Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Association between obesity and the brain-derived neurotrophic factor gene polymorphism Val66Met in individuals with bipolar disorder in Mexican population
Authors Morales Marín ME, Genis A , Tovilla-Zarate CA , Lanzagorta N, Escamilla M, Nicolini H
Received 20 January 2016
Accepted for publication 15 March 2016
Published 25 July 2016 Volume 2016:12 Pages 1843—1848
DOI https://doi.org/10.2147/NDT.S104654
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Mirna Edith Morales-Marín,1 Alma Delia Genis-Mendoza,1,2 Carlos Alfonso Tovilla-Zarate,3 Nuria Lanzagorta,4 Michael Escamilla,5 Humberto Nicolini1,4
1Genomics of Psychiatric and Neurodegenerative Diseases Laboratory, National Institute of Genomic Medicine (INMEGEN), CDMX, Mexico; 2Psychiatric Care Services, Child Psychiatric Hospital Dr Juan N Navarro, CDMX, Mexico; 3Genomics Research Center, Juarez Autonomous University of Tabasco, Comalcalco, Mexico; 4Carracci Medical Group, CDMX, Mexico; 5Department of Psychiatry, Paul L Foster School of Medicine, Texas Tech University Health Science Center, El Paso TX, USA
Background: The brain-derived neurotrophic factor (BDNF) has been considered as an important candidate gene in bipolar disorder (BD); this association has been derived from several genetic and genome-wide studies. A polymorphic variant of the BDNF (Val66Met) confers some differences in the clinical presentation of affective disorders. In this study, we evaluated a sample population from Mexico City to determine whether the BDNF (rs6265) Val66Met polymorphism is associated with the body mass index (BMI) of patients with BD.
Methods: This association study included a sample population of 357 individuals recruited in Mexico City. A total of 139 participants were diagnosed with BD and 137 were classified as psychiatrically healthy controls (all individuals were interviewed and evaluated by the Diagnostic Interview for Genetic Studies). Genomic DNA was extracted from peripheral blood leukocytes. The quantitative polymerase chain reaction (qPCR) assay was performed in 96-well plates using the TaqMan Universal Thermal Cycling Protocol. After the PCR end point was reached, fluorescence intensity was measured in a 7,500 real-time PCR system and evaluated using the SDS v2.1 software, results were analyzed with Finetti and SPSS software. Concerning BMI stratification, random groups were defined as follows: normal <25 kg/m2, overweight (Ow) =25.1–29.9 kg/m2, and obesity (Ob) >30 kg/m2.
Results: In the present work, we report the association of a particular BMI phenotype with the presence of the Val66Met allele in patients with BD (P=0.0033 and odds ratio [95% confidence interval] =0.332 [157–0.703]), and correlated the risk for valine allele carriers with Ow and Ob in patients with BD.
Conclusion: We found that the methionine allele confers a lower risk of developing Ow and Ob in patients with BD. We also confirmed that the G polymorphism represents a risk of developing Ow and Ob in patients with BD. In future studies, the haplotype analysis should provide additional evidence that BDNF may be associated with BD and BMI within the Mexican population.
Keywords: brain-derived neurotrophic factor, bipolar disorder, single nucleotide polymorphism, body mass index
Background
Bipolar disorder (BD) is a mental disease affecting behavior, commonly characterized by manic-depressive episodes. The personal and social impact is frequently very high for the afflicted person, even individuals under treatment can suffer relapse and become disabled. BD can also have other consequences, such as an economic impact or increased risk of suicide, which can vary from 25% to 50%.1 This disease has a high heritability, its strong genetic component ranks in 80%–85%, which results in familial aggregation.2 The existent risk in first-degree relatives is of ~9%, nearly ten times higher than in the general population.3
An elevated number of candidate genes have been studied regarding this disease; one of such is the brain-derived neurotrophic factor (BDNF) gene.4,5 BDNF is a neurotrophin involved in diverse functions of the brain, for example, neuronal development, maturation, differentiation, migration, survival, signaling during neurodevelopment, synaptic plasticity, and dendrite growth.6
The BDFN gene is located in 11p13–14; this region has been linked to BD in previous studies.7,8 The BDNF gene has nine exons with independent promoters and with few alternative splicing forms. Messenger RNAs are translated into a protein called pro-BDNF and later posttranslationally modified to produce a mature BDNF protein. Several single nucleotide polymorphisms (SNPs) have been identified within the gene; in this study, we evaluated the rs6265 G/A (Val66Met) polymorphism found in pro-BDNF. This SNP apparently affects messenger RNA and protein traffic and it has been associated with psychiatric diseases9 (Figure 1).
  | Figure 1 BDNF gene structure. |
The relevance of BDNF as a candidate gene involved in BD has been shown in past reports, although their results have been found controversial because of sample ethnicity and affliction level.10–12 Patients carrying the methionine (Met) allele had overall smaller hippocampus volume than healthy control patients.13 On the other hand, the Met/Met genotype was significantly associated with severe depressive episodes in patients with BD.14 This gene has been previously linked with BD, specifically when presenting the Val66Met polymorphism.7,8 In a UK population, this SNP was also associated with susceptibility to the rapid-cycling subset of BD.15 In cognitive performance, Val66Met was also associated with BD, thus demonstrating its involvement in cognitive executive function deficit.16
Some environmental factors have a direct influence on the body mass index (BMI) of an open population, such as an inadequate diet, sedentary way of life and stress, and adding the genetic component. Moreover, in patients with BD, disease itself, and prescription of antipsychotics and/or mood stabilizers have been proved as important predisposition factors for overweight (Ow) and obesity (Ob) development as well as metabolic syndrome, whose risk is elevated almost twice compared with general population.17–19 Disease complexity is increased as a consequence, and the patients, now under a complicated course, show a poor response to treatment which makes it more difficult to overcome BD.19
In animal models, BDNF gene has been strongly associated with weight regulation; its expression takes place in the hypothalamic nuclei, which is related to eating behavior, food intake, and body weight.17,20 In human studies, BDNF has been associated with BMI. As an example, healthy persons carrying the BDNF Met/Met genotype could have lower BMI than people with other polymorphisms.21 However, Caucasian Met allele carriers were more obese than people lacking this allele.22 Regardless, another study did not reveal any association between BDNF and BMI;23 therefore, no conclusive outcome was attained.
Furthermore, the prescription of antipsychotics could increase the development risk of metabolic syndrome in patients afflicted with eating disorders and mental illness.24,25 The association between Ob and psychiatric disorders has been observed earlier,26 and some clinical cases have been reported about gene abnormalities in BDNF and Ob. To date, the association between BDNF and BMI in the Mexican population afflicted with BD has not yet been determined. Therefore, we propose the hypothesis that the BDNF (rs6265) Val66Met polymorphism may be associated with BMI in patients with BD. To test this hypothesis, we stratified a Mexican population sample exhibiting BD and evaluated the association between BDNF and BMI.
Materials and methods
Characteristics of the samples
We performed an association study using blood samples collected from mestizo individuals residing in Mexico City, 139 were diagnosed with BD (49 with BD type 1 with psychosis, 90 with BD type 1 without psychosis) (n=84 females and 55 males). Inclusion criteria can be reviewed elsewhere.27 One hundred and thirty-seven psychiatrically healthy individuals were used as controls (n=75 females and 62 males) (best estimated; all individuals were directly interviewed by the Diagnostic Interview for Genetic Studies and Diagnostic and Statistical Manual of Mental Disorders IV criteria). All of the participants gave a written informed consent. The present study used existing data from the Genetics of Bipolar Disorder in Latino Populations studies, a multicenter study designed to investigate the genetic determinants of BD.27 All of the participating subjects in this study provided written informed consent. The project and the consent were reviewed and approved by the Institutional Review Board at the Ethics Committee at Carracci Medical Group and at the INMEGEN, in accordance with the principles of the Helsinki Declaration of 1975 and in compliance with the Code of Ethics of the World Medical Association.
Obesity measure
The patients were classified in either Ow or Ob categories based on their BMI, which was calculated as follows: weight (kg)/height (m)2, this method has been previously used in a Mexican population. The cutoff values were of 25–29.9 kg/m2 for Ow and 30 kg/m2 or more for Ob. The value assigned for a normal (N) BMI status was <25 kg/m2.28
Genotyping
The genomic DNA from both patients and healthy controls was extracted from peripheral white blood cells by conventional methods. The nucleic acids obtained were quantified by spectrophotometry using a NanoDrop (Thermo Fisher Scientific, Waltham, MA, USA), working dilutions were at a concentration of 10 ng/μL. Genotyping was performed using the TaqMan 5′ exonuclease method (Thermo Fisher Scientific), characterization of the BDNF gene SNP rs6265 was performed following the manufacturer’s instructions. The quantitative polymerase chain reaction was done in a 7,500 AB real-time system with SDS v2.1 software (Thermo Fisher Scientific). Afterward, the allelic discrimination was determined to genotype each sample. For quality control, duplicate samples were genotyped randomly.
Statistical analysis
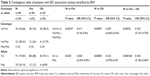
Sociodemographic characteristics were evaluated as follows: the initial comparison between male and female subjects was analyzed with a chi-square test for categorical variables and a t-test for independent samples for continuous variables (Table 1).
  | Table 1 Sociodemographic and clinical characteristics of Mexican patients with BD |
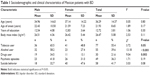
In the analysis of the patient subgroups (normal weight, Ow, and Ob), an analysis of variance followed by Bonferroni’s correction was performed. The significance cutoff value was set at P<0.05 and to address multiple comparisons, the significance level for Bonferroni’s test was established at P=0.016 (0.05/3) (Table 2).
  | Table 2 Patients with BD distributed according to sex and body mass index |
The association analysis between allelic and genotypic frequencies was obtained using the programs Finetti (http://ihg.gsf.de/cgi-bin/hw/hwa1.pl) and SPSS v2.1 software (SPSS, Chicago, IL, USA); we used a chi-square test, which retrieved the odds ratio (OR), with a 95% confidence interval and P-values (P<0.05), which were statistically significant. The analysis included multivariate logistic regression, with sex and age as covariates.
Results
Patients diagnosed with BD were grouped according to sociodemographic characteristics such as sex, age and age of onset, years of education, substance abuse, psychotic episodes, BMI, and other characteristics shown in Table 1. We observed some peculiar characteristics in patients with BD when separated by sex; for instance, tobacco abuse was higher in females than in males (P=0.05). In the case of alcohol and substance abuse, males presented a higher index than females (P<0.001 and P=0.003, respectively) (Table 1).
We also observed a positive correlation between BMI and age regardless of sex (P<0.001) (Table 2). Post hoc analysis showed that patients with normal weight were found within a lower age range than those presenting Ow (P<0.05) or Ob (P<0.05).
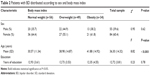
There was no direct association between BD and BDNF rs6265 (P=0.81). Although, when comparing the patients with BD stratified by BMI, adding the Met allele carrier groups, we found a statistically significant association between BD and BDNF rs6265 (Table 3).
A higher frequency of the Met/Met genotype, or a single Met allele, was present in patients with BD with normal weight when compared with individuals with Ob and Ow. Interestingly, all the cases of Met/Met genotype were found in individuals with normal weight only (Table 3).
Discussion
BDNF is an important neurotrophin involved in neurodevelopment and neuron maintenance; therefore, it has been studied at length. This protein has been correlated with diverse mental illnesses such as depression, anxiety, schizophrenia, and BD.29–31 Moreover, this gene and its protein product has also been related to eating disorders, Ob, and metabolic syndrome. Within this the gene, a number of different SNPs have been described and analyzed in association studies, one of them analyzing the nucleotide change G/A producing a Val to Met amino acid change in position 66; this change has been studied in numerous mental diseases.32
In the present study, when analyzing the BDNF SNP rs6265, we found an existent association between patients with BD and their BMI. We show that the SNP Met allele genotype confers lower risk of developing Ow and Ob. So far, this is the first report showing this effect in the analysis of BMI and BDNF Val66Met in Mexican patients with BD.
There is evidence suggesting that the prescription of antipsychotics elevates the risk of metabolic syndrome, but we found this to be true only if associated with the Met allele in male schizophrenics.24 Chronic schizophrenia in patients prescribed with different antipsychotics is correlated with weight gain and the Met allele.33 The existing controversy concerning the effect of BDNF in mental diseases is still in discussion among the scientific community, mainly because of differences in the genetic structure of the studied populations. This aspect must be considered in future association studies.32
It must be highlighted that we also found an existing association between the G polymorphism and the risk of developing Ow and Ob in the studied patients with BD (P=0.00164, OR =2.828 [1.455–5.498]), in contrast with other reports performed in different populations, such as by Zhang et al,33 where an A polymorphism resulted in an increased impact to BMI during treatment with antipsychotics; this could probably be due to the studied population’s ethnicity.32
This polymorphism has been studied in some psychiatric illnesses in Mexican populations, such as in people of Mexican-American descendant living in Los Angeles, USA, whose GG genotype was associated with a higher risk of developing major depression symptoms.31 On the other hand, the Val/Val genotype was associated with an increased risk of developing an obsessive–compulsive disorder29 and with suicidal tendencies in BD.34 Concerning Ob, a higher G polymorphism incidence has been associated with this disease in a healthy Boston population from Puerto Rican descent.35 Also, an association between a GG genotype and higher BMI and weight was found in males from the same population.35,36
Similar to our results, but in healthy adults, Gunstad et al21 reported an association between low BMI and BDNF Met/Met when compared against Val/Met and Val/Val genotypes. However, no association has been observed in patients with schizophrenia or depression.37–40
In future studies, some aspects need to be taken into account. The BDNF gene presents other reported polymorphisms, which need to be studied within the Mexican population for the construction of haplotypes, thus increasing the power of the study. Also, it is necessary to conduct a study in an increased sample size to correlate the genotype depending on the drug prescribed (before and after treatment), and to evaluate the quantity of serum BDNF, which would improve our understanding of BD pathogenesis in a Mexican sample population.
Conclusion
We found a significant correlation between an increased BMI and the presence of the Val66Met allele in a BD Mexican sample population. On the other hand, we also found that the Met allele confers a lower risk of developing Ow and Ob in Mexican patients with BD. We also confirm that the G polymorphism represents a significant risk of developing Ow and Ob in Mexican patients with BD.
Disclosure
The authors report no conflicts of interest in this work.
References
Latalova K, Kamaradova D, Prasko J. Suicide in bipolar disorder: a review. Psychiatr Danub. 2014;26:108–114. | ||
Barnett JH, Smoller JW. The genetics of bipolar disorder. Neuroscience. 2009;164:331–343. | ||
Smoller JW, Finn CT. Family, twin, and adoption studies of bipolar disorder. Am J Med Genet C Semin Med Genet. 2003;123C:48–58. | ||
Wu R, Fan J, Zhao J, Calabrese JR, Gao K. The relationship between neurotrophins and bipolar disorder. Expert Rev Neurother. 2014;14:51–65. | ||
Szczepankiewicz A. Evidence for single nucleotide polymorphisms and their association with bipolar disorder. Neuropsychiatr Dis Treat. 2013;9:1573–1582. | ||
Binder DK, Scharfman HE. Brain-derived neurotrophic factor. Growth Factors. 2004;22:123–131. | ||
Sklar P, Gabriel SB, McInnis MG, et al. Family-based association study of 76 candidate genes in bipolar disorder: BDNF is a potential risk locus. Brain-derived neutrophic factor. Mol Psychiatry. 2002;7:579–593. | ||
Neves-Pereira M, Mundo E, Muglia P, King N, Macciardi F, Kennedy JL. The brain-derived neurotrophic factor gene confers susceptibility to bipolar disorder: evidence from a family-based association study. Am J Hum Genet. 2002;71:651–655. | ||
Pruunsild P, Kazantseva A, Aid T, Palm K, Timmusk T. Dissecting the human BDNF locus: bidirectional transcription, complex splicing, and multiple promoters. Genomics. 2007;90:397–406. | ||
Wang Z, Li Z, Gao K, Fang Y. Association between brain-derived neurotrophic factor genetic polymorphism Val66Met and susceptibility to bipolar disorder: a meta-analysis. BMC Psychiatry. 2014;14:366. | ||
Le-Niculescu H, Patel SD, Bhat M. Convergent functional genomics of genome-wide association data for bipolar disorder: comprehensive identification of candidate genes, pathways and mechanisms. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:155–181. | ||
Maletic V, Raison C. Integrated neurobiology of bipolar disorder. Front Psychiatry. 2014;5:98. | ||
Chepenik LG, Fredericks C, Papademetris X. Effects of the brain-derived neurotrophic growth factor Val66Met variation on hippocampus morphology in bipolar disorder. Neuropsychopharmacology. 2009;34: 944–951. | ||
Hosang, GM, Uher R, Keers R. Stressful life events and the brain-derived neurotrophic factor gene in bipolar disorder. J Affect Disord. 2009;125:345–349. | ||
Green EK, Raybould R, Macgregor S, et al. Genetic variation of brain-derived neurotrophic factor (BDNF) in bipolar disorder: case-control study of over 3000 individuals from the UK. Br J Psychiatry. 2006;188:21–25. | ||
Rybakowski JK, Borkowska A, Skibinska M. Prefrontal cognition in schizophrenia and bipolar illness in relation to Val66Met polymorphism of the brain-derived neurotrophic factor gene. Psychiatry Clin Neurosci. 2006;60:70–76. | ||
Unger TJ, Calderon GA, Bradley LC, Sena-Esteves M, Rios M. Selective deletion of Bdnf in the ventromedial and dorsomedial hypothalamus of adult mice results in hyperphagic behavior and obesity. J Neurosci. 2007;27:14265–14274. | ||
Maina G, Salvi V, Vitalucci A, D’Ambrosio V, Bogetto F. Prevalence and correlates of overweight in drug-naive patients with bipolar disorder. J Affect Disord. 2008;110:149–155. | ||
McIntyre RS, et al. Bipolar disorder and metabolic syndrome: an international perspective. J Affect Disord. 2010;126:366–387. | ||
Kernie SG, Liebl DJ, Parada LF. BDNF regulates eating behavior and locomotor activity in mice. EMBO J. 2000;19:1290–1300. | ||
Gunstad J, Schofield P, Paul RH, et al. BDNF Val66Met polymorphism is associated with body mass index in healthy adults. Neuropsychobiology. 2006;53:153–156. | ||
Skledar M, Nikolac M, Dodig-Curkovic K, Curkovic M, Borovecki F, Pivac N. Association between brain-derived neurotrophic factor Val66Met and obesity in children and adolescents. Prog Neuropsychopharmacol Biol Psychiatry. 2012;36:136–140. | ||
Nikolac M, Sagud M, Nedic G. The lack of association between catechol-O-Methyl-transferase Val108/158Met polymorphism and smoking in schizophrenia and alcohol dependence. Psychiatry Res. 2013;205:179–180. | ||
Zhang Y, Chen M, Wu Z. Association study of Val66Met polymorphism in brain-derived neurotrophic factor gene with clozapine-induced metabolic syndrome: preliminary results. PLoS One. 2013;8:e72652. | ||
Gamero-Villarroel C, Gordillo I, Carrillo JA. BDNF genetic variability modulates psychopathological symptoms in patients with eating disorders. Eur Child Adolesc Psychiatry. 2013;23(8):669–679. | ||
Tsai SJ. Is mania caused by overactivity of central brain-derived neurotrophic factor? Med Hypotheses. 2004;62:19–22. | ||
Gonzalez S, Xu C, Ramirez M, et al. Suggestive evidence for association between L-type voltage-gated calcium channel (CACNA1C) gene haplotypes and bipolar disorder in Latinos: a family-based association study. Bipolar Disord. 2013;15:206–214. | ||
Martinez-Hernandez A, Córdova EJ, Rosillo-Salazar O. et al. Association of HMOX1 and NQO1 polymorphisms with metabolic syndrome components. PLoS One. 2015;10:e0123313. | ||
Marquez L, Camarena B, Hernández S, Lóyzaga C, Vargas L, Nicolini H. Association study between BDNF gene variants and Mexican patients with obsessive-compulsive disorder. Eur Neuropsychopharmacol. 2013;23:1600–1605. | ||
Autry AE, Monteggia LM. Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev. 2012;64:238–258. | ||
Ribeiro L, Busnello JV, Cantor RM, et al. The brain-derived neurotrophic factor rs6265 (Val66Met) polymorphism and depression in Mexican-Americans. Neuroreport. 2007;18:1291–1293. | ||
Petryshen TL, Sabeti PC, Aldinger KA, et al. Population genetic study of the brain-derived neurotrophic factor (BDNF) gene. Mol Psychiatry. 2009;15:810–815. | ||
Zhang XY, Zhou DF, Wu GY, et al. BDNF levels and genotype are associated with antipsychotic-induced weight gain in patients with chronic schizophrenia. Neuropsychopharmacology. 2008;33:2200–2205. | ||
Gonzalez-Castro TB, Nicolini H, Lanzagorta N, et al. The role of brain-derived neurotrophic factor (BDNF) Val66Met genetic polymorphism in bipolar disorder: a case-control study, comorbidities, and meta-analysis of 16,786 subjects. Bipolar Disord. 17:27–38. | ||
Leon-Mimila P, Villamil-Ramírez H, Villalobos-Comparán M. Contribution of common genetic variants to obesity and obesity-related traits in Mexican children and adults. PLoS One. 2013;8:e70640. | ||
Ma XY, Qiu WQ, Smith CE, et al. Association between BDNF rs6265 and obesity in the Boston Puerto Rican Health Study. J Obes. 2012;2012:102942. | ||
Chen SL, Lee SY, Chang YH, et al. The BDNF Val66Met polymorphism and plasma brain-derived neurotrophic factor levels in Han Chinese patients with bipolar disorder and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:99–104. | ||
Vinberg M, Bukh JD, Bennike B, Kessing LV. Are variations in whole blood BDNF level associated with the BDNF Val66Met polymorphism in patients with first episode depression? Psychiatry Res. 2013;210:102–108. | ||
Terracciano A, Piras MG, Lobina M, et al. Genetics of serum BDNF: meta-analysis of the Val66Met and genome-wide association study. World J Biol Psychiatry. 2011;14:583–589. | ||
Tramontina J, Frey BN, Andreazza AC, Zandona M, Santin A, Kapczinski F. Val66Met polymorphism and serum brain-derived neurotrophic factor levels in bipolar disorder. Mol Psychiatry. 2007;12:230–231. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.