Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Association between hemoglobin and prognosis in patients admitted to hospital for COPD
Authors Toft-Petersen AP, Torp-Pedersen C, Weinreich UM , Rasmussen BS
Received 2 July 2016
Accepted for publication 17 August 2016
Published 10 November 2016 Volume 2016:11(1) Pages 2813—2820
DOI https://doi.org/10.2147/COPD.S116269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Anne Pernille Toft-Petersen,1,2 Christian Torp-Pedersen,1,3 Ulla Møller Weinreich,1,4 Bodil Steen Rasmussen1,2
1Department of Clinical Medicine, Aalborg University, 2Department of Anaesthesia and Intensive Care, 3Department of Clinical Epidemiology, 4Department of Respiratory Diseases, Aalborg University Hospital, Aalborg, Denmark
Abstract: Low concentrations of hemoglobin have previously been demonstrated in many patients with COPD. There is evidence of anemia as a prognostic factor in acute exacerbations, but the detailed relationship between concentrations of hemoglobin and mortality is not known. A register-based cohort of patients admitted for the first time to Danish hospitals for acute exacerbations of COPD from 2007 through 2012 was established. Age, sex, comorbidities, medication, renal function, and concentrations of hemoglobin were retrieved. Sex-specific survival analyses were fitted for different rounded concentrations of hemoglobin. The cohort encompassed 6,969 patients. Hemoglobin below 130 g/L was present in 39% of males and below 120 g/L in 24% of females. The in-hospital mortality rates for patients with hemoglobin below or above these limits were 11.6% and 5.4%, respectively. After discharge, compared to hemoglobin 130 g/L, the hazard ratio (HR) for males with hemoglobin 120 g/L was 1.45 (95% confidence interval [CI] 1.22–1.73), adjusted HR 1.37 (95% CI 1.15–1.64). Compared to hemoglobin 120 g/L, the HR for females with hemoglobin 110 g/L was 1.4 (95% CI 1.17–1.68), adjusted HR 1.28 (95% CI 1.06–1.53). In conclusion, low concentrations of hemoglobin are frequent in COPD patients with acute exacerbations, and predict long-term mortality.
Keywords: pulmonary disease, chronic obstructive, anemia, mortality, polycythemia, epidemiology
Introduction
COPD is a persistent, progressive airflow limitation associated with enhanced chronic inflammatory response in the airways.1 It is among the leading causes of mortality and morbidity worldwide, and is predicted to be the third-leading cause of death by 2020.1
Our understanding of COPD has evolved rapidly, and it has become clear that COPD is not an isolated disease of the lungs. Instead, COPD is a complex interplay between emphysema and airway obstruction, systemic inflammation, comorbidities, and metabolism, which all contribute to prognosis.2–8 Recently developed prognostic tools take this multifaceted pathology into account by incorporating systemic as well as lung-specific parameters.9,10
Hemoglobin has been suggested as an easily and inexpensively measured prognostic indicator. Both low and high values are encountered in COPD, though the distribution varies highly with the population studied. Historically, especially before the introduction of domiciliary oxygen, secondary polycythemia was a striking feature in COPD, but today the prevalence seems to be low.11 Instead, anemia might be more common, with a reported prevalence of 6.2%–46.3%.12,13
Hemoglobin can potentially capture a range of prognostic factors, as homeostasis can be impaired by nutrient deficiency, comorbid disease, and medication, and is modified by tissue oxygen supply and systemic inflammation. Importantly, anemia might reflect iron deficiency, which has been linked to the development of pulmonary arterial hypertension14 and presence of chronic inflammation, which is associated with frailty.15 Concentrations of hemoglobin and hematocrit have been shown to provide prognostic information in different populations of COPD patients,16–25 but in many of these studies patients with diseases associated with chronic anemia were excluded.12 While this strategy provides estimates of the prevalence and prognostic importance of hemoglobin directly ascribable to COPD, it does not reflect the importance of hemoglobin in a real-life COPD population, where most patients have numerous chronic diseases.5 Cardiovascular diseases, diabetes mellitus, and chronic renal failure frequently coexist with COPD, and are associated independently of COPD with anemia, which aggravates prognosis.5,26,27
The aims of the present study were firstly to outline the pattern of hemoglobin concentrations in a large representative population of patients hospitalized for acute exacerbation in COPD (AECOPD), and secondly to investigate the association between hemoglobin concentrations at admission and mortality.
Materials and methods
All in-patient hospitalizations from 1997 through 2012 were identified in the Danish National Patient Registry. Successive hospitalizations were merged if the discharge date of the first and the admission date of the second were identical. AECOPD hospitalizations were defined as hospitalizations with either a primary diagnosis of COPD (International Classification of Diseases [ICD]-10: DJ44) or with a complex of either acute respiratory failure (ICD-10: DJ96) or pneumonia (ICD-10: DJ13–DJ18) as the primary diagnosis and COPD as a secondary, as described by Thomsen et al.28 Hospitalizations where the patients were less than 30 years old were not considered AECOPD admissions, as they most likely represented misclassified asthma. Patients with first AECOPD hospitalizations in 2007 and onward were included in the cohort, provided they had no AECOPD hospitalizations in 1997 through 2006 and only the first hospitalization of a given patient was considered. Patients admitted with an AECOPD hospitalization in 1997–2006 were excluded to minimize the risk of including a repeated admission as a first admission.
In the National Register of Medicinal Product Statistics, selected prescriptions redeemed by patients in the year preceding first AECOPD hospitalizations were identified and used for quantification of competing risk factors for anemia. A patient was considered a user of either antidiabetics (Anatomical Therapeutic Chemical [ATC] codes A10A and A10B) or angiotensin converting enzyme (ACE) inhibitors/angiotensin II receptor blocker (AT2R) inhibitors (ATC code C09), respectively, if at least one prescription had been redeemed. Redeemed prescriptions for medication for obstructive airway diseases (ATC code R03) were retrieved for sensitivity analysis. Entries of malignant diseases (ICD-10: DC), heart failure (ICD-10: DI50), and acute myocardial infarction (AMI; ICD-10: DI20–DI25) within 5 years prior to first hospitalizations were retrieved from the Danish National Patient Registry and used as proxies for presence of these diseases.
Laboratory test results were obtained for patients admitted to hospitals participating in our collaboration. This collaboration consists of hospitals situated in different parts of Denmark, and admitted about 17% of all first COPD admissions in Denmark. First hemoglobin and lowest creatinine concentrations measured in venous blood during the hospitalization were sampled. The final cohort consisted of patients who had had hemoglobin measured. According to the World Health Organization (WHO), concentrations of hemoglobin below 130 g/L for males and 120 g/L for females are considered diagnostic of anemia regardless of age,29 and this definition was applied here. Polycythemia was defined as concentrations of hemoglobin above 170 g/L for males and above 150 g/L for females.22 For survival models, concentrations of hemoglobin were rounded to the nearest 10 g/L. Estimated glomerular filtration rate (eGFR), which is glomerular filtration normalized to the body surface area, was calculated from concentrations of creatinine by the Modification of Diet in Renal Disease formula,30 assuming that all patients were Caucasian. Quartiles of eGFR based on the distribution in the entire cohort were established and used as a proxy for renal function.
Information on time of death was obtained from the Danish Civil Registration System. Each patient was followed until time of death or until December 31, 2013, whichever came first. Cox regression models were built for the unadjusted and adjusted relation between mortality and concentrations of hemoglobin in males and females. Covariates in the adjusted model included age, use of antidiabetics, use of ACE or AT2R inhibitors, use of antithrombotics, quartile of eGFR, and diagnoses of cancer, heart failure, or AMI. We did not adjust for any previously documented hemoglobin values.
Sensitivity analyses were performed in three subsets of patients. One subset was restricted to patients who had redeemed medication for obstructive airway diseases within the year preceding the hospitalization for AECOPD, and another was restricted to patients who had used neither diabetics, ACE/AT2R inhibitors, nor antithrombotics, who had eGFR in the upper three quartiles and who had no registrations of cancer, heart failure, or AMI. The last sensitivity analysis was performed with a definition of AECOPD hospitalizations that included admissions only where the primary diagnosis was DJ44.
Cox proportional hazard models were used for prediction of death beyond discharge. P-values below 0.05 were considered significant. Statistical analyses were performed in SAS 9.4 (SAS Institute Inc, Cary, NC, USA) and R version 3.2.2. In Denmark, retrospective use of register data does not require ethical approval or patient consent. The Danish Data Agency gave permission to use the data (GEH-2014–018, I-Suite 02736).
Results
At least one measurement of hemoglobin was accessible from 6,969 first AECOPD hospitalizations from 2007 through 2012, corresponding to 98.3% of all AECOPD hospitalizations in our collaboration. Patients without hemoglobin measurements had shorter length of stay (median 1 [0–4] vs 5 [2–9] days, P<0.00001) and reduced risk of death after discharge (P=0.02), but did not differ with regard to in-hospital mortality (5% vs 7.3%, P=0.42). Hemoglobin had been measured on the day of admission in 93.5% of patients and within 2 days in 98.3%. Prescriptions for medication for COPD had been redeemed within the year preceding admission by 70.8% of patients with accessible measurements of hemoglobin.
Median length of hospital stay was 8 (interquartile range [IQR] 3–16) days for patients who died in hospital and 5 (IQR 2–9) days for patients who were discharged alive. Median follow-up time for patients discharged alive was 1,048 (range 1–2,556) days. With anemia, normal hemoglobin, and polycythemia, respectively, in-hospital mortality was 11.6%, 5.2%, and 7% (P<0.0001). Postdischarge mortality at 30 days was 7.8%, 3%, and 1.8% (P<0.0001) and at 1 year 31.4%, 15.6%, and 15.3% (P<0.0001).
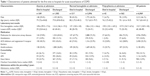
Demographics, laboratory test results, medication, and presence of selected comorbidities are reported in Table 1. The overall prevalence of anemia in the population was 30.9%. Concentrations of hemoglobin for males and females are depicted in Figure 1. Anemia was found in 39.1% and 23.8% of admitted males and females, respectively, and in 37.5% and 22.7% of males and females discharged alive. Polycythemia was found in 2.6% of the admitted males and in 13.8% of the admitted females. Calculations of anemia prevalence upon standardization to definitions applied and sex ratios prevalent in populations found in the literature can be found in Table 2.
  | Figure 1 Distribution of concentrations of hemoglobin (Hb), measured after admission for all first-time admitted patients. |
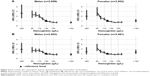
Figure 2 shows univariate analyses of associations between concentrations of hemoglobin rounded to the nearest 10 g/L and risk of death after discharge for males and females, respectively. Decreasing concentrations were associated with increasing risk, and even mild anemia was associated with increased risk. For males, compared to hemoglobin 130 g/L, the hazard ratio (HR) with hemoglobin 120 g/L was 1.45 (95% confidence interval [CI] 1.22–1.73), whereas for females, compared to hemoglobin 120 g/L, the HR with hemoglobin 110 g/L was 1.4 (95% CI 1.17–1.68). Unadjusted HRs for males with anemia and polycythemia relative to normal hemoglobin concentrations were 2 (95% CI 1.8–2.21) and 0.97 (95% CI 0.69–1.35), respectively. The corresponding HRs for females were 1.83 (95% CI 1.64–2.04) and 1.01 (95% CI 0.87–1.16). Adjustment for age, use of antidiabetics, use of ACE or AT2R inhibitors, use of antithrombotics, quartile of eGFR, and presence of cancer, heart failure, or AMI did not significantly change this. For males, compared to hemoglobin 130 g/L, the adjusted HR with hemoglobin 120 g/L was 1.37 (95% CI 1.15–1.64), whereas for females, compared to hemoglobin 120 g/L, the adjusted HR with hemoglobin 110 g/L was 1.28 (95% CI 1.06–1.53). Adjusted HRs for males with anemia and polycythemia relative to normal hemoglobin concentrations were 1.51 (95% CI 1.36–1.68) and 1.07 (95% CI 0.77–1.5), respectively. The corresponding HRs for females were 1.45 (95% CI 1.3–1.62) and 1.17 (95% CI 1.01–1.36). An age-adjusted subgroup analysis of patients who used neither antidiabetics, ACE/AT2R inhibitors, nor antithrombotics, who had eGFR in the upper three quartiles, and who had no registrations of cancer, heart failure, or AMI gave consistent results, though for females significance was lost. In this subgroup analysis, for males, compared to hemoglobin 130 g/L, the HR with hemoglobin 120 g/L was 1.55 (95% CI 1.05–2.28), and for females, compared to hemoglobin 120 g/L, the HR with hemoglobin 110 g/L was 1.08 (95% CI 0.69–1.7).
The same associations were seen when only patients who had redeemed prescriptions for COPD medication in the previous year were included. For males, compared to concentrations of hemoglobin 130 g/L, the unadjusted HR with hemoglobin 120 g/L was 1.49 (95% CI 1.21–1.84). For females, compared with hemoglobin 120 g/L, the unadjusted HR with hemoglobin 110 g/L was 1.51 (95% CI 1.22–1.87). Adjustment for age, medication, and comorbidity gave corresponding HRs of 1.37 (95% CI 1.11–1.69) for males and 1.42 (95% CI 1.14–1.77) for females, respectively.
There were 5,132 first AECOPD admissions with DJ44 (COPD) as the primary diagnosis, and 4,862 of the patients survived to discharge. For males, compared to concentrations of hemoglobin 130 g/L, the unadjusted HR with hemoglobin 120 g/L was 1.37 (95% CI 1.12–1.69). For females, compared with hemoglobin 120 g/L, the unadjusted HR with hemoglobin 110 g/L was 1.4 (95% CI 1.13–1.72). Adjustment for age, medication, and comorbidity gave corresponding HRs of 1.21 (95% CI 0.98–1.49) for males and 1.33 (95% CI 1.07–1.64) for females, respectively.
Survival curves for patients discharged alive with anemia, normal hemoglobin levels, and polycythemia are presented in Figure 3. These show that when stratified for anemia, males and females had the same expected survival following hospitalization for AECOPD.
  | Figure 3 Survival curves for patients discharged alive, by sex and level of hemoglobin. |
Discussion
The present study demonstrates a high prevalence of anemia among patients on their primary admission for AECOPD. Very low concentrations of hemoglobin but also concentrations close to the WHO lower normal value are associated with significantly increased mortality.
The prevalence of anemia in this study exceeds the prevalence found by Martinez-Rivera et al.19 A possible explanation is the exclusion from that study of patients with certain comorbidities or severe acute disease, both of which are associated with low hemoglobin. In contrast, a higher prevalence than ours was found in Silverberg et al.31 Possible explanations are a different case mix where, for example, diabetes was twice as frequent as in our population and the exclusion from our study of patients admitted previously for AECOPD. In a study of patients treated with noninvasive ventilation for AECOPD, Mydin et al18 found higher prevalence of anemia than in our population. Probably, the inclusion of only patients in need of noninvasive ventilation shifted the case mix with regard to severity of illness compared to our population, which might explain the in-hospital mortality rate of 33% compared to only 7% in our study. Previous studies have shown a low frequency of anemia in invasively ventilated patients.32 It might be that very old patients are not selected for invasive ventilation and that this accounts for the low frequency of anemia, as hemoglobin is negatively related to age.33
This study demonstrates that low concentrations of hemoglobin are associated with increasing mortality after discharge in patients admitted for AECOPD. Though this association is known in stable-phase COPD patients,34 to our knowledge only one small study has examined the association between anemia and long-term mortality in patients admitted to hospital with AECOPD.19 The association found with hemoglobin <130 g/L in that population was very strong, with an odds ratio for death within a year after admission of 5.9. The inclusion of patients in this study differed from ours in several ways. An unknown number of admitted patients were not included, due to comorbidities or immediate need of assisted ventilation, which limits generalizability. Of included patients, 57% were GOLD (Global Initiative for Chronic Obstructive Lung Disease) stage IV and 46% received long-term oxygen therapy, suggestive of a case mix with more advanced disease than usually seen among admitted COPD patients.35 It might be that anemia attributable to comorbidities is less strongly associated with severity of COPD and mortality.
In our population, even concentrations of hemoglobin around the lower end of the normal range were predictive of mortality in COPD. This finding is consistent with a German study of stage III/IV COPD patients, where the association was strongest with cutoff levels of 151 g/L for males and 143 g/L for females.21 However, the CIs around these cutoff levels were wide and overlapped with CIs based on the WHO cutoff levels. The relationship between hemoglobin and mortality was nonlinear, as also found in our study. About 40% of potential participants were not included in the German study, due to comorbidities or treatment of anemia, which limits comparison with our patients. It might be argued that as COPD patients have high burdens of comorbidity,36 exclusion of study participants, while limiting confounding, produces estimates with limited generalizability.
The strengths of our study are the large number of patients and the high reliability of the Danish medical registers, with high positive predictive values for a number of diagnoses.37 The COPD diagnosis applied here has a positive predictive value of 92%.28 In addition, the inherent ability to track unique patient courses virtually eliminates all but emigration as loss to follow-up.38 We minimized bias from probably low recording of anemia as a diagnosis by assessing laboratory test results directly and bias from the association between anemia and readmission by including only patients hospitalized for AECOPD for the first time.
Limitations
There are, however, notable limitations to our study. Firstly, our study was observational, which prevents inference of causality. Secondly, the generalizability of our data is limited by a skewness in the accessibility of laboratory test results. We only have access to laboratory test results from a limited number of hospitals and clinics. Although we have excluded patients admitted to outpatient clinics or part-time units, there is still a disproportionately low number of accessible laboratory test results from hospitalizations with rapid discharge relative to the number from prolonged hospitalizations. Thirdly, we chose to sample the first concentrations of hemoglobin measured during the hospitalizations to minimize the impact of fluid administration on the concentrations, but the trade-off is spuriously high concentrations of hemoglobin in patients with severe dehydration on admission. Arguably, our results might thus not represent an association between steady-state hemoglobin concentration and mortality. Fourthly, we made no attempts to characterize anemia further when present. Fifthly, as discussed, comorbidities might be a confounder of the association between concentrations of hemoglobin and mortality. We have adjusted for surrogate markers of selected diseases, but the negative predictive values of at least some comorbidities are low in the Danish registers,39 which are designed mainly for administrative purposes. Therefore, this adjustment is probably insufficient, with a notable risk of residual confounding. Finally, we did not adjust for severity of COPD, and severity might confound the association between hemoglobin and mortality.
Conclusion
Anemia is a common feature in patients admitted to hospital for AECOPD, and the lower the concentration of hemoglobin at admission, the higher the risk of death after discharge. Even mild anemia was associated with significantly increased risk.
Author contributions
APTP had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. CTP, UMW, and BSR contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Bethesda (MD): GOLD; 2015. | ||
Roberts CM, Lowe D, Bucknall CE, Ryland I, Kelly Y, Pearson MG. Clinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2002; 57(2):137–141. | ||
Chung LP, Winship P, Phung S, Lake F, Waterer G. Five-year outcome in COPD patients after their first episode of acute exacerbation treated with non-invasive ventilation. Respirology. 2010;15(7):1084–1091. | ||
Schols AM, Broekhuizen R, Weling-Scheepers CA, Wouters EF. Body composition and mortality in chronic obstructive pulmonary disease. Am J Clin Nutr. 2005;82(1):53–59. | ||
Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. | ||
Berry CE, Wise RA. Mortality in COPD: causes, risk factors, and prevention. COPD. 2010;7(5):375–382. | ||
Connors AF, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. Am J Respir Crit Care Med. 1996;154(4 Pt 1):959–967. | ||
Han MK, Agusti A, Calverley PM, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182(5):598–604. | ||
Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. | ||
Almagro P, Soriano JB, Cabrera FJ, et al. Short- and medium-term prognosis in patients hospitalized for COPD exacerbation: the CODEX index. Chest. 2014;145(5):972–980. | ||
Kent BD, Mitchell PD, McNicholas WT. Hypoxemia in patients with COPD: cause, effects, and disease progression. Int J Chron Obstruct Pulmon Dis. 2011;6:199–208. | ||
Hoepers AT, Menezes MM, Fröde TS. Systematic review of anaemia and inflammatory markers in chronic obstructive pulmonary disease. Clin Exp Pharmacol Physiol. 2015;42(3):231–239. | ||
Similowski T. The potential impact of anaemia of chronic disease in COPD. Eur Respir J. 2006;27(2):390–396. | ||
Plesner LL, Schoos MM, Dalsgaard M, et al. Iron deficiency in COPD associates with increased pulmonary artery pressure estimated by echocardiography. Heart Lung Circ. Epub 2016 May 25. | ||
Röhrig G. Anemia in the frail, elderly patient. Clin Interv Aging. 2016; 11:319–326. | ||
Boutou AK, Karrar S, Hopkinson NS, Polkey MI. Anemia and survival in chronic obstructive pulmonary disease: a dichotomous rather than a continuous predictor. Respiration. 2013;85(2):126–131. | ||
Martinez FJ, Foster G, Curtis JL, et al. Predictors of mortality in patients with emphysema and severe airflow obstruction. Am J Respir Crit Care Med. 2006;173(12):1326–1334. | ||
Mydin HH, Murphy S, Clague H, Sridharan K, Taylor IK. Anemia and performance status as prognostic markers in acute hypercapnic respiratory failure due to chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2013;8:151–157. | ||
Martinez-Rivera C, Portillo K, Muñoz-Ferrer A, et al. Anemia is a mortality predictor in hospitalized patients for COPD exacerbation. COPD. 2012;9(3):243–250. | ||
Lima DF, Coleta KD, Tanni SE, Silveira LV, Godoy I, Godoy I. Potentially modifiable predictors of mortality in patients treated with long-term oxygen therapy. Respir Med. 2011;105(3):470–476. | ||
Kollert F, Tippelt A, Müller C, et al. Hemoglobin levels above anemia thresholds are maximally predictive for long-term survival in COPD with chronic respiratory failure. Respir Care. 2012;58(7):1204–1212. | ||
Cote C, Zilberberg MD, Mody SH, Dordelly LJ, Celli B. Haemoglobin level and its clinical impact in a cohort of patients with COPD. Eur Respir J. 2007;29(5):923–929. | ||
Coleta KD, Silveira LV, Lima DF, Rampinelli EA, Godoy I, Godoy I. Predictors of first-year survival in patients with advanced COPD treated using long-term oxygen therapy. Respir Med. 2008;102(4):512–518. | ||
Schneckenpointner R, Jörres RA, Meidenbauer N, Kollert F, Pfeifer M, Budweiser S. The clinical significance of anaemia and disturbed iron homeostasis in chronic respiratory failure. Int J Clin Pract. 2014; 68(1):130–138. | ||
Seyhan EC, Özgül MA, Tutar N, Ömür I, Uysal A, Altin S. Red blood cell distribution and survival in patients with chronic obstructive pulmonary disease. COPD. 2013;10(4):416–424. | ||
García-Olmos L, Alberquilla A, Ayala V, et al. Comorbidity in patients with chronic obstructive pulmonary disease in family practice: a cross sectional study. BMC Fam Pract. 2013;14:11. | ||
Nissenson AR, Goodnough LT, Dubois RW. Anemia: not just an innocent bystander? Arch Intern Med. 2003;163(12):1400–1404. | ||
Thomsen RW, Lange P, Hellquist B, et al. Validity and underrecording of diagnosis of COPD in the Danish National Patient Registry. Respir Med. 2011;105(7):1063–1068. | ||
World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Geneva: WHO; 2011. | ||
National Institute of Diabetes and Digestive and Kidney Diseases. Estimating glomerular filtration rate (GFR). 2015. Available from: https://www.niddk.nih.gov/health-information/health-communication-programs/nkdep/lab-evaluation/gfr/estimating/Pages/estimating.aspx. Accessed October 11, 2016. | ||
Silverberg DS, Mor R, Weu MT, Schwartz D, Schwartz IF, Chernin G. Anemia and iron deficiency in COPD patients: prevalence and the effects of correction of the anemia with erythropoiesis stimulating agents and intravenous iron. BMC Pulm Med. 2014;14:24. | ||
Rasmussen L, Christensen S, Lenler-Petersen P, Johnsen SP. Anemia and 90-day mortality in COPD patients requiring invasive mechanical ventilation. Clin Epidemiol. 2011;3:1–5. | ||
Nilsson-Ehle H, Jagenburg R, Landahl S, Svanborg A. Blood haemoglobin declines in the elderly: implications for reference intervals from age 70 to 88. Eur J Haematol. 2000;65(5):297–305. | ||
Chambellan A, Chailleux E, Similowski T. Prognostic value of the hematocrit in patients with severe COPD receiving long-term oxygen therapy. Chest. 2005;128(3):1201–1208. | ||
Roberts CM, Lopez-Campos JL, Hartl S. The European COPD Audit: brothers in arms. Breathe. 2012;8(4):267–270. | ||
Dal Negro RW, Bonadiman L, Turco P. Prevalence of different comorbidities in COPD patients by gender and GOLD stage. Multidiscip Respir Med. 2015;10(1):24. | ||
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83. | ||
Schmidt M, Pedersen L, Sørensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29(8): 541–549. | ||
Kümler T, Gislason GH, Kirk V, et al. Accuracy of a heart failure diagnosis in administrative registers. Eur J Heart Fail. 2008;10(7): 658–660. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.