Back to Journals » International Journal of General Medicine » Volume 15
Association Between Body Mass Index and Female Infertility in the United States: Data from National Health and Nutrition Examination Survey 2013–2018
Authors Zhu L, Zhou B, Zhu X , Cheng F, Pan Y, Zhou Y, Wu Y, Xu Q
Received 2 December 2021
Accepted for publication 9 February 2022
Published 19 February 2022 Volume 2022:15 Pages 1821—1831
DOI https://doi.org/10.2147/IJGM.S349874
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lei Zhu,1,* Bin Zhou,1,* Xi Zhu,1,* Feng Cheng,1 Ying Pan,2 Yi Zhou,2 Yong Wu,1 Qingna Xu3
1Thyroid Surgery Department, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Central Hospital, Lishui City, Zhejiang Province, People’s Republic of China; 2Breast Surgery Department, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Central Hospital, Lishui City, Zhejiang Province, People’s Republic of China; 3Health Care Office, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Central Hospital, Lishui City, Zhejiang Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qingna Xu, Health Care Office, The Fifth Hospital Affiliated to Wenzhou Medical University, Lishui Central Hospital, No. 289, Kuocang Road, Lishui City, Zhejiang Province, People’s Republic of China, Tel +86 13735910709, Email [email protected]
Purpose: This study aimed to investigate the effects of body mass index (BMI) on infertility in women of childbearing age.
Patients and Methods: We performed a cross-sectional study using data from 3624 participants from the National Health and Nutrition Examination Survey (NHANES). We used BMI and fertility status in the survey as independent and dependent variables, respectively. We evaluated their relationship and used smoothed curve fitting and multivariate logistic regression analysis as well as a generalized additive model (GAM) to determine the effect of BMI.
Results: Logistic regression model analysis linked BMI and infertility after adjusting for potential confounders OR 1.03, 95%Cl: 1.02– 1.05). There was a non-linear relationship between BMI and infertility, with each unit increase in BMI reducing the risk of infertility by 33% when BMI was < 19.5 kg/m2. In contrast, when BMI ≥ 19.5 kg/m2, each unit increase in BMI predicted a 3% increase in the risk of infertility.
Conclusion: The relationship between infertility and BMI presented a U-shaped curve. Therefore, a BMI that lay at the extremes of the spectrum tended to predict infertility. We believe that this study will support the maintenance of suitable BMI levels in women preparing for pregnancy.
Keywords: BMI, infertility, nonlinear, NHANES
Introduction
Infertility is the inability to conceive despite regular unprotected intercourse without using any contraception for more than 1 year. It affects millions of families worldwide, touching approximately one in seven couples in developed countries and one in four couples in developing countries.1 In the United States, infertility affects approximately 6.7%- 15.5% of women of reproductive age.2,3 As a result, the Centers for Disease Control and Prevention (CDC) have prioritized its diagnosis and treatment.4
Although it is clearly a global health concern, research has not fully elucidated the factors of its determinants. Infertility stems from occupational factors [eg, shift work, stress, physical (radiation), and toxic (chemicals) sources] or various lifestyle factors (age, nutrition, exercise, obesity, psychological stress, smoking, or alcohol consumption) in addition to environmental pollution factors.5–7
Obesity (BMI ≥ 30 kg/m2) amongst women of reproductive age has increased significantly in the last decades.8,9 This is pertinent because obesity factors increase the time it takes to conceive, reduce conception rates, and render patients less responsive to fertility treatments.10 Several studies have shown that obesity increases the risk of prenatal complications such as gestational hypertension and gestational diabetes.11–13 It is also responsible for prolonging labor, increasing the risk of obstructed labor and cesarean delivery,14 and has notable effects on the fetus.12,15,16 Recent animal experiments have shown that lean and obese animals are typically less fertile, but not necessarily in humans.17 Few high-quality studies have explored the nonlinear relationship between body mass index and infertility. Data in a large 15-year population-based cohort study from Australia shows that higher BMI positively correlates with fertility problems.18 However study shows that low BMI is also associated with infertility.19
A literature review concerning nutrient intake and its effects on female fertility revealed many studies that reported a J-shaped association between infertility and BMI.20 However, they suggest that the effect of body mass on fecundity could be bimodal. We summarized previous studies of the relationship between BMI and infertility and found it to be limited and inconclusive. Therefore, the current study aimed to determine the relationship between BMI and infertility, in terms of linearity, using a large sample from the NHANES database from 2013 to 2018.
Materials and Methods
Data Source
We obtained the original data for this study from the National Health and Nutrition Examination Survey (NHANES), a program that began in the early 1960s. Published by the National Center for Health Statistics (NCHS), it includes surveys on various populations and health topics under the jurisdiction of the US Centers for Disease Control and Prevention (CDC). NHANES is a research program of studies designed to assess the health and nutritional status of the US population, combining interviews and physical examinations. It employs a complex, multistage sampling design to select a nationally representative sample of about 5000 individuals each year.21 Thereafter, it provides comprehensive information on nutrition and health every 2 years for a representative sample of the noninstitutionalized civilian population in the US. The NCHS Research Ethics Review Committee approved the NHANES survey protocol, and all participants of the study provided informed written consent.22
Population
We selected data from the 2013–2018 cycle of the NHANES because only those cycles included health questionnaires concerning infertility issues.23 A total of 29,400 adults participated in this survey over that period. Our study excluded male participants (n =14,452), women older than 45 (n = 4995) and younger than 18 (n= 5630). Similarly, the study also excluded responses with incomplete fertility information (n= 656), missing BMI information (n = 43) and special abnormalities (n= 1). Thus, the final sample population for the purposes of this study was 3623 participants (Figure 1).
 |
Figure 1 Flow chart of sample selection from the NHANES 2013–2018. |
Dependent and Independent Variable
The dependent variable of infertility derived from each woman’s self-report from the Reproductive Health Questionnaire (variable name in questionnaire: RHQ074). In this questionnaire, the investigators asked questions such as, “Have you ever attempted to become pregnant over a period of at least a year without becoming pregnant?”24 The affirmative answer “yes” denoted an “infertile” case; if not, the assumed response would be “fertile.”
The independent variable was BMI. Conventionally, practitioners calculate this value as mass in kilograms divided by height in meters squared, rounded to one decimal place. The NHANES website provides detailed description.25 In accordance with previous literature, we classified BMI into four groups: “Low” (<18.5), “Normal” (18.5–24.9), “Overweight” (24.9–29.9), and “Obese” (>29.9).26
Other Variables
In accordance with previous studies, we used additional covariates in our study. We classified these covariates as demographic or potential confounders that may affect BMI, or fertility status in the NHANES database.2,18,19,24,27,28 They were derived from self-reported data, examination data. Covariates included: age (18–45 years), race/ethnicity (Mexican-American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian, Other Race), educational attainment (Less than high school, High school, More than high school), marital status (Married or Living with partner, Living alone), ratio of family income to poverty (ratio of household income to poverty indicators29), alcohol consumption (at least 12 drinks of alcoholic beverages in the last year), active smoking (at least 100 cigarettes/year), diabetes mellitus, hypertension, and prior pregnancy.
In addition, there are studies that suggest that lifestyle behaviors affect BMI, such as lack of physical activity, thus affecting fertility directly or indirectly. In particular, physical activity induces vasodilation and improves the perfusion of many organs including the female reproductive system and its follicular development.30,31 In contrast, sedentary activity increases the likelihood of conditions such as cardiovascular disease and cancer, while also contributing to weight gain.32–34 Thus, our study included physical activity and sedentary time in the covariates. We divided physical activity into two categories: “vigorous exercise” and “moderate recreational activities.”35 The questionnaire data also from the NHANES database.
Statistical Analysis
In our study, we described continuous variables using the mean and standard deviation, and presented categorical variables as percentages. The main analysis included three steps. First, we used a multiple regression model to test the independent correlation between BMI and infertility. Specifically, we used three models to assess this relationship: 1) no adjustment; 2) adjustment for socio-demographic data only; 3) other covariates shown in Table 1. Second, we detected a nonlinear relationship between BMI and infertility. We calculated the volume inflection point by using a recursive algorithm. Third, we constructed a logistic regression model at the inflection point co-test. The model that gave the best fit based on likelihood-ratio tests and P-values was included.
 |
Table 1 Baseline Characteristics of Participants (N =3623) |
We performed data analyses using the R® statistics package (v.3.4.3, http://www.r-project.org) and Empower® software (v.2.0, http://www.empowerstats.com, X&Y Solutions,Inc. Boston,MA, USA). We expressed statistical significance as two-sided P<0.05.
Results
Baseline Characteristics of Study Participants
Figure 1 shows the inclusion and exclusion criteria of selected participants, after the exclusion of all participants with incomplete or ambiguous responses. In total, 3623 participants took part in this study and Table 1 presents the baseline characteristics of the selected female participants, with respect to infertility (dichotomous variable).
Results of Multiple Regression Models
We constructed three models to explore the independent effect of BMI on infertility and analyzed its independent effect on infertility, using binary logistic regression with single and multiple variables. Table 2 shows the relevant effect size [odds ratio [OR]], 95% confidence intervals (CI), and P-values. There was a significant association between BMI and infertility in models 1, 2, and 3 and the generalized additive model (GAM). The association between body mass index and infertility was positive regardless of the type of adjusted covariates. In the initial model (model 1), each 1-unit increase in body mass index increased the risk of infertility by 4% (OR=1.04; 95% Cl: 1.03–1.05). In model 2 (OR: 1.03, 95% Cl: 1.02–1.05) and model 3 (OR=1.03; 95% Cl: 1.02–1.05), we converted BMI into a categorical variable from the continuous variable (four groups of “Low,” “Normal,” “Overweight,” and “Obese”) for sensitivity analysis. There was a nonlinear relationship between BMI and infertility, and the trends in effect size were analogous for different BMI groups. To solve the nonlinear problem, we used GAM to adjust all the continuous variables in covariates (shown in Table 1) (OR=1.03; 95% Cl: 1.00–1.05), which remained largely consistent with model 3. This sensitivity analysis confirmed the robustness of the results (Table 2).
 |
Table 2 Relationship Between Body Mass Index (Kg/M2) and Fertile or Infertile |
Stratified Analysis by Potential Effect Modifiers
We then performed subgroup analysis to assess the effect of BMI on infertility. As shown in Figure 2, the interactions tested were not statistically significant among the different ethnic/racial groups, different education groups, or household income to poverty ratio. The same was true with regard to physical activity, alcohol consumption, smoking habits, history of hypertension, or type of insurance. The interactions of the abovementioned values were 0.70, 0.10, 0.93, 0.52, 0.64, 0.97, 0.28 0.46, 0.22, 0.73 respectively. Conversely, we found statistically significant differences (P<0.05) with respect to age groups, marital status, history of diabetes, and whether or not the couple had undergone a prior pregnancy. Therefore, there was an evident interaction between BMI and age, marital status, history of diabetes mellitus, and prior pregnancy. Moreover, BMI was positively associated with infertility in the subgroup with a history of diabetes with or without diabetes stratification, negatively associated with infertility in the critical status subgroup, and positively associated with infertility with respect to age, marital status, and prior pregnancy.
 |
Figure 2 Subgroups* analyses of the effect of BMI on infertility. |
Results of Nonlinear of BMI and Infertility
We fitted the GAM and the smoothed curve (penalized curve method) to explore the potential nonlinear relationship between BMI and infertility (Figure 3) and found a nonlinear U-shaped relationship. We calculated the volume inflection point using a recursive algorithm, resulting in a value of 19.5 (Table 3). The OR and 95% Cl on the left side of the inflection point were 0.67 and 0.47–0.95, respectively. Similarly, the OR and 95% CI on the right side were 1.03 and 1.02–1.05, respectively.
 |
Table 3 Threshold Effect Analysis of Body Mass Index (Kg/M2) and Infertility Rate Using Piece-Wise Linear Regression |
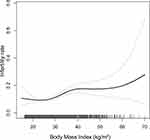 |
Figure 3 The correlation between BMI and infertility rate (using penalized spline method). |
Discussion
Our cross-sectional study used data from women of childbearing age enrolled in NHANES from 2013–2018 in the US to investigate the existence of an independent relationship between BMI and infertility. After adjusting for other covariates, BMI positively associated with infertility. After transforming BMI into a categorical variable, we observed the possibility of a nonlinear relationship with univariate and multifactorial logistic regression. Hence, we considered a smooth curve fit and a bipartite linear regression model and determined the inflection point to be 19.5 kg/m2. The trends of the effect size were not consistent on the two sides of the inflection point [left side OR: 0.67, 95% Cl (0.47, 0.95); right side OR: 10.3, 95% Cl (1.02, 1.05)]. The above results presented a U-shaped curve relationship between BMI and infertility.
Infertility is a prevalent problem that has a significant impact on individuals, families, and communities. Modifiable lifestyle factors may affect the chances of conceiving and delivering a baby. Among these lifestyle factors, BMI is an important component.
Previous studies have pointed out the non-negligible effect of leanness on the menstrual cycle and female infertility, where it causes gonadotropin dysregulation and subsequent anovulation.36 In another study, researchers used a weight gain regimen to treat 29 slim women with unexplained infertility.37 As they gradually gained weight, the follicle-stimulating hormone (FSH) and luteinizing hormone (LH) of the subjects gradually reached normal ratios. This accompanied the gradual improvement of ovulatory cycles and amenorrhea symptoms, culminating in conception in 19 of the subjects. These studies suggest that a low BMI can lead to infertility in women of reproductive age, which is consistent with the findings in our study.
In addition, obesity is a growing global health concern, especially for women of reproductive age and infertility has been attributable to a variety of chronic diseases such as polycystic ovary syndrome (PCOS), hypertension, and diabetes.38–40 Similarly, reduced fertility has been attributable to obesity resulting in biochemical pregnancies, ectopic and spontaneous abortions.41 A Danish study showed a slight increase in the chance of infertility in children of overweight mothers compared to those of mothers of normative weight.39 Additional reports suggest that obese women tend to present dysregulation of the hypothalamic-pituitary-gonadal axis.42 This results in reduced gonadotropin levels, producing symptoms such as irregular menstruation and anovulation, causing infertility. These studies on obesity and infertility correspond with the findings of our study that suggest the probability of infertility increasing as BMI increases.
In our study, we noted the existence of a threshold effect between BMI and infertility, such that different association were evident when BMI levels were below or above 19.5 kg/m2.
Overall, there was some clinical value in our novel study. First, it detected a U-shaped curve association between infertility and BMI for the first time in a large-scale cross-sectional study in US women. Second, the GAM model and smoothed curve fit (penalized curve method) explored the nonlinear relationship between infertility and BMI, which offers a more significant clinical application than previous studies. Third, we based our study on a national survey with a large sample size. To support the robustness of our findings, we also used a series of sensitivity analyses on the relationship between BMI and female infertility, which fully explained this nonlinear relationship. Fourth, the results of our study will contribute to the development of strategies to improve infertility treatment and add to the body of knowledge concerning female reproductive health.
However, our study also has limitations. First, we conducted our study on 3623 women in the US, aged 18–45 years, thus it is not applicable to women outside this age range or men. In addition, the findings may not apply to women outside the US. Second, we were unable to draw a causal relationship between BMI and infertility because of the cross-sectional nature of our study. As with other studies, ours had inevitable and inherent flaws. We noted that most participants in the study were multipara. Owing to the lack of supplementary information in the NHANES database, we were unable to determine whether they experienced primary or secondary infertility, thus, we could not ascertain the duration of their infertility. Finally, we could not assess additional indicators related to obesity, such as body fat, waist, hip circumference, or waist-to-hip ratio.
Conclusion
In our study, we found a U-shaped curve between infertility and BMI. Therefore, a BMI that was too low or too high was a potential hazard for infertility in women. We believe that this study will support the maintenance of more appropriate BMI levels in women preparing for pregnancy.
Such measures are useful for increasing the possibility of pregnancy in women with infertility, for the improvement of social population has a certain effect.
Abbreviations
BMI, body mass index; NHANES, National Health and Nutrition Examination Survey; GAM, generalized additive model; CI, confidence interval; OR, odds ratio.
Data Sharing Statement
All the data sets we used for this study are publicly available from the NHANES website https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
Ethics Approval and Consent to Participate
This study was reviewed and approved by the Ethics Committee of the Lishui Central Hospital,Zhejiang Province (N0.2021-224). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).The NCHS Research Ethics Review Committee approved the NHANES survey protocol (https://www.cdc.gov/nchs/nhanes/irba98.htm), and all participants of the study provided informed written consent.
Acknowledgments
We would like to thank all of the NHANES participants. Meanwhile, we gratefully thank Dr. Xin-Lin Chen for providing statistical methodology consultation. Also, we would like to thank the Charlesworth Group (www.charlesworth-group.com) for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Lishui Municipal Science and Technology Program (2020SJZC045).
Disclosure
The authors declare no conflicts of interest.
References
1. MasCarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356. doi:10.1371/journal.pmed.1001356
2. Key Statistics from the National Survey of Family Growth. Available from: https://www.cdc.gov/nchs/nsfg/key_statistics/i.htm#infertility. Accessed February 4, 2019.
3. Thoma ME, McLain AC, Louis JF, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99(5):1324–1331.e1321. doi:10.1016/j.fertnstert.2012.11.037
4. Macaluso M, Wright-Schnapp TJ, Chandra A, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril. 2010;93(1):
5. Zhu F, Chen C, Zhang Y, et al. Elevated blood mercury level has a non-linear association with infertility in U.S. women: data from the NHANES 2013-2016. Reprod Toxicol. 2020;91:53–58. doi:10.1016/j.reprotox.2019.11.005
6. Lee S, Min JY, Min KB. Female infertility associated with blood lead and cadmium levels. Int J Environ Res Public Health. 2020;17:5.
7. Sharma R, Biedenharn KR, Fedor JM, Agarwal A. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol. 2013;11:66. doi:10.1186/1477-7827-11-66
8. Chandrasekaran S, Neal-Perry G. Long-term consequences of obesity on female fertility and the health of the offspring. Curr Opin Obstet Gynecol. 2017;29(3):180–187. doi:10.1097/GCO.0000000000000364
9. Reynolds R, Gordon A. Obesity, fertility and pregnancy: can we intervene to improve outcomes? J Endocrinol. 2018;239(3):R47–R55. doi:10.1530/JOE-18-0199
10. Broughton DE, Moley KH. Obesity and female infertility: potential mediators of obesity’s impact. Fertil Steril. 2017;107(4):840–847. doi:10.1016/j.fertnstert.2017.01.017
11. Booker WA. Hypertensive disorders of pregnancy. Clin Perinatol. 2020;47(4):817–833. doi:10.1016/j.clp.2020.08.011
12. Gualdani E, Di Cianni G, Seghieri M, Francesconi P, Seghieri G. Pregnancy outcomes and maternal characteristics in women with pregestational and gestational diabetes: a retrospective study on 206,917 singleton live births. Acta Diabetol. 2021;58(9):1169–1176. doi:10.1007/s00592-021-01710-0
13. Retnakaran R. Diabetes in pregnancy 100 years after the discovery of insulin: hot topics and open questions to be addressed in the coming years. Metabolism. 2021;119:154772. doi:10.1016/j.metabol.2021.154772
14. Carroza Escobar MB, Ortiz Contreras J, Bertoglia MP, Araya Bannout M. Pregestational obesity, maternal morbidity and risk of caesarean delivery in a country in an advanced stage of obstetric transition. Obes Res Clin Pract. 2021;15(1):73–77. doi:10.1016/j.orcp.2020.12.006
15. Otero-Naveiro A, Gómez-Fernández C, Álvarez-fernández R, Pérez-López M, Paz-Fernández E. Maternal and fetal outcomes during pregnancy and puerperium in obese and overweight pregnant women. A cohort study. Arch Gynecol Obstet. 2021;304(5):1205–1212. doi:10.1007/s00404-021-06059-x
16. Pereda J, Bove I, Pineyro MM. Excessive maternal weight and diabetes are risk factors for macrosomia: a cross-sectional study of 42,663 pregnancies in Uruguay. Front Endocrinol (Lausanne). 2020;11:588443. doi:10.3389/fendo.2020.588443
17. Tiezzi F, Maltecca C, Cecchinato A, Penasa M, Bittante G. Thin and fat cows, and the nonlinear genetic relationship between body condition score and fertility. J Dairy Sci. 2013;96(10):6730–6741. doi:10.3168/jds.2013-6863
18. Mena GP, Mielke GI, Brown WJ. Do physical activity, sitting time and body mass index affect fertility over a 15-year period in women? Data from a large population-based cohort study. Human reprod. 2020;35(3):676–683. doi:10.1093/humrep/dez300
19. Foucaut AM, Faure C, Julia C, Czernichow S, Levy R, Dupont C. Sedentary behavior, physical inactivity and body composition in relation to idiopathic infertility among men and women. PLoS One. 2019;14(4):e0210770. doi:10.1371/journal.pone.0210770
20. Fontana R, Della Torre S. The deep correlation between energy metabolism and reproduction: a view on the effects of nutrition for women fertility. Nutrients. 2016;8(2):87. doi:10.3390/nu8020087
21. National Center for Health Statistics (NCHS).National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021. Available from: https://www.cdc.gov/nchs/nhanes/index.htm.
22. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2017. Available from: https://www.cdc.gov/nchs/nhanes/irba98.htm.
23. Kim SY, Min C, Kim HJ, Choi HG. Low thyroid-stimulating hormone levels are associated with annoying tinnitus in adult women: Korea National Health and Nutrition Examination Surveys. Otol Neurotol. 2021;42(4):e408–e415. doi:10.1097/MAO.0000000000003030
24. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2020. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/BMX_J.htm.
25. Arya S, Dwivedi AK, Alvarado L, Kupesic-Plavsic S. Exposure of U.S. population to endocrine disruptive chemicals (Parabens, Benzophenone-3, Bisphenol-A and Triclosan) and their associations with female infertility. Environ Pollution. 2020;265(PtA):114763. doi:10.1016/j.envpol.2020.114763
26. Brenes-Monge A, Saavedra-Avendaño B, Alcalde-Rabanal J, Darney BG. Are overweight and obesity associated with increased risk of cesarean delivery in Mexico? A cross-sectional study from the National Survey of Health and Nutrition. BMC Pregnancy Childbirth. 2019;19(1):239. doi:10.1186/s12884-019-2393-5
27. Denison FC, Norwood P, Bhattacharya S, et al. Association between maternal body mass index during pregnancy, short-term morbidity, and increased health service costs: a population-based study. BJOG. 2014;121(1):
28. Fazzi C, Mohd-Shukri N, Denison FC, Saunders DH, Norman JE, Reynolds RM. Activity behaviors in lean and morbidly obese pregnant women. Scand J Med Sci Sports. 2018;28(10):2189–2195. doi:10.1111/sms.13219
29. Devarshi PP, Legette LL, Grant RW, Mitmesser SH. Total estimated usual nutrient intake and nutrient status biomarkers in women of childbearing age and women of menopausal age. Am J Clin Nutr. 2021;113(4):1042–1052. doi:10.1093/ajcn/nqaa392
30. Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. 2018;5:135. doi:10.3389/fcvm.2018.00135
31. Hunter RH. Components of oviduct physiology in eutherian mammals. Biol Rev Camb Philos Soc. 2012;87(1):244–255. doi:10.1111/j.1469-185X.2011.00196.x
32. Ekelund U, Tarp J, Fagerland MW, et al. Joint associations of accelerometer measured physical activity and sedentary time with all-cause mortality: a harmonised meta-analysis in more than 44 000 middle-aged and older individuals. Br J Sports Med. 2020;54(24):1499–1506. doi:10.1136/bjsports-2020-103270
33. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021. Available from: https://wwwn.cdc.gov/nchs/nhanes/Search/DataPage.aspx?Component=Questionnaire&CycleBeginYear=2017.
34. Piirtola M, Kaprio J, Svedberg P, Silventoinen K, Ropponen A. Associations of sitting time with leisure-time physical inactivity, education, and body mass index change. Scand J Med Sci Sports. 2020;30(2):322–331. doi:10.1111/sms.13575
35. Lemes ÍR, Pinto RZ, Turi Lynch BC, et al. The association between leisure-time physical activity, sedentary behavior, and low back pain: a cross-sectional analysis in primary care settings. Spine. 2021;46(9):596–602. doi:10.1097/BRS.0000000000003996
36. Bringer J, Hedon B, Giner B, Richard JL, Jaffiol C. [Influence of abnormal weight and imbalanced diet on female fertility]. Presse Medicale. 1990;19(31):1456–1459. French.
37. Bates GW. Body weight control practice as a cause of infertility. Clin Obstet Gynecol. 1985;28(3):632–644. doi:10.1097/00003081-198528030-00018
38. Arya S, Hansen KR, Peck JD, Wild RA. Metabolic syndrome in obesity: treatment success and adverse pregnancy outcomes with ovulation induction in polycystic ovary syndrome. Am J Obstet Gynecol. 2021;225(3):
39. Arendt LH, Høyer BB, Kreilgaard AF, et al. Maternal pre-pregnancy overweight and infertility in sons and daughters: a cohort study. Acta Obstet Gynecol Scand. 2021;100(5):843–849. doi:10.1111/aogs.14045
40. Lang AY, Harrison CL, Boyle JA. Preconception lifestyle and weight-related behaviors by maternal body mass index: a cross-sectional study of pregnant women. Nutrients. 2019;11:4.
41. Whynott RM, Summers KM, Van Voorhis BJ, Mejia RB. Effect of body mass index on intrauterine insemination cycle success. Fertil Steril. 2021;115(1):221–228. doi:10.1016/j.fertnstert.2020.07.003
42. Lainez NM, Coss D. Obesity, neuroinflammation, and reproductive function. Endocrinology. 2019;160(11):2719–2736. doi:10.1210/en.2019-00487
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
