Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 14
Assessment of Quality of Life and Supporting Structures in Implant Retained Mandibular Overdenture: A 5-Year Cohort Study
Authors Abd El Rahim NS , Ashour AA
Received 2 March 2022
Accepted for publication 1 June 2022
Published 10 June 2022 Volume 2022:14 Pages 171—182
DOI https://doi.org/10.2147/CCIDE.S364814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Neveen S Abd El Rahim,1,2 Asmaa A Ashour1
1Department of Removable Prosthodontics, Faculty of Dental Medicine for Girls, Al- Azhar University, Cairo, Egypt; 2Department of Removable Prosthodontics, College of Dentistry, Taibah University, Medina, Saudi Arabia
Correspondence: Asmaa A Ashour, Department of Removable Prosthodontics, Faculty of Dental Medicine for Girls, Al- Azhar University, Nasr City, Cairo, Egypt, Tel +201284048535, Email [email protected]
Aim: To assess oral health-related quality of life (OHRQoL), marginal bone loss (MBL), and changes in soft tissue including probing pocket depth and implant stability in 2 implants retained mandibular overdentures during 5 years follow-up periods.
Methods: Forty completely edentulous patients with age 51– 64 years were recruited for that longitudinal cohort study. Complete dentures were performed for all participants. Two implants (3.6 × 11.5 mm) were installed in the canine areas of the mandible. OHRQoL and MBL measures were performed every 1 year for 5 years, while clinical measures were made every 6 months for 60 months. Data were examined using repeated ANOVA and Friedman test.
Results: Thirty-seven patients had 74 implants; with mean age 56 ± 3.6 years; 43% females (n = 16) and 57% males (n = 21) accomplished the study. There were statistically significant differences in OHRQoL, MBL, and changes in soft tissue, including probing pocket depth and implant stability in 2 implants retained mandibular overdentures during 5 years follow-up periods, p ≤ 0.05.
Conclusion: Mandibular overdentures retained by 2 implants provide a positive long-term effect on OHRQoL, MBL, probing pocket depth, and implant stability.
Keywords: implant-retained overdenture, quality of life, marginal bone loss, pocket depth, COVID-19
Introduction
Dental implants are widely used to retain mandibular overdentures. Two implants that retained mandibular overdentures have been documented to be highly valuable in completely edentulous patients showing great patient delight, comfort, satisfaction, masticatory efficiency, achieving patients’ needs, and providing less complication compared with complete overdentures.1–3
Both functionality and longevity of implants have influenced implant-retained overdentures. Implant success is greatly affected by osseointegration. An adequate healing period following implant installation is needed to allow the osseointegration. Consequently, a delayed implant loading procedure was regularly accomplished; the mandibular overdenture should be connected to the implants at the 2nd phase following a 3–6 months healing period. Certainly, both the lack of micro-movements and the initial stability of the implant are considered important determinants in the success of the implant.4–6
The implant success is assessed in clinical guidelines including survival of the implant and supra-structure, loss of marginal bone, aesthetics, and complications. The general quality of life in many people is influenced by poor oral health, which represents an important factor in assessing the success of prosthetic treatment. The quality and type of prosthetic treatment, implants retained mandibular overdentures, can be assumed to be one feature of oral health.7,8
The oral health‐related quality of life (OHRQoL) is frequently utilized for the evaluation of implant retained prosthesis in edentulous patients. Quality of life greatly improves as the implant-retained prosthesis is delivered to the edentulous patients.9,10
The oral health impact profile for edentulous patients (OHIP-EDENT) is a 19-element questionnaire formed to estimate the OHRQoL with elderly or following missing teeth replacement. The OHIP-EDENT is a commonly utilized tool, considered principally described and demonstrated good reliability and validity.11,12
Marginal bone loss (MBL) around an implant is inevitable due to bone remodelling and crestal bone resorption after implant installation and prosthetic insertion. MBL around implant causes biological complications in the implant-abutment connection, which prompts tissue inflammation around the implant and the development of peri-implant diseases. Preservation of marginal bone represents a major role in the success and survival of dental implants, which keep peri-implant soft tissue healthy.13,14
Implant stability (IS) includes mechanical stability and biologic stability. The mechanical and biologic stabilities are established due to osseointegration and the healing period after the implant installation. Implant stability could be measured by several methods. Resonance frequency analysis (RFA) is the most popular procedure to estimate the implant stability quotient (ISQ). The RFA is an adequate, simple, non-invasive, practical, and well-documented procedure to estimate the stability of the dental implant.15–17
Pocket probing is an important and reliable diagnostic tool in the longitudinal assessment and detection of soft tissues around an implant. It is usually used to assess the interface between implant and tissue to detect areas of peri-implantitis and mucositis, thus leading to implant failure. The plastic periodontal probe has been recommended to be used safely during probing around implant restorations, and this procedure does not seem to jeopardize the integrity of oral implants.18,19
Since the end of 2019, the COVID-19 pandemic has been known for its adverse effects on nearly all aspects of daily life. Shortly after COVID-19 onset, it was considered a global pandemic. It was reported that the coronavirus can be transferred by aerosols through droplets of the respiratory system. Social distancing and isolation face masks, and strict personal hygiene methods have been announced as the principal protective methods for controlling the transmission of the coronavirus.20–22
Procedures during dental treatment have been recognized as one of the greatest threats to transmission of viruses, involving transmission through aerosol and non-aerosol methods. Therefore, it was advised that all dental approaches be suspended unless for emergency treatments, including acute dental pain, cellulitis or abscess, dental trauma, and osteitis. Therefore, all non-urgent treatments were postponed as regular maintenance visits and prosthetic treatment.23,24
This longitudinal cohort study was designed to evaluate OHRQoL, MBL, and changes in soft tissue, including probing pocket depth and implant stability in delayed loading 2 implants retained mandibular overdenture during 5 years follow-up periods.
The null hypotheses (H0) were no differences detected in OHRQoL, MBL, or changes in soft tissue including probing depth or implant stability in mandibular overdentures retained by 2 implants during 5 years follow-up periods.
Materials and Methods
Study Design
A longitudinal cohort study has been carried out between July 2015 and December 2020 at Removable Prosthodontics Department, Faculty of Dental Medicine for Girls, Al- Azhar University (Cairo, Egypt). It was conducted on forty completely edentulous patients, 23 males and 17 females, age 51 to 64 years. Power size calculation revealed a sample size of N = 30 for a power of more than 80% to detect a correlation at confidence interval 0.95 and alpha level 0.05; drop-out 10%.11,25 Patients were chosen following special inclusion and exclusion guidelines; good general health and free from any systemic or local diseases, bone disease, temporomandibular joint disorders, or neuromuscular disease. The selected patients had sufficient inter-arch space and Angle’s class I jaw relationship. They had well-developed residual upper and lower ridges with firm mucosa free from inflammation, ulceration, and flappy tissues. Smokers and patients performing abnormal tongue habits, bruxism, or clenching were precluded to avoid the adverse effects on the oral functions and musculatures. At least six months had elapsed from the last extracted teeth before implant placement. The treatment was accepted by all patients, and they have provided written accepted consent according to the declaration of Helsinki. This has been approved by the Ethics Committee of the University Institutional Review Board (No.AUFDREC/19-022).
Clinical Protocol
Preoperative panoramic radiograph and cone-beam computed tomography (CBCT) were made for all patients to examine bone height and conclude a preliminary idea about bone quantity and quality. Maxillary and mandibular complete dentures were delivered to all patients. Standard conventional laboratory and clinical techniques were followed during dentures construction. For adaptation, patients have been informed to utilize their complete dentures 3 months after delivery. CBCT was taken using a radiographic template to determine the availability of bone height and buccolingual width for implant placement. Quality of bone, especially at the expected sites of the implant, was determined and the position of the mental foramen was also detected. All patients have obtained two tapered, self-tapping, endosteal implants (3.6 × 11.5 mm) in the mandibular canine areas (Dayan Dental Engineering BV, Holland). Implants were installed by flapless surgical procedures and were kept submerged for three months for osseointegration. The implants were exposed after 3 months, and the cover screw of the implant was unthreaded and replaced by a healing collar. The fitting surface areas opposing the healing collars were relieved to accommodate the healing collars. After ten days the healing collars were replaced by ball and socket attachments (Dyna Dental Engineering BV, Holland). The fitting surface of the lower denture was relieved to adapt to the female housing of attachments; self-cured acrylic resin was placed in the relieved sites for the pick-up. The patient was instructed to bite lightly in centric occlusion until polymerization was completed. Patients have received 2 ball/socket attachments attached to 2 dental implants supported mandibular overdenture, Figure 1.
 |
Figure 1 Two dental implants at canine areas of the mandibular ridge. |
Follow-Up Appointment
Before follow-up appointments, many protocols need to be considered and integrated into a comprehensive and concise protocol. All patients were carefully assessed. If patients exhibit a fever of more than 37.5°C, symptoms such as cough, runny nose, phlegm, sore throat, muscle pain, shortness of breath, and a travel history within 2 weeks from regions or countries showed high risk or had new contact with a patient infected with COVID-19, they did not allow access. If asymptomatic patients evade screening, the extensive wearing of personal protective equipment should be accomplished. Face masks, goggles, gloves, disposable gowns, surgical scrubs, and clothing should be changed frequently, also patients’ companions were avoided as much as possible. Proper disinfection and sufficient room ventilation were achieved. For room disinfection, ethyl-alcohol (78%) is considered to be the most effective.26–28
OHRQoL, radiographic estimation, and clinical measures were done for all patients after implants loading. Patients used their dentures for 5 years as follow-up periods. OHRQoL and intraoral indirect digital periapical radiographs were made at loading and every 1 year for 5 years. Meanwhile, clinical measures were made at loading and every 6 months for 60 months as follows:
Measurement of (OHRQoL)
The OHIP-EDENT is used to measure OHRQoL. It comprises 7 items as (Appendix 1). 1: functional limitation; FL = 3 items, physical pain; P1 = 4 items, psychological discomfort; P2 = 2 items, physical disability; D1 = 3 items, psychological disability; D2 = 2 items, Social disability, D3 = 3 items, and handicap; H = 2 items. Patients replied by recording how their oral problems had affected their activities (0: never, 1: hardly ever, 2: occasionally, 3: fairly often, and 4: very often). The total OHIP-EDENT is the sum of patients’ replays to each item. The OHIP-EDENT is scored between 0 and 76; where 0 represented the maximum positive score (high quality of life) and 76 represented the worst score (low quality of life).29 The OHIP-EDENT was translated into Arabic by 2 translators. An Arabic version was introduced to each patient, who was interviewed by 2 different clinicians, and the clinician registered any problems that patients had demonstrated. After implant loading, patients were asked to complete a modified short Arabic version of OHIP-EDENT to assess OHRQoL in patients. A single clinician carried out the oral examination and denture bearing areas were determined at the end of the questionnaire. This was performed at every arranged follow-up appointment. The recorded data during the follow-up period were tabulated and statistically analyzed.
Radiographic Assessment
Intraoral Indirect Digital Radiographic Measurements
The radiographic template was constructed for each patient from auto-polymerized acrylic resin. Then, the template for radiographic evaluation was tried intraorally and checked for extension, stability, and fitting with the opposing occlusion. Assessment of mesial and distal bone heights for each implant was carried out at follow-up periods. The Orix x-ray machine (Orix-Aet, ARDET, S.V.R., Milano, Italy) was used for radiographic exposure at 65-kilovolt, 10-milliampere, for 0.4 seconds for the mandibular ridge to provide standardized radiographs. Exposure items were constant for all patients at the baseline and the follow-up intervals. The film holder with the mounted image plate was placed inside the prepared area of the radiographic template so that the central x-ray beam was perpendicular to the plate. Then, Digora’s computerized system, image processing software (Orion Corporation, Soredex Medical Systems, Helsinki, Finland), was used to calculate measurements of bone height. The exposed image plate was loaded into the scanner, which reads the image and converts it to digital form. After completion of the readout, the new read image was evaluated, re-took or enhanced, and/or finally saved on the previously prepared active patient card as needed. Images were exported in the Joint Photographic Experts Group (JPEG) file format. For each patient, information including the patient’s name, age, radiographic images, and other data was registered and saved in a specific card for the patient. The saved images of each patient were examined and analysed to study the changes in the amount of mesial and distal marginal bone levels. Image analysis measurements for MBL were performed. The implant shoulder and the crest alveolar bone were used as reference points. The extent between the 2 reference points, which represents the total marginal vertical loss of bone, was recorded mesially and distally. The extent from the apex of the implant to the shoulder of the implant was measured, which was then used to divide the original length of the implant from the finish line to the apex to calculate the magnification factor. The magnification factor was then multiplied by the measured distance mesially and distally of the implant to derive the actual distance of bone loss. This was performed at every arranged follow-up appointment. The recorded data during the follow-up period were tabulated and statistically analysed.
Clinical Evaluation
Probing Pocket Depth Measurement
Hawe Neos colour-coded (3/5/7/9 mm) plastic periodontal probe with flexible tip (Kerr, Lugano, Switzerland) specially designed for measuring pocket depth around implants was used. The probe was placed parallel to the implant’s long axis and kept in contact with the implant surface. The gap between the gingival margin and the tip of a plastic periodontal probe was recorded as probing pocket depth (PD). The PD measurements are recorded for 4 specific sites on each implant in the following sequence: facial, lingual, mesial, and distal. Only one reading per site is recorded. PD assessments were recorded to the closest full mm, recorded on a periodontal chart and become a permanent part of the patient chart. The average of right and left implant assessments for every patient was statistically analysed.
Implant Stability Measurement
Implant stability (IS) was estimated with the ISQ assessment scale and RFA. The assessment was carried out by Osstell ISQ (Osstell AB, Gothenburg – Sweden). ISQ values are (1–100). When the ISQ value increased, the stability of the implant increased. The following steps were achieved: Ball attachment was unscrewed and a smart peg specially supplied for the previously used implants (smart peg number 27) was attached to the abutment utilizing the smart peg mount. A finger-tight connection should be present, nearly 4–6 Ncm tightening torque. The hand of the assessment probe was held near the smart peg at a proximity-free gap to ensure that the probe tip was directed to the summit of the smart peg magnet. The smart peg was stimulated with the probe magnetic pulses. An audible sound was heard when the measurement was recorded. The value of ISQ appeared on the display. Two perpendicular measurements were achieved, the highest and the lowest ISQ values. Occasionally, two values of ISQ were very close, or even identical, if not, the mean of both values was used for statistical analysis. ISQ values were recorded for each patient, the smart peg was removed and the ball attachment was re-screwed. If at any of the mentioned visits, the ISQ fell to 45 or lower, the implant was considered a potential failure and placed under unloaded healing for 12 weeks before repeat stability testing. The average of right and left implant assessments for every patient was statistically analysed.
Statistical Analysis
SPSS 20 was used to analyse the computerized data. Shapiro–Wilk normality tests were carried out for constant variables and normally distributed data was disclosed. The mean value and standard deviation were used to represent the quantitative data. To clarify the significance of differences between the means of three or more groups in which the same patients presented in each group, repeated ANOVA test and Friedman test were used. Bonferroni tests were used for pairwise comparisons. The results were found to be significant at a p-value ≤0.05.
Results
Patients
Forty patients, who had 80 implants, were selected for this study. Three patients, one female and two males, discontinued the follow-up period. A male patient had a brain stroke after two years of implant loading and could not continue to follow-up periods, a male patient refused to continue the follow-up periods after one year, and a female patient died due to infection with Covid-19 after four years of the follow-up period. Eventually, thirty-seven patients had 74 implants; with mean age 56 ± 3.6 years; 43% females (n = 16) and 57% males (n = 21) accomplished the study.
Reported Outcomes During COVID-19
The follow-up period from July 2019 to July 2020, 5th year of follow-up, was completely missed. The complete lockdown was introduced during this period to increase social distancing and address the present world crisis. The 5th year follow-up period was postponed 6 months till the end of lockdown in December 2020.
Measurement of (OHRQoL)
The OHIP-EDENT included 7 items: FL, P1, P2, D1, D2, D3, and H, which were computed for all patients after implants loading and every 1 year for 5 years. The mean FL, P1, and P2 were “hardly ever (1)” at loading, after 1st, 2nd, and 3rd years then it became worse “occasionally (2)” after 4th and 5th years. There were statistically significant differences after 5 years follow-up periods on each of these subscales, p ≤ 0.05. The mean D1 and D2 were “hardly ever (1)” at loading, after 1st, 2nd, 3rd and 4th years then it became worse “occasionally (2)” after 5th years. There were statistically significant differences after 5 years follow-up periods on each of these subscales, p ≤ 0.05. The mean D3 and H were “never (0)” at loading, after 1st, 2nd, and 3rd years, then it became worse “hardly ever (1)” after 4th and 5th years. There were statistically significant differences after 5 years follow-up periods on each of these subscales, p ≤ 0.05. Regarding the mean of the total score of OHIP-EDENT, there were statistically significant differences after 5 years follow-up periods, p≤ 0.05, Table 1 and Figure 2.
 |
Table 1 The OHIP-EDENT During 5 Years Time Intervals |
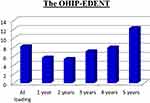 |
Figure 2 The total score of OHIP-EDENT during 5 years time intervals. |
Radiographic Measurements
The MBL was measured for all patients since implants loading and every 1 year for 5 years. The mean MBL for the mesial, distal, right, and left measurements was increased from 1st year till 5th year in patients who had delayed loading implant-retained mandibular overdenture; MBL.1y < MBL.2y < MBL.3y < MBL.4y < MBL.5y, Figure 3. There were statistically significant differences in MBL after 5 years follow-up periods, p ≤ 0.05, Table 2 and Figure 4.
 |
Table 2 Marginal Bone Loss (MBL) During 5 Years Time Intervals |
 |
Figure 3 Radiographic measurements for delayed loading implant MBL after a: 1 year, b: 2 years, c: 3 years, d: 4 years, and e: 5 years. |
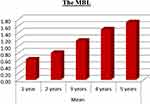 |
Figure 4 The mean of MBL during 5 years time intervals. |
Probing Pocket Depth Measurement
Changes in soft tissue including probing pocket depth and implant stability in delayed loading implant-retained mandibular overdenture were measured for all patients at loading and every 6 months for 60 months follow-up periods. The mean probing pocket depth (PD) was increased since loading and every 6 months for 60 months; PD.6m< PD.12m< PD.18m< PD.24m< PD.30m= PD.36m>PD.42m< PD.48m< PD.54m> PD.60m. There were statistically significant differences in probing pocket depth after 60 months follow-up periods, p ≤ 0.05, Table 3 and Figure 5.
 |
Table 3 Probing Pocket Depth and Implant Stability During 5 Years Time Intervals |
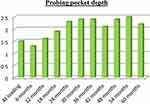 |
Figure 5 The mean of probing pocket depth during 60 months time intervals. |
Implant Stability Measurement
Implant stability (IS) was increased since loading and every 6 months for 60 months; IS.6m< IS.12m> IS.18m< IS.24m> IS.30m< IS.36m> IS.42m< IS.48m< IS.54m<IS.60m. There were statistically significant differences in implant stability after 60 months follow-up periods, p ≤ 0.05, Table 3 and Figure 6.
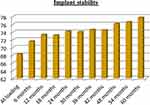 |
Figure 6 The mean of implant stability during 60 months time intervals. |
Discussion
That longitudinal cohort study was designed to evaluate OHRQoL, MBL, and changes in soft tissue including probing pocket depth and implant stability in delayed loading 2 implants retained mandibular overdenture during 5 years follow-up periods in COVID-19 pandemic.
The study was designed with standardized inclusion and exclusion criteria. Parameters that can affect the results of the study as; patients’ age, bone quantity, and quality, implant design, surgical procedures, and loading time were standardized in the study.
This study was caught during 2019–2020 as a follow-up period in the known clinical dilemma because of the Covid-19 pandemic. Even after that, there were fear and anxiety especially among the elderly patients who were reported as higher risk cases. During the ongoing pandemic situation, many extra precautionary measures were achieved, according to the updated guidelines, to avoid coronavirus transmission. These procedures such as checking body temperature, reducing exposure of the patients and period in the dental clinic, efficient surfaces’ cleaning with H2O, and 1% NaCl following every patient.27,28
Since installation and loading of implant, implants were survived and attained the success criteria for the accepted implant. All of the 74 implants survived in good function with healthy overlying soft tissues and without any signs of infection, mobility around the implants, or pain; the survival rate was 100%. There was not any persistent radiolucency around the mesial or distal sides of the implant as shown radiographically.
The implant survival rate from loading to 5 years follow-up period was 100%. This result was in agreement with a result found that; at 5‐years results of delayed loading implants in disparate designs, implants’ survival rate was 98.3–100%.30
In this longitudinal cohort study, a two-stage loading procedure of implant was escorted. It was revealed that delayed loading of an implant is correlated with high bone healing and is essential when there is less bone quality. Meanwhile, the results of another study revealed that delayed and immediate implant loading procedures provide the same results as implant-supported lower overdenture.14,31,32
Regarding the results of the current study, the first null hypothesis of no difference in OHRQoL in delayed loading implant-retained mandibular overdenture during 5 years follow-up periods was rejected. Statistically significant differences were noticed in the total scores of OHRQoL during 5 years of follow-up intervals. The OHRQoL improved from loading to 1st year then the treatment effect was stable overtime till 4th year than worsen in the 5th year of follow-up. These might be attributed to patients being informed to utilize their complete dentures 3 months after delivery for adaptation before implant installation and another 3 months after implant installation for osseointegration. At loading OHRQoL scores were worse as they were affected by complete dentures effects on the treatments than they improved after 1 year of loading as the presence of implants has improved mandibular overdentures stability, retention, and effectiveness. Then, the treatment effect was stable over time till the 4th year then worsens in the 5th year of follow-up. This might be due to, with time mandibular overdentures and maxillary complete dentures need maintenances as relining, rebasing, repair, and correction of occlusal problems which affected the scores of OHRQoL to worsen in the 5th year of follow-up. That was in accordance with the study which found that, 2 months after delivery of 2 implants retained lower overdenture and an upper complete denture, the patients expressed better oral function compared with those who had upper and lower complete dentures, also the implant group expressed better OHRQoL.11,33
The second null hypothesis of no difference in MBL in delayed loading implant-retained mandibular overdenture during 5 years follow-up periods was rejected. There were statistically significant differences in mean MBL during 5 years follow-up periods. The MBL was increased during 5 years follow-up periods. In this study, the mean MBL after 5th-year follow-up was (1.71±0.51mm). This was in agreement with 5 years results of a study; MBL in different types of implants in implant-retained overdenture was 0.69–1.74 mm. It was reported that MBL measurements were 1 mm or less after 1st year of implant delivery, which can be due to measurement’s limitations more than biological factors.6,14,34
The third null hypothesis of no difference in soft tissue condition including probing pocket depth or implant stability in delayed loading implant-retained mandibular overdenture during 5 years follow-up periods was rejected.
There were statistically significant differences in mean probing pocket depth during 5 years follow-up periods. The probing pocket depth was increased during 5 years follow-up periods. It was found that, in general, pocket depths around the implant should be ≤5 mm, and probing depths were increased from loading due to implantitis and mucositis around the implants. In this study, all pocket depths measured around the implants showed a pocket depth ≤4 mm. It was reported that peri-implant probing depths may be a poor diagnostic tool, if not associated with signs and/or symptoms, such as purulent exudate, bleeding, radiographic radiolucencies, discomfort, or pain. Accordingly, crestal bone loss over time is associated with increased probing depths, but there is no evidence of an endosteal implant disease.25,35,36
There were statistically significant differences in mean implant stability during 5 years follow-up periods. The implant stability was increased during 5 years follow-up periods. This was in agreement with a study which found that patients with insufficient quality of bone and extended length of the implant could obtain great primary stability of the implant. It was observed that after completion of osseointegration in 72 self-tapping implants there was a gradual increase in implant stability and ISQ values from surgery up to 5 years. Also, it was reported that the implant stability at the beginning changed due to bone compression created by mechanical factors such as bone relaxation, biological variations through bone recovery, and starting from resorption of crestal bone.14,16,36
Conclusion
Within the parameters of this study design, mandibular overdentures retained by 2 implants provide a positive long-term effect on OHRQoL, MBL, probing pocket depth, and implant stability.
Data Sharing Statement
Datasets related to this article will be available upon request to the corresponding author.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yao CJ, Cao C, Bornstein MM, Mattheos N. Patient-reported outcome measures of edentulous patients restored with implant-supported removable and fixed prostheses: a systematic review. Clin Oral Implants Res. 2018;29(S16):241–254. doi:10.1111/clr.13286
2. De Bruyn H, Raes S, Matthys C, Cosyn J. The current use of patient-centered/reported outcomes in implant dentistry: a systematic review. Clin Oral Implants Res. 2015;26(1):45–56. doi:10.1111/clr.12634
3. Hasegawa T, Kawabata S, Takeda D, et al. Survival of Brånemark System Mk III implants and analysis of risk factors associated with implant failure. Int J Oral Maxillofac Surg. 2017;46(2):267–273. doi:10.1016/j.ijom.2016.10.014
4. Sanz-Sánchez I, Sanz-Martín I, Figuero E, Sanz M. Clinical efficacy of immediate implant loading protocols compared to conventional loading depending on the type of the restoration: a systematic review. Clin Oral Implants Res. 2015;26(8):964–982. doi:10.1111/clr.12428
5. Liu W, Cai H, Zhang J, Wang J, Sui L. Effects of immediate and delayed loading protocols on marginal bone loss around implants in unsplinted mandibular implant-retained overdentures: a systematic review and meta-analysis. BMC Oral Health. 2021;21(1):1–15. doi:10.1186/s12903-021-01486-3
6. Pardal-Peláez B, Flores-Fraile J, Pardal-Refoyo JL, Montero J. Implant loss and crestal bone loss in immediate versus delayed load in edentulous mandibles: a systematic review and meta-analysis. J Prosthet Dent. 2021;125(3):437–444. doi:10.1016/j.prosdent.2020.01.032
7. Sánchez-Siles M, Ballester-Ferrandis JF, Salazar-Sánchez N, Gómez-García FJ, Moraleja-Ruiz R, Camacho-Alonso F. Long-term evaluation of quality of life and satisfaction between implant bar overdentures and conventional complete dentures: a 23 years retrospective study. Clin Implant Dent Relat Res. 2018;20(2):208–214. doi:10.1111/cid.12576
8. Da Cunha MC, Santos JF, Santos MB, Marchini L. Patients’ expectation before and satisfaction after full-arch fixed implant-prosthesis rehabilitation. J Oral Implantol. 2015;41(3):235–239. doi:10.1563/AAID-JOI-D-12-00134
9. Mifsud DP, Cortes ARG, Zarb MJ, Attard NJ. Maintenance and risk factors for fractures of overdentures using immediately loaded conventional diameter or mini implants with Locator abutments: a cohort study. Clin Implant Dent Relat Res. 2020;22(6):706–712. doi:10.1111/cid.12952
10. Abdou ELsyad M, Elgamal M, Mohammed Askar O, Youssef Al-Tonbary G. Patient satisfaction and oral health-related quality of life (OHRQoL) of conventional denture, fixed prosthesis and milled bar overdenture for all-on-4 implant rehabilitation. A Crossover Study Clin Oral Implants Res. 2019;30(11):1107–1117. doi:10.1111/clr.13524
11. Dellepiane E, Pera F, Zunino P, Mugno MG, Pesce P, Menini M. Oral health-related quality of life and full-arch immediate loading rehabilitation: an evaluation of preoperative, intermediate, and posttreatment assessments of patients using a modification of the OHIP questionnaire. J Oral Implantol. 2020;46(6):541–547. doi:10.1563/aaid-joi-D-19-00274
12. Fernández-Ruiz JA, Sánchez-Siles M, Guerrero-Sánchez Y, Pato-Mourelo J, Camacho-Alonso F. Evaluation of quality of life and satisfaction in patients with fixed prostheses on zygomatic implants compared with the all-on-four concept: a prospective randomized clinical study. Int J Environ Res Public Health. 2021;18(7):3426. doi:10.3390/ijerph18073426
13. Weerapong K, Sirimongkolwattana S, Sastraruji T, Khongkhunthian P. Comparative study of immediate loading on short dental implants and conventional dental implants in the posterior mandible: a randomized clinical trial. Int J Oral Maxillofac Implants. 2019;34(1):141–149. doi:10.11607/jomi.6732
14. Albertini M, Herrero-Climent F, Díaz-Castro CM, et al. A radiographic and clinical comparison of immediate vs. early loading (4 weeks) of implants with a new thermo-chemically treated surface: a randomized clinical trial. Int J Environ Res Public Health. 2021;18(3):1–19. doi:10.3390/ijerph18031223
15. Herrero-Climent M, Falcão A, López-Jarana P, Díaz-Castro CM, Ríos-Carrasco B, Ríos-Santos JV. In vitro comparative analysis of two resonance frequency measurement devices: Osstell implant stability coefficient and Penguin resonance frequency analysis. Clin Implant Dent Relat Res. 2019;21(6):1124–1131. doi:10.1111/cid.12868
16. Herrero-Climent M, López-Jarana P, Lemos BF, et al. Relevant design aspects to improve the stability of titanium dental implants. Materials. 2020;13(8):1–12. doi:10.3390/ma13081910
17. Delgado-Ruiz RA, Calvo-Guirado JL, Romanos GE. Effects of occlusal forces on the peri-implant-bone interface stability. Periodontol 2000. 2019;81(1):179–193. doi:10.1111/prd.12291
18. Coli P, Sennerby L. Is peri-implant probing causing over-DIAGNOSIS and over-treatment of dental implants? J Clin Med. 2019;8(8):1–13. doi:10.3390/jcm8081123
19. Werbelow L, Weiss M, Schramm A. Long-term follow-up of full-arch immediate implant-supported restorations in edentulous jaws: a clinical study. Int J Implant Dent. 2020;6(1). doi:10.1186/s40729-020-00232-8
20. Mandal AK, Paulami Dam OL, Franco HS, et al. Evaluation of quality of life and oral hygiene attitudes of individuals using dental prostheses during the COVID-19 pandemic. Ann Oncol. 2020:126;19–21.
21. Toro MD, Bremond-Gignac D, Brézin AP, et al. COVID-19 outbreak and increased risk of amblyopia and epidemic myopia: insights from EUROCOVCAT group. Eur J Ophthalmol. 2021;32(1):17–22. doi:10.1177/11206721211053175
22. Duvendack M, Sonne L. Responding to the multifaceted COVID-19 crisis: the case of Mumbai, India. Prog Dev Stud. 2021;21(4):361–379. doi:10.1177/14649934211030449
23. Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):1–5. doi:10.1038/s41368-020-0074-x
24. Chauhan N, Soni S, Jain U. Optimizing testing regimes for the detection of COVID-19 in children and older adults. Expert Rev Mol Diagn. 2021;1–18. doi:10.1080/14737159.2021.1962708
25. Salman A, Thacker S, Rubin S, Dhingra A, Ioannidou E, Pietro SG. Immediate versus delayed loading of mandibular implant-retained overdentures: a 60-month follow-up of a randomized clinical trial. J Clin Periodontol. 2019;46(8):863–871. doi:10.1111/jcpe.13153
26. Banakar M, Lankarani KB, Jafarpour D, Moayedi S, Banakar MH, MohammadSadeghi A. COVID-19 transmission risk in dentistry: a review and protective protocols. BMC Oral Health. 2020;20(275):1–12. doi:10.1186/s12903-020-01270-9
27. Kwak EJ, Kim J, Perinpanayagam H, Kum KY. Guidance for dental treatment of patients with disabilities during COVID-19 pandemic. J Dent Sci. 2021;16(1):540–543. doi:10.1016/j.jds.2020.08.003
28. Witton R, Plessas A, Wheat H, et al. The future of dentistry post-COVID-19: perspectives from urgent dental care centre staff in England. Br Dent J. 2021;1–5. doi:10.1038/s41415-021-3405-1
29. Bural C, Geckili O, Erdogan O, Bektas-kayhan K, Dayan SC. Reliability and validity of the Turkish version of oral health impact profile for edentulous subjects. Eur Oral Res. 2021;55(2):67–73. doi:10.26650/eor.20210007
30. Jonker BP, Gil A, Naenni N, Jung RE, Wolvius EB, Pijpe J. Soft tissue contour and radiographic evaluation of ridge preservation in early implant placement: a randomized controlled clinical trial. Clin Oral Implants Res. 2021;32(1):123–133. doi:10.1111/clr.13686
31. Bahammam MA, Fareed WM. Effect of immediate versus delayed loadings of dental implants on the oral health-related quality of life in Saudi population: experimental clinical trial. Saudi Med J. 2019;40(1):79–86. doi:10.15537/smj.2019.1.23370
32. Abdelaal M, Fayyad A, Sheta N, Abdelnabi N, Elfar MM. Oral health-related quality of life in single implant mandibular overdenture retained by CM LOC versus ball attachment: a randomized controlled trial. Open Access Maced J Med Sci. 2019;7(21):3642–3646. doi:10.3889/oamjms.2019.792
33. Anitua E, Fernandez-de-Retana S, Anitua B, Alkhraisat M. Long-term retrospective study of 3.0-mm-diameter implants supporting fixed multiple prostheses: immediate versus delayed implant loading. Int J Oral Maxillofac Implants. 2020;35(6):1229–1238. doi:10.11607/jomi.8180
34. Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol. 2018;89:S304–S312. doi:10.1002/JPER.17-0588
35. Yadav R, Verma U, Tiwari R, Article O. A comparative evaluation of immediate versus delayed loading of two implants with mandibular overdenture: an in vivo study. Natl J Maxillofac Surg. 2019;10(1):3–7. doi:10.4103/njms.NJMS_55_18
36. Carmen Díaz-Castro M, Falcao A, López-Jarana P, et al. Repeatability of the resonance frequency analysis values in implants with a new technology. Med Oral Patol Oral Y Cir Bucal. 2019;24(5):e636–e642.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
