Back to Journals » Journal of Inflammation Research » Volume 12
Assessment of T helper 17-associated cytokines in thromboangiitis obliterans
Authors Keramat S , Sadeghian MH, Keramati MR, Fazeli B
Received 2 June 2019
Accepted for publication 25 July 2019
Published 5 September 2019 Volume 2019:12 Pages 251—258
DOI https://doi.org/10.2147/JIR.S218105
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ning Quan
Video abstract presented by Shayan Keramat.
Views: 138
Shayan Keramat,1 Mohammad Hadi Sadeghian,1,2 Mohammad Reza Keramati,1,2 Bahare Fazeli3,4
1Hematology Department, Faculty of Medicine, Mashhad University of Medical Science, Mashhad, Iran; 2Pathology Department, Cancer Molecular Pathology Research Center, Mashhad University of Medical Sciences, Mashhad, Iran; 3Immunology Department, Immunology Research Center, Inflammation and Inflammatory Diseases Division, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran; 4Department of Angiology, L.Sacco Hospital, Vascular Independent Research and Education, European Organization, Milan, Italy
Correspondence: Bahare Fazeli
Immunology Department, Immunology Research Center, Inflammation and Inflammatory Diseases Division, School of Medicine, Mashhad University of Medical Sciences, Pardis Campus, Azadi Sqr, Mashhad, Iran
Tel +98 513 800 2379
Fax +98 513 841 4499
Email [email protected]
Background: The management of thromboangiitis obliterans (TAO) remains a medical challenge because of its unknown etiology. It is also not known whether it is a systemic or localized disease or a type of autoimmune vasculitis.
Methods: In this study, we evaluated the serum level of IL-17 and IL-23 which increase in both systemic inflammation and autoimmunity, in 60 TAO patients and 30 age- and smoking habit-matched controls. Also, IL-22, which has reported high level during infection but not in autoimmunity, was evaluated.
Results: The serum levels of IL-17, IL-22 and IL-23 were significantly higher in the TAO patients in comparison with the controls (P<0.001). Notably, the serum levels of IL-17, IL-22 and IL-23 were highest in the patients with the chief complaint of chronic ulcer and lowest in the patients with gangrene (P<0.05). Also, the serum level of IL-22 was significantly higher in the anemic patients in comparison with the non-anemic patients (P=0.03).
Conclusion: Owing to our findings, TAO appears more likely to be a systemic disorder rather than a localized vasculopathy. Therefore, treatment protocols based on systemic treatment of TAO patients may be more helpful than localized treatment, such as bypass surgery and endovascular procedures. Also, according to our findings regarding the high level of IL-22, the trigger of TAO development may be an infectious pathogen. However, additional research is highly recommended to investigate whether TAO is an infectious disease or an infectious-induced autoimmunity.
Keywords: thromboangiitis obliterans, Buerger’s disease, autoimmunity, interleukin-17, interleukin-22, interleukin-23
Introduction
Thromboangiitis obliterans (TAO), or Buerger’s disease, is an episodic, non-atherosclerotic peripheral vascular disease, which is usually seen in young male smokers and is especially common in the Middle East, Southeast Asia, the Far East and Eastern Europe. Its highly inflammatory thrombosis formation could lead to occlusions of small- and medium-sized vessels and, consequently, can lead to tissue gangrene and limb loss.1
The etiology of TAO remains unknown. It is also not known whether it is a systemic or localized disease.2 Therefore, management of TAO remains a medical challenge. Although there is a close relationship between TAO outcomes and smoking, smoking on its own cannot explain the low prevalence, male gender-based and geographical distribution of the disease.3 It has been suggested that TAO might be a type of autoimmune vasculitis. However, unlike in other types of vasculitis, TAO patients usually do not demonstrate a favorable response to immunosuppressants.4,5 In addition, there is evidence that the trigger of TAO development might be an infectious pathogen, such as Porphyromonas gingivalis or Rickettsiales. However, this hypothesis has neither been confirmed nor ruled out.6,7
Owing to the fact that consideration of TAO as a systemic inflammatory disease influences treatment policies, more investigation regarding this issue is needed.
Notably, the presence of pro-inflammatory cytokines and inflammatory mediators in plasma is known as systemic inflammation.8
Until recently, the serum levels of several cytokines and inflammatory mediators in TAO have been measured, and the results of measurement indicate evidence for systemic inflammation.7,9–13 However, TAO is not yet considered a systemic disease, and some treatment protocols, such as endovascular or bypass surgery, are pursued based on the assumption that TAO is a localized vasculopathy.14
In this study, we evaluated the serum level of IL-17 and its inducer, the so-called IL-23 in TAO patients and controls. It has been demonstrated that these cytokines increase in both systemic inflammation and autoimmunity.9,15,16 Also, a high serum level of IL-22 has been reported during infection but not in autoimmunity.17 If all of these cytokines were significantly higher in TAO patients than in controls, it could indicate that TAO is more likely a systemic inflammatory disease.9,18 To differentiate the trigger of systemic inflammation, it was hoped that IL-22 would provide a clue regarding whether the TAO trigger is more likely an infection or an auto-antigen.19
Materials and methods
We analyzed plasma samples from 60 male Caucasian patients from February 2016 through February 2019. TAO diagnosis was clinically confirmed according to Shionoya’s criteria with angiography confirmation.20 To prevent bias regarding the influence of smoking on Th17-associated cytokines, 30 age- and smoking habit-matched male Caucasian controls were enrolled in this study. The clinical manifestations of the patients, along with complete blood count (CBC) data, were documented for each patient. IL-22, IL-23 and IL-17 were evaluated using the ELISA method (ZellBio GmbH, Ulm, Germany). This study has been approved by the ethical committee of Mashhad University of Medical Sciences and all patients and controls signed a written consent form before participating in this study (ethical code: MUMS-961500). The data were analyzed using Statistical Package for the Social Sciences (SPSS) version 11.5 (SPSS Inc., Chicago, IL, USA).
Results
Demographic features
In total, 60 TAO patient plasma samples and 30 plasma samples from age-, gender- and smoking habit-matched controls were enrolled in the current study. All of the TAO patients were Caucasian men with a previous TAO diagnosis according to Shionoya’s criteria and angiography confirmation who reported due to paraesthesia (35%), pain (35%), chronic ulcer (14%) or gangrene (16%). The mean age of the patients was 42±7 years. The mean daily cigarette smoking was 18±13 cigarettes per day (maximum 60 and minimum 2 cigarettes/day), and the mean duration of smoking was 21±8 years (maximum 37 and minimum 2 years). The duration of disease diagnosis was 7.7±5.3 years (maximum 16 and minimum 1 year).
Complete blood count results
According to the most recent definition of anemia by the WHO,21 25% of the patients had anemia (hemoglobin <13 g/dL), with a mean of 12±0.9 g/dL. Approximately, 18% had hemoglobin (Hgb) >13 g/dL (14.4±1 g/dL), but with abnormal mean corpuscular volume, mean corpuscular hemoglobin (MCH) and MCH concentration (MCHC) indices. Approximately, 36% of the patients had Hgb >14 g/dL, with a mean of 16±1.2 g/dL.
According to the definition of neutrophilia (i.e., absolute neutrophil count >7700 cells/μL),22 approximately 11% of the patients had neutrophilia, with a mean of 8510±89 cells/μL.
A total of 45% of the patients had platelet aggregation in the CBC analysis. Notably, 45% of the patients also had low mean platelet volume (MPV), with a mean of 8.7±0.4 fL, and the rest of the patients had normal MPV, with a mean of 10.2±0.2 fL.
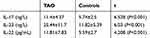
Th17-associated cytokines
The mean levels of IL-17, IL-22 and IL-23 in the TAO patients and the control group are summarized in Table 1. The serum levels of IL-17, IL-22 and IL-23 were significantly higher in the TAO patients in comparison with the controls (P<0.001).
Among the TAO patients, the serum levels of IL-17, IL-22 and IL-23 were highest in the patients with the chief complaint of chronic ulcer and lowest in the patients with gangrene (Figure 1).
Also, the serum level of IL-22, but not IL-17 or IL-23, was significantly higher in the anemic patients, with a Hgb level of less than 13 g/dL in comparison with the non-anemic patients, with a Hgb level of >14 g/dL (P=0.03) (Figure 2).
 |
Figure 2 The mean serum levels of (A) IL-17, (B) IL-22 and (C) IL-23 in the anemic and non-anemic thromboangiitis obliterans patients. |
Similarly, the serum levels of IL-17 and IL-22 were significantly higher in the patients with neutrophilia (Figure 3).
 |
Figure 3 The mean serum levels of (A) IL-17, (B) IL-22 and (C) IL-23 in thromboangiitis obliterans patients with and without neutrophilia. |
The serum levels of IL-17, IL-22 and IL-23 showed no significant differences between the patients with or without platelet aggregation. However, the serum level of IL-22 was significantly lower in the patients with low MPV (P=0.001) (Figure 4).
 |
Figure 4 The mean serum levels of (A) IL-17, (B) IL-22 and (C) IL-23 in thromboangiitis obliterans patients with low and normal mean platelet volume. |
Discussion
TAO is regarded as an inflammatory, occlusive, peripheral vascular disease. The etiology of TAO remains unknown.2,3 However, the close relationship between TAO and smoking was noted soon after the definition of the disease by Leo Buerger. Currently, smoking cessation is a mandatory feature of TAO treatment. However, smoking on its own cannot explain the low prevalence and geographical distribution of TAO.1,2 Even TAO classification is challenging: it is usually viewed as a peripheral arterial disease rather than a type of vasculitis, and TAO patients are typically referred to angiologists or vascular surgeons as opposed to rheumatologists.23 Although several studies found significantly higher serum levels of tumor necrosis factor-α (TNF-α), IL-1 and IL-6 as the negative feedback of TNF and IL-1 in TAO patients in comparison to smoker controls,9,10,12 TAO is not yet considered a systemic disease.
This may be because of the unfavorable response of TAO to immunosuppressant medication and its favorable response to smoking cessation.5,23
In this study, the serum levels of IL-17, IL-22 and IL-23 were significantly higher in the TAO patients in comparison to the controls. Even in the patients without manifestation of critical limb ischemia and those in the silent phase of the disease with only toe paraesthesia, the Th17-related cytokines were significantly higher than in the controls. This finding may indicate that Th17-related cytokines play a role in the development and pathology of TAO.
Notably, the increased number of circulating Th17 cells and increased serum levels of IL-17 and IL-23 have been demonstrated in systemic vasculitis.24 Also, a study in 2012 on 20 TAO patients demonstrated a significantly higher level of Th17 in comparison to the controls, and the authors concluded that TAO could be an autoimmune disorder.9 However, high levels of IL-17 and IL-23 have also been demonstrated in infectious diseases.25–29 In this study, we evaluated not only the serum levels of IL-17 and IL-23 but also IL-22 in a larger sample size of TAO patients (n=60) in different phases of the disease along with a smoking habit-matched control group to control for the bias of influence of smoking on Th17.
Th17 cells are a subset of T helper cells that play a key role in inflammation by activating neutrophils and enhancing the production of inducible nitric oxide synthase by neutrophils.30 As such, Th17 cells play a role in immune defense against extracellular bacteria, the released outer membrane vesicles of intracellular bacteria, and also fungal species. It has been demonstrated that Th17 cells can play a role in autoimmune diseases, possibly by indirectly influencing anti-neutrophil cytoplasmic antibodies (ANCA) production.31,32
IL-17 is the main cytokine of Th17.33 Notably, co-secretion of IL-17 and IL-22 indicates that the source of both cytokines is Th17.19,34 However, it has been demonstrated that there is an array of cell types, the so-called Th22, that can produce IL-22 independent of IL-17.35 IL-22 induces antimicrobial peptides from epithelial cells and also recruits the neutrophils to sites of bacterial invasion.36,37 In addition, it has been demonstrated that IL-22 can regulate wound healing and angiogenesis.38 IL-23 is the key cytokine required for IL-17 and IL-22 secretion from Th17, and its main source is monocyte and dendritic cells.39
In this study, the serum levels of both IL-17 and IL-23 significantly decreased in the patients with a chief complaint of gangrene, which might have been due to the omission of Th17 in the gangrenous tissue. However, owing to the fact that the serum levels of the studied cytokines in the patients with gangrenous tissue were also significantly higher than in the controls, there must be another source of Th17 in TAO, such as the lymph nodes. On the other hand, high levels of the studied cytokines, regardless of the clinical manifestations of the TAO patients, may indicate that TAO is more likely a systemic disease rather than a localized vasculopathy.
Moreover, according to a significantly higher serum level of IL-22 in the TAO patients in comparison with the controls, evidence of a high serum level of IL-22 during active infection, and no evidence supporting the role of IL-22 in developing ANCA antibodies, TAO appears to be a systemic disease that is triggered by an infectious pathogen.6,7
However, our findings cannot offer a conclusion regarding whether TAO is an infectious-induced autoimmunity or entirely an infectious disease.2,3
Notably, 32.5% of the TAO patients had anemia (Hgb <13 g/dL), and IL-22 was significantly higher in the anemic patients as compared to the non-anemic patients. In this vein, it has been demonstrated that IL-22 plays a role in inducing hepcidin production. Hepcidin is a systemic iron hormonal regulator that generally increases with inflammation and infection and acts as a host defense mechanism to decrease iron availability for pathogens. Therefore, IL-22 may play a role in the induction of anemia by increasing hepcidin and, consequently, reducing the access of erythroblasts to iron for the production of hemoglobin.40,41
Owing to the fact that neutrophils are the source of IL-17 and IL-22 production during infection by promoting the synthesis of antimicrobial peptides,42–44 significantly higher levels of IL-17 and IL-22 in the patients with neutrophilia are a reasonable outcome and may suggest support for the role of an infectious pathogen in the pathogenesis of TAO.
Several research reports have been published on the association between IL-17, IL-22 and IL-23 and platelet aggregation.45,46 However, according to our findings, no significant differences in the serum levels of these cytokines in the patients with or without platelet aggregation were observed. This finding may indicate that another, as yet unknown cause must be identified for platelet aggregation in TAO patients. Also, given the significant correlation between IL-22 and MPV, we did not find adequate research to justify this relationship.
Conclusion
Given the significantly higher serum levels of IL-17, IL-22 and IL-23 even in the TAO patients in the quiescent phase of the disease in comparison to the controls, TAO appears more likely a systemic disorder rather than a localized vasculopathy, and Th17-related cytokines could play a role in the pathology of TAO. Therefore, treatment policies based on systemic treatment of TAO patients may be more helpful than localized treatment, such as bypass surgery and endovascular procedures. Also, our findings relative to the high level of IL-22, particularly in the patients with neutrophilia and a low level of MPV, suggest that the trigger of TAO development may be an infectious pathogen. However, additional research is highly recommended to investigate whether TAO is an infectious disease or an infectious-induced autoimmunity.
Acknowledgment
The authors appreciate Dr Hossein Taheri and Mrs Saeede Mehraban for their helpful cooperation in this study.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Fazeli B. Buerger’s disease as an indicator of socioeconomic development in different societies, a cross-sectional descriptive study in the North-East of Iran. Arch Med Sci. 2010;6(3):343–347. doi:10.5114/aoms.2010.14253
2. Fazeli B, Rezaee SA. A review on thromboangiitis obliterans pathophysiology: thrombosis and angiitis, which is to blame? Vascular. 2011;19(3):141–153. doi:10.1258/vasc.2010.ra0045
3. Olin JW. Thromboangiitis obliterans : 110 years old and little progress made. J Am Heart Assoc. 2018;7(23):e011214. doi:10.1161/JAHA.118.008528
4. Bajema IM, Bruijn JA, Casian A, et al. The European Vasculitis Society 2016 meeting report. Kidney Int Rep. 2017;2(6):1018–1031. doi:10.1016/j.ekir.2017.06.007
5. Saha K, Chabra N. Treatment of patients with thromboangiitis obliterans with cyclophosphamide. Angiology. 2001;52(6):399–407. doi:10.1177/000331970105200605
6. Fazeli B, Ravari H, Ghazvini K. Rickettsia infection could be the missing piece of the Buerger’s disease puzzle. Int Angiol. 2017;36(5):410–416. doi:10.23736/S0392-9590.17.03420-4
7. Mohareri M, Mirhosseini A, Mehraban S, Fazeli B. Thromboangiitis obliterans episode: autoimmune flare-up or reinfection? Vasc Health Risk Manag. 2018;14:247–251. doi:10.2147/VHRM.S127393
8. Zotova NV, Chereshnev VA, Gusev EY. Systemic inflammation: methodological approaches to identification of the common pathological process. PLoS ONE. 2016;11(5):e0155138. doi:10.1371/journal.pone.0155138
9. Dellalibera-Joviliano R, Joviliano EE, Silva JS, Evora PR. Activation of cytokines corroborate with development of inflammation and autoimmunity in thromboangiitis obliterans patients. Clin Exp Immunol. 2012;170(1):28–35. doi:10.1111/j.1365-2249.2012.04624.x
10. Slavov ES, Stanilova SA, Petkov DP, Dobreva ZG. Cytokine production in thromboangiitis obliterans patients: new evidence for an immune-mediated inflammatory disorder. Clin Exp Rheumatol. 2005;23(2):219–226.
11. Dellalibera-Joviliano R, Jacob-Ferreira AL, Joviliano EE, Tanus-Santos JE, Evora PR. Imbalanced matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 activities in patients with thromboangiitis obliterans. Vasc Med. 2012;17(2):73–78. doi:10.1177/1358863X11435979
12. Wu S, Sun X, Wu W, Shi D, Jiang T. Effect of revascularization on IL-6 and TNF-α in patients with thromboangiitis obliterans. Exp Ther Med. 2018;15(4):3947–3951. doi:10.3892/etm.2018.5877
13. De Caridi G, Bitto A, Massara M, et al. Increased Serum HMGB-1, ICAM-1 and metalloproteinase-9 levels in Buerger’s patients. Curr Vasc Pharmacol. 2016;14(4):382–387.
14. Lee CY, Choi K, Kwon H, et al. Outcomes of endovascular treatment versus bypass surgery for critical limb ischemia in patients with thromboangiitis obliterans. PLoS ONE. 2018;13(10):Oct.
15. Peris K, Orlandi A, Ferlosio A, et al. Expression of IL-23/Th17-related cytokines in basal cell carcinoma and in the response to medical treatments. PLoS ONE. 2017;12(8):e0183415. doi:10.1371/journal.pone.0183415
16. Xu L, Zhang T, Liu Z, Li Q, Xu Z, Ren T. Critical role of Th17 cells in development of autoimmune hemolytic anemia. Exp Hematol. 2012;40(12):994–1004.e4. doi:10.1016/j.exphem.2012.08.008
17. Yen J-H, Tükel Ç, Rapsinski GJ, et al. Microbial amyloids induce interleukin 17A (IL-17A) and IL-22 responses via toll-like receptor 2 activation in the intestinal mucosa. Infect Immun. 2012;80(12):4398–4408. doi:10.1128/IAI.06224-11
18. Taku K, Fumio I, Motonari K. The role of IL-17 and related cytokines in inflammatory autoimmune diseases. Mediators Inflamm. 2017;20. Epub 2017, Februaty 20. doi:10.1155/2017/3908061
19. Maria V, Manuela R. Cytokines IL-17 and IL-22 in the host response to infection. Pathog Dis. 2016;74(9):ftw111. doi:10.1093/femspd/ftw111
20. Shionoya S. Diagnostic criteria of Buerger’s disease. Int J Cardiol. 1998;66(Suppl.1):13. doi:10.1016/S0167-5273(98)00175-2
21. World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Wordld Health organisation; 2011. Available form: https://apps.who.int/iris/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf. Accessed August 8, 2019.
22. Rosenthal EA, Makaryan V, Burt AA, et al. Association between absolute neutrophil count and variation at TCIRG1: the NHLBI exome sequencing project. Genet Epidemiol. 2016;40(6):470–474. doi:10.1002/gepi.21976
23. Fazeli B, Dadgar Moghadam M, Niroumand S. How to treat a patient with thobliterans: a systematic review. Ann Vasc Surg. 2018;49:219–228. doi:10.1016/j.avsg.2017.10.022
24. Weyand CM, Goronzy JJ. Immune mechanisms in medium and large vessel vasculitis. Nat Rev Rheumatol. 2013;9(12):731–740. doi:10.1038/nrrheum.2013.161
25. Fernandes JR, Berthoud TK, Kumar A, Angel JB. IL-23 signaling in Th17 cells is inhibited by HIV infection and is not restored by HAART: implications for persistent immune activation. PLoS ONE. 2017;12(11):e0186823. doi:10.1371/journal.pone.0186823
26. Kagami S, Rizzo HL, Kurtz SE, Miller LS, Blauvelt A. IL-23 and IL-17A, but not IL-12 and IL-22, are required for optimal skin host defense against Candida albicans. J Immunol. 2010;185(9):5453–5462. doi:10.4049/jimmunol.1001153
27. Qu N, Xu M, Mizoguchi I, et al. Pivotal roles of T-helper 17-related cytokines, IL-17, IL-22, and IL-23, in inflammatory diseases. Clin Dev Immunol. 2013;2013. Epub 2013, July 14. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3728507/pdf/CDI2013-968549.pdf
28. Sano T, Huang W, Hall JA, et al. An IL-23R/IL-22 circuit regulates epithelial serum amyloid A to promote local effector Th17 responses. Cell. 2015;163(2):381–393. doi:10.1016/j.cell.2015.08.061
29. Schön MP, Erpenbeck L. The interleukin-23/interleukin-17 axis links adaptive and innate immunity in psoriasis. Front Immunol. 2018;9(JUN):1–13. doi:10.3389/fimmu.2018.01323
30. Yang J, Zhang R, Lu G, et al. T cell-derived inducible nitric oxide synthase switches off T H 17 cell differentiation. J Exp Med. 2013;210(7):1447–1462.
31. Nogueira E, Hamour S, Sawant D, et al. Serum IL-17 and IL-23 levels and autoantigen-specific Th17 cells are elevated in patients with ANCA-associated vasculitis. Nephrol Dial Transplant. 2010;25(7):2209–2217. doi:10.1093/ndt/gfp783
32. Abdulahad WH, Lamprecht P, Kallenberg CGM. T-helper cells as new players in ANCA-associated vasculitides. Arthritis Res Ther. 2011;13(4):236. doi:10.1186/ar3362
33. McGeachy MJ, Cua DJ, Gaffen SL. The IL-17 family of cytokines in health and disease. Immunity. 2019;50(4):892–906. doi:10.1016/j.immuni.2019.03.021
34. Blake SJ, Teng MWL. Role of IL-17 and IL-22 in autoimmunity and cancer. Actas Dermosifiliogr. 2014;105(Supl1):41–50. doi:10.1016/S0001-7310(14)70017-1
35. Jia L, Wu C. The biology and functions of Th22 cells. Adv Exp Med Biol. 2014;841:209–230. doi:10.1007/978-94-017-9487-9_8
36. Schreiber F, Arasteh JM, Lawley TD. Pathogen resistance mediated by IL-22 signaling at the epithelial–microbiota interface. J Mol Biol. 2015;427(23):3676–3682. doi:10.1016/j.jmb.2015.10.013
37. Zenewicz LA, Zenewicz LA. IL-22?: there Is a gap in our knowledge IL-22?: there is a gap in our knowledge. J Immunol. 2019;2(6):198–207.
38. Kolumam G, Wu X, Lee WP, et al. IL-22R ligands IL-20, IL-22, and IL-24 promote wound healing in diabetic db/db mice. PLoS ONE. 2017;12(1):e0170639. doi:10.1371/journal.pone.0170639
39. Louis S, Dutertre CA, Vimeux L, et al. IL-23 and IL-12p70 production by monocytes and dendritic cells in primary HIV-1 infection. J Leukoc Biol. 2010;87(4):645–653. doi:10.1189/jlb.1009684
40. Smith CL, Arvedson TL, Cooke KS, et al. IL-22 regulates iron availability in vivo through the induction of hepcidin. J Immunol. 2013;191(4):1845–1855. doi:10.4049/jimmunol.1202716
41. Sangkhae V, Nemeth E. Regulation of the iron homeostatic hormone hepcidin. Adv Nutr. 2017;8(1):126–136. doi:10.3945/an.116.013961
42. Moyat M, Bouzourene H, Ouyang W, et al. antimicrobial peptides are key determinants of mucosal vaccine-induced protection against H. pylori in mice. Mucosal Immunol. 2017;10(1):271–281. doi:10.1038/mi.2016.38
43. Valeri M, Raffatellu M. Cytokines IL-17 and IL-22 in the host response to infection. Pathog Dis. 2016;74(9):ftw111. doi:10.1093/femspd/ftw111
44. Hu S, He W, Du X, et al. Production of neutrophils enhances antibacteria ability but promotes arthritis development during mycobacterium tuberculosis infection. EBioMedicine. 2017;23:88–99. doi:10.1016/j.ebiom.2017.08.001
45. Ye X, Zhang L, Wang H, Chen Y, Zhang W, Zhu R. The role of IL-23/Th17 pathway in patients with primary immune thrombocytopenia. PLoS ONE. 2015;10(1):e0117704. doi:10.1371/journal.pone.0117704
46. Chyuan I, Chen J. Review article role of interleukin- (IL-) 17 in the pathogenesis and targeted therapies in spondyloarthropathies. Mediators Inflamm. 2018;2018:2403935. doi:10.1155/2018/2403935
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.