Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 12
Assessment of Practice and Factors associated with Sunlight Exposure of Infants among Mothers in Debre Berhan Town, North Shewa Zone, Amhara Region, Ethiopia
Authors Teklehaimanot WZ, Kitawu LD, Tesfaye T , Mihretie A , Tizazu MA , Mekuriyaw AM, Negash KM , Muluneh MA
Received 31 July 2021
Accepted for publication 16 October 2021
Published 8 November 2021 Volume 2021:12 Pages 507—517
DOI https://doi.org/10.2147/PHMT.S330896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Wegayehu Zeneb Teklehaimanot,1 Leul Deribe Kitawu,2 Tewodros Tesfaye,2 Abebe Mihretie,1 Michael Amera Tizazu,1 Abebayehu Melesew Mekuriyaw,1 Kassa Mamo Negash,1 Mikyas Arega Muluneh1
1College of Health Science, Debre Berhan University, Debre Berhan, Ethiopia; 2College of Health Science, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Wegayehu Zeneb Teklehaimanot Tel +251 912768453
Email [email protected]
Background: Vitamin D deficiency is a common worldwide problem with its prevalence magnified in infants. Prevalence in infants is believed to range from 2.7% to 45% in different countries of the world. Appropriate sunlight exposure of skin is thought to be vital for the prevention of vitamin D deficiency. However, due to a dearth of study the practice of sunlight exposure is incompletely understood. Thus, assessing practice and factors affecting sunlight exposure of infants by mothers was relevant.
Objective: To assess practice level and factors associated with sunlight exposure of infants by mothers in Debre Berhan town, North Showa, Ethiopia, 2019.
Materials and Methods: A community-based cross-sectional study was conducted to collect relevant data among 530 mothers with infants at selected kebeles in Debre Berhan town. A simple random sampling technique was used to select kebeles and systematic sampling was complemented to identify study participant. Data were collected with interview using a pre-tested structured and semi-structured questionnaire. Bivariable and multivariable logistic regressions were run to examine the association among dependent and independent variable. Significant association was declared at P value ≤ 0.05.
Results: All the mothers were interviewed and 65.7% of them had good practice in sunning of their infant. In multi-variable analysis, mothers who are housewives or government employees, have a maternal age of 33 and above, perceive that sunlight strengthen infant bones, perceive that sunlight makes their infants healthier, and who got information from health-care professionals were significantly associated with good practice in sunning of their infant.
Conclusion and Recommendation: Finding of this study indicated that 34.3% of participants have poor practice in sunning of infants. This is a pointer that sunlight exposure of infants still needs attention from the government and other concerned bodies.
Keywords: rickets, sunlight exposure, ultraviolet index, vitamin D, VDD
Introduction
The healing power of the sun and its use in medical treatment (heliotherapy) has extended back into ancient times1 starting from about 1400 BC.2 In 1919, the first scientifically established health benefit of sun exposure was that sunlight can be used to prevent and cure rickets.3
Recently being exposed to ultraviolet radiation has been a subject of epidemiological interest due to both its beneficial and detrimental effects. Excessive ultraviolet radiation (UVR) is associated with skin cancer, sunburn, accelerated skin aging, and cataracts and it also reduces the effectiveness of the immune system. Contrary to the adverse effect, small amounts of UVR are beneficial to health, and play an essential role in the production of vitamin D.4 Sunlight exposure also still has inadequately explored benefits, which include release of nitric oxide, production of beta-endorphin, and regulation of circadian rhythms.5
Vitamin D is used for maintaining the plasma concentration of calcium and phosphate in normal physiologic range and it interacts with parathyroid hormone to maintain bone mineralization.6 Around 80–90% of vitamin D in humans is sunlight-derived production in the skin.7 But, to get such amount of vitamin D there are different factors to considered. Such factors are time spent outdoors, skin pigmentation, degree of latitude, season, the amount of cloud cover, the extent of air pollution, the amount of skin exposed, and the extent of ultra-violet B (UVB) protection, including clothing and sunscreens.8–10 For efficient production of vitamin D regular exposure of unprotected skin (without use of sunscreen and/or without clothing) to the available UVB radiation is recommended.11 UVB (short-wave ultraviolet rays) is found maximum in the midday sun. Thus, the best time of day for vitamin D production is near to solar noon from 10 a.m. to 2 p.m.5,11,12 Below latitudes of approximately 35° north, UVB radiation is sufficient for vitamin D3 synthesis throughout the year, however, at higher latitudes (above 35° north) vitamin D3 is not produced during the winter months and people may be predisposed to vitamin D deficiency unless taking vitamin D supplementation.13
Vitamin D deficiency (VDD), which is serum 25-hydroxyvitamin D (25OHD) level less than 30 nmol/l, is a worldwide health problem with numerous health consequences.14 Around 1 billion people worldwide, across all age groups, have a VDD. Epidemiological studies in different countries revealed that VDD is highly prevalent among infants, regardless of age, ethnicity, geographic location and climatic conditions and is believed to range from 2.7% to 45%.15,16 Ethiopia is not an exception from this burden. A study done in Addis Ababa revealed that 41% of children below three years of age visiting an out-patient department had vitamin D deficiency rickets and the frequency was higher in infants.17 Another study done in Jimma town found that the prevalence of vitamin D deficiency rickets in infants was 11%.18
Low vitamin D status is associated with demineralization of the skeleton, cardiovascular disease, cognitive decline, depression, diabetes mellitus, pregnancy complications and autoimmune diseases,19 growth retardation and skeletal deformities in children and infantile eczema in neonates.8,20,21 VDD has also substantial economic burdens. As much as 25% of health-care dollars could be saved just by improving the world’s vitamin D status.10
Although it is fairly simple to obtain vitamin D, lack of appreciation for the importance of sensible sunlight exposure to meet vitamin D requirements of children and adults has led to a worldwide VDD pandemic.10 Furthermore social, religious norms and health practice of mothers might lead to vitamin D deficiency by preventing infants from sunlight exposure.22 Previous study revealed that maternal age, maternal educational status, maternal occupation, family size and fathers’ educational status were significantly associated with practice of sunlight exposure.23
Efforts to prevent VDD with supplementation of vitamin D, fortification of milk or other foods with vitamin D and/or adequate sunlight exposure are recommended worldwide.15 Guidelines in Ethiopia recommend sunning of neonates starting from 2 weeks old for 15–20 minutes per day.24 Although health education to change maternal behaviour to expose infants to sunshine was adopted as the main strategy to combat rickets in the early 1960s, the implementation of this strategy is inconsistent.25 Despite all these efforts, lack of sunlight exposure continues to be the major risk factor of VDD rickets in Ethiopian children.26,27
There is an abundance of sunlight in Ethiopia throughout the year, but studies indicating the practice of mothers on sunning of their infants and factors barring infants from getting adequate sunshine are insufficient and especially no evidence is available in the study area. Therefore, this study aimed to assess the practice and factors associated with sunlight exposure of infants by mothers in the study area.
Materials and Methods
Study Design, Period, Setting and Populations
A community based cross-sectional study was conducted from March 15, 2019 to April 15, 2019 in Debre Berhan town. Debre Berhan town was founded by Emperor Zara Yaqob and it is a zonal administrative town of North Shewa, Amhara national regional state. It is 130 km away from Addis Ababa, the capital city of Ethiopia and 690 km from Bahir Dar, capital of Amhara region. The town is located at a latitude and longitude of 9°41ʹN 39°32ʹE and has an elevation of 2840 m above sea level. It has 14 kebeles, one referral hospital, 3 health centers and 14 health posts. A kebele is the smallest administrative unit in Ethiopia. Each kebele in larger cities of Ethiopia has its own kebele office encompassing at least 500 households. Data obtained from health extension workers’ family folders in all 14 kebeles of the Debre Berhan town indicated that there were 1946 mothers with a child less than 12 months old in 2019.
All mothers with a child less than 12 months old living in Debre Berhan town were the source population and all mothers with child less than 12 months old living in selected kebeles of Debre Berhan town were the study population. Respondents who were living in the town for less than 6 months and who were not able to speak or were severely ill during the data collection time were excluded from the study.
Sample Size and Sampling Procedure
A single population proportion formula was used to determine a total sample of 530 with the assumption of: 95% confidence interval, 5% margin of error, proportion (P) = 50% to get maximum sample size since there was no previous community-based study, design effect 1.5 and 10% non-response rate.
To identify study participants a multistage sampling technique was used. First, seven kebeles were selected from the existing 14 kebeles with a simple random sampling technique. Then the calculated sample size was proportionally allocated to each selected kebele of the town based on the number of infants available from the health extension workers’ family folders. Then, participants in each kebele were selected with systematic random sampling technique with an every two interval. During data collection the center of each selected kebele was located and with spinning pen the direction where the first household with infant was identified towards the tip of pen. Afterwards the first household with infant included in the study was selected by lottery methods from the first two households in the selected direction. In cases where two infants were found in one household only the caretaker of one infant was selected by lottery method. Revisit of three times was made in cases where eligible respondents were not available at the time of the survey.
Data Collection Tool and Procedure
Data were collected with face-to-face interview using pre-tested, structured and semi-structured Amharic version questionnaires by trained nurses. Data collection tools were prepared in English by reviewing different literatures and adapted to the local context then translated into Amharic language and back to English by respective language experts to check consistency. The questionnaire included seven questions related to socio-demographic characteristics; seven questions to evaluate practice of mother on sunning of infants; and four questions related to perceived consequence of sunlight exposure and three questions linked to health service utilization.
The data collection tool was pre-tested among 5% of the total sample size, and its clarity, length, and completeness were checked and appropriate amendment was undertaken. The pre-test was conducted in Chacha town, which is 51 km away from Debre Berhan town, to avoid information contamination. Six diploma nurses were recruited to conduct interview questionnaires with two BSc nurse supervisors. Training was given for one day on the objective, relevance of the study, informed consent, confidentiality of information and technique of interviewing.
Data Processing and Analysis
First data were checked for completeness and consistency before being entered in the computer. Then data were coded and entered to Epi-Data version 3.1 software and exported to SPSS statistical software version 22 for analysis. Descriptive statistics including frequency distribution, percentages, and measures of central tendency were used to summarize data. Binary and multiple logistic regression analysis were determined to assess the association between independent and dependent variables. The strength of statistical association was measured by odds ratio and 95% confidence intervals, and statistical significance was declared at p<0.05.
Key Words and Operational Definitions
Good practice: Mother responded to practice questions and scored above 3.5 median values
Poor practice: Mother responded to practice questions and scored 3.5 and below 3.5 median values
Completely covered: Infant wearing clothes that cover the whole body except the face. Unclothed: Infant wearing no clothes except pants.
Partly covered: Infant wearing minimal clothing (pants and vest) and not long shorts such that legs, arms and face are not covered.
Got antenatal care: mother who had at least one visit in health facility prior to onset of labour.
Got postnatal care: mother who had at least one return visit of health facility for postnatal care within six weeks of postpartum period.
Ethical Consideration
Ethical clearance was obtained from the Institutional Review Board (IRB) of Addis Ababa
University, school of nursing and midwifery. Then a formal letter of cooperation was written to Debre Berhan Town Health Office, and permission was obtained. Informed written consent was obtained from study participants and from their parents for those lower than 18 years old beside to individual assent. The purpose of the study was explained to the study participants, and anonymity, privacy, and confidentiality were ensured. Participants had the right to self-determination regarding to participate in study, both initially and during the data collection process. This study was conducted in accordance withthe Declaration of Helsinki.
Results
Socio-Demographic Characteristics of Respondents
A total of 530 mothers were asked and responded to the interviewee. From those 331 (62.5%) mothers had infants less than or equal to six months old. The mean age (±SD) of the participants was 27.96 (± 4.252) years. Two hundred and thirty-six (44.5%) participants had an age range of 27–32 years old. The majority of mothers (437; 82.5%) were orthodox followers. Most (468; 88.3%) mothers were married, 231 (43.6%) mothers had reached grade 9–12 in their educational status, 302 (57%) of mothers were housewife in their occupation. Four hundred and eight (77%) of mothers had three to four family members. Regarding their husbands’ educational status, 193 (36.4%) had diploma and above (Table 1).
 |
Table 1 Distribution of Socio-Demographic Characteristics of Study Participants in Debre Berhan Town, North Shewa Zone, Ethiopia, 2019 (n = 530) |
Practice of Mothers About Sunlight Exposure of Their Infants
Out of 530 respondents almost all (525; 99.1%) respondents intentionally expose their infant to direct sunlight. Four hundred and fifty (85.7%) of mothers start to expose their infants before they are 15 days old. Furthermore, in this study 322 (60.8%) mothers expose their infants to sunlight daily, with 509 (96%) mothers exposing in the morning before 10 a.m. and 188 (35.5%) mothers exposing their infants for a duration of 10−15 minutes. Regarded the condition of clothing during sunning of infant, 290 (54.7%) mothers expose with only putting diaper or naked. Three hundred and six (57.7%) of respondents did not apply any lubricant/body lotion during sunning of their infant (Table 2).
 |
Table 2 Distribution of Mothers by Their Practice Concerning Sunlight Exposure of Infants in Debre berhan Town, North Shewa, Ethiopia, 2019 |
Mother’s Level of Practice About Sunlight Exposure of Their Infants
For the above seven practices questions the median value is 3.5. Out of 530 respondents 182 (34.3%) scored less than the median value. Therefore, depending on the operational definition 34.3% of mothers had poor practice (Figure 1).
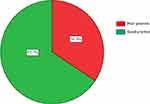 |
Figure 1 Distribution of mothers by their level of practice score regarding sunlight exposure of infants in Debre Berhan town, North Shewa, Ethiopia, 2019 (n = 530). |
Mother’s Source of Information for Intentional Exposure of Their Infant to Sunlight
Regarding the source of information for sunlight exposure of infants, most (370; 70.5%) mothers got information form health professionals followed by 202 (38.5%) mothers who got information from neighbours/family (Figure 2).
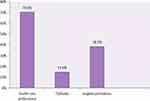 |
Figure 2 Distribution of mothers by their source of information about sunlight exposure of infants in Debre Berhan town, North Shewa zone, Ethiopia, 2019 (n = 525 to each). |
Perception of Mothers Towards Sunlight Exposure of Infant
Concerning the benefit of sunlight exposure, 515 (97.2%) respondents perceive sunlight exposure is good for infants. The majority (411; 79.8%) of mothers perceive sunlight exposure is important to strengthen infant bones followed by 332 (64.5%) mothers who thought that exposure benefits the sleep of infants. On the other hand, 18 (3.4%) mothers perceive that sunlight exposure had harmful effect and 13 (72.2%) of them thought sunning of infant predispose to pneumonia (Table 3).
 |
Table 3 Distribution of Mothers by Their Perception Related to Sunlight Exposure of Infants in Debre Berhan Town, North Shewa Zone, Ethiopia, 2019 |
Health Service Utilization of Mothers
Almost all respondents (527; 99.4%) delivered in a health facility but only 242 (45.9%) of them were advised to expose their child to sunlight and out of 504 mother who had ANC 155 (30.8%) were advised about sunning of their infant. Moreover from 473 (89.2%) mothers who had postnatal follow up, 285 (60.3%) were advised about sunning of their infant (Figure 3).
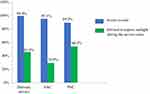 |
Figure 3 Distribution of mother by health service utilization in Debre Berhan town, North Shewa, Ethiopia, 2019. Notes: |
Bivariable and Multivariable Analysis of Mother’s Practices Regarding Sunlight Exposure Their Infant
In this study occupational status, infant age, family size, maternal educational status, marital status, source of information from health-care professional, from television/radio and from neighbours/relatives, maternal perception related to the benefit of sunning specifically to strengthening infant bones and to being healthier, to help the child sleep well and to grow faster, maternal perception regarding harmful effect of sunlight exposure, antenatal care, delivered at health facility and postnatal follow-up were tested on bivariable analysis at p-value < 0.2 to segregate candidate variables for multivariable analysis.
Afterwards in multivariable analysis the factors maternal age, occupational status, perceived to strengthen infant bones, perceived to be healthier infant and source of information from health-care professional were found to be significantly associated with maternal practice of infant sunlight exposure. Mothers whose age was 33 and above were 3 times (AOR = 2.97, 95% CI: 1.073, 8.223) more likely at having good practice in sunlight exposure of infant compared with mothers of age 15–20 years. Mother whose occupational status was housewife (Adjusted Odds Ratio (AOR) = 2.29, 95% CI: 1.03, 8.19) and government employee (AOR = 5.10, 95% CI: 1.54, 16.92) were 2 times and 5 times more likely to practice good sunning of infant compared with students, respectively. Furthermore, maternal perception of sunlight exposure as beneficial to strength infant bones (AOR = 2.79, 95% CI: 1.78, 4.37), to make the infant healthier(AOR = 1.83, 95% CI: 1.09, 3.16) and mother’s source information for sunning being health-care professionals (AOR = 2.11, 95% CI: 1.09, 4.06) showed statistically significant association with maternal practice of sunlight exposure of infant (Table 4).
 |
Table 4 Bivariable and Multivariable Analysis of Maternal Practice Towards Sunlight Exposure of Their Infants in Debre Berhan Town, North Shewa, Ethiopia, 2019 |
Discussion
This study was carried out to assess practice of mothers and associated factors concerning sunlight exposure of their infant in Debre Berhan town, Ethiopia in the study period. The finding of this study indicated that 34.3% of participants have poor practice in sunlight exposure of infants. This finding supports the fact that insufficient sun exposure is a major public health concern, and health education with particular emphasis for mothers and caregivers of young children should be provided.3,28
The finding of this study showed that 99.1% of mothers did intentionally expose their infant to direct sunlight. This is higher than a study done in Debre Markos which was 93%,23 but slightly lower than a study done in Jimma town which was 100%.18 This difference might be due to socio-demographic differences of respondents. Furthermore, study done at Townsville in Australia showed that only 20% of mothers intentionally expose their baby29 which was lower than the finding of this study. The possible reason behind this may be that the Australian cancer prevention society does not recommend infant sunlight exposure because of the high prevalence of skin cancer there and hence fear of skin cancer.
In this study 85.7% of respondents started to expose their infants to sunlight by the time they were 15 days old. This finding was not in agreement with a study of Debre Markos that showed only 23.4% started within 15 days.23 This discrepancy might be the study participants’ source of information. In this study the majority of respondents got information from health-care professionals and source of information from health-care professionals was positively and statistically significant associated with the practice level of mothers. Source of information for participants in that study was neighbor/elderly people, which has insignificant association with practice level of sunning of infant. Furthermore, a study done in Kiambu District Hospital, Kenya30 found that 40.3% infants started sunlight exposure within the second week of age which is lower than this study result. This difference could be due to the fact that Kiambu is nearer to the equator where the intensity of UVR is high compared with Debre Berhan, as a result mothers in Kiambu might fear this intense ultraviolet ray may harm their infant. This study also uncovered that 60.8% of mothers were sunning their infant on daily basis. This finding is in line with a study done in Debre markos which was 57.9%,23 but lower than a study done in Jimma town which was 92%.18 The possible reason for this variation might be climatic differences between the two towns.
This study showed that 97% of respondents exposed their infant to sunlight in the morning before 10 a.m. This implies almost all respondents did not expose their infant at the best time of day for vitamin D production, the time near to solar noon from 10 a.m. to 2 p.m.5,11,12 Evidence from IMNCI 2015 of Ethiopia indicated that babies need to be exposed to sunlight for 15–20 minutes per day.24 Moreover anecdotal evidence cited that regular exposure of unprotected skin (without use of sunscreen and/or without clothing) to the available UVB radiation is efficient for the production of vitamin D.11 In the present study only 55.2% and 32% of respondents were sunning their infant with only diaper/naked and for a duration of 15−20 minutes/day, respectively. Moreover, 41.7% of respondent in this study applied body lotion/lubricants at the time of sunning their infant. This implies that it is crucial to increase the awareness of communities regarding the appropriate practice of sunning of infants for optimal cutaneous vitamin D production.
This study presented that mothers who thought sunlight exposure is beneficial to strengthen infant bones, and will make their infants healthier, were 2.8 times and 1.8 times more likely at having good practice of sunning infants than their counterpart, respectively. This finding is in line with a study conducted in Addis Ababa that verified that maternal perceived consequences of sunlight exposure were significantly associated with maternal intention of exposing their infant to sunlight.25 This benefit is also clinically supported in that vitamin D is produced owing to sunlight exposure of bare skin. Vitamin D helps in maintaining the plasma concentration of calcium and phosphate in normal physiologic range and interacts with parathyroid hormone to maintain bone mineralization.6,31
Finding of this study also revealed that the odds of practicing good sunlight exposure of infant in mothers with age group of 33 and above years were 3-fold more than those in the age group of 15−20 years. Occupational status of mother was significantly associated with their practice of sunlight exposure. Mothers whose occupational status was housewife or government employee were 2 times and 5 times more likely to have good practice in sunning of infants compared with students, correspondingly. Similarly, a study in Debre markos showed that maternal age and occupational status were significantly associated.23
Limitation
Due to scarcity of similar studies, the researcher is faced with a challenge for comparing the result of the study in Ethiopia as well as in an African context. The information was self-reported and no experience of the mother was observed. Due to social desirability bias respondents might respond what they did not experience.
Conclusion
The finding of this study revealed that 34.3% of participants have poor practice in sunlight exposure of their infant. This low practice level is an indicator that the federal ministry of health, mass media, health care professionals and other concerned body did not give as much attention as is necessary to provide detailed information about the importance of infant sunlight exposure.
Maternal age, occupational status, perceived benefit by mothers on infant sunlight exposure particularly to strengthen infant bones, for the health of their infants, and source of information from health-care professionals were positively associated with maternal practice of infant sunning.
Recommendations
The federal ministry of health should coordinate concerned bodies for preparing a detail counseling steps on the appropriate practice of sunning of infants and incorporate these in the other health service guidelines. Non-governmental organizations should give attention and integrate this practice with other micronutrient deficiency preventive strategies.
Mass medias and health-care professionals should give more attention to the importance of sunlight exposure, how to practice this and give better information for the mothers. In addition, health-care professionals should prepare a leaflet on the appropriate practice of infant sunning and give it to each mother.
Future researchers are recommended to do further studies to determine the most appropriate way of sunning infants to maintain adequate serum vitamin D based on a study area’s ultra-violet index.
Acknowledgments
First and foremost, we would like to thank Almighty God who is our power and strength.
We have a great pleasure in acknowledging data collectors, supervisors and study participant. Finally, our gratitude reached to Addis Ababa University, school of Nursing and Midwifery for their financial support to conduct this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
The study was funded by Addis Ababa University, Ethiopia. The funder had no role in the study design, data collection, and analysis, interpretation of data, the decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Wunsch A. Lichtbiologie und lichtpathologie [Light biology and light pathology]. Erfahrungsheilkunde. 2006;55(7):361–369. German. doi:10.1055/s-2006-932357
2. Fitzpatrick TB, Pathak M. Part IV: basic considerations of the psoralens: historical aspects of methoxsalen and other furocoumarins. J Invest Dermatol. 1959;32(2):229–231. doi:10.1038/jid.1959.40
3. Hoel DG, Berwick M, de Gruijl FR, et al. The risks and benefits of sun exposure 2016. Dermato Endocrinol. 2016;8(1):e1248325. doi:10.1080/19381980.2016.1248325
4. World Health Organization. Ultraviolet radiation and human health. Fact Sheet. 2009;305:380–384.
5. Baggerly CA, Cuomo RE, French CB, et al. Sunlight and vitamin D: necessary for public health. J Am Coll Nutr. 2015;34(4):359–365. doi:10.1080/07315724.2015.1039866
6. DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004;80(6):1689S–1696S. doi:10.1093/ajcn/80.6.1689S
7. Tehrani FR, Behboudi-Gandevani S. Vitamin D and Human Reproduction. IntechOpen; 2017.
8. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi:10.1056/NEJMra070553
9. Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80(6):1678S–1688S. doi:10.1093/ajcn/80.6.1678S
10. Wacker M, Holick MF. Sunlight and Vitamin D: a global perspective for health. Dermatoendocrinology. 2013;5(1):51–108. doi:10.4161/derm.24494
11. Webb AR. Who, what, where and when—influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92(1):17–25. doi:10.1016/j.pbiomolbio.2006.02.004
12. Meena P, Dabas A, Shah D, et al. Sunlight exposure and vitamin D status in breastfed infants. Indian Pediatr. 2017;54(2):105–111. doi:10.1007/s13312-017-1010-9
13. Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362–371. doi:10.1093/ajcn/79.3.362
14. Holick MF. Vitamin D; extraskeletal health. Rheum Dis Clin North Am. 2012;38(1):141–160. doi:10.1016/j.rdc.2012.03.013
15. Almeida ACF, de Paula FJA, Monteiro JP, et al. Do all infants need vitamin D supplementation? PLoS One. 2018;13(4):e0195368. doi:10.1371/journal.pone.0195368
16. Atas E, Karademır F, Ersen A, et al. Comparison between daily supplementation doses of 200 versus 400 IU of vitamin D in infants. Eur J Pediatr. 2013;172(8):1039–1042. doi:10.1007/s00431-013-1997-4
17. Aust-Kettis A, Cvibah T, Clark P, Debele M. Rickets in Ethiopia. Ethiop Med J. 2008;3:109–121.
18. Getaneh T, Assefa A, Taddese Z. Rickets and the knowledge and practice of exposure to sunlight in Jimma town. Ethiopian J Heal Develop. 1998;12:29–32.
19. Hossein-nezhad A, Holick MF. Optimize dietary intake of vitamin D: an epigenetic perspective. Curr Opin Clin Nutr Metab Care. 2012;15(6):567–579. doi:10.1097/MCO.0b013e3283594978
20. Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81(3):353–373. doi:10.4065/81.3.353
21. Marwaha RK, Tandon N, Reddy DRH, et al. Vitamin D and bone mineral density status of healthy schoolchildren in northern India–. Am J Clin Nutr. 2005;82(2):477–482. doi:10.1093/ajcn/82.2.477
22. Marks R. The use of sunscreens in the prevention of skin cancer. Cancer Forum Aust Cancer Soc. 1996;20:211–214.
23. Abate A, Murugan R, Gualu T. Assessment of practice and factors affecting sunlight exposure of infants among mothers attending governmental health facilities in debre markos town, East Gojjam, Ethiopia, 2015. Am J Nurs. 2016;5(1):30–36. doi:10.11648/j.ajns.20160501.15
24. Federal ministry of health. Integrated Management of Newborn and Childhood Illness. Addis Ababa: Ethiopia; 2015.
25. Lulseged S, Deste C. Behavioural intention and factors influencing intention of Ethiopian mothers to expose infants to sunshine. Ethiopian J Heal Develop. 2002;16(1):31–40. doi:10.4314/ejhd.v16i1.9824
26. Kenenisa C, Ewnetu H, Sime H. Retrospective analysis of prevalence of rickets and associated factors among children admitted to pediatric Ward in Jimma University Specialized Hospital. J Pediatr Neonatal Care. 2014;1(7):00044.
27. Wondale Y, Shiferaw F, Lulseged S. A systematic review of nutritional rickets in Ethiopia: status and prospects. Ethiop Med J. 2005;43(3):203–210.
28. Ekbote V, Khadilkar A, Mughal M, et al. Sunlight exposure and development of rickets in Indian toddlers. Indian J Pediatr. 2010;77(1):61–65. doi:10.1007/s12098-009-0263-2
29. Harrison S, Buettner P. Why do mothers still sun their infants? J Paediatr Child Health. 1999;35(3):296–299. doi:10.1046/j.1440-1754.1999.00362.x
30. Muthoni ME. Risk factors associated with rickets in infants and children aged 6–59 months attending Kiambu District Hospital. Kenya: Kenyatta University; 2012.
31. Robert M, Kliegman M. Nelson Textbook of Pediatrics. Elsevier; 2016.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




