Back to Journals » Clinical Interventions in Aging » Volume 16
Association Between Charlson Comorbidity Index and Community-Acquired Pressure Injury in Older Acute Inpatients in a Chinese Tertiary Hospital
Authors Zhang Z , Yang H , Luo M
Received 14 September 2021
Accepted for publication 19 November 2021
Published 1 December 2021 Volume 2021:16 Pages 1987—1995
DOI https://doi.org/10.2147/CIA.S338967
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Zhili Zhang,1,* Hongli Yang,2,* Man Luo3
1Department of Surgical, Wuhan Third Hospital Affiliated to Wuhan University, Wuhan, 430070, People’s Republic of China; 2Department of Public Health, The First Community Health Service Center of Guanshan, Wuhan, 430073, People’s Republic of China; 3Department of Nursing, Wuhan Third Hospital Affiliated to Wuhan University, Wuhan, 430070, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Man Luo
Department of Nursing, Wuhan Third Hospital Affiliated to Wuhan University, Wuhan, 430070, People’s Republic of China
Tel +86 18207139227
Fax +86 27-88850381
Email [email protected]
Purpose: To explore the correlation between community-acquired pressure injury (CAPI) and comorbidities in elderly patients with emergency admission.
Patients and Methods: Patients aged 65 years or above were enrolled from multiple departments, such as Internal Medicine, Surgery, Geriatrics, and Intensive Care Unit of Wuhan Third Hospital, which is affiliated to Wuhan University, from January to December 2020. Comorbidity data were extracted using the 10th edition of the International Classification of Diseases (ICD-10) from the hospital electronic medical record system, and the Charlson Comorbidity Index (CCI) was calculated using these data. Participants were divided into two groups according to whether pressure injury was present at admission. The baseline characteristics of the two groups were compared using Student’s t-tests, Mann–Whitney U-tests, and chi-square tests. Univariate and multivariate logistic regression models were constructed to explore the relationship between CAPI and the CCI. Smooth curve fitting was used to show the relationship between the CCI and CAPI. By drawing the receiver operating characteristic curve, the CCI was used to predict CAPI.
Results: A total of 5759 participants with an average age of 75.1 ± 7.6 were included in this population-based study. The prevalence of CAPI was 4.3%. In logistic regression analysis, there was a positive relationship between the CCI and CAPI after adjustment for sex, age, hypoproteinemia, and anemia (OR = 1.37, 95% CI = 1.29– 1.45, p < 0.001, trend test p < 0.001). The area under the receiver operating characteristic curve was 0.75, and the maximum value of the Youden index was 0.35, with a critical value of 5.5.
Conclusion: The development of CAPI was positively correlated with the CCI. The risk of developing pressure injury increases with the number and severity of comorbidities. This study shows that the CCI has certain reference value in predicting CAPI.
Keywords: aged, comorbidity, chronic disease, frailty, pressure ulcer, present on admission
Introduction
A pressure injury (PI) is defined as a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure or pressure in combination with shear.1 It is a major health challenge worldwide that imposes a significant financial burden on healthcare systems and negatively affects people’s quality of life.2 People of any age and with any health condition can be affected by PI, but it is most common among elderly and critically ill people with several comorbidities.3 Populations are aging and life expectancy is increasing, and 23% of the total global burden of disease is now associated with chronic diseases in people aged 60 and over.4 As a result, a large number of elderly people living in communities may be potentially at risk of developing PI. Some studies have confirmed that older adults living in the community become more vulnerable to developing PI with increasing age and multiple comorbidities.5 However, current research on PI has mainly focused on the hospital setting, and research examining the presence of PI before hospitalization, known as community-acquired PI (CAPI), has been limited.6 In addition, researchers have found that environmental factors are related to the occurrence of PI.7 Therefore, CAPI needs further study.
Comorbidity is defined as the “presence of more than one disorder in a person in a defined period of time.”8 The Charlson Comorbidity Index (CCI) is a weighted index of comorbidity that combines the number and severity of the conditions.9 The CCI is used widely in clinical research to explore the influence of comorbidity on prognosis and outcome. The CCI is a well-established surrogate marker of comorbidity.10
With further study of the etiology of PI, it has been found that internal factors characterized by comorbidity play an important role in the pathogenesis of PI.11 Although researchers have recognized that contributing comorbidities are associated with the development of PI, the effects of the combination, number, and severity of comorbid conditions on PI are unknown, and there have been few studies examining the correlation between multiple comorbidities as the main exposure factor and PI. Therefore, the purpose of this study was to explore the association between the CCI and CAPI to provide a reference for family caregivers and community workers to prevent CAPI and to promote clinical workers’ understanding of the etiology of PI. This will provide a basis for further study of the influence of different combinations of comorbidities on PI.
Methods
Study Design
This was a case-control study, and it was registered with the China Clinical Trial Center (ChiCTR2100047018, reg. date: 2021/06/07). Participants aged 65 years or above were enrolled from the acute inpatients admitted to the multiple department, such as Internal Medicine, Surgery, Geriatrics, and Intensive Care Unit in Wuhan Third Hospital, which is affiliated to Wuhan University, from January to December 2020. All participants were residents of urban communities.
Demographic and clinical characteristics of participants were extracted from the hospital’s electronic medical records system. This was a retrospective study and all variables were collected prior to the study. First, we extracted participants’ gender, age, all diagnoses names and diagnostic codes to establish a database. These diagnostic codes were based on the 10th revision of the International Classification of Diseases (ICD-10). Secondly, Charlson comorbidities was extracted with ICD-10 codes listed in Table 1,12,13 and their CCI values were calculated. However, acute comorbidity diagnosed for the first time was excluded from the calculation of CCI. Finally, enter the diagnostic names “hypoproteinemia” and “anemia” respectively to find participants with hypoproteinemia and anemia, but acute anemia was ruled out. The establishment of CAPI was based on nursing records from the first nursing assessment within 4 h of admission. CAPI data are extracted from the nursing PI reporting system. The participants were divided into a case group and a control group according to whether CAPI was present on admission.
 |
Table 1 Charlson Comorbidity Index with International Classification of Diseases (ICD-10) Coding |
This study was conducted in compliance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects and the Declaration of Helsinki (as revised in Brazil 2013). It was approved by the Wuhan Third Hospital affiliated to Wuhan University Ethics Committee (number KY2021-011). The study’s data was anonymous, and the requirement for informed consent was therefore waived.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: the inpatients aged 65 and older between January and December 2020. The exclusion criteria were as follows: patients with repeated admissions, younger than 65 years of age, hospital-acquired PI, PI was not described in the case record or was inconsistent. The inclusion and exclusion process is shown in Figure 1.
 |
Figure 1 Flow diagram of the screening and enrollment of study participants. |
CAPI Measurements
All patients completed the first nursing assessment within 4 h of admission, and each patient’s skin condition was recorded. The definition, staging, and characteristics of PI were revised by the National Pressure Ulcer Advisory Panel in 2016.14 Stage 1 PI is local skin integrity with non-blanchable erythema. In Stage 2 PI, the epidermis is lost and the dermis is exposed, forming superficial ulcers. Stage 3 is a full-thickness loss of skin with adipose tissue visible. Stage 4 is a full-thickness skin defect with the tendon fascia skeleton exposed. Non-staging refers to full-thickness skin and tissue loss covered by scabs or carrion, meaning that the depth of the damage cannot be determined. Deep tissue damage often presents as skin integrity with pain and changes in skin temperature, with purple or maroon skin color or congestive blisters.
CCI Measurements
The CCI, introduced by Charlson et al in 1987, is a score based on the number and severity of chronic diseases that accompany a patient’s major disease. It considers 19 comorbid conditions, which are each given a score of 1, 2, 3, or 6. Age-based scoring starts at the age of 50 years, with a 1-point increase for every 10 years above age 50. The sum of all these scores determines the CCI, which ranges from 0 to 24. It contains 19 categories of diseases and their score weights are reproduced in Appendix Table 1.
ICD Measurements
The ICD-10 is the current version of an internationally unified disease-classification system developed by the World Health Organization. The system of coding for a disease is based on its etiological, pathological, clinical, and anatomical features. Comorbidity status was classified using the CCI based on the ICD-10 (see Table 1).
Statistical Analysis
All the analyses were performed with the statistical software package R version 3.3.2 (https://www.r-project.org/, The R Foundation) and the Free Statistics software package version 1.3. Two-tailed tests were performed, with p < 0.05 being considered statistically significant. The baseline characteristics of the participants are expressed as “mean ± standard deviation” (normal distribution) or “median (interquartile range [IQR])” (skewed distribution) for continuous variables, and as percentages for categorical variables. For patient demographics and clinical characteristics, differences between groups were assessed using a chi-squared test for categorical variables, and Student’s t-test or the Mann–Whitney U-test for continuous variables. In this study, univariate logistic regression was used to investigate the associations between the demographic data and clinical characteristics of participants and their CAPI status. The effect of the CCI on CAPI was evaluated using binary logistic regression models (odds ratio [OR] and 95% confidence interval [CI]) with adjustment for major covariables including age, sex, hypoproteinemia, and anemia. The study converted the CCI into a categorical variable and calculated the p value for the trend to verify the results of the CCI as the continuous variable. Smooth curve fitting were used to show the relationship between the CCI and CAPI. By drawing the receiver operating characteristic curve, the CCI was used to predict CAPI.
Results
In this population-based case-control study, the prevalence of CAPI was 4.3% in acute inpatients aged 65 and older. The mean age of participants without PI was 74.9 ± 7.5 years, and the mean age of those with PI was 78.0 ± 8.6 years. A comparison of demographic information and clinical characteristics between the two groups is shown in Table 2.
 |
Table 2 Differences in Baseline Characteristics Between without Pressure Injury and with Pressure Injury |
In univariate analysis, gender, age, myocardial infarction, congestive heart failure, cerebrovascular disease, dementia, moderate or severe renal disease, hemiplegia/paraplegia, severe liver disease, metastatic tumor, hypoproteinemia, and anemia complications were significantly associated with the occurrence of CAPI. The risk of PI was 37% higher in men than in women, and the risk of developing PI increased by 6% for each additional year of age (see Table 3).
 |
Table 3 Univariate Analysis of Community-Acquired Pressure Injury |
A positive relationship was found between the CCI and CAPI in the logistic regression analysis. In non-adjusted Model (OR = 1.45, 95% CI = 1.37–1.53, p < 0.001), and after adjustment for sex, age, hypoproteinemia, and anemia (OR = 1.37, 95% CI = 1.29–1.45, p < 0.001). The CCI was divided into three groups with scores of 2–3, 4–6, or ≥7. The adjusted model showed that the risk of CAPI increased with increasing CCI; trend test p < 0.001 (see Table 4).
 |
Table 4 Association Between Charlson Comorbidity Index and Occurrence Pressure Injury in Regression Model |
To further verify the relationship between CCI and CAPI, smooth curve fitting showed that there was a nonlinear relationship between the CCI and CAPI (p for non-linearity: <0.001, Figure 2). By drawing the receiver operating characteristic (ROC) curve, the CCI was used to predict CAPI. The resulting area under the ROC curve was 0.75 (95% CI = 0.7470–0.7755), and the maximum value of the Youden index was 0.35 with a critical value of 5.5 (Figure 3).
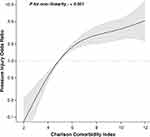 |
Figure 2 Association between CCI and risk of CAPI. The black solid curve represents the odds ratio, and the gray area indicates its 95% confidence interval. |
 |
Figure 3 Receiver operating characteristic (ROC) curve of CAPI and CCI, constructed to evaluate the sensitivity and 1-specificity of CCI in the predict CAPI. |
Discussion
The development of a PI is a complex process that cannot be explained by a single factor but is the result of the interaction between internal and external factors for each individual.15,16 Regrettably, internal factors are often downplayed or disregarded.17 Older people are often at risk of multiple comorbidities,18 and the interactions between comorbidities can increase the complexity of internal factors that cannot be observed directly, making the prevention of PI more difficult. The CCI addresses this complex interaction of multiple comorbidities into a single numeric score, thereby quantifying these complex internal factors and making them observable.19 In the original study, the CCI covered 19 chronic diseases, and these were weighted according to their potential influence on mortality; this was validated for predicting the 1-year mortality in a cohort of hospitalized patients.9 Although the CCI was developed and validated in hospitalized patients, it was further adapted and validated in primary care and community populations, being used to describe the effect of comorbidity in community populations on health outcomes.20 Therefore, previous studies also provide a basis for this study.
The original CCI was based on a review of medical records, and it was first defined by the ICD in the 1990s.21 The ICD is updated as the understanding of chronic diseases evolves, and there are therefore also different versions of the CCI. Several previous studies do not specify the CCI version considered, which ICD edition was applied, or the weightings that were used. This may affect the accuracy and reproducibility of their results. In this study, the ICD-10 version of the CCI was used, and the weights of the comorbidities were clearly defined. This improves the credibility of the present results and is a point of difference between this and other studies.
According to the results of Jaul et al’s research,11 multiple chronic diseases and complicating factors associated with immobility, tissue ischemia, and undernutrition are causes of PI among older adults in community settings. PI is caused by a constant external pressure on local tissues that cannot be released, and It’s addressed via pressure redistribution. However, aging lead to physical decline and limited mobility, they are unable to change their position autonomously to relieve pressure, resulting in persistent exposure to pressure and shear. Therefore, immobility is the immediate cause of PI. Elderly people with multiple chronic diseases often face the cumulative effects of impaired functions of multiple systems, which can aggravate their frailty and lead to limited mobility. Long-duration chronic diseases lead to increased nutrient consumption and decreased physiological reserves while increasing the vulnerability of the skin and susceptibility to PI.22 As a result, comorbidity may reduces an individual’s ability to cope with pressure.
The CCI includes chronic diseases, and among these, congestive heart failure and liver and kidney failure may cause chronic edema and increase skin vulnerability. Neurological diseases such as dementia or Alzheimer’s disease may cause agitation and friction. Parkinson’s disease, antipsychotic drugs, and dementia increase the risk of spasticity. Cancer and other terminal conditions can impair immunocompetence. For example, end-stage renal disease, Uremia is often accompanied by gastrointestinal symptoms, it can significantly affect the ingestion, digestion, and absorption of nutrients, thus resulting in the deterioration of nutritional status.23 Most patients with chronic liver disease have poor appetite and low intake, end-stage liver disease and its complications affect energy synthesis and metabolism, which in turn influence nutritional status.24 Patients with malignant tumors are often in a state of high catabolism and low anabolism, and a large amount of muscle tissue is consumed, leading to physical degeneration and malnutrition, and the body’s activity ability is impaired due to the consumption of muscle tissue.25 Therefore, multiple comorbidities influence all of the body’s systems, including the skin,26 and it appears that the prevalence of PI increases with underlying disease.27 This was also confirmed in this study, and CCI was found to be positively correlated with CAPI.
This study showed that peripheral vascular disease, rheumatism and digestive ulcer diseases had no significant correlation with CAPI, which these comorbidities may not be independent risk factors for PI, but the effect of their combinations on PI is unknown. Leukemia, Lymphoma and HIV/AIDS included a relatively small number of patients, making significance difficult to achieve for the variables analyzed. It is worth noting that there is no significant correlation between diabetes and PI, which may be that diabetes is very common in older adults with or without PI. Therefore, the significance of the difference between PI and diabetes is obscured.
Previous studies have confirmed that low levels serum Albumin and Hemoglobin and higher age increase the risk of PI, which were confirmed in this study. In univariate analysis, gender, age, hypoproteinemia, and anemia were significantly associated with PI. Therefore, these factors that might influence the study results must be excluded. So, after controlling for confounding factors in the regression analysis, the risk of the occurrence of CAPI was found to increase by 37% for every 1-point score increase in the CCI. This suggests that the risk of CAPI increases with the number and severity of comorbidities. In this study, smooth curve fitting was used to confirm the relationship between the CCI and CAPI (see Figure 2). Similar to the results of this study, Kalava et al found that CCI was associated with an increased risk of PI in 60 elderly people living in the community; for every 1-point increase in the CCI, the risk of developing PI increased by 14%.28
The present study found that in those over 65 years of age, for each additional year of age, the risk of developing PI increased by 6%. This increasing age may be the result of increasing skin aging, epidermal barrier defects, and immune senescence increasing skin vulnerability, as well as subcutaneous fat atrophy and the underlying bony structure providing less support to the skin.29
This study also found a correlation between gender and the occurrence of CAPI, which is in contrast to the results of other studies. The higher risk of CAPI found in males may be related to the different lifestyle habits of people of different genders, and this needs to be studied further. Anemic and hypoproteinemic elderly people were found to have a higher risk of CAPI, and this is consistent with the results of previous studies.
In addition, through analysis of the ROC curve and the Youden index, we determined that when the CCI score exceeds 5.5, we should be vigilant about the risk of CAPI. A 10-year PI prevalence survey from China reported that 71.3% of patients with PI had a CCI score 4 or higher, also the results indicate that CCI may be a good indicator for PI risk assessment.30 This is similar to the results of our study. Some risk-assessment measures that require extensive care resources or specialized equipment may be difficult to implement in community and home settings.31 In contrast, the CCI is a simple observational indicator for community workers and family caregivers to provide reference for the prevention of PI. Based on comorbidity and weight of CCI, comorbidity weights were added together, the risk of CAPI should be vigilant when the score reached 5 points or above.
There are several limitations to this study. Firstly, CAPI was defined as having occurred before admission, but the CCI data were extracted after admission. The diagnosis in the CCI is based on chronic conditions that may have been present prior to admission. Therefore, CCI calculations excluded acute comorbidities that were first diagnosed. However, the possibility of inadequately controlled confounding cannot be excluded. In addition, the definition of comorbidity was based on the ICD-10, and the accuracy of this will affect the CCI score. However, in February 2020, China incorporated improving the accuracy of the inpatient diagnosis code into the national medical quality and safety goals and attached great importance to the accuracy of the code. Nevertheless, coding errors may not be completely avoidable. Finally, this study was a single-center sample, therefore, It may affect the generality of research results.
Conclusion
This study found that higher numbers of comorbidities and their greater severity increased the risk of developing CAPI. As such, immobile elderly with multiple comorbidities should be vigilant against developing CAPI. The results show that the CCI has a certain reference value in predicting CAPI for community workers and family caregivers. The influence of different comorbidity combinations on PI is worth further investigation.
Data Sharing Statement
The data that support the findings of this study are openly available in “ResMan” at (http://www.medresman.org.cn/uploads/attachment/share/data/96e71142-f724-4e7a-881f-3ebf8ace08d9.xls).
Acknowledgments
We gratefully thank Jie Liu, PhD of Department of Vascular and Endovascular Surgery, Chinese PLA General Hospital for his contribution to the statistical support and comments regarding the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Haesler E, Editor. Cambridge Media: Osborne Park, Western Australia; 2014.
2. Mervis JS, Phillips TJ. Pressure ulcers: pathophysiology, epidemiology, risk factors, and presentation. J Am Acad Dermatol. 2019;81(4):881–890. doi:10.1016/j.jaad.2018.12.069
3. Hajhosseini B, Longaker MT, Gurtner GC. Pressure injury. Ann Surg. 2020;271(4):671–679. doi:10.1097/SLA.0000000000003567
4. Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi:10.1016/S0140-6736(14)61347-7
5. Latimer S, Chaboyer W, Thalib L, McInnes E, Bucknall T, Gillespie BM. Pressure injury prevalence and predictors among older adults in the first 36 hours of hospitalisation. J Clin Nurs. 2019;28(21–22):4119–4127. doi:10.1111/jocn.14967
6. Chen G, Lin L, Yan-Lin Y, Loretta CY-F, Han L. The prevalence and incidence of community-acquired pressure injury: a protocol for systematic review and meta-analysis. Medicine. 2020;99(48):e22348. doi:10.1097/MD.0000000000022348
7. McGraw C, Drennan VM. Evaluation of the suitability of root cause analysis frameworks for the investigation of community-acquired pressure ulcers: a systematic review and documentary analysis. J Clin Nurs. 2015;24(3–4):536–545. doi:10.1111/jocn.12644
8. Spoorthy MS, Chakrabarti S, Grover S. Comorbidity of bipolar and anxiety disorders: an overview of trends in research. World J Psychiatry. 2019;9(1):7–29. doi:10.5498/wjp.v9.i1.7
9. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
10. Kachlíková M, Sabaka P, Koščálová A, Bendžala M, Dovalová Z, Stankovič I. Comorbid status and the faecal microbial transplantation failure in treatment of recurrent clostridioides difficile infection - pilot prospective observational cohort study. BMC Infect Dis. 2020;20(1):52. doi:10.1186/s12879-020-4773-x
11. Jaul E, Barron J, Rosenzweig JP, Menczel J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr. 2018;18(1):305. doi:10.1186/s12877-018-0997-7
12. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
13. Armitage JN, van der Meulen JH; Royal College of Surgeons Co-morbidity Consensus G. Identifying co-morbidity in surgical patients using administrative data with the Royal college of surgeons Charlson score. Br J Surg. 2010;97(5):772–781. doi:10.1002/bjs.6930
14. Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585–597. doi:10.1097/WON.0000000000000281
15. Coleman S, Gorecki C, Nelson EA, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 2013;50(7):974–1003. doi:10.1016/j.ijnurstu.2012.11.019
16. Bouten CV, Oomens CW, Baaijens FP, Bader DL. The etiology of pressure ulcers: skin deep or muscle bound? Arch Phys Med Rehabil. 2003;84(4):616–619. doi:10.1053/apmr.2003.50038
17. Thomas DR. Does pressure cause pressure ulcers? An inquiry into the etiology of pressure ulcers. J Am Med Dir Assoc. 2010;11(6):397–405. doi:10.1016/j.jamda.2010.03.007
18. Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–674. doi:10.1016/S0895-4356(00)00363-2
19. Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish national registry of patients. BMC Med Res Methodol. 2011;11:83. doi:10.1186/1471-2288-11-83
20. Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med. 2012;10(2):134–141. doi:10.1370/afm.1363
21. Brusselaers N, Lagergren J. The Charlson comorbidity index in registry-based research. Methods Inf Med. 2017;56(5):401–406. doi:10.3414/ME17-01-0051
22. Jaul E. Assessment and management of pressure ulcers in the elderly: current strategies. Drugs Aging. 2010;27(4):311–325. doi:10.2165/11318340-000000000-00000
23. Dinorah C-J, Paola MA, Ximena AC, Ricardo CR, Ángeles E-C. Relationship between nutritional status and gastrointestinal symptoms in geriatric patients with end-stage renal disease on dialysis. Nutrients. 2018;10(4):425. doi:10.3390/nu10040425
24. Juakiem W, Torres DM, Harrison SA. Nutrition in cirrhosis and chronic liver disease. Clin Liver Dis. 2014;18(1):179–190. doi:10.1016/j.cld.2013.09.004
25. Fearon K, Arends J, Baracos V. Understanding the mechanisms and treatment options in cancer cachexia. Nat Rev Clin Oncol. 2013;10(2):90–99. doi:10.1038/nrclinonc.2012.209
26. Campbell JL, Coyer FM, Osborne SR. The skin safety model: reconceptualizing skin vulnerability in older patients. J Nurs Scholarsh. 2015;48(1):14. doi:10.1111/jnu.12176
27. Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17(6):763–771. doi:10.1111/j.1524-475X.2009.00543.x
28. Kalava UR, Cha SS, Takahashi PY. Association between vitamin D and pressure ulcers in older ambulatory adults: results of a matched case-control study. Clin Interv Aging. 2011;6(1):213–219. doi:10.2147/CIA.S23109
29. Chang ALS, Wong JW, Endo JO, Norman RA. Geriatric dermatology review: major changes in skin function in older patients and their contribution to common clinical challenges. J Am Med Dir Assoc. 2013;14(10):724–730. doi:10.1016/j.jamda.2013.02.014
30. Zhao J, Zhang L-X, Zhong Y-L, et al. A 10-year prevalence survey and clinical features analysis of pressure injury in a tertiary hospital in China, 2009–2018. Adv Skin Wound Care. 2021;34(3):150–156. doi:10.1097/01.ASW.0000732740.92841.51
31. Chou R, Dana T, Bougatsos C, et al. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness review. Ann Intern Med. 2013;159(1):28–38. doi:10.7326/0003-4819-159-1-201307020-00006
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
