Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 10
Assessment of quality of life in patients undergoing hemodialysis using WHOQOL-BREF questionnaire: a multicenter study
Authors Joshi U , Subedi R, Poudel P , Ghimire PR, Panta S, Sigdel MR
Received 9 March 2017
Accepted for publication 27 June 2017
Published 19 July 2017 Volume 2017:10 Pages 195—203
DOI https://doi.org/10.2147/IJNRD.S136522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Pravin Singhal
Utsav Joshi, Roshan Subedi, Prakash Poudel, Prajwol Ram Ghimire, Sagar Panta, Mahesh Raj Sigdel
Department of Internal Medicine, Tribhuvan University, Institute of Medicine, Maharajgunj, Kathmandu, Nepal
Background: Assessment of quality of life (QOL) of patients with end-stage renal disease has become increasingly important, both in order to evaluate the influence of the disease on patients and the type of renal replacement therapy they require. Therefore, in this study, we aimed to assess QOL in patients undergoing hemodialysis and evaluated the effects of various sociodemographic factors affecting QOL of such patients in Nepal.
Methods: A cross-sectional study was conducted among 150 patients with chronic kidney disease undergoing hemodialysis at two major centers in Nepal. Demographic data including age, sex, ethnicity, educational status, marital status, employment, income, duration of illness, and duration on hemodialysis were collected. QOL was assessed using the World Health Organization Quality of life (WHOQOL-BREF) questionnaire. Four domains (physical, psychological, social, and environmental) and two items (overall perception of QOL and health) of the WHOQOL‑BREF were the primary end points of this study. Bivariate relationship between sociodemographic factors and QOL scores were analyzed using independent samples t-test and one-way analysis of variance. Multiple linear regression analysis was performed to determine independent predictors of QOL.
Results: Following QOL scores were recorded: environmental domain (53.17±15.59), psychological domain (51.23±18.61), social domain (49.86±21.64), and physical domain (45.93±16.90). Older age was associated with a better QOL score in the social domain (p=0.005), and employed patients scored better in the environmental domain (p=0.019). Unemployed patients and those of the Terai/Madhesi ethnic group had significantly low scores in overall perception of health (p<0.05) as compared to other groups. Low income status and increased duration on hemodialysis were found to be the only independent negative predictors of QOL in patients with hemodialysis (p<0.05).
Conclusion: Patients with chronic kidney disease on dialysis had overall low QOL scores in all four domains. Age, ethnicity, employment status, income, and duration on hemodialysis affected one or more domains of QOL in such patients. Low income status and increased duration on hemodialysis were the only independent negative predictors of QOL of patients on maintenance hemodialysis.
Keywords: quality of life, hemodialysis, WHOQOL-BREF, chronic kidney disease
Introduction
Chronic kidney disease (CKD) is an important cause of morbidity and mortality worldwide. Individual, social, and economic consequences of CKD are enormous. According to 2013 Global Burden of Disease study, CKD accounted for 956,200 deaths worldwide, which was approximately 134% increase from that of 1990.1 A large number of screening programs conducted in countries with high per-capita income have demonstrated the prevalence of CKD in the general adult population to be in the range of 10–13%. Another study conducted across 12 countries, including Nepal, showed that the overall prevalence of CKD in Nepal was at 20.1%.2
The advent of renal replacement therapy (RRT) has significantly reduced morbidity, resulting in longer survival of patients with CKD.3 It has been estimated that over 1.1 million people are currently on MHD globally and this figure is increasing by 7% every year.4 In developing countries, such as Nepal, limited access to RRT, physical inaccessibility to health facilities, economic and cultural barriers with respect to transplantation, high prevalence of communicable diseases, and lack of infrastructure pose challenges in effective management of CKD.5 Patients with CKD on MHD have to bear significant physical, psychological, and economic challenges.6,7 Patients, along with their families, must change their lifestyles to adapt to the rigor and frequencies of hemodialysis sessions, which can be up to thrice a week. In addition, specific dietary regimens and associated health problems can adversely affect QOL of these patients. Thus, in patients with CKD on MHD, there is a considerable effect on functional state and QOL.8
QOL is an important parameter that needs to be addressed in chronic diseases like CKD. Unlike in the past, when the sole concern was to prolong survival of patients with CKD, equal importance is now being given toward maintenance of QOL.9,10 Several studies have shown that patients with CKD undergoing hemodialysis have a lower QOL than those undergoing peritoneal dialysis,11 those with renal transplantation,6,12 and the healthy individuals.13,14 Assessment of QOL of patients with CKD not only helps to assess the quality of dialysis program but also is useful to guide nephrologists to develop better interventions and plans of care for the future.15,16 Several studies, especially conducted in developed countries, have assessed QOL of patients with CKD and identified multiple factors influencing their QOL. However, to the best of our knowledge, only a few studies have been conducted to assess the QOL of patients with CKD in Nepal.4,17 Therefore, we performed a cross-sectional study of patients at two major dialysis centers in Kathmandu. We assessed QOL of patients undergoing hemodialysis with respect to physical, psychological, social, and environmental domains as outlined in the World Health Organization Quality of Life (WHOQOL-BREF) questionnaire. We also evaluated the effects of various sociodemographic factors on QOL of these patients.
Materials and methods
This is an observational, cross-sectional study conducted among patients with CKD undergoing MHD at two major centers in Kathmandu, Nepal (Bir Hospital, n1=30; National Kidney Center (NKC), n2=112). Data were collected at these centers for a total duration of 5 months from July to November of 2016. Ethical approval for the study was obtained from the Institutional Review Board of Bir Hospital and the hospital administration of NKC.
Consecutive patients who were able to understand, speak, or read Nepali language were selected by the method of non-probability sampling. We included patients who were at least 18 years of age and had been on regular MHD for at least 3 months. Patients with cognitive impairment and coexisting diseases such as stroke, chronic obstructive pulmonary diseases, heart diseases, and chronic liver diseases were excluded from the study as these factors could potentially affect their QOL and act as confounding factors.
Sociodemographic information including age, gender, marital status, education, employment, income, ethnicity, duration of illness, and duration on hemodialysis were collected using a structured questionnaire, and QOL was measured using WHOQOL-BREF questionnaire. Educated participants were encouraged to fill the questionnaire by themselves. However, for patients who were illiterate, questions were read out clearly by an investigator and their responses were noted. Written informed consent was obtained from all the participants (or their primary caretakers if applicable), after explaining the nature and purpose of the study. Out of a total of 250 patients evaluated initially, 150 patients met the inclusion criteria, of which 8 were excluded due to incomplete responses.
WHOQOL-BREF questionnaire consists of 26 items. Items 1 and 2 assess individual’s overall perception of QOL and health, respectively; the remaining items are categorized under physical, psychological, social, and environmental domains. Each item is rated by a 5-point Likert scale. The responses were scaled in a positive direction. The mean score of the items within each domain was used to calculate the raw score. Raw scores were then transformed to a 0–100 scale using a transformation formula.18 Higher score reflects a better QOL. WHOQOL-BREF questionnaire has been validated for assessing QOL in patients with CKD in different settings14 and has been used to assess QOL by a number of studies elsewhere.3,4,19 We used sociodemographic data as predictor variables and all four domains, including items 1 and 2, as outcome variables.
SPSS version 23.0 was used for the analysis of data. The normality of distribution of the collected data was evaluated using Shapiro–Wilk test and Q-Q plot. Cronbach’s alpha was used to assess reliability of the Nepalese version of WHOQOL-BREF. A value of 0.7 or more would indicate good internal consistency. The following typical values of Cronbach’s alpha for different domains were considered as reference: physical (0.80–0.84), psychological (0.75–0.77), social (0.66–0.69), and environmental (0.80).20 Results of descriptive analysis are presented as mean±SD. Pearson’s correlation coefficient was used to assess the inter domain correlation and the correlation between various demographic factors and domain scores. Bivariate relationship between sociodemographic factors and QOL scores was analyzed using t-test and one-way analysis of variance. Using Fisher’s least significant difference method, post hoc analysis was performed for variables with more than two groups, whenever a significant difference was established. Multiple linear regression analysis was performed to determine the independent predictors of QOL. A p-value <0.05 was considered to be statistically significant.
Results
Demographic characteristics of the respondents
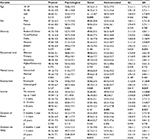
A total of 142 respondents were included in this study. Their mean age was 45.48 years (SD=15.31 years). Male to female ratio was 1.8:1. Among 142 patients on MHD, 29 (20.6%) were illiterate, 112 (78.9%) were married, and 120 (85.1%) were unemployed. Most of the respondents were of Brahmin or Chhetri caste under the traditional caste system. Annual family income was less than 500,000 NPR (1$ is equivalent to around 107 NPR) in the majority of the patients (75.8%). The demographic characteristics of the study population (n=142) are presented in Table 1.
  | Table 1 Characteristics of study population (n=142) |
QOL scores and correlations among various domains of WHOQOL-BREF
QOL scores in all domains except psychological domain showed normal distribution (i.e., p-values in Shapiro–Wilk test were <0.05). Although the p-value in Shapiro–Wilk test for psychological domain was >0.05, a graphical analysis of the data indicated consistency with a normal distribution. Cronbach’s alpha for all 26 questions of WHOQOL-BREF was acceptable (0.892). The following values of Cronbach’s alpha for individual domain were obtained: physical domain (0.720), psychological domain (0.744), social domain (0.568), and environmental domain (0.713). The low value of Cronbach’s alpha in social domain was expected as it was determined based on three scores only (i.e. personal relationships, social support, and sexual activity). In general, at least four scores are recommended in order to assess internal reliability; therefore, the value for social domain should be interpreted with caution.
The following QOL scores for various domains were obtained: environmental domain (53.17±15.59), psychological domain (51.23±18.61), social domain (49.86±21.64), and physical domain (45.93±16.90).
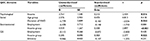
There were statistically significant correlations among all domains (p<0.05 in all cases). There were also statistically significant correlations between overall perception of QOL and general health and scores obtained from different domains (p<0.05 in all cases). Details of Pearson’s correlations among various domains are given in Table S1. Analysis of the strength of correlation among various domains showed moderate inter domain correlation between social and environmental domains (Pearson’s r>0.3 and <0.5) and strong inter domain correlation among rest of the domains (Pearson’s r>0.5).
Correlations between demographic characteristics and QOL
Correlations between the demographic characteristics and QOL scores in different domains are tabulated in Table S2. Significant negative correlation was observed between age and physical domain (Pearson’s r=0.177, p=0.035). Significant positive correlation was also observed between educational level and psychological domain (Pearson’s r=0.172, p=0.042); income and physical domain (Pearson’s r=0.197, p=0.028), income and social domain (Pearson’s r=0.248, p=0.010), and income and environmental domain (Pearson’s r=0.194, p=0.031); duration of illness and psychological domain (Pearson’s r=0.244, p=0.003); and duration of illness and environmental domains (Pearson’s r=0.226, p=0.007).
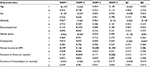
Sociodemographic characteristics and QOL scores
Table 2 shows the bivariate relationship between demographic characteristics and the domain scores. A statistically significant difference was observed between the scores of various age groups and social domain (p=0.005). Patients in the age group of ≥60 years had higher QOL scores in their social domain (61.11±18.70) than patients in both the age group of 18–34 years (53.19±21.32) and 35–60 years (44.65±21.26). Post hoc analysis showed that the greatest difference was between the age groups of 35–60 years and ≥60 years. We observed significantly lower scores in overall perception of general health (p=0.035) in Terai/Madhesi group than in other groups.
A significant difference was observed in the environmental domain (p=0.019) and overall perception of general health (p=0.039) based on the employment status of the patients. Employed patients had significantly higher QOL scores in the environmental domain (60.42±13.38) and overall perception of general health (3.10±0.83) than patients who were unemployed. Income was found to significantly affect QOL scores in the psychological domain (p=0.011), environmental domain (p=0.001), and overall perception of general health (p=0.037). Patients with an annual income of 5 lakhs to 10 lakhs NPR had higher QOL scores in psychological domain (64.95±17.06), environmental domain (62.32±15.64), and overall perception of general health (3.41±0.71).
Patients who were on MHD for more than 5 years scored significantly lower in the social domain than patients dialyzed for shorter duration (p=0.022). Using post hoc analysis, significant difference was found between the group with ≥5 years’ duration of MHD and other groups (3 months to 1 year and 1 year to 5 years).
Table 3 shows that income and duration on hemodialysis were independent predictors of QOL affecting one or more domains of WHOQOL-BREF. Duration on hemodialysis was found to be a significant negative predictor affecting the social domain (p=0.044) but not the other domains. Income was a significant positive predictor affecting the psychological domain (p=0.016), environmental domain (p<0.001), and overall perception of general health (p=0.025). We observed that variables such as age, ethnicity, and employment were not associated with any of the domains of WHOQOL-BREF in multivariate analysis. Age behaved as a confounding factor in social domain and employment was a confounding factor in environmental domain.
Discussion
CKD severely impacts QOL of patients with adverse effects observed in case of social, environmental, physical, and psychological domains. The gravity of the disease and its chronic nature make it important to pay due attention to the QOL of such individuals. QOL is emerging as an important outcome parameter to assess patients undergoing hemodialysis and monitor their progress and efficacy of disease management. This study demonstrates QOL in different domains, of patients with CKD undergoing MHD, and the factors responsible for such outcome.
Our findings indicate that older patients had significantly better QOL than younger patients in the social domain. Lemos et al also found social aspects to be better in older patients than younger patients.15 This could be attributed to the fact that older people may have a better understanding of the limitations of social life and so may be more satisfied with life despite the presence of the disease. Moreover, younger patients identify disease as a challenge and a loss, whereas older individuals regard it as less challenging and a part of life.21 Negative correlation between age and physical domain of QOL observed in this study is quite plausible given that with increasing age, there is a decrease in working capacity and mobility, and an increase in physical pain and discomfort which negatively affect physical health. However, a previous study did not report any significant relation between QOL score and age.10
Although employed individuals in this study scored better in every domain of QOL than those who were unemployed, the results were statistically significant only for the environmental domain and overall perception of general health. We observed better scores of “financial resources”, “accessibility and quality of health care”, and “opportunities for acquiring new information and skills” within the environmental domain in employed patients. This finding is consistent with that of Yang et al who showed significant improvement in the scores of the environmental domain with employment. Their study presented the higher scores as being due to the increased scores of “health care availability and quality” and “transportation” in the environmental domain.14 Employment significantly improved QOL scores in physical, psychological, and environmental domains in the study conducted by Sathvik et al.3
Income appears to be a novel predictor of QOL. Income was significantly associated with three domains of the WHOQOL-BREF: psychological domain, environmental domain, and overall perception of general health. Sathvik et al also reported higher QOL score among people with higher income, in all domains except social domain.3 This is not surprising because patients with higher income can easily afford better treatment and fulfill their needs. In addition, financial security would be expected to lead to better self-esteem, feeling of satisfaction, and less worry about the future, all of which result in better QOL. This may also be the reason for a positive correlation between income and physical, social, and environmental domains of QOL in our study. A similar pattern of QOL and its relation with income were also found in other studies.15,22
We observed a significantly lower QOL score in social domain in patients who had undergone dialysis for more than 5 years than patients dialyzed for shorter duration. Yang et al found similar results and correlated the low score in the social domain with dissatisfaction with sexual life and feeling less respected.14 Our study is also in congruence with the results reported by other studies.7,23 The low QOL score in the social domain may be due to the fact that with increase in the duration of dialysis, patients have less time and desire to spend with their families and friends which may negatively affect their personal and social relationships. In addition, patients who had been on dialysis for more than 5 years were least satisfied with their sexual life which might also have accounted for the poorer score in the social domain. In contrast, Atapour et al found no relation between duration on hemodialysis and QOL in patients with CKD.24
It is interesting to note that ethnicity affected the overall perception of general health in the patients undergoing hemodialysis. Terai/Madhesi ethnic group had lower scores in this dimension than other groups. Since the number of respondents from this ethnic group in our study was very small (2.1%), a bigger sample size is required before we can draw a definite conclusion from this. Studies comparing ethnicity and QOL score in patients on MHD have not been reported in Nepal.
A number of sociodemographic factors that seem to affect QOL in other studies have not been found to be significant predictors of QOL in this study. We did not observe any effect of gender on QOL of patients on MHD. This result is in line with studies by Saad et al and Gemmell et al. In both of these studies, the investigators found no significant difference in QOL scores between males and females.6,25 Nevertheless, several studies have reported a significant influence of gender on QOL. Sayin et al documented males to have worse QOL than females, whereas Valderrábano et al reported the opposite.8,26
While we expected education to affect QOL in patients with CKD, we did not come across any significant results. Our study is consistent with another study which found no significant differences when relating QOL with educational level.10 In contrast, according to Gerasimoula et al, participants with higher education had better QOL.7 Even though educated people have a better understanding of the disease and compliance, they were also likely to have higher expectations from health care facilities which might result in increased dissatisfaction that affects their psychological well-being. This might be the reason why educated patients did not score better in QOL assessment.
While many previous studies have indicated that married people have higher QOL,11 marital status did not affect QOL score in this study, a finding consistent with a study by Bayoumi et al.27 In Nepal, due to extended family structure, even unmarried people usually get adequate emotional and financial support from their families. This is in contrast to many other cultures, where support is most often linked to marriage.
Duration of illness had no effect on any domains of QOL. We posit that during the initial stages of CKD, patients often remain asymptomatic and they may not perceive significant effect on their QOL. As the disease progresses toward end-stage renal disease, requiring RRT, patients begin to feel decline in their QOL. With majority of the patients in this study being diagnosed with CKD for a duration of 5 years or less, it is highly probable that they did not experience the myriad of symptoms that the patients with this disease for a longer duration experience or those experiencing this illness in an advanced stage. This may account for the duration of illness having no effect on QOL in this study.
In bivariate analysis, age was significantly associated with the social domain and employment was found to have a significant association with the environmental domain. However, when these factors were considered together with income and duration on dialysis in multiple linear regression model, age and employment were found to be less significant. This suggests that income and duration on dialysis have a greater significance with respect to social and environmental domains than that of other factors included in analysis. Even though older patients had a better QOL than younger ones in bivariate analysis, the reason for the lack of significance in multivariate study may be due to the greater impact of duration on dialysis on the social domain. Younger patients in the age group of 18–34 years and 35–60 years had undergone dialysis for a longer duration than older patients aged ≥60 years. Hence, it might actually have been the shorter duration on dialysis, rather than the older age itself, that resulted in better QOL in the older population. Reason for the non-significant association between employment and environmental domain in the multivariate analysis may be due to the fact that only 24.2% of the employed individuals had an income of greater than 5 lakhs NPR and the vast majority of the employed patients were still earning less than 5 lakhs NPR. Since almost three quarters of our sample population had a lower income, this may have had a more significant impact on environmental domain than simply the status of their employment.
One of the major limitations of this study was that we did not evaluate the possible effect of biochemical parameters on QOL of patients with CKD. We also could not look into the effects of medications used on QOL and whether patients had twice a week versus thrice a week MHD. Majority of the QOL questionnaires were self-reported except in cases of illiterate patients where the questionnaires were conducted with the help of investigators. In these cases, reporting biases may have acted as confounding factor in our data. We also did not have a control group to make appropriate comparisons of the findings obtained from patients with CKD.
Despite the limitations, the findings of this study shed light on the status of QOL of Nepalese patients on MHD and might inspire the healthcare providers of social and nephrology unit to strive for betterment in dialysis care delivery in the future. The findings of this study could help doctors, medical professionals, and family members to better understand the physical and psychological problems of patients with CKD on MHD. This, in turn, allows personnel to provide physical, psychological, and social support to the affected patients. Better social support is necessary for young patients and patients on MHD for a longer duration. Unemployed and poorer patients, whose QOL is significantly affected by the accessibility and quality of health care, should be provided with free and easily accessible dialysis services. Better access to basic necessities and appropriate management of physical pain for such patients could play a vital role in enhancing physical health of the patients with end-stage renal disease.
Conclusion
Using WHOQOL-BREF questionnaire, we found that the sample population in this study, that is, patients with CKD on MHD, had overall low QOL scores: environmental domain (53.17±15.59), psychological domain (51.23±18.61), social domain (49.86±21.64), and physical domain (45.93±16.90). Age, ethnicity, employment status, income, and duration on hemodialysis were found to affect one or more domains of QOL in such patients. From this study, we can say that low income status and increased duration on hemodialysis were the only independent negative predictors of QOL of patients on MHD.
Acknowledgment
We would like to thank Bishwas Sharma, Vishakha Agrawal, Majel McGranahan, and Suman Acharya for their invaluable help in the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Naghavi M, Wang H, Lozano R, et al; GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. | ||
Ene-Iordache B, Perico N, Bikbov B, et al. Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health. 2016;4(5):e307–e319. | ||
Sathvik BS, Parthasarathi G, Narahari MG, Gurudev KC. An assessment of the quality of life in hemodialysis patients using the WHOQOL-BREF questionnaire. Indian J Nephrol. 2008;18(4):141–149. | ||
Sapkota A, Sedhain A, Rai MK. Quality of life of adult clients on renal replacement therapies in Nepal. J Ren Care. 2013;39(4):228–235. | ||
Wetmore JB, Collins AJ. Global challenges posed by the growth of end-stage renal disease. Ren Replace Ther. 2016;2(1):15. | ||
Saad MM, El Douaihy Y, Boumitri C, et al. Predictors of quality of life in patients with end-stage renal disease on hemodialysis. Int J Nephrol Renovasc Dis. 2015;8:119–123. | ||
Gerasimoula K, Lefkothea L, Maria L, Victoria A, Paraskevi T, Maria P. Quality of life in hemodialysis patients. Mater Sociomed. 2015;27(5):305–309. | ||
Valderrábano F, Jofre R, López-Gómez JM. Quality of life in end-stage renal disease patients. Am J Kidney Dis. 2001;38(3):443–464. | ||
Cukor D, Ver Halen N, Fruchter Y, Kimmel PL. Psychosocial issues in chronic kidney disease patients. Chronic Renal Disease. 2014:229–236. | ||
Ferreira RC, da Silva Filho CR. Quality of life of chronic renal patients on hemodialysis in Marília, SP, Brazil. J Bras Nefrol. 2011;33(2):129–135. | ||
Ogutmen B, Yildirim A, Sever MS, et al. Health-related quality of life after kidney transplantation in comparison intermittent hemodialysis, peritoneal dialysis, and normal controls. Transplant Proc. 2006;38(2):419–421. | ||
Fujisawa M, Ichikawa Y, Yoshiya K, et al. Assessment of health-related quality of life in renal transplant and hemodialysis patients using the SF-36 health survey. Urology. 2000;56(2):201–206. | ||
Anees M, Hameed F, Mumtaz A, Ibrahim M, Saeed Khan MN. Dialysis-related factors affecting quality of life in patients on hemodialysis. Iran J Kidney Dis. 2011;5(1):9–14. | ||
Yang SC, Kuo PW, Wang JD, Lin MI, Su S. Quality of life and its determinants of hemodialysis patients in Taiwan measured with WHOQOL-BREF (TW). Am J Kidney Dis. 2005;46(4):635–641. | ||
Lemos CF, Rodrigues MP, Veiga JR. Family income is associated with quality of life in patients with chronic kidney disease in the pre-dialysis phase: a cross sectional study. Health Qual Life Outcomes. 2015;13(1):202. | ||
Gorodetskaya I, Zenios S, McCulloch CE, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int. 2005;68(6):2801–2808. | ||
Shrestha S, Ghotekar LR, Sharma SK, Shangwa PM, Karki P. Assessment of quality of life in patients of end stage renal disease on different modalities of treatment. JNMA J Nepal Med Assoc. 2008;47(169):1–6. | ||
Saxena S, Carlson D, Billington R, Orley J. The WHO quality of life assessment instrument (WHOQOL-Bref): the importance of its items for cross-cultural research. Qual Life Res. 2001;10(8):711–21. | ||
Anees M, Malik MR, Abbasi T, Nasir Z, Hussain Y, Ibrahim M. Demographic factors affecting quality of life of hemodialysis patients – Lahore, Pakistan. Pak J Med Sci. 2014;30(5):1123–1127. | ||
World Health Organization. WHOQOL user manual: Programme on mental health. Geneva: World Health Organization; 1998 Available from:http://apps.who.int/iris/bitstream/10665/77932/1/WHO_HIS_HSI_Rev.2012.03_eng.pdf. Accessed July 7, 2017. | ||
Laudański K, Nowak Z, Niemczyk S. Age-related differences in the quality of life in end-stage renal disease in patients enrolled in hemodialysis or continuous peritoneal dialysis. Med Sci Monit. 2013;19:378–385. | ||
Rocco MV, Gassman JJ, Wang SR, Kaplan RM. Cross-sectional study of quality of life and symptoms in chronic renal disease patients: the Modification of Diet in Renal Disease Study. Am J Kidney Dis. 1997;29(6):888–896. | ||
Overbeck I, Bartels M, Decker O, Harms J, Hauss J, Fangmann J. Changes in quality of life after renal transplantation. Transplant Proc. 2005;37(3):1618–1621. | ||
Atapour A, Nasr S, Boroujeni AM, Taheri D, Dolatkhah S. A comparison of the quality of life of the patients undergoing hemodialysis versus peritoneal dialysis and its correlation to the quality of dialysis. Saudi J Kidney Dis Transpl. 2016;27(2):270–280. | ||
Gemmell LA, Terhorst L, Jhamb M, et al. Gender and racial differences in stress, coping, and health-related quality of life in chronic kidney disease. J Pain Symptom Manage. 2016;52(6):806–812. | ||
Sayin A, Mutluay R, Sindel S. Quality of life in hemodialysis, peritoneal dialysis, and transplantation patients. Transplant Proc. 2007;39(10):3047–3053. | ||
Bayoumi M, Al Harbi A, Al Suwaida A, Al Ghonaim M, Al Wakeel J, Mishkiry A. Predictors of quality of life in hemodialysis patients. Saudi J Kidney Dis Transpl. 2013;24(2):254–259. |
Supplementary materials
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.