Back to Journals » Clinical Interventions in Aging » Volume 10
Association between physiological falls risk and physical performance tests among community-dwelling older adults
Authors Singh D , Pillai SGK, Tan ST, Tai CC, Shahar S
Received 16 December 2014
Accepted for publication 12 May 2015
Published 13 August 2015 Volume 2015:10 Pages 1319—1326
DOI https://doi.org/10.2147/CIA.S79398
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Devinder KA Singh,1 Sharmila GK Pillai,1 Sin Thien Tan,1 Chu Chiau Tai,1 Suzana Shahar2
1Physiotherapy Programme, School of Rehabilitation Sciences, 2Nutrition and Dietetics Programme, School of Healthcare Sciences, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, Malaysia
Background: Physical performance and balance declines with aging and may lead to increased risk of falls. Physical performance tests may be useful for initial fall-risk screening test among community-dwelling older adults. Physiological profile assessment (PPA), a composite falls risk assessment tool is reported to have 75% accuracy to screen for physiological falls risk. PPA correlates with Timed Up and Go (TUG) test. However, the association between many other commonly used physical performance tests and PPA is not known. The aim of the present study was to examine the association between physiological falls risk measured using PPA and a battery of physical performance tests.
Methods: One hundred and forty older adults from a senior citizens club in Kuala Lumpur, Malaysia (94 females, 46 males), aged 60 years and above (65.77±4.61), participated in this cross-sectional study. Participants were screened for falls risk using PPA. A battery of physical performance tests that include ten-step test (TST), short physical performance battery (SPPB), functional reach test (FRT), static balance test (SBT), TUG, dominant hand-grip strength (DHGS), and gait speed test (GST) were also performed. Spearman’s rank correlation and binomial logistic regression were performed to examine the significantly associated independent variables (physical performance tests) with falls risk (dependent variable).
Results: Approximately 13% older adults were at high risk of falls categorized using PPA. Significant differences (P<0.05) were demonstrated for age, TST, SPPB, FRT, SBT, TUG between high and low falls risk group. A significant (P<0.01) weak correlation was found between PPA and TST (r=0.25), TUG (r=0.27), SBT (r=0.23), SPPB (r=-0.33), and FRT (r=-0.23). Binary logistic regression results demonstrated that SBT measuring postural sways objectively using a balance board was the only significant predictor of physiological falls risk (P<0.05, odds ratio of 2.12).
Conclusion: The reference values of physical performance tests in our study may be used as a guide for initial falls screening to categorize high and low physiological falls risk among community-dwelling older adults. A more comprehensive assessment of falls risk can be performed thereafter for more specific intervention of underlying impairments.
Keywords: balance, postural sways, agility, mobility, strength, gait speed
Introduction
Aging-associated issues have been under the global lens for some time now. It is estimated that approximately 13% of the 7 billion people worldwide are older adults aged 60 years and above.1 This number is expected to increase in proportion to 21% in the year 2050.1 Malaysia faces a similar phenomenon with an estimated 7% out of 28 million population consisting of older adults aged 60 years and above.2 By year 2035, this number is expected to rise to 15%, and this is likely to gain Malaysia the status of an aging nation.3
Physical and cognitive function is known to decline with age.4 This is accelerated with other related deterioration of various functions and prerequisites of body to optimum physical performance among older adults,4 which may result in an increase in falls and related issues.5,6 Falls among older adults is the major contributor to loss of independence, hospitalization from trauma, injury-related deaths and fractures,7 decrease in quality of life,8 and associated health care cost.9
One method for effective management of health care resources is preventive care that includes early detection and management of falls in older adults.10 Early screening among older adults is recommended for preventive fall strategies.11,12 In line with this, screening should be simple, fast, and inexpensive to perform. Some of these physical performance tests may meet those criteria.
Numerous simple and composite physical performance tests have been used for screening risk of falls among older adults. Examples of simple assessment tools include gait speed,13 limits of stability, and 30-second chair stand that focuses primarily on mobility, balance, or strength function.14 Meanwhile, composite tests measure physiological impairments (sensation, vision, strength, postural sway, and reaction time) and a battery of physical performance tasks (sit-to-stand (STS), static standing balance, and gait speed) such as physiological profile assessment (PPA)6 and short physical performance battery (SPPB),15 respectively. An association between simple and more complex physical performance tests provides the concurrent validity of simple physical performance tests.
Previous studies among community-dwelling older adults have found a correlation between some of the simple and composite falls assessment tools such as gait speed, STS, near tandem standing tests, and subcomponents of physiological factors among community-dwelling older adults.16–18 Similarly, significant correlation between physiological falls risk assessed using PPA, Timed Up and Go (TUG) test,19 and self-reported physical functional measures20 has also been demonstrated. We recently reported a correlation between some physical performance measures and physiological falls risk measured using PPA among older adults with undernutrition.21 However, there is no such information among community-dwelling older adults.
The aim of the present study was to examine the association between physiological falls risk measured using PPA, agility, dynamic and static balance, physical performance battery, grip strength, gait speed, and TUG tests. This further assisted in identifying the most robust physical performance test to measure physiological falls risk and to determine its predictive and discriminative ability among community-older adults.
Method
Participants
This cross-sectional study involved 140 community-dwelling older adults (46 men and 94 women) aged 60–82 years (mean: 65.77 years, SD: 4.61), who were ambulating independently with or without assistive device. Participants were recruited through flyers and posters at a senior citizens club in Kuala Lumpur, Malaysia. Participants who were unable to comprehend and follow instructions with a mini-mental state examination score <23; having known acute illnesses, current or recent fractures, ear infection, or vestibular disorders; taking drugs that could affect muscle strength and balance; unable to hold shoulder at 90° flexion; unstable chronic diseases such as unstable diabetes mellitus and uncompensated heart failure; medical conditions such as malignancy and musculoskeletal disorders; and neurological problems such as Parkinson and stroke were excluded from the study. Ethical approval was obtained from the Secretariat for Research and Ethics of Universiti Kebangsaan, Kuala Lumur, Malaysia.
Participants’ falls risks were measured using PPA and physical performance tests as listed in the following subsections. These tests were performed by trained final year physiotherapy undergraduates. To avoid inter-rater reliability issues, each test was performed by the same rater all the time. A 10-minute rest or more when required was provided between each test.
Measurements
Physiological profile assessment
Falls risk is measured using the short version PPA that included contrast sensitivity, proprioception, muscle strength, simple hand reaction time, and postural sway tests.6 Intraclass coefficient (ICC) for these tests was found to range from 0.50 to 0.97.6 PPA has 75% accuracy to screen falls risk in both community-dwelling and institutionalized older adults.6 Composite falls risk score of PPA was calculated using a web-based program (FallScreen©).
Short physical performance battery
SPPB is a composite outcome measure of lower limbs function including strength, endurance, gait, and balance.15 SPPB measures three components, namely, walking speed, chair stands, and standing balance, and have excellent ICC =0.88–0.92.22 Previous studies show that SPPB is able to predict disability, institutionalization, falls, and mortality among older adults.15,23–25 A score ranging from 0 to 4 (0= inability to complete the task; 4= highest level of function) was scored for each task of SPPB with the sum of these three tests (0–12) reflecting the complete measurement of physical function.15
Ten-step test
TST is a modified agility test for older adults.26 The test–retest reliability of TST was reported to have an ICC of 0.86 (P<0.01). TST was performed by instructing participants to step up and down a block with the height of 10 cm using alternate feet. The time to complete ten repetitions was recorded. A familiarization trial was provided before performing the test twice. The quickest time was taken as the measurement in units of 0.1 second using a stopwatch.
Static balance test
Static balance test (SBT) was measured using an intelligent balance board (Probalance; Lab Rehab Pte Ltd., Singapore).27 Reliability of this balance board is reported to be within 0.92–0.93.28 The balance board detects anteroposterior and mediolateral sways in degrees and an overall function score was calculated using the balance board computer software interface. Participants were assessed by instructing them to stand on the balance board with eyes open and both hands at the sides of body for 30 seconds. This test was repeated three times, and the mean value of the scores was taken as the overall function scores.
Functional reach test
Dynamic balance was assessed using functional reach test (FRT) that mainly focused on anterior and posterior stability.29 FRT has excellent reliability (ICC =0.89–0.92) and is able to predict falls risk among older adults.29,30 Healthy individuals with adequate balance function are expected to reach 25 cm or more.30 Participants were instructed to stand close against a wall with a measurement tape fixed on the wall and to keep their shoulder in 90° flexion parallel to the measurement tape. Participants were required to reach forward maximally with arm outstretched equal to shoulder’s height without moving their feet or touching the wall. Participant’s way of reaching was not restricted and the distance (in cm) of reach was represented by differences between the starting and ending position of knuckle of third metacarpal. Three experimental trials were performed with the average taken as the result, and two practice trials were done before experimental trials.
Dominant hand-grip strength
Dominant hand-grip strength (DHGS) was measured using a handheld dynamometer (Jamar® Lafayette Instrument Company, Lafayette, IN, USA). DHGS has been reported to have a good-to-excellent reliability in older adults (ICC =0.60–0.90).31 DHGS was performed by instructing the participants to sit comfortably with the dominant arm at side of the body and at right angles with the elbow and hand held in mid-supination/pronation position. Participants were then instructed to squeeze the handle of the dynamometer and maintain for 5 seconds. Three trials were performed with adequate rest in between trials. The best reading of three trials was taken as the DHGS in unit of kilogram (kg).
Gait speed test
Gait speed test (GST) is a measure of mobility and has been reported to be able to predict falls risk among older adults.32 GST has a high test–retest reliability with ICCs ≥0.90 among older adults.33 GST was assessed by having participants to walk a 10 m pathway at self-paced speed. No assistance was allowed but any walking aids used by participants were permitted. Time was recorded after participants had walked past the first 2 m and stopped at 8 m to allow acceleration and deceleration during walking. Assessors walked with the participants for safety purposes and three trials were performed. Gait speed was calculated by dividing the total distance (6 m) to the time taken in seconds. The average speed of the three trials was taken as the gait speed in meters per second.
Timed Up and Go test
The TUG test is a measure of functional mobility among older adults.34 TUG test has been reported to have high reliability (ICC =0.98) in older adults.35 Participants were instructed to sit on a chair (height of 46 cm and with arm rest height of 65 cm) that was placed against the wall. Participants were instructed to stand, walk at their normal pace on a 3 m pathway, turn at the end point mark, walk back on the determined pathway, and resit on the chair. Participants were allowed to use their walking aid but were not provided with any assistance. Time in seconds (s) were recorded when the buttock of the participants touched the chair on completion. Participants were allowed a trial session for familiarization, and three experimental sessions were performed with an adequate rest between each tests. The mean of the three scores was taken as the TUG test score.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences software version 20 (IBM Corporation, Armonk, NY, USA). Spearman’s rank correlation was performed as only FRT data were found to be normally distributed. A statistical significance level of P<0.05 was set. The Mahalanobis distance values for all the variables were below 11. A binomial logistic regression was performed while controlling for age and sex to examine the significantly correlated independent variables (physical performance tests) with falls risk (dependent variable).
Results
Physiological falls risks
The physiological falls risk based on PPA categorization is as depicted in Figure 1. Falls risk was reorganized based on only high and low risk of falls. High and low risk of falls were defined as older adults who scored above and below the score of 2, respectively, based on a previous study.19 Only 12.86% of the total participants were categorized to have high risk of falls, whereras 87.14% participants were of low risk of falls.
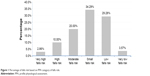  | Figure 1 Percentage of falls risk based on PPA category of falls risk. |
The demographic characteristics of the participants are as shown in Table 1. Approximately 50% of the participants in the high risk of falls had history of falls. Significant differences (P<0.05) were demonstrated for age, TST, SPPB, FRT, SBT, and TUG test between high and low falls risk group.
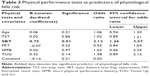
Table 2 shows the correlation coefficients between physiological falls risk and physical performance tests. A significant weak correlation was found between physiological falls risk and all physical performance tests except for DHGS and GST. Physical performance tests as predictors for physiological falls risk are as depicted in Table 3. Binary logistic regression was used as the data did not meet the assumptions for a multivariate regression. Significant correlations of physiological falls risk that comprised of TST, SBT, SPPB, and TUG were included in the regression model to predict the tests that were able to predict physiological falls risk. Age was also added to this model as age significantly correlated with physiological falls risk. SBT was demonstrated to be a significant (P<0.05) predictor of physiological falls risk.
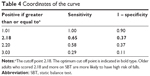
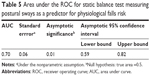
Further test for discriminative ability of SBT measured using a balance board to discriminate between high and low physiological falls risk showed that area under the receiver operating curve (ROC; area under curve) was 0.70 (P=0.01) with confidence interval of 0.59–0.82. Based on the receiver operating curve, coordinates of the curve of 2.18 (sensitivity of 0.65 and specificity of 0.37) were identified as the cutoff value to identify high risk fallers among community-dwelling older adults (Table 4). These results indicate that for every 2.12° increase in sway detected using the balance board, there is one-unit increase in falls risk. The results showed that approximately 65% older adults will be correctly identified as high risk fallers when using SBT. The total area under curve of the test was significant (P<0.05) (Table 5), indicating that SBT measured using a balance board was a good discriminative test to identify high risk fallers among community-dwelling older adults.
Discussion
The aim of the study was to establish the association between various physical performance tests such as agility (TST), physical performance (SPPB), dynamic balance (FRT), static balance (SBT), functional mobility (TUG), gait speed (GST), dominant hand-grip strength (DHGS), and falls risk (PPA). The results of this study showed that SBT measured objectively using a balance board was the most robust physical performance measure for physiological falls risk.
Age was a covariate identified in this study with a positive significant correlation with physiological falls risk in community-dwelling older adults. Further tests showed that it was not a predictor of falls risk. The relationship of age and sex with falls risk among older adults is inconsistent so far. Age and sex are significant risk factors for falls risk36 but was not reported to affect falls incidence.37 In contrast, age was demonstrated to predict falls among older adults in some findings.20,38 Age-related changes such as decreased muscle strength and postural stability explain the correlation of age and falls risk. Age, however, does not predict falls and possibly could be attributed to interactions of other related factors such as participants’ age range. For example, effect of sex on falls risk was determined by location of the fall.39,40 Indoor and outdoor falls were related to older females and younger males, respectively.39,40
Agility and balance has been argued to be difficult to differentiate.41 Agility is the ability to move quickly without losing balance. This supports our findings regarding a significant correlation between agility, measured using TST with physical functional measures related to dynamic balance such as FRT, gait speed, and TUG. In our previous study, agility was demonstrated to be related to cognitive function.42 Agility significantly improved with balance exercises43 in older adults. Agility may not have appeared as a predictor for physiological falls risk in this study, probably because balance and age have accounted for this effect. A correlation between agility and age has also been reported.44
Static balance measuring postural sways objectively using a balance board was found to be the only predictor of physiological falls risk in the present study. Similar results were previously found.45 It is believed that older adults use hip rather than ankle strategy in maintaining balance due to age-related impairments. An association between increased muscle co-contractions in the ankles and falls was reported in a previous study during static balance.46 In agreement, postural sways have also been found to be predictors of falls risk.47 One of the components measured in physiological falls risk is postural sway and this may also possibly explain the reason for its association with falls risk in the present study.
In this study, SPPB as a battery of test was significantly correlated with physiological falls. STS test as one of the test in SPPB was noted to be correlated with all the subtests in PPA that measures physiological falls risk.48 The results showed that STS function was significantly correlated (P<0.01) with knee extensor strength (r=-0.43), contrast sensitivity (r=-0.22), proprioception (r=0.15), simple hand reaction time (r=0.25), and postural sway (r=0.26).17 Similarly, a correlation was also reported between STS and all other sensorimotor measures.48 Unlike in our study, physical performance measured using upper body strength and flexibility, lower body strength, balance, and endurance was reported to be a strong predictor of falls risk.20 This inconsistent finding may be due to the fact that all the subtests in SPPB focus more on lower limb functions compared to overall body strength, balance, and endurance.
Total score of physiological falls had a significant negative correlation with dynamic balance, measured using FRT in our study. In a previous study, maximum balance range and coordinated stability tests to measure dynamic balance were significantly correlated with subscores of physiological falls comprising contrast sensitivity, simple hand reaction time, proprioception, and knee extensor strength.48 However, FRT did not appear to be a predictor for physiological falls in the present study. It is noteworthy that dynamic balance measured using FRT was also not correlated with SBT. This could be attributed to the fact that FRT although a dynamic balance test is limited to a single direction of reaching forward. In higher functioning older adults, FRT may not provide enough challenge in postural control system.
TUG test had a significant correlation but did not appear as a predictor of physiological falls risk among community-dwelling older adults. This finding is consistent with a recent report about TUG test having limited ability in predicting falls risk.49 However, TUG test has been known to be a sensitive measure for falls risk in older adults with impairments.35 A nonlinear relationship between functional mobility and falls risk has also been highlighted in a previous study.50
Further studies may be required to determine the discriminative and predictive validity of TUG test in community-dwelling older adults. Probably, the cutoff values of TUG in relation to falls risk in community-dwelling older adults may be much lower compared to the 13.5 seconds recommended among adults with impairments.35 Even older adults categorized to have a higher risk of falls in the present study scored 40% lower scores compared to these scores. It can be considered that cutoff values of TUG test established in many case control studies may be biased49 and not applicable to community-dwelling older adults.
Falls risk is dependent on multiple intrinsic and extrinsic factors. In our study, falls risk was limited to physiological factors measured using PPA and among community-dwelling older adults. Participants with diseases were excluded and details of other conditions such as insomnia and types of medication were not obtained. Therefore, the results may not be generalized to frail and institutionalized older adults.
Conclusion
The conclusion, the weak correlation results between PPA and the physical performance tests such as TST, SPPB, FRT, TUG, and SBT suggest that physical performance tests may not be useful as a stand-alone test to screen for falls risk among community-dwelling older adults. The results of our study also showed that postural sways measured objectively can predict physiological falls risk, with an increase of every 2.12° resulting in a one-unit increase in falls risk. Although unsatisfactory, with 65% sensitivity and 35% specificity, measuring postural sways objectively, eg, using a balance board is simple and fast. This method may be of use for initial falls risk screening in community-dwelling older adults and clinical settings. Further studies with a larger number of participants and prospective falls incidence followed up for a year may be beneficial in establishing precise cutoff values and predictive validity of falls risk using objective measurements of postural sways.
Moreover, the reference values of physical performance tests in our study may be used as a guide for initial falls screening in categorizing high and low physiological falls risk among community-dwelling older adults. A more comprehensive assessment of falls risk can be performed thereafter for more specific intervention of underlying impairments.
Acknowledgments
Funding for this research was provided by grants from Universiti Kebangsaan Malaysia (KOMUNITI-2012-003, UKM-AP-2011-27, LRGS/BU/2012/UKM-UKM/K/O1). The authors would like to thank all the participants for their participation, and Manal Badrasawi for her assistance in sorting the data from Kuala Lumpur Aging Study.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper.
Disclosure
The authors report no conflicts of interest in this work.
References
United Nation, Department of economic and social affairs, Population division. World Population Prospects. The 2010 Revision Volume 2. Demographic Profiles. New York: United Nation, Department of economic and social affairs, Population division; 2011. | ||
Department of Statistics Malaysia. Demographic Indicators. Available from https://www.statistics.gov.my/. Accesed September 14, 2014. | ||
Ganesan S. Managing the Country’s Ageing Population. 2010. Available from: http://thestar.com.my/lifestyle/story.asp?file=/2010/10/25/lifefocus/6865382&sec=lifefocus. Accessed June 14, 2012. | ||
Nitz JC, Hourigan SR. Physiotherapy Practice in Residential Aged Care. China. Oxford: Butterworth-Heinemann; 2004. | ||
Onder G, Penninx BW, Lapuerta P, et al. Change in physical performance over time in older women: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 2002;57(5):289–293. | ||
Lord SR, Menz HB, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther. 2003;83(3):238–252. | ||
Kannus P. Preventing osteoporosis, falls, and fractures among elderly people. Br Med J. 1999;318(7178):205–206. | ||
Thiem U, Klaaβen-Mielke R, Trampisch U, Moschny A, Pientka L, Hinrichs T. Falls and EQ-5D rated quality of life in community-dwelling seniors with concurrent chronic diseases: a cross-sectional study. Health Qual Life Outcomes. 2014;12(2):1–7. | ||
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(suppl 6):s37–s41. | ||
Nicholas JA, Hall WJ. Screening and preventive services for older adults. Mt Sinai J Med. 2011;78(4):498–508. | ||
Gillespie LD, Robertson MC, Gillespie WH, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. | ||
Moyer VA. Prevention of falls in community-dwelling older adults: U.S. preventive services task force recommendation statement. Ann Intern Med. 2012;157(3):197–204. | ||
Quach L, Galica AM, Jones RN, et al. The nonlinear relationship between gait speed and falls: the Elderly of Boston Study. J Am Geriatr Soc. 2011;59(6):1069–1073. | ||
Rogers ME, Rogers NL, Takeshima N, Islam MM. Methods to assess and improve the physical parameters associated with fall risk in older adults. Prev Med. 2003;36(3):255–264. | ||
Guralnik JM, Seeman TE, Tinetti ME, Nevitt MC, Berkman LF. Validation and use offunction measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano). 1994;6(6):410–419. | ||
Tiedemann A, Sherrington C, Lord SR. Physiological and psychological predictors of walking speed in older community-dwelling people. Gerontology. 2005;51(6):390–395. | ||
Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-standfunction depends on sensation, speed, balance and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci. 2002;57(8):539–543. | ||
Lord SR, Rogers MW, Howland A, Fitzpatrick R. Lateral stability, sensorimotor function and falls in older people. J Am Geriatr Soc. 1999;47(9):1077–1081. | ||
Whitney JC, Lord SR, Close JCT. Streamlining assessment and intervention in a falls clinic using the Timed Up and Go Test and physiological profile assessments. Age Ageing. 2005;34(6):567–571. | ||
Smee DJ, Anson JM, Waddington GS, Berry HL. Association between physical functionality and falls risk in community-living older adults. Curr Gerontol Geriatr Res. 2012;2012:864516. | ||
Singh DK, Manaf ZA, Yusoff NA, Muhammad NA, Phan MF, Shahar S. Correlation between nutritional status and comprehensive physical performance measures among older adults with undernourishments in residential institutions. Clin Interv Aging. 2014;9:1415–1423. | ||
Ostir GV, Volpato S, Fried LP. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the Women’s Health and Aging Study. J Clin Epidemiol. 2002;55(9):916–921. | ||
Penninx BW, Ferrucci L, Leveille SG, Rantanen T, Pahor M, Guralnik JM. Lower extremity performabce in nondisabled older persons as a predictor of subsequent hospitalization. J Gerontol A Biol Sci Med Sci. 2000;55(11):691–697. | ||
Quadri P, Tettamanti M, Bernasconi S, Trento F, Loew F. Lower limb function as predictor of falls and loss of mobility with social repercussions one year after discharge among elderly inpatients. Aging Clin Exp Res. 2005;17(2):82–89. | ||
Perera S, Mody S, Woodman R, Studenski S. Meaningful change and responsiveness in common physical performance measures in older adults. J Gerontol A Biol Sci Med Sci. 2005;54(5):743–749. | ||
Miyamoto K, Takebayashi H, Takimoto K, Miyamoto S, Morioka S, Yagi F. A new simplefunction test focused on agility in elderly people: the Ten Step Test. Gerontology. 2008;54(6):365–372. | ||
Ang WT, Tan UX, Tan HG, et al. Design and development of a novel balancer with variable difficulty for training and evaluation. Disabil Rehabil Assist Technol. 2008;3(6):325–331. | ||
Koh K, Wee L. Reliability and validity of pro.balance. Presented at: 7th National Congress, Singapore Physiotherapy Association; May 16–17, 2009; Singapore. | ||
Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):192–197. | ||
Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol. 1992;47(3):93–98. | ||
RehabMeasures.org. [Homepage on the internet]. Chicago. Hand Held Dynamometer/Grip Strength [updated March 9, 2014]. Available from: http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=1052. Accessed September 14, 2014. | ||
Fritz S, Lusardi M. White paper, walking speed, the sixth vital sign. J Geriatr Phys Ther. 2009;32(2):2–5. | ||
Steffen TM, Hacker TA. Research report age- and gender-related testfunction in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–137. | ||
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. | ||
Shumway-cook A, Brauer S. Research report predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80:896–903. | ||
Lin C, Liao K, Pu S, Chen Y, Liu M. Associated factors for falls among the community-dwelling older people assessed by annual geriatric health examinations. PLoS One. 2011;6(4):2–6. | ||
Vicacaro LJ, Perera S, Studenski S. Is timed up and go better than gait speed in predicting health, function and falls in older adults. J Am Geriatr Soc. 2012;59(5):887–892. | ||
Bhatt T, Espy D, Yang F, Pai YC. Dynamic gait stability, clinical correlates, and prognosis of falls among community-dwelling older adults. Arch Phys Med Rehabil. 2011;92(5):799–805. | ||
Kelsey JL, Berry SD, Procter-Gray E, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. J Am Geriatr Soc. 2010;58(11):2135–2141. | ||
Duckham RL, Procter-gray E, Hannan MT, Leveille SG, Lipsitz LA. Sex differences in circumstances and consequences of outdoor and indoor falls in older adults in the MOBILIZE Boston cohort study. BMC Geriatr. 2013;13(133):1–11. | ||
Davis JC, Donaldson MG, Ashe MC, Khan KM. The role of balance and agility training in fall reduction. Eura Medicophys. 2004;40(3):211–221. | ||
Won H, Singh DK, Din NC, et al. Relationship between physical performance and cognitive function measures among community-dwelling older adults. Clin Epidemiol. 2014;3(6):343–350. | ||
Singh DK, Rajaratnam BS, Palaniswamy V, Raman VP, Bong PS, Pearson H. Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric. 2013;16(1):141–146. | ||
Teimoori A, Raisi MS, Abodarda Z, Ghorbanlo ZH, Ghojebeigloo AA. Effects of aging on muscle velocity, balance, and agility in healthy Iranian females. Ann Biol Res. 2012;3(5):2096–2099. | ||
Tucker MG, Kavanagh JJ, Morrison S, Barrett RS. Differences in rapid initiation and termination of voluntary postural sway associated with ageing and falls-risk. J Mot Behav. 2010;42(5):277–287. | ||
Nelson-Wong E, Appell R, McKay M. Increased fall risk is associated with elevated co-contraction about the ankle during static balance challenges in older adults. Eur J Appl Physiol. 2012;112(4):1379–1389. | ||
Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55(11):1088–1094. | ||
Menz HB, Morris ME, Lord SR. Foot and ankle characteristics associated with impaired balance and functional ability in older people. J Gerontol A Biol Sci Med Sci. 2005;60(12):1546–1552. | ||
Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;14(1):1–14. | ||
Barker AL, Nitz JC, Choy NLL, Haines TP. Mobility has a non-linear association with falls risk among people in residential aged care: an observational study. J Physiother. 2012;58:117–125. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.