBNP in 1,567 participants (mean age 61.0 years, range 21–96 years) from a community-based population in Beijing, People’s Republic of China.
Results: In patients with high resting heart rate (≥75 beats/min), NT-proBNP was higher than in those having low resting heart rate (<75 beats/min). In multiple linear stepwise regression analysis, plasma NT-proBNP was associated with resting heart rate (partial correlation coefficient, 0.82; 95% confidence interval, 0.18–1.51; P=0.011). A subsequent subgroup analysis revealed that the association between resting heart rate and plasma NT-proBNP was strengthened in subjects over 60 years old (partial correlation coefficient 1.28; 95% confidence interval, 0.49–2.36; P=0.031); while the relativity between resting heart rate and plasma NT-proBNP was not emerged in the younger subgroup (<60 years old).
Conclusions: Resting heart rate was associated with plasma NT-proBNP in the elderly, which indicated a relationship between resting heart rate and cardiac function damage.
Keywords: resting heart rate, N-terminal pro-brain natriuretic peptide, epidemiology, cardiac function, relationship
Introduction
Increased resting heart rate is associated with development of hypertension, atherosclerosis, sudden death, and coronary heart diseases, which all increase cardiovascular morbidity and mortality.1,2 In addition, increased resting heart rate is associated with oxidative stress, subclinical inflammation, sympathetic tone, and endothelial dysfunction. All of these may lead to the development of cardiac function damage.3 Whether the resting heart rate is associated with cardiac function damage to the cardiovascular system is still unclear.
B-type natriuretic peptide (BNP) is a member of a four natriuretic peptide family that shares a common 17-peptide ring structure.4 Circulating levels of the BNP system can help in the diagnosis of cardiovascular disease (CVD) and provide prognostic information not only in patients with heart failure but also the general population and other patient groups.5 Changes over time also carry prognostic information, and studies are assessing BNP-guided treatment strategies.6 Is possible to exclude the diagnosis of heart failure with the use of natriuretic peptides, but that they are not able to discriminate the two clinical and echocardiographic types of heart failure, ie, heart failure with preserved and the one with reduced ejection fraction, which must be differentiated using ultrasound.7 Values of N-terminal pro-brain natriuretic peptide (NT-proBNP) are affected by age or the presence of one or several comorbidities, such as chronic renal failure, type 2 diabetes, and acute coronary syndrome.8
Whether resting heart rate is associated with plasma levels of NT-proBNP in asymptomatic subjects has not been well established yet. The present study investigated the association between measures of resting heart rate and manifestations of cardiac function damage (NT-proBNP) in a community-dwelling population without overt CVD.
Materials and methods
Study population and design
This was a community-based cross-sectional study of people living in the Pingguoyuan area of the Shijingshan district in a metropolitan area of Beijing, People’s Republic of China. After routine health checkups between September 1, 2007 to January 31, 2009, 1,859 permanent residents were recruited for the study as described previously.9 Of these, 31 subjects with bedridden status, mental illness, arrhythmia, and severe systemic diseases were excluded from the analysis.
Resting heart rate assessment was attempted in 1,828 subjects. Adequate measurement was either not attempted or not obtained in 86 excluded participants. A total of 141 participants with overt CVD (defined as a composite of coronary heart disease [recognized or unrecognized myocardial infarction, angina pectoris, or coronary insufficiency], cerebrovascular disease [stroke or transient ischemic attack], congestive heart failure, and intermittent claudication) were excluded. Thus, testing of cardiac biomarkers was attempted in 1,680 subjects. Among these, a total of 1,567 subjects (mean age 61 years, range 21–96 years) with available NT-proBNP results were eligible for analysis. The study was approved by the ethics committee of the Chinese People’s Liberation Army (PLA) General Hospital, and each participant provided informed consent.
Clinical data collection
Information on medical history, family history of CVD, and lifestyle was obtained through self-reporting standardized questionnaires. Anthropometrics were deployed in the clinic with participants wearing light clothing and no shoes. Height was measured in centimeters by a wall-mounted measuring tape, and weight was measured in kilograms by a digital scale. Resting heart rate was measured by cardiac auscultation for 1 minute. Tobacco smoking was defined as having smoked at least one cigarette per day for 1 year or more; one cigarette was considered to be equivalent to 1 gram of tobacco.
Systolic blood pressure (SBP) and diastolic blood pressures (DBP) were measured by well-trained staff members on the right arm of the seated participant, after at least 5 minutes of rest, with a mercury sphygmomanometer and an appropriately sized cuff. Three sequential BP measurements were obtained, and the average was used for analysis.
Biomarker variable determination
All subjects underwent full laboratory evaluation (lipid profile and liver and kidney function indices). Blood samples were obtained between 8 am and 10 am from fasting participants after they had been in the supine position for 10 to 15 minutes. Samples were centrifuged immediately, and stored at −80°C until assays were performed. Concentrations of NT-proBNP were determined with an electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany) using a Roche analyzer (Roche Diagnostics, Indianapolis, IN, USA), which has a measuring range from 5 to 35,000 pg/mL. According to the manufacturer’s information, values below the detection limit are reported as 4.99 pg/mL. Concentrations of fasting glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, homocysteine, and uric acid were determined using the Roche enzymatic assays (Roche Diagnostics GmbH) on a Roche AutoAnalyzer (Roche Diagnostics). Concentrations of high-sensitivity C-reactive protein were determined by an immunoturbidimetric assay (Siemens Healthcare Diagnostics, USA) using a Dimension RxL Max analyzer (Siemens Healthcare Diagnostics). Concentrations of serum creatinine were measured by enzymatic assay (Roche Diagnostics GmbH) on a Hitachi 7600 autoanalyser (Hitachi, Tokyo, Japan).
All testing was performed by well-trained personnel blinded to clinical data in the Department of Biochemistry of Chinese PLA General Hospital.
Definition of variables
Resting heart rate measurements were conducted in a quiet environment at stable temperature. Subjects were requested to abstain from caffeine, smoking, and alcohol for at least 12 hours before assessment was performed. Participants were studied in the supine position after resting 5 to 10 minutes.
Body mass index was calculated as weight in kilograms divided by the height in square meters (kg/m2). Hypertension was defined as a mean SBP ≥140 mmHg, a mean DBP ≥90 mmHg, or use of antihypertensive medication. Diabetes mellitus was defined as a fasting glucose ≥7.0 mmol/L, nonfasting glucose ≥11.1 mmol/L, or use of antihyperglycemic medication.10 The creatinine was standardized using a calibration equation: Jaffe’s kinetic method Scr (mg/dL) =0.795 × (enzymatic method Scr [mg/dL]) +0.29.11 The estimated glomerular filtration rate (eGFR) was calculated with the Chinese-modified Modification of Diet in Renal Disease equation as follows: eGFR (mL/min/1.73m2) =175 × standardized creatinine (mg/dL)-1.234 × age (year)-0.179 × 0.79 (if female).12
Statistical analysis
Continuous variables are presented as mean ± standard deviation or median and with interquartile range. Dichotomous variables are presented as numbers and percentages. The distribution test of continuous variables was performed; NT-proBNP levels were logarithmically transformed to normalize their distributions. Resting heart rate was classified into a high level group (≥75 beats/min) or a low level group (<75 beats/min). Differences in log NT-proBNP levels between the high and low resting heart rate groups were analyzed with Student’s t-tests.
We assessed the association of resting heart rate with manifestations of cardiac function damage (NT-proBNP) by means of multiple regression analysis models. NT-proBNP was treated as the dependent variable. Forward stepwise multiple regression analysis was performed to obtain the partial correlation coefficient (PR) and 95% confidence intervals (CIs). Regression models were adjusted with age and sex as independent variables (model 1) and additionally adjusted for the factors hypertension, diabetes, SBP, DBP, current smoking, body mass index, waist circumference, resting heart rate, levels of plasma fasting glucose, total cholesterol, triglyceride, and high-density lipoprotein cholesterol, eGFR as the independent variable (model 2). Model 3 was adjusted from model 2 plus use of medications.
Because age is an important determinant of NT-proBNP levels, we repeated the regression analysis on participants younger than 60 years old (n=688) and 60 years of age and older (n=879) respectively.
All statistical analyses were performed using Stata software (version 11.0, Stata Corporation, College Station, TX). A bilateral value of P<0.05 was considered significant.
Results
Characteristics
Altogether, 1,567 participants were included in the present study. The mean ± SD age of participants in the study was 61.0±11.2 years. The characteristics of the study population are summarized in Table 1.
Distribution of NT-proBNP concentrations
Among the 1,567 participants, 1,474 (94.1%) had detectable values of NT-proBNP (≥5 pg/mL). The range of detectable NT-proBNP concentrations was 5.07–3,804 pg/mL with a median value of 42.95 pg/mL (interquarile range, 1.9–81.9 pg/mL).
Resting heart rate and the presence of NT-proBNP concentrations
The levels of NT-proBNP in the high resting heart rate group were higher than the levels in the low resting heart rate group (P=0.002) (Figure 1). The levels of NT-proBNP increased within females (Figure 2).
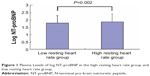  | Figure 1 Plasma Levels of log NT-proBNP in the high resting heart rate group and low resting heart rate group. |
  | Figure 2 Plasma Levels of log NT-proBNP in male and female groups. |
On univariate regression analysis, the NT-proBNP levels were significantly related to resting heart rate (P<0.01). In patients with high resting heart rates (≥75 beats/min), NT-proBNP was higher than in those having low resting heart rates (<75 beats/min). In multiple linear stepwise regression analysis, plasma NT-proBNP was associated with resting heart rate (PR, 0.82; 95% CI, 0.18–1.51; P=0.011) (Table 2).
A subsequent subgroup analysis revealed that the association between resting heart rate and plasma NT-proBNP was strengthened in subjects over 60 years old (PR, 1.28; 95% CI, 0.49–2.36; P=0.031), while the relativity between resting heart rate and plasma NT-proBNP was not emerged in the younger subgroup (<60 years old). However, in participants younger than 60 years of age, the relationship between resting heart rate (PR, -0.06; 95% CI, -0.58 to 0.60; P=0.729) and NT-proBNP levels disappeared (Table 3).
Discussion
In this study, we demonstrated for the first time that in a community-dwelling asymptomatic population, resting heart rate was positively associated with plasma NT-proBNP levels independent of age, sex, or other risk factors. These results indicated an independent association between resting heart rate and cardiac function damage. Notably, in the predefined subgroup analysis, the association between resting heart rate and cardiac function damage was strengthened in elderly participants but not present in those younger than 60 years old.
Higher resting heart rate has been reported to be associated with oxidative stress, subclinical inflammation, higher sympathetic tone, and endothelial dysfunction. And these pathologic changes are known to promote hypertension, atherosclerosis, and coronary heart diseases.1–3 In the present study, we demonstrated an association between resting heart rate and levels of NT-proBNP, which is a sensitive marker for the assessment of cardiac function damage. The findings of the present study suggest that higher resting heart rate might be partly mediated by cardiac function damage.
There are several ways that resting heart rate may predispose cardiac function damage. Firstly, an increased resting heart rate may have direct detrimental effects on cardiovascular function by increasing myocardial oxygen consumption and reducing coronary blood flow.10 Secondly, an increased resting heart rate can exert local haemodynamic forces that can adversely impact on the arterial wall.10 In previous studies,13–14 pressure or volume overload were considered the major stimuli for BNP release. Thirdly, an increased resting heart rate might be a trigger for the activation of the sympathetic nervous system.10 Fourthly, several prospective studies have reported resting heart rate be a risk predictor for certain specific causes of death, including CVD and non-CVD deaths. These studies include the Framingham Study, the NHANES I Epidemiologic Follow-up Study, the NIPPONDATA80 Study, and others.15–19 The mechanisms by which increased resting heart rate increases the risk of CVD are still largely unknown. Findings from the study of Liu et al20 suggest the resting heart rate–CVD association may be related to the positive association between resting heart rate and blood pressure. Increased blood pressure might be an important trigger for BNP release.
As in previous studies,21–23 we found that female sex was an independent positive factor for NT-proBNP levels. Because post-menopausal women are rarely treated with oral estrogens in the People’s Republic of China,24 an influence of oral estrogens on NT-proBNP levels is likely negligible.
In this study, resting heart rate was associated with cardiac function damage only in elderly participants. This difference can be attributed to a number of factors. Firstly, our study population was relatively old, with 53.1% of the participants being older than or equal to 65 years of age (range, 21–75 years; median, 60 years). Resting heart rate increases with age, the steepest rise occurs after the age of 65, resulting in strengthened cardiac function damage in older subjects. Secondly, age itself is one of the most important cardiovascular risk factors, heavily modifying the strength of the others. Thirdly, elderly subjects had a higher presence of other vascular risk factors than younger participants. These factors can interact with resting heart rate, which may increase susceptibility to cardiac function damage in this group of subjects.
The present study also has some limitations. Firstly, the present study was performed in Chinese residents from one community in Beijing; the results may not represent Chinese from other areas of the People’s Republic of China and might not be applicable to other ethnic groups. Secondly, because of the cross-sectional design and its inherent limitations, the present study cannot determine causal relationships among the factors. Therefore, our observations need confirmation in longitudinal and interventional studies. Thirdly, a significant proportion of residents were excluded because of missing or inadequate clinical and biomarker data. This is a well-known but unavoidable limitation of large epidemiological studies that may bias toward the null hypothesis because of loss of cases that presumably had more extreme values for the analyzed variables. Fourthly, the presence of sex, current smoking and potential comorbidities (such as diastolic dysfunction, left ventricular hypertrophy, hypertension, diabetes mellitus, obesity) may influence the association of resting heart rate and NT-proBNP. Although the results were adjusted for multiple covariates that might be associated with NT-proBNP levels, the possibility of residual confounding still remained.
There are several strengths to our study. Firstly, to the best of our knowledge, the present investigation is the first study evaluating the association between resting heart rate and cardiac function damage in a large community-based population. Secondly, the most sensitive detection method of cardiac function damage (NT-proBNP) and several manifestations of clinical data are included, which allows us to explore the relationship between resting heart rate and cardiac function damage.
Conclusion
In conclusion, we observed a robust, cross-sectional association between resting heart rate and NT-proBNP, which indicated a consistent positive relationship between resting heart rate and cardiac function damage, particularly in elderly subjects. However, long-term follow-up studies are needed to evaluate whether increased resting heart rate can cause manifestations such as cardiac function damage. Whether reducing the resting heart rate can have a favorable effect on cardiac function needs to be investigated further in prospective intervention studies using heart rate-lowering drugs.
Acknowledgments
This work was supported by grants from the Key National Basic Research Program of China (2012CB517503, 2013CB530804) and Nature Science Foundation of China (81270941) to P Ye and the Beijing Nova Program (Z121107002513124) to Y Bai.
Disclosure
The authors declare no conflicts of interest in this work.
References
Palatini P. Role of elevated heart rate in the development of cardiovascular disease in hypertension. Hypertension. 2011;58(5):745–750. | ||
Zhang GQ, Zhang W. Heart rate, lifespan, and mortality risk. Ageing Res Rev. 2009;8(1):52–60. | ||
Kwon HS, Lim YH, Kim HY, et al. Association of ambulatory blood pressure and heart rate with advanced white matter lesions in ischemic stroke patients. Am J Hypertens. 2014;27(2):177–183. | ||
Raizada V, Thakore K, Luo W, McGuire PG. Cardiac chamber-specific alterations of ANP and BNP expression with advancing age and with systemic hypertension. Mol Cell Biochem. 2001;216(1–2):137–140. | ||
McMurray JJ, Adamopoulos S, Anker SD, et al; ESC Committee for Practice Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33(14):1787–1847. | ||
Troughton R, Michael Felker G, Januzzi JL Jr. Natriuretic peptide-guided heart failure management. Eur Heart J. 2014;35(1):16–24. | ||
Maries L, Manitiu I. Diagnostic and prognostic values of B-type natriuretic peptides (BNP) and N-terminal fragment brain natriuretic peptides (NT-pro-BNP). Cardiovasc J Afr. 2013;24(7):286–289. | ||
deFilippi CR, Christenson RH, Gottdiener JS, Kop WJ, Seliger SL. Dynamic cardiovascular risk assessment in elderly people. The role of repeated N-terminal pro-B-type natriuretic peptide testing. J Am Coll Cardiol. 2010;55(5):441–450. | ||
Bai Y, Ye P, Luo L, et al. Arterial stiffness is associated with minimally elevated high-sensitivity cardiac, troponin T levels in a community-dwelling population. Atherosclerosis. 2011;218(2):493–498. | ||
Lang CC, Gupta S, Kalra P, et al. Elevated heart rate and cardiovascular outcomes in patients with coronary artery disease: Clinical evidence and pathophysiological mechanisms. Atherosclerosis. 2010;212(1):1–8. | ||
Zhang L, Zuo L, Xu G, et al. Community-based screening for chronic kidney disease among populations older than 40 years in Beijing. Nephrol Dial Transplant. 2007;22(4):1093–1099. | ||
Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–2944. | ||
Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50(25):2357–2368. | ||
de Lemos JA, McGuire DK, Drazner MH. B-type natriuretic peptide in cardiovascular disease. Lancet. 2003;362(9380):316–322. | ||
Okamura T, Hayakawa T, Kadowaki T, et al. Resting heart rate and cause-specific death in a 16.5-year cohort study of the Japanese general population. Am Heart J. 2004;147(6):1024–1032. | ||
Kaplan JR, Manuck SB, Clarkson TB. The influence of heart rate on coronary artery atherosclerosis. J Cardiovasc Pharmacol. 1987;10(suppl 2):S100–S102, discussion S103. | ||
Gillum RF, Makuc DM, Feldman JJ. Pulse rate, coronary heart disease, and death: the NHANES I Epidemiologic Follow-up Study. Am Heart J. 1991;121:172–177. | ||
Drukteinis JS, Roman MJ, Fabsitz RR, et al. Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart Study. Circulation. 2007;115(2):221–227. | ||
Franklin SS, Pio JR, Wong ND, et al. Predictors of new-onset diastolic and systolic hypertension: the Framingham Heart Study. Circulation. 2005;111(9):1121–1127. | ||
Liu L, Mizushima S, Ikeda K, Nara Y, Yamori Y; Cardiovascular Disease and Alimentary Comparison Study Group. Resting heart rate in relation to blood pressure: results from the World Health Organization-Cardiovascular Disease and Alimentary Comparison study. Int J Cardiol. 2010;145(1):73–74. | ||
Galasko GI, Lahiri A, Barnes SC, Collinson P, Senior R. What is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease? Eur Heart J. 2005;26(21):2269–2276. | ||
Costello-Boerrigter LC, Boerrigter G, Redfield MM, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide in the general community: determinants and detection of left ventricular dysfunction. J Am Coll Cardiol. 2006;47(2):345–353. | ||
Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40(5):976–982. | ||
Zhou JL, Lin SQ, Shen Y, Chen Y, Zhang Y, Chen FL. Serum lipid profile changes during the menopausal transition in Chinese women: a community-based cohort study. Menopause. 2010;17(5):997–1003. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



