Back to Journals » Patient Preference and Adherence » Volume 11
Assessment of quality of life, satisfaction with anticoagulation therapy, and adherence to treatment in patients receiving long-course vitamin K antagonists or direct oral anticoagulants for venous thromboembolism
Authors Keita I , Aubin-Auger I, Lalanne C, Aubert JP, Chassany O , Duracinsky M , Mahé I
Received 27 December 2016
Accepted for publication 7 March 2017
Published 25 September 2017 Volume 2017:11 Pages 1625—1634
DOI https://doi.org/10.2147/PPA.S131157
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Ingre Keita,1 Isabelle Aubin-Auger,2–4 Christophe Lalanne,4 Jean-Pierre Aubert,2–4 Olivier Chassany,2,4 Martin Duracinsky,4 Isabelle Mahé1,2,4
1Internal Medicine Department, Louis Mourier Hospital, APHP, Colombes, 2Paris 7 University, 3General Medicine Department, Université Paris 7, Paris, 4Recherche Clinique Ville-Hôpital, Méthodologies et Société (REMES) EA 7334, Université Paris Diderot, Sorbonne Paris Cité, Paris, France
Introduction: Direct oral anticoagulants (DOACs) have shown non-inferiority and ease of use compared to vitamin K antagonists (VKA) in the treatment of venous thromboembolism (VTE). No study so far has been directed toward real-life experience of outpatients receiving anticoagulants for VTE in France.
Methods: This is an observational descriptive real-life epidemiological study, using three validated questionnaires (Morisky Medication Adherence Scale-8, EQ-5D, and part 2 of the Perception of Anticoagulant Treatment Questionnaire), to assess adherence, quality of life, and satisfaction in 100 VTE outpatients receiving anticoagulation therapy by VKA (primary or switched from DOAC to VKA) or by DOAC (primary or switched from VKA to DOAC).
Results: Patients were very much satisfied with their treatment in both DOAC and VKA groups. Despite advantages of DOACs, therapeutic adherence was only moderate. The best adherence scores were observed in the primary VKA switched to DOAC for at least 3 months (S-DOAC) subgroup. Quality of life was better in the DOAC group mainly because of the absence of the requirement for blood testing. Most of the complaints concerned the pain/discomfort dimension in the VKA group and anxiety/depression dimension in the DOAC group.
Conclusion: Patients were satisfied with their anticoagulant treatment, especially when they were involved in choosing the anticoagulant, and the treatment suited them. Quality of life of patients in the DOAC group was better than in the VKA group, but adherence remains to be improved. This study highlights the importance of the physician–patient relationship, pretreatment initiation, and follow-up of any anticoagulation therapy throughout.
Keywords: medication adherence, oral anticoagulant, deep venous thrombosis, pulmonary embolism, quality of life, treatment satisfaction
Introduction
Venous thromboembolism (VTE) includes deep venous thrombosis (DVT), generally affecting the lower limbs, and pulmonary embolism (PE), which is the most severe complication. In all, >70% of PEs are due to DVT.1 VTE is frequent (annual incidence, 1–2/1,000) and serious;2–6 mortality in France is 7.2/100,0004 and increases with age.7
VTE (proximal DVT and stable PE) is essentially managed on an outpatient basis or by following short hospital admission.8–10 The objective is to reduce immediate morbidity and mortality and then to reduce the risk of recurrence. Since the mid-20th century, the gold standard long-course oral treatment used vitamin K antagonists (VKA), but a new class of direct oral anticoagulants (DOACs) was developed to avoid certain pitfalls: narrow therapeutic window, wide intersubject variation, and fluctuating international normalized ratio (INR) due to interaction with drugs and food.
Two DOACs are presently available in VTE:11–13 rivaroxaban (Xarelto®) and apixaban (Eliquis®), having demonstrated non-inferiority to VKA in the treatment and prevention of recurrence of symptomatic VTE, with comparable rates of major and minor bleeding.6,8,14 DOACs have theoretic advantages over VKA in terms of ease of use for both patient and physician: fixed dosage, short active life, no requirement for biological surveillance, low drug and food interaction, and wide therapeutic window. Qualitative studies of patients from clinical trials with acute symptomatic DVT showed overall satisfaction15–17 that was comparable11,16,18–20 or better with DOAC than VKA.12,15
VTE (stable PE and DVT) is managed on an outpatient basis,8,10 but trials were all conducted in hospital settings. It seems important to assess patients’ everyday experience, as conditions differ between therapeutic trials and “real life.” There have been no real-life assessments of oral anticoagulation therapy in VTE. Therefore, the present study sought to assess the everyday experience of outpatients receiving VKA or DOAC for VTE on 3 complementary parameters (quality of life, treatment satisfaction, and adherence) assessed on 3 respective questionnaires with validated French language versions:21–23 Euroqol EQ-5D (measuring the impact of choice of anticoagulant: VKA or DOAC),21,22 part 2 of the Perception of Anticoagulant Treatment Questionnaire (PACT-Q2),23–25 and Morisky Medication Adherence Scale-8 (MMAS-8).22,26–28 These parameters were chosen as being complementary and determining in curative treatment and recurrence prevention in VTE: treatment satisfaction is essential to adherence, which in turn improves quality of life.29,30
Patients and methods
This is a quantitative descriptive observational study including VTE outpatients, aged ≥18 years, speaking and understanding French, and receiving anticoagulation therapy by VKA or DOAC for at least 3 months, between July 2014 and July 2015. Non-French speakers and patients with cognitive or neuropsychiatric disorder or declining to participate were excluded.
Objectives
The main objective of this study was to assess the experience of VTE patients receiving DOAC or VKA for at least 3 months, on 3 complementary parameters: quality of life, treatment satisfaction, and adherence. These were assessed on 3 anticoagulant validated questionnaires:17,24,31 EQ-5D measuring quality of life (EuroQol), PACT-Q2 measuring satisfaction with anticoagulation therapy (Prins), and MMAS-8 measuring adherence (Morisky).
Secondary objectives comprised comparison of quality of life, satisfaction, and adherence between patients receiving DOAC versus VKA and between those treated for <6 versus >6 months, and assessment of factors affecting ease of use of DOAC, quality of life, satisfaction, and adherence between patients receiving DOAC without prior VKA and patients switched from VKA to DOAC.
Patient selection and inclusion
Patients receiving oral anticoagulants for VTE were recruited from general community medicine offices in the Paris region of France (Ile de France), and hospital and outpatient vascular medicine department consultations. The physicians in charge of the patients (as specified in the medical files) were contacted and informed of the study and provided a list of consecutive patients receiving DOAC or VKA for VTE. Patients were informed of the study and provided oral consent before completing the questionnaires over the telephone.
Patient groups
Choice of treatment was decided by the patients’ physicians, and the patients were distributed between 2 groups accordingly: VKA, with primary VKA for at least 3 months, and no prior DOAC (P-VKA subgroup) or with primary DOAC switched to VKA for at least 3 months (S-VKA subgroup); and DOAC, with primary DOAC for at least 3 months, and no prior VKA (P-DOAC) or with primary VKA switched to DOAC for at least 3 months (S-DOAC). Balance was determined from the last INR recorded.
Within each group, 2 subgroups were distinguished: patients under anticoagulation for <6 and for >6 months.
Questionnaires
Questionnaire administration was tried out in 5 patients (not included in the analysis) to check patient understanding and the clarity of the investigator.
Quality of life was assessed on the EuroQol EQ-5D, a generic questionnaire measuring health-related quality of life in 5 domains (mobility, autonomy, usual activities, pain/discomfort, and anxiety/depression) with responses on 3 levels per item. It was completed by a subjective quality of life score, from 0 to 100, generally using a visual analog scale (VAS); as this was not possible by telephone, the patient was asked “How would you rate your health today, from 0 to 100, where 0 is the worst imaginable state of health and 100 the best?”
Treatment satisfaction was assessed on a questionnaire specific to anticoagulation therapy, PACT-Q2, which explores 3 domains: practical aspects (11 items), burden of disease and treatment (2 items), and anticoagulation treatment satisfaction (7 items), with 5 response levels on each, giving rise to a total score and 3 sub scores (practical aspects, satisfaction, and adherence).
For the convenience score (parts B + C), all the elements are inverted (score on B1–B11 and C1 + C2 =6, minus initial score) and then summed. For the satisfaction score (part D), the elements are simply summed.
The two scores were summed and recalibrated on a scale from 0 to 100 by summing the scores on the 3 parts (B, C, and D) and applying the following formula: SCORE =100×(score-20)/80.21,24
PACT-Q2 question B5 (difficulty avoiding certain foods while undergoing an anticoagulant treatment) was not suited to DOACs, which show little food interaction compared with VKA, and, for patients receiving DOAC, it was replaced by “Is it difficult for you to take your tablet during meals, as recommended?” Concomitant feeding increases the absorption of DOACs, and especially rivaroxaban, which is the most common, and therefore, it is recommended to take the drug during a meal.
Adherence to treatment was assessed on MMAS-8, a recent version of the 4-item Morisky scale originally intended to assess adherence to antihypertension treatment and more recently used to assess adherence to VKA therapy.26–28,31 It comprises 8 items: 7 yes/no questions and 1 with a Likert scale. The total score (out of 8) is interpreted as 8= high adherence, 6−<8 moderate adherence, and <6= low adherence.
Data collection
Data were collected over telephone by a single investigating physician, and rendered anonymous. The investigator was trained in the use of the tool and had performed many interviews before starting the study in getting good standardized qualitative data. They were recorded on standardized, strictly confidential, forms, numbered 1–100, and entered on Excel for analysis. Data comprised age, gender, diagnosis (DVT and/or PE), type of oral anticoagulant (DOAC, or VKA with last INR), anticoagulation treatment duration (≥6 or <6 months), any switch (and reasons for switching), and quality of life, satisfaction, and adherence scores.
The study protocol (2016/45NI) received institutional review board approval (CPP Ile de France IV, n° IRB 00003835) as a noninterventional study.
Analyses
Statistical methods
For each variable, a descriptive numerical summary was provided, comprising, for continuous variables, the mean value and 2 measures of scatter (standard deviation, and the interquartile range including 50% of observations) and, for categorical variables, number and percentage. The DOAC and VKA arms were compared on nonparametric Wilcoxon test for continuous variables and Pearson’s χ2 test for categorical variables. Associations between continuous variables were assessed on Spearman rank correlation coefficient. First-order risk threshold was set at 5%. Analyses used R 3.2.3 software.
Required sample size was calculated for an expected 12-point difference in means on the EQ-5D VAS (PACT-Q2 convenience scale, 6 points; satisfaction scale, 6 points) between two equal independent groups with identical standard deviations (20 and 10 points, respectively), for an expected effect size of 12/20=6/10=0.6. For a 5% error risk and 80% power, the total required sample size was 90 (45 subjects per group).
Quality of life, satisfaction, and adherence scores were recorded for each subgroup (P-VKA, S-VKA, P-DOAC, and S-DOAC), with comparison between groups (DOAC [P-DOAC + S-DOAC] vs VKA [P-VKA + S-VKA]) and between subgroups, and >6 months versus <6 months of treatment.
Results
Response rate
Between July 2014 and July 2015, 105 patients were contacted and asked to respond to the questionnaires. There was 1 refusal, 1 patient was unable to respond due to cognitive disorder, and 3 were lost to follow-up (Figure 1). Otherwise, all questionnaires were fully completed. Mean administration time was 11±4 min.
Patient characteristics
In all, 100 patients were included and distributed between 2 groups: VKA (n=50) and DOAC (n=50). Table 1 presents patient data. Mean age was 60.9 years, with a nonsignificant trend for greater age in the DOAC group (63.3 vs 56.6 years). VKA patients were more often treated in the community (46% vs 8%) and DOAC patients more often in hospital (94% vs 54%). Most patients (62%) had isolated DVT, 18% isolated PE, and 26% associated DVT and PE, without intergroup difference. All VKA patients were P-VKA, without prior DOAC, whereas 80% of DOAC patients were P-DOAC and 20% had switched from VKA (S-DOAC). Switching was the patient’s personal choice in 3 cases; other reasons comprised need for biological surveillance under VKA in 3 cases, or thrombophilia (protein S deficit in 2 cases, alopecia in 1, INR fluctuation in a psychiatric context in 1). Mean anticoagulation therapy duration was 27.6 months for VKA and 6.1 months for VKA; DOAC patients had longer treatment (70% >6 months) than VKA patients (40% >6 months). Disease progression and treatment duration were longer under VKA than DOAC (28 vs 6 months).
Quality of life
EQ-5D score by group
Table 2 presents the distribution of responses on the EQ-5D questionnaire, and Figure 2 presents the distribution of VAS scores as a histogram showing numbers and 20-point class interval, with “moderate” and “intense” responses grouped together. A significant intergroup difference can be seen on the pain scale, with VKA patients reporting negative experience more often than DOAC patients: 29/50 versus 18/50 “moderate” and “intense” responses. There was a nonsignificant difference in overall quality of life in favor of DOAC: 71±14 versus 65±14 (P=0.063). There were no sex differences on the various EQ-5D dimensions.
  | Figure 2 Quality of life scores (EQ-5D) in DOAC and VKA groups. |
Most patients in both groups (75%) reported no problems on 4 of the 5 dimensions of the questionnaire (mobility, autonomy, usual activities, anxiety/depression). More patients reported moderate or severe discomfort/pain in the VKA than in the DOAC group (48% vs 36% and 10% vs 0%, respectively): mainly pain due to sampling and puncture site hematoma, and anxiety.
Approximately 40% of patients in both groups reported problems on the discomfort/pain dimension: notably lower limb pain due to DVT or ulceration; 25% reported problems on the anxiety/depression dimension: fear of hemorrhagic accident.
EQ-5D score according to treatment duration
Overall, 80% of VKA patients treated for at least 6 months reported “no problems,” whereas 20%–25% reported problems on the discomfort/pain and anxiety/depression dimensions. Also, 80% of DOAC patients (P-DOAC + S-DOAC) treated for <6 months reported “no problems,” whereas 20% reported disease-related problems on the discomfort/pain dimension: edema and post-thrombotic syndrome.
Otherwise, 60%–65% of VKA patients treated for >6 months reported problems on the discomfort/pain dimension (pain due to sampling and puncture site hematoma) and anxiety/depression dimension (disease-related anxiety, fear of hemorrhage and of being outside the INR target range). Also, 25% of DOAC patients were anxious, notably regarding risk of hemorrhage and lack of antidote.
EQ-VAS score in the 2 groups
There was a nonsignificant trend toward better quality of life (EQ-VAS score) in the DOAC group (70.2 vs 60.7; P=0.063; Figure 3).
  | Figure 3 Scores on EQ-5D visual analog scale (EQ-VAS). |
Satisfaction
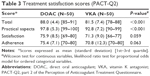
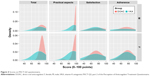
Satisfaction with treatment (PACT-Q2)
Table 3 and Figure 4 present PACT-Q2 data per group. In all, >90% of VKA and DOAC (P-DOAC + S-DOAC) patients were very much satisfied with the practical aspects of treatment, and 70% were very much satisfied overall. “Practical aspects” scores were significantly better in the DOAC group (97.8 vs 92.8; P<0.001), with a nonsignificant trend toward better satisfaction (75.9 vs 91.3; P=0.059). Both before and after 6 months treatment, P-VKA and DOAC (P-DOAC + S-DOAC) patients were very much satisfied with treatment, regarding both practical aspects and overall results.
Results were very good in S-DOAC patients, whether treated for <6 or >6 months: satisfaction with practical aspects, 100 and 97.5; overall satisfaction, 86.3 and 77.7, respectively.
Correlation between quality of life (EQ-5D) and satisfaction (PACT-Q2)
Nonparametric correlations (Spearman coefficient) between EQ-5D VAS score and the various PACT-Q2 scores were weak and systematically nonsignificant: practical aspects (0.013), satisfaction (0.045), and adherence (−0.030).
Stratifying correlation analysis by group revealed a difference in correlation between the practical aspects and quality of life: DOAC, r=−0.134 (P=0.354); VKA, r=0.006 (P=0.966). Likewise, for satisfaction and quality of life: DOAC, r=−0.103 (P=0.475); VKA, r=0.138 (P=0.338).
Adherence
Adherence to treatment (MMAS-8)
Mean MMAS-8 adherence score was 7.2 in the VKA group and 7.7 in the DOAC group (high adherence: 8, moderate: 6<8, low: <6).
Adherence was greater in the DOAC (P-DOAC + S-DOAC) group, especially before 6 months of treatment; scores were “moderate”: P-DOAC, 7.8; S-DOAC, 7.4. The rate of high adherence was 50% for S-DOAC, 67.5% for P-DOAC, and 50% for VKA. Women had better scores than men: 75.7±7.8 versus 70.9±11.5; P=0.019. There was no significant difference according to isolated DVT versus isolated PE (73.6±11.3 and 71.7±9.2, respectively; P=0.155).
Adherence seemed unrelated to treatment duration (r=0.010; P=0.918), quality of life on the EQ-5D VAS (r=−0.030; P=0.769), or practical aspects of DOAC or VKA treatment (r=−0.069 −0.080, respectively).
Discussion
DOACs were assessed in phase III trials in hospital patients. They were developed, however, to make anticoagulation therapy easier to implement on an outpatient basis than with VKA, improving patient comfort and simplifying follow-up for the physician. The present study assessed the patients’ real-life experience of DOAC and VKA on several parameters.
Overall, patients were very much satisfied with anticoagulation therapy, whether by DOAC or VKA, while adherence was moderate in both groups, as were overall quality of life scores (EQ-VAS).
Patients were real-life patients recruited consecutively from a list provided by general practitioners and vascular physicians. Therefore, they are representative of patients encountered in usual care. In addition, the study population was representative of typical VTE patients in France and Europe in terms of age, sex ratio, and DVT and PE rates: predominantly, middle-aged males with usually idiopathic DVT and/or PE. The results also agreed with French and European data.29,32
The high satisfaction with anticoagulation therapy confirms Willish’s findings for VTE patients under 6 months treatment by low molecular weight heparin (LMWH), LMWH + VKA, or DOAC assessed on the PACT-Q2 questionnaire in an international real-life observational study.25
The multicenter prospective XALIA study, comparing LMWH + VKA versus rivaroxaban in DVT, agreed with the present satisfaction and adherence results.29 In the EINSTEIN PE study,12,16 Prins showed that rivaroxaban provided better satisfaction than LMWH + VKA.
In the present study, the S-DOAC patients had chosen their anticoagulant, in agreement with their physician, and it was in this subgroup that scores were best: in 50% of cases, “practical aspect” scores were between 95 and 100, and better than in the P-DOAC or P-VKA subgroups.
Unlike satisfaction, which was high for both DOAC and VKA, adherence was moderate in both the groups, mainly due to repeatedly forgetting to take the drug. VKA was replaced by DOAC in 20% of cases after blood tests (reported in 50% of cases). Time within the INR target range could be used to assess compliance in VKA therapy, but has no equivalent in DOAC. As in the literature,30 54% of VKA patients had INRs of 2–3, 16% were overdosed, and 30% underdosed. There were more “highly adherent” patients in the DOAC than the VKA group (64% and 50%, respectively), but adherence was low in 14% of VKA patients and moderate in the DOAC group, whereas ease of use might have promised better adherence in the latter.
The absence of the requirement for blood testing and low food and drug interactions were not enough to promote adherence to DOAC therapy. Paradoxically, certain VKA patients were reassured by the necessary INR monitoring.
Qualitative studies and patient interviews identified several factors for poor adherence to long-course anticoagulation, notably by VKA: inconvenience of taking the drug and monitoring INR, loss of efficacy, perceived safety, and autonomy, anxiety related to side effects, quality of patient information provided by the physician and patient involvement in pretreatment decision making, failure of symptom reduction or prevention, and drug impact on activities.25,33 DOACs have useful advantages in patients poorly controlled by VKA, in whom they seem to improve adherence: anticoagulation is more stable (short half-life, no requirement for biological surveillance, and very low drug and food interaction).34 Treatment duration is another factor to be taken into account: the present study showed a tendency for adherence to diminish in both groups after 6 months. Castellucci reported a high inadequate adherence rate among patients on long-term oral anticoagulation, for both DOACs and VKA.35 Concerning the location of thromboembolism, poor prognosis for PE might have been expected to increase adherence, but in fact scores did not significantly differ between isolated PE and isolated DVT.
Quality of life is an abstract and subjective concept that is also progressive and relative. Perceived quality of life changes over time and space and varies between social groups. Although a single universal definition of quality of life is hard to imagine, the concept has become a new major concern in medical practice.
In the present study, overall quality of life scores (EQ-VAS) were moderate (~65/100) for both VKA and DOAC. This may partly be due to the negative impact of VTE on quality of life, physically (pain, dyspnea, reduced mobility) and psychologically (anxiety), aggravated by comorbidity.36,37
Quality of life as assessed on EQ-5D was better in the DOAC group, and especially the S-DOAC subgroup, mainly due to the lack of requirement for blood sampling, experienced as burdensome, lower frequency of consultations, and enhanced autonomy, with the patient taking charge of treatment.
In recent years, there has been increasing interest in the quality of life of patients under oral anticoagulation therapy, and increasing effort to improve it, with new questionnaires, specific studies of quality of life in anticoagulation, self-monitoring of INR, and telemedicine.
The main patient complaints in the present series concerned the anxiety/depression dimension (fear of dying and of recurrence and hemorrhage, which was mainly minor bleeding, and post-thrombotic syndrome) in DOAC patients, and the discomfort/pain dimension (puncture site pain, hematoma, stress when outside the target INR range) in VKA patients.
One hypothesis is that better treatment satisfaction improved adherence to treatment and hence quality of life. INR monitoring in VKA is anxiogenic due to sampling pain, while in DOAC there is fear of bleeding in case of overdose, with no antidote presently available, and of thrombosis in case of underdosing, and of disappointing the physician in case of poor results. These fears impair quality of life, especially in VKA when the INR is fluctuating, requiring increased blood sampling.36
In the present study, quality of life did not correlate significantly with satisfaction; however, in VKA patients, there seemed to be a trend for quality of life to correlate with satisfaction, especially regarding the practical aspects of treatment.
A randomized controlled study of 333 patients under anticoagulation therapy for atrial fibrillation with a minimum 2 years follow-up regularly assessed quality of life on validated scales measuring global function, well-being, and perceived health, to analyze factors affecting adherence and the impact of warfarin on quality of life; the impact was found to be negative.33,38 The authors stressed on the wide intersubject variation and the importance of involving the patient in choice of treatment after full information. In the present study, 7% of patients, 80% of whom were taking VKA, completely changed lifestyle out of fear of hemorrhage: 5 ceased sport, 1 ceased handiwork, and 1 ceased air travel.
Marvig assessed quality of life in patients with VTE and atrial fibrillation receiving coumarin anticoagulation therapy,17 immediately after diagnosis and at 3 months of treatment; quality of life improved after 3 months of treatment. The present results agree with this finding: quality of life scores were high, but treatment durations were not identical. Good quality of life may have been due to symptom relief thanks to treatment, and to the patient getting used to the treatment over time.
The present study had certain limitations. First, it was not randomized; however, only an observational study could enable real-life assessment of treatment satisfaction, adherence, and quality of life without altering the conditions of prescription and follow-up. To ensure a sample optimally representative of the French population, VTE patients under oral anticoagulation were recruited from areas within the Paris region of France (Ile de France). Second, the choice of questionnaires is open to question. Treatment satisfaction was assessed on PACT-Q2, whereas Marvig and Prins, respectively, used the Anti-Clot Treatment Scale and Treatment Satisfaction Questionnaire for Medication version II questionnaires,15,17 both comparing isolated rivaroxaban versus LMWH-VKA. This raises the question of whether variables are comparable when assessed on different scales. Quality of life after at least 3 months’ treatment was assessed on the EQ-5D questionnaire and on a verbal numeric scale instead of the original VAS (EQ-VAS), as data were collected over telephone. Third, the researcher performed clinical care and research at coercion but questionnaires are well structured, minimizing the risk of bias in getting the results. Fourth, there might be a bias linked to self-reporting of adherence through MMAS-8. But this questionnaire has been validated with this method. In addition, this study was performed in France, but one can expect the perception of anticoagulants in usual care to be the same across countries, which is a limitation of this study.
Patients receiving VKA and DOAC were satisfied with their treatment overall, especially when they were involved in choosing the anticoagulant, and the treatment suited them. There seemed to be little difference between VKA and DOAC in terms of quality of life, adherence, or satisfaction; but there was a greater rate of high adherence in patients receiving DOAC for <6 months, and the best scores were in the S-DOAC subgroup.
To improve quality of life, adherence, and satisfaction, the patient should be involved in choice of treatment. This requires information on the pros and cons of each anticoagulant before treatment initiation, and accompaniment throughout follow-up. These simple measures make the patient the main agent in his or her health, allowing him or her to make an informed choice of the treatment best-suited in terms of age, living conditions, occupation, comorbidity, and contraindications.
Acknowledgments
The MMAS (8-item) content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from Donald E. Morisky, ScD, ScM, MSPH, 14725 NE 20th St Bellevue, WA 98007, USA; [email protected].
Disclosure
The authors report no conflicts of interest in this work.
References
Kearon C. Natural history of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I22–I30. | ||
Anderson FA, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT study. Arch Intern Med. 1991;151(5):933–938. | ||
Spencer FA, Emery C, Lessard D, et al. The Worcester Venous Thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism. J Gen Intern Med. 2006;21:722–727. | ||
Oger E. Incidence of venous thromboembolism: a community-based study in Western France. EPI-GETBO Study Group. Groupe d’Etude de la Thrombose de Bretagne Occidentale. Thromb Haemost. 2000;83:657–660. | ||
Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379(9828):1835–1846. | ||
Hirschl M, Kundi M. New oral anticoagulants in the treatment of acute venous thromboembolism – a systematic review with indirect comparisons. Vasa. 2014;43(5):353–364. | ||
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ 3rd. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585–593. | ||
Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: Chest Guideline and Expert panel. Chest. 2016;149:315–352. | ||
Yeh CH, Gross PL, Weitz JI. Evolving use of new oral anticoagulants for treatment of venous thromboembolism. Blood. 2014;124(7):1020–1028. | ||
Konstantinides S, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014:35(43):3033–3069. | ||
The EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–2510. | ||
The EINSTEIN–PE Investigators, Buller HR, Prins MH, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366(14):1287–1297. | ||
Agnelli G, Buller HR, Cohen A, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369:799–808. | ||
Van Es N, Coppens M, Schulman S, Middeldorp S, Büller HR. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood. 2014;124(12):1968–1975. | ||
Marvig L, Wang MY, Prins MH, et al. Patient-reported treatment satisfaction with oral rivaroxaban versus standard therapy in the treatment of acute symptomatic deep vein thrombosis. Thromb Haemost. 2013;110(4):732–741. | ||
Prins MH, Marvig L, Cano SJ. Patient-reported treatment satisfaction with oral Rivaroxaban versus standard therapy in the treatment of pulmonary embolism; results from the EINSTEIN PE trial. Thromb Res. 2015;135(2):281–288. | ||
Marvig CL, Verhoef TI, de Boer A, et al. Quality of life in patients with venous thromboembolism and atrial fibrillation treated with coumarin anticoagulants. Thromb Res. 2015;136(1):69–75. | ||
Cano SJ, Lamping DL, Marvig L, et al. The anticlot treatment scale in clinical trials: cross cultural validation in venous thromboembolism patients. Health Qual Life Outcomes. 2012;10:120. | ||
Atkinson MJ, Kumar R, Cappelleri JC, Hass SL. Hierarchical construct validity of the treatment satisfaction questionnaire for medication (TSQM version II) among outpatient pharmacy consumers. Value Health. 2005;8:S9–S24. | ||
Dantas GC, Thompson BV, Manson JA, Tracy CS, Upshur RE. Patients’ perspectives on taking warfarin: qualitative study in family practice. BMC Fam Pract. 2004;5:15. | ||
Chevalier J, de Pouvourville G. Valuing EQ-5D using time trade-off in France. Eur J Health Econ. 2013;14:57–66. | ||
Korb-Salvadelli V, Gillaizeau F, Pouchot J, et al. Validation of a French version of the 8-item Morisky medication adherence scale in hypertensive adults. J Clin Hypertens. 2012;14:429–434. | ||
Prins MH, Marrel A, Carita P, et al. Multinational development of a questionnaire assessing patient satisfaction with anticoagulant treatment: the ‘Perception of Anticoagulant Treatment Questionnaire’ (PACT-Q). Health Qual Life Outcomes. 2009;7:9. | ||
Prins MH, Guillemin I, Gilet H, et al. Scoring and psychometric validation of the perception of anticoagulant treatment questionnaire (PACT-Q). Health Qual Life Outcomes. 2009;7:30. | ||
Willich SN, Bauersachs R, Gitt AK, et al. Treatment satisfaction in patients with venous thromboembolism as measured with Pact-Q2: prefer in VTE Registry. Value Health. 2014;17(7):A496–A497. | ||
Morisky DE, Ang A, Krousel-Wood M, Ward H. Predictive Validity of a Medication Adherence Measure in a Patient Setting. J Clin Hyper. 2008;10(5):348–354. | ||
Krousel-Wood MA, Islam T, Webber LS, Re RS, Morisky DE, Muntner P. New Medication Adherence Scale Versus Pharmacy Fill Rates in Seniors with Hypertension. Am J Manag Care. 2009;15(1):59–66. | ||
Morisky DE, DiMatteo MR. Improving the measurement of self-reported medication nonadherence: Final response. J Clin Epidem. 2011;64:258–263. | ||
Ageno W, Mantovani LG, Haas S, et al. Safety and effectiveness of oral rivaroxaban versus standard anticoagulation for the treatment of symptomatic deep-vein thrombosis (XALIA): an international, prospective, non-interventional study. Lancet Haematol. 2016;3(1):e12–e21. | ||
MacLean S, Mulla S, Akl EA, et al. Patient values and preferences in decision making for antithrombotic therapy: a systematic review: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e1S–e23S. | ||
Wang Y, Kong MC, Ko Y. Psychometric properties of the 8-item Morisky Medication Adherence Scale in patients taking warfarin. Thromb Haemost. 2012;108:789–795. | ||
Olié V, Fuhrman C, Chin F, Lamarche-Vadel A, Scarabin PY, de Peretti C. Time trends in pulmonary embolism mortality in France, 2000–2010. Thromb Res. 2015;135(2):334–338. | ||
Kneeland P, Fang MC. Current issues in patient adherence and persistence: focus on anticoagulants for the treatment and prevention of thromboembolism. Patient Prefer Adherence. 2010;4:51–60. | ||
Shehab A, Elnour AA, Bhagavathula AS, et al. Novel oral anticoagulants and the 73rd anniversary of historical Warfarin. J Saudi Heart Assoc. 2016;28(1):31–45. | ||
Castellucci LA, Shaw J, van der Salm K, et al. Self-reported adherence to anticoagulation and its determinants using the Morisky medication adherence scale. Thromb Res. 2015;136:727–731. | ||
Soliman Hamad MA, Van Eekelen E, van AgtT, van Straten AH. Self-management program improve anticoagulation control and quality of life: a prospective randomized study. Eur J Cardiothorac Surg. 2009;35(2):265–269. | ||
Lubberts B, Paulino Pereira NR, Kabrhel C, Kuter DJ, DiGiovanni CW. What is the effect of venous thromboembolism and related complications on patient reported health-related quality of life? A meta-analysis. Thromb Haem. 2016;116(3):417–431. | ||
Lancaster TR, Singer DE, Sheehan MA, et al. The impact of long-term warfarin therapy on quality of life. Evidence from a randomized trial. Boston Area Anticoagulation Trial for Atrial Fibrillation Investigators. Arch Intern Med. 1991;151(10):1944–1949. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.