Back to Journals » Patient Preference and Adherence » Volume 15
Assessment of Prescription Pattern of Systemic Steroidal Drugs in the Outpatient Department of Menelik II Referral Hospital, Addis Ababa, Ethiopia, 2019
Authors Wondmkun YT, Ayele AG
Received 6 October 2020
Accepted for publication 16 December 2020
Published 6 January 2021 Volume 2021:15 Pages 9—14
DOI https://doi.org/10.2147/PPA.S285064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Yohannes Tsegyie Wondmkun, Akeberegn Gorems Ayele
Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Yohannes Tsegyie Wondmkun
Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Sciences, Addis Ababa University, P.O. Box 1176, Addis Ababa, Ethiopia
Email [email protected]
Background: Because systemic corticosteroids are associated with severe adverse effects, a study on the prescribing pattern for rationalizing drug therapy is needed.
Objective: The purpose of this study was to assess the prescription pattern of systemic steroidal drugs at the outpatient department of Menelik II Referral Hospital, Addis Ababa, Ethiopia, 2019.
Methods: A cross-sectional study design was used to assess the prescription pattern of systemic steroidal drugs in the outpatient department of Menelik II Referral Hospital. A total of 384 patient charts were included in the study. The sample was selected by using a non-probability quota sampling method. The data was collected from patient charts by using a checklist and analyzed by using SPSS version 20 computer software package. Finally, the data was presented with tables, graphs and charts.
Results: A total of 384 patient medical charts were reviewed during the study period. From which, 61.2% were females and 22.4% were in the age group of 31– 40 years. The majority, 63.5%, of systemic corticosteroid use was indicated for respiratory disorders and the most frequently prescribed drug was prednisolone (42.4%). It was also found that intermediate acting corticosteroids (prednisolone and methyl prednisolone) were mostly prescribed during the study period.
Conclusion: In this study, most steroids were indicated for respiratory disorders and prednisolone was found to be the most widely prescribed medication among systemic steroids.
Keywords: prescribing pattern, systemic steroid, corticosteroid, prednisolone
Introduction
Steroids are among the most frequently prescribed drugs in the world because they are extremely effective for the relief of symptoms of many inflammatory and immune disorders and other conditions.1 Systemic steroids are synthetic forms of natural steroids, cortisol, developed by adrenal glands, which have powerful anti-inflammatory effects. Oral or parenteral systemic corticosteroids (e.g. dexamethasone, prednisolone, and methyl prednisolone) exhibit strong immunomodulatory, anti-inflammatory, and anticancer properties and are essential to the treatment of various disorders, including autoimmune disorder, allergic reactions, chronic obstructive pulmonary disease, asthma exacerbations, and in some selected malignancies2,3. Glucocorticoids (GCs) provide rapid relief within hours of treatment. Systemic treatment is started with large doses that are then tapered quickly and tapering is frequently part of treatment protocols to decrease the risk of relapse.4 Since GCs potently inhibit inflammation and are used in a number of inflammatory and autoimmune diseases, they are one of the most commonly prescribed drug categories. Because GCs affect almost every organ system, the therapeutic use and removal of corticosteroids is affected by a variety of severe adverse effects, some of which are life-threatening. Therefore, the decision to apply systemic corticosteroid therapy also requires careful consideration of relative risks and benefits for each patient, intra-articular GCs are useful if only a few joints are involved and septic arthritis is removed.5
The under-use of steroids results in a sub-therapeutic effect, while overdose of steroids, not considering the exact amount of steroids, results in different adverse effects. The pharmacists should also share responsibility for educating patients on the proper administration of systemic corticosteroids, the pace of administration, and so on. Patients should also consider the disease and its progression, the complications caused by insufficient treatment, and the use and abuse of drugs and their consequences.6
Drug use or drug use measurement trials are legitimate and structured quality assurance systems. These studies are designed to review medication usage and suggest medication trends with existing recommendations or guidelines for the treatment of a particular disease. Drug use is measured at the community level by age, sex, and social status. Daily audits of medications are required to improve clinical efficacy, minimize adverse effects, question prescribers and assess the application of medical care requirements. Inappropriate prescriptions are known worldwide as a main healthcare concern, particularly in developing countries.7,8 Since corticosteroids play a crucial role in the treatment of many diseases, including the skin, they are commonly prescribed by clinicians. According to World Health Organization figures, 50% of all drugs are wrongly prescribed, administered or sold, in particular, by GCS. These drugs are extensively administered due to their strong immunosuppressive and anti-inflammatory action. This activity has also contributed to over-prescription of these medications and, as a result, increased adverse drug reactions. Corticosteroids were developed in the early 1950s; since then, these drugs have been commonly used for different clinical conditions, requiring important caution in the selection of corticosteroid medications for use and their dosing schedule.9,10 Although drug prescription patterns are widely studied in Ethiopia,11,12 specific information is lacking for GCs in this regard. It is therefore essential to research the medication prescription pattern of systemic corticosteroids. Therefore, this study was aimed to assess prescription pattern of systemic steroid drugs at the outpatient department of Menelik II Referral Hospital, Addis Ababa, Ethiopia.
Methods
Study Area and Period
This study was conducted in Menelik II Referral Hospital, Addis Ababa, the capital city of Ethiopia and the headquarter of the African Union. Addis Ababa has 13 public hospitals, 32 private hospitals and 93 health centers. The study was conducted from April to June 2019 GC.
Study Design and Population
A cross-sectional study design was used to assess prescription patterns of systemic steroidal drugs at the outpatient department of Menelik II Referral Hospital. All patient medical charts with systemic steroidal drugs at the outpatient department of Menelik II Referral Hospital were included in the study.
Sample Size Determination and Sampling Techniques
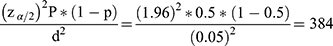
The sample size for the study was determined using single population proportion formula by assuming 95% confidence level, 5% marginal error, and 50% proportion of appropriate systemic steroidal prescription pattern.
Therefore, the sample size for the study was 384 patient medical charts with systemic steroidal prescriptions. Non-probability quota sampling method was used to select patient medical charts. Patient medical charts with systemic steroidal prescription were included in the study until the required sample size is reached (384 patient medical charts with systemic steroidal prescriptions).
Inclusion and Exclusion Criteria
Medical charts which contain systemic steroidal drugs were included in the study whereas, incomplete patient medical charts and those contain non-systemic steroidal drugs were excluded from the study.
Study Variables
The dependent variable was systemic steroidal prescription pattern while the independent variables were socio demographic characteristics (sex and age), indication, type of drug dose, route of administration, frequency and duration.
Data Collection Procedure
Data was collected by using a data abstraction checklist developed by the investigators. The data were collected by reviewing patient medical charts that contain systemic steroidal prescriptions.
Data Quality Management
To maintain the quality of the data only complete medical charts were included in the study. The collected data were checked for completeness and accuracy. After data entry, data cleaning was performed.
Data Analysis and Procedures
Data were entered and analyzed using SPSS version 20 statistical software. Frequencies and percentages were done to organize and summarize the data. Finally, the result was presented with tables, graphs and charts.
Ethical Consideration
Ethical clearance was obtained from Addis Ababa University, College of Health Sciences, School of Pharmacy institutional review board with a reference number of ERB/SOP/251/02/2019 and an official letter was written to Menelik II Referral Hospital to secure permission. Confidentiality and privacy of the data was ensured during the collection period. The patient’s name and address were not recorded on the data abstraction checklist and the collected information was used for research only. Moreover, the study was carried out in accordance with World Medical Association Declaration of Helsinki.13
Operational Definition
Adverse Drug Reaction
Unwanted or harmful reaction following administration of drugs.
Prescription Pattern
Are prescribing, dispensing and distribution of medicine.
Systemic Steroid
Is one of a group of chemical substances found in our body and made artificially and used for the treatment of various disease ailments.
Outpatient
A patient who is not hospitalized, but instead comes to a physician office, clinic, for treatment.
Results
Socio-Demographic Characteristics
In this study, from 384 assessed patient medical charts with steroids, the majority of them, 235 (61.2%), were female. The age group of 31–40 and <20 years accounted for the highest and the lowest number of patients respectively (Table 1).
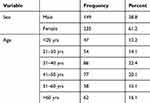 |
Table 1 Socio-Demographic Characteristics of Patients Receiving Systemic Corticosteroids, Menelik II Referral Hospital, Addis Ababa, Ethiopia, 2019 |
Common Indication of Systemic Corticosteroids
A total of 384 patient medical charts were analyzed in Menelik II Referral Hospital in the outpatient department. Out of this, respiratory disorders 244 (63.5%), meningitis 39 (10.2%) and rheumatoid arthritis 29 (7.6%) are the top three disease conditions in which corticosteroids are prescribed with the highest frequency (Table 2). On the other hand, stroke, deep vein thrombosis, lung and esophageal cancer represent conditions where corticosteroids are prescribed with the lowest frequency 1 (0.26%) (not shown on the table).
 |
Table 2 Common Indications of Systemic Corticosteroids at Menelik II Referral Hospital in Outpatient Department, Addis Ababa, Ethiopia, 2019 |
Patterns of Systemic Corticosteroid Use
From the total of 384 patient medical charts analyzed, prednisolone was the most frequently prescribed drug 163 (42.4%), followed by hydrocortisone 117 (30.5%), dexamethasone 92 (24.0%), beclometasone puff 10 (2.6%), and methyl prednisolone 2 (5%) (Figure 1).
 |
Figure 1 Patterns of systemic corticosteroid use at the OPD of Menelik II Referral Hospital, Addis Ababa, Ethiopia, 2019. |
Route of Administration of Systemic Steroidal Drugs
Most systemic GCs were administered intravenously (IV) (51.3%) out of the total of 384 examined patient medical charts at Menelik II Referral Hospital, while the least number of GCs were given through intramuscular (IM) route 5 (1.3%) (Figure 2).
Polypharmacy
The number of drugs per prescription varied from one to three and greater than three. The majority of the prescriptions contained two drugs per prescription 163 (42.4%), followed by >three drugs per prescription 94 (24.5%), three drugs per prescription 75 (19.5%), and one drug per prescription 52 (13.5%) (Table 3).
 |
Table 3 Number of Drugs per Prescription at Menelik II Referral Hospital in Outpatient Department, Addis Ababa, Ethiopia, 2019 |
Common Class of Steroid Use Based on the Duration
Intermediate-acting corticosteroids (prednisolone, methyl prednisolone) were mostly prescribed 165 (43.0%) followed by short-acting (hydrocortisone, beclomethasone) 127 (33.1%) and long-acting corticosteroids (dexamethasone) 92 (24%) (Table 4).
 |
Table 4 Common Class of Corticosteroid Use Based on Duration at OPD of Menelik II Referral Hospital, Addis Ababa, Ethiopia, 2019 |
Discussion
In the present study, patients treated with corticosteroids were mostly between 31–40 years of age (22.4%), and most of them were female (61.2%). As per the demographic data collected, this result was in line with the study conducted in India in which out of the total, 58.3% were female patients.14 This data showed that mid-aged group in both populations are almost equally prone to diseases for which steroids are used. But it is inconsistent with the study done at the District General Hospital in Amravati region, India which showed that 94 (53%) individuals were male patients.15
Respiratory diseases 244 (63.5%) were the major and cancer 4 (1.0%) was the least disorder for systemic corticosteroids to be indicated. This result is comparable with a study done in India, where 61.82% of indications were for respiratory tract disorders.16 The finding of this study also showed that prednisolone was the most commonly prescribed corticosteroid 163 (42.4%) while beclomethasone was the least prescribed drug 10 (2.6%). This finding is comparable with a study done in Denmark where prednisolone was the most frequently prescribed GC, accounting for 50% of all prescriptions assessed in the period.17 Out of the 384 patient medical charts analyzed, the highest number of systemic corticosteroids were administered through the intravenous (IV) route, accounting for 197 (51.3%), and the least was intramuscular, 5 (1.3%). This result is contrary to a study done in India where systemic corticoids administered through inhalation (44.5%) is higher than the IV route (24%).18 The majority of the prescriptions in this study contained two drugs per prescription 163 (42.4%). But, in another study done in India, the most common number of drugs per prescription was three (42.2%).19 This difference might be due to the degree of disease progression which requires more drugs in the latter study. Intermediate-acting corticosteroids (prednisolone, methyl prednisolone) were prescribed in most of the cases 165 (43.0%). This finding was in line with a study done in India, in which out of 119 GCs prescribed, intermediate acting corticosteroids that comprised of prednisolone and methyl prednisolone were most commonly prescribed (38.66%).18
Limitation of the Study
This was a cross-section study and the cause and effect were evaluated simultaneously. Therefore, the causal link could not be established due to the lack of a temporal link. As the sample size for this analysis was taken from one hospital using a quota sampling procedure, the findings presented here should be interpreted with caution and cannot be generalized to the entire population. The present study was also focused on the examination of the records; therefore, there were no inherent design limitations such as incompleteness of the data.
Conclusion
From this study, it can be concluded that among systemic steroids prednisolone was found to be the most frequently prescribed drug followed by hydrocortisone. Most of these corticosteroids were prescribed for respiratory disorders.
Abbreviations
GC, glucocorticoids; IV, intravenous; IM, intramuscular; PO, per oral; WHO, World Health Organization.
Data Sharing Statement
The datasets used during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors sincerely thank Addis Ababa University, College of Health Sciences, School of Pharmacy, Department of Pharmacology and Clinical Pharmacy for approving this study. We also thank the staff of Menelik II Referral Hospital for their cooperation and allowing us to conduct this study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was done with no financial support for any of the partial or complete work.
Disclosure
The authors declare that they have no financial and/or non-financial competing interests.
References
1. Moura MDG, Lopes LC, Silva MT, Barberato-Filho S, Motta RHL, de Cássia Bergamaschi C. Use of steroid and nonsteroidal anti-inflammatories in the treatment of rheumatoid arthritis: systematic review protocol. Medicine. 2018;97:41.
2. Salek S, Boscoe AN, Evans C, et al. Development of Patient-Reported Outcome Measures (Symptoms and Impacts) in Adults with Pyruvate Kinase Deficiency. Washington, DC: American Society of Hematology; 2019.
3. Wan ES, Qiu W, Baccarelli A, et al. Systemic steroid exposure is associated with differential methylation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(12):1248–1255. doi:10.1164/rccm.201207-1280OC
4. Ericson-Neilsen W, Kaye AD. Steroids: pharmacology, complications, and practice delivery issues. Ochsner J. 2014;14(2):203–207.
5. Luís M, Freitas J, Costa F, et al. An updated review of glucocorticoid-related adverse events in patients with rheumatoid arthritis. Expert Opin Drug Saf. 2019;18(7):581–590. doi:10.1080/14740338.2019.1615052
6. Ahmad DS, Wazaify MM, Albsoul-Younes A. the role of the clinical pharmacist in the identification and management of corticophobia–an Interventional Study. Trop J Pharm Res. 2014;13(3):445–453. doi:10.4314/tjpr.v13i3.20
7. Bylappa BK, Patil RT, Pillai RT. Drug prescribing pattern of topical corticosteroids in dermatology unit of a tertiary-care hospital. Int J Med Sci Public Health. 2015;4(12):1702. doi:10.5455/ijmsph.2015.17052015351
8. Enato EF, Sounyo AA, Madadi P. Assessment of disease profiles and drug prescribing patterns of health care facilities in Edo state, Nigeria. J Public Health Africa. 2012;e25–e. doi:10.4081/jphia.2012.e25
9. Ankit P, Bharat G. Study of drug utilization pattern of glucocorticosteroid drugs with special emphasis on their immediate adverse effects in a tertiary care teaching rural hospital. Int J Pharm Pract. 2010;3:4.
10. Rathi SK, D’Souza P. Rational and ethical use of topical corticosteroids based on safety and efficacy. Indian J Dermatol. 2012;57(4):251. doi:10.4103/0019-5154.97655
11. Desta Z, Abula T, Gebre-Yohannes A, Worku A. Drug prescribing patterns for outpatients in three hospitals in north-west Ethiopia. Ethiop J Health Dev. 2002;16(2):183–189. doi:10.4314/ejhd.v16i2.9809
12. Berha AB, Seyoum N. Evaluation of drug prescription pattern using world health organization prescribing indicators in tikur anbessa specialized hospital: a cross sectional study. J Drug Deliv Ther. 2018;8(1):74–80. doi:10.22270/jddt.v8i1.1652
13. Association WM. World Medical Association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373.
14. Gupta R, Malhotra P. Prescribing pattern of corticosteroids among the dermatology inpatients in a tertiary care teaching hospital of north India-a retrospective, observational study. Natl J Physiol Pharm Pharmacol. 2018;8(2):158–162. doi:10.5455/njppp.2018.8.0518424052018
15. Mulchand S, Bhupesh G, Dhanshree P, Aparna K. Assessment of drug utilization pattern of steroids in a district general hospital in Amravati region. Res Results Pharmacol. 2019;5:2.
16. Issac A, Yogananda R, Shehin M. Assessment of prescription pattern and monitoring adverse drug reaction of antibiotics in paediatric inpatients. Int J Contemp Pediatr. 2016;3(3):1071–1075. doi:10.18203/2349-3291.ijcp20162393
17. Laugesen K, Jørgensen JOL, Sørensen HT, Petersen I. Systemic glucocorticoid use in Denmark: a population-based prevalence study. BMJ Open. 2017;7(5):e015237. doi:10.1136/bmjopen-2016-015237
18. Aryal A, Kunwar K, Shadvar S, et al. Study on steroid utilization pattern in a tertiary care teaching hospital. Int J Pharm Pract. 2017;10(2):96–103. doi:10.5530/ijopp.10.2.19
19. Thakur PK, Majid A, Shramik M, Kumar S, Prospective A. Study on drug utilization evaluation of corticosteroids among out-patients of teaching hospital. Int J Pharm Pract Teach Pract. 2015;6(4):1–5.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.