Back to Journals » Clinical Epidemiology » Volume 13
Assessment of a Claims-Based ICD-9 and ICD-10 Medication-Related Osteonecrosis of the Jaw Algorithm in the United States
Authors Stevens LAS, Spangler L, Yochum L, Ding Y, Wang FT
Received 24 June 2021
Accepted for publication 27 September 2021
Published 28 October 2021 Volume 2021:13 Pages 1019—1026
DOI https://doi.org/10.2147/CLEP.S325080
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Lars Pedersen
Lauren AS Stevens,1 Leslie Spangler,2 Laura Yochum,1 Yan Ding,1 Florence T Wang1
1Optum Epidemiology, Optum, Boston, MA, USA; 2Center for Observational Research, Amgen, Inc., Thousand Oaks, CA, USA
Correspondence: Florence T Wang
Optum Epidemiology, Optum, Boston, MA, USA
Email [email protected]
Purpose: Medication-related osteonecrosis of jaw (MRONJ) is associated with certain drug therapies. Pharmacoepidemiologic studies often rely on electronic healthcare data to assess adverse events following drug exposure. Few studies have developed and validated claims-based MRONJ identification algorithms. This study assessed the performance of claims-based MRONJ algorithms by chart review of potential cases among postmenopausal (PM) women and women with postmenopausal osteoporosis (PMO).
Methods: Among PM and PMO women sourced from a large US commercial health insurance database affiliated with Optum, potential cases were identified by International Classification of Diseases, 9th and 10th Revisions (ICD-9, ICD-10) diagnosis codes; 200 were selected for chart retrieval, with the goal of obtaining 100 charts in each coding era. Procured charts were redacted and then reviewed by an oral surgeon who determined case status. Positive predictive values (PPV) and 95% confidence intervals (CI) were calculated overall, by cohorts, and coding eras. Baseline characteristics were assessed. Two potential algorithm refinements were explored: using a restricted set of ICD codes; requiring antibiotic use after MRONJ diagnosis.
Results: A total of 1273 potential cases were identified. Of the 200 potential cases selected, 104 (52%) were procured, and six cases were confirmed (PPV 5.8%, 95% CI 2.2, 12.1). Baseline characteristics were largely similar across all strata. Potential algorithm refinements yielded marginal PPV improvement.
Conclusion: This study identified a small number of confirmed cases, and the resulting PPVs were low, but consistent with reported studies. Potential algorithm refinements yielded minimal improvements. To our knowledge, this study is the first to report on the identification of MRONJ using ICD-10 codes in the US.
Keywords: medication-related osteonecrosis of the jaw, MRONJ, algorithm validation, medical record review, health care database
Key Points
- Pharmacoepidemiologic studies often rely on electronic healthcare data to assess adverse events following drug exposure.
- Medication-related osteonecrosis of the jaw (MRONJ) is a rare condition that is associated with certain drug therapies.
- There are no validated claims-based ICD-10 algorithms for identifying medication-related osteonecrosis of the jaw in the US.
- Our study identified a small number of confirmed cases, and the resulting PPVs were low, but consistent with previously reported studies.
Introduction
Medication-related osteonecrosis of the jaw (MRONJ) is a condition defined by exposed bone, or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region, that has persisted for more than 8 weeks in a patient without prior radiation or obvious metastatic disease to the jaws.1 This condition has been associated with the use of anti-resorptive agents in the treatment of osteoporosis and other conditions.1–5
Pharmacoepidemiologic studies often rely on electronic healthcare data to evaluate the occurrence of adverse events following drug exposure. The validity of such studies depends on the existence of code-based algorithms that reliably capture true cases of events. To date, few studies have been conducted to develop and validate ICD (International Classification of Diseases, 9th and 10th Revisions) claims-based algorithms for the identification of MRONJ,6–8 and no studies have been reported on the use of ICD-10 codes in identifying MRONJ in the United States (US). We aimed to assess the performance of ICD-9 and ICD-10 claims-based MRONJ algorithms through a medical record review of potential cases of MRONJ identified in administrative claims data, among postmenopausal women and women with postmenopausal osteoporosis.
Methods
Study Design
We assessed the positive predictive value (PPV) of a claims-based MRONJ algorithm among a cohort of post-menopausal women (with and without osteoporosis), utilizing data from a large US commercial health insurance claims database. Potential cases of MRONJ were identified from 26 May 2010 to 31 March 2017 by the presence of at least one ICD-9 or ICD-10 diagnosis code associated with MRONJ, and medical records were sought for a sample of eligible potential cases. Procured medical records were reviewed by a practicing oral surgeon, and a case definition was applied to determine the final MRONJ case status. To assess the performance of the claims-based algorithm, PPVs and 95% confidence intervals (95% CIs) were calculated by cohort and coding era. Potential refinements to the claims-based algorithm were also assessed.
Data Source
The study population was sourced from the Optum Research Database (ORD). The ORD contains demographics and pharmacy, medical, and facility claims for US commercial health plan members, which provide dates of services, procedures, and their accompanying diagnoses. The underlying insured population from which the data are drawn is geographically diverse and comprises approximately 4% of the US population. In this study, claims data were supplemented with information recorded in the medical records relating to MRONJ diagnosis and/or treatment among a subset of patients for whom medical records were eligible for request (medical record request eligibility is determined by the health plan). Confidentiality of patient medical records was maintained at all times. Approval of the study protocol and a waiver of authorization for medical record procurement and review from a central Institutional Review Board (IRB) were obtained (#120180072).
Study Population
For inclusion in the cohort of post-menopausal women (PM cohort), women were required to be at least 55 years of age; as post-menopausal status is not available within the database, age 55 years or older served as a proxy for post-menopausal status, reflecting the average age of menopause in the US.9 Additionally, the women were required to have been continuously enrolled in the health plan for a minimum of one year (365 days), and to have had at least one medical encounter in the year prior to (and including) their cohort entry date, with at least one day of follow-up. Among the women meeting the PM cohort criteria, the subset with at least one diagnosis code indicative of osteoporosis, osteoporotic fracture, or relevant osteoporosis treatment (bisphosphonates, denosumab, calcitonin, teriparatide, or romosozumab) were eligible for inclusion into the cohort of postmenopausal women with osteoporosis (PMO cohort). Those with a baseline diagnosis of MRONJ, Paget’s disease, or diagnosis or treatment for malignancy (excluding skin cancer) were excluded. The cohort entry date for women in both the PM and PMO cohorts was defined as the first date when the patient satisfied all the cohort criteria, respectively, between 26 May 2010 and 31 March 2017. The 12 months prior to meeting PM or PMO cohort eligibility was set as the baseline period, with the cohort entry date defined as the last day of the baseline period.
Outcomes
Potential cases of MRONJ were identified from 26 May 2010 to 31 March 2017 by the presence of at least one ICD-9 or ICD-10 MRONJ-related diagnosis code among the PM and PMO cohorts (Supplemental Table A). To reduce the risk of missing true cases, the MRONJ code list included codes relating to inflammation of the jaw, and osteonecrosis of non-specific sites. To validate the claims-based MRONJ algorithm, we aimed to seek up to 200 medical records (one chart per potential case of MRONJ) among the PM and PMO cohort members. Since the PMO cohort was the primary cohort of interest, medical records were requested for all potential cases that were eligible for procurement within this cohort. The remaining medical records in the sample were randomly selected from the potential MRONJ cases identified in the PM cohort, with the goal of requesting up to 100 medical records among ICD-9 identified potential cases and 100 medical records among ICD-10 identified potential cases across the two cohorts (Table 1). Procured medical records were redacted with respect to personally identifiable information and mentions of osteoporosis treatment, then reviewed by a practicing oral surgeon who completed a case questionnaire specific to the diagnosis of MRONJ that was then used to determine case status. A confirmed MRONJ case was defined by confirmation of the following four criteria in the medical record: 1) demonstration of exposed bone in the oral cavity; 2) demonstration of exposed bone or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region; 3) evidence that the exposed bone lesion lasted longer than 8 weeks; and 4) confirmation that the patient did not have a history of radiation therapy, or obvious metastatic disease, to the jaws.1 Cases not meeting all four criteria were classified as either a confirmed non-case (based on the presence of a definitive MRONJ rule-out or an alternative diagnosis unrelated to MRONJ in the medical record), or as a case containing insufficient information for review (where the medical record contained insufficient information to definitively confirm or deny any of the four case criteria).
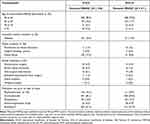 |
Table 1 Patient Characteristics of Potential Cases of MRONJ, 26 May 2010 Through 31 March 2017 |
Analysis
To assess the algorithm performance, PPVs, defined as the number of confirmed cases divided by the number of medical records received containing sufficient information for review, and corresponding 95% CIs were calculated, overall, and stratified by cohort (PM, PMO) and coding era (ICD-9, ICD-10). Baseline characteristics were described for all potential cases.
Two potential algorithm refinements were explored. First, we identified potential cases using only the subset of the diagnosis codes contained in the original algorithm that captured chart-confirmed cases (restricted algorithm). The second potential refinement was to require antibiotic use during the month following the claims-identified MRONJ diagnosis. PPVs and 95% CIs were calculated to assess the performance of both potential algorithm refinements.
Results
From May 2010 to March 2017, there were 1,951,191 women who were eligible for inclusion in the PM cohort, and 278,136 who were eligible for the PMO cohort. Across these two cohorts 1273 potential claims-identified cases of MRONJ were identified by the presence of at least one ICD-9 or ICD-10 diagnosis code pertaining to MRONJ across the two cohorts (Supplemental Table A). The majority of the potential cases were identified by the diagnosis code for inflammatory conditions of the jaw, 551 by ICD-9 526.4 (43.3%) and 191 by ICD-10 M27.2 (15.0%), and 193 by ICD-10 M87.9, osteonecrosis, unspecified (15.2%) (Table 2).
 |
Table 2 Chart Retrieval Statistics of the Claims-Based MRONJ Algorithm, 26 May 2010 Through 31 March 2017 |
Medical records were ultimately sought for 198 potential cases (133 in the PM cohort, 65 in the PMO cohort). Of these, 104 (52%) containing sufficient information for review were procured (72 in the PM cohort, 32 in the PMO cohort), the majority corresponding to ICD-9 526.4 (73.3%), and ICD-10 M27.2 (39.0%) and M87.9 (40.7%). No medical records containing sufficient information for review were procured for ICD-9 526.5 (alveolitis of jaw) or for ICD-10 M87.180 (osteonecrosis due to drugs, jaw), M87.28 (osteonecrosis due to previous trauma, other site), and M87.38 (other secondary osteonecrosis, other site) (Table 2).
Baseline characteristics among potential cases were largely similar across cohort and coding era, with the exception of use of antibiotics, which was more prevalent among ICD-9 identified potential cases than among ICD-10 identified potential cases (61.3% v. 41.5%) and use of corticosteroids, which was less prevalent among ICD-9 identified potential cases than among ICD-10 identified potential cases (46.1% 59.5%) (Table 1). Baseline characteristics among records procured and not procured were also similar across both cohorts and coding eras (data not presented).
Six cases were confirmed overall (PPV 5.77%, 95% CI 2.2, 12.1), split equally across coding era (3 identified by ICD-9 (PPV 6.67%, 95% CI 1.4, 18.3), 3 identified by ICD-10 (PPV 5.08%, 95% CI 1.1, 14.2)). Four cases were confirmed in the PM cohort (PPV, 5.56%, 95% CI 1.5, 13.6), and two in the PMO cohort (PPV 6.25%, 95% CI 0.8, 20.8) (Table 3). Four confirmed cases were identified by the ICD-9 and ICD-10 diagnosis code for inflammatory conditions of the jaw; ICD-9 526.4 (PPV 6.06%, 95% CI 0.7, 20.2), and ICD-10 M27.2 (PPV 8.70%, 95% CI 1.1, 28.0). The two remaining confirmed cases were captured by the ICD-9 diagnosis code for aseptic necrosis of bone, jaw, 733.45 (PPV 12.50%, 95% CI 0.3, 52.7) and the ICD-10 diagnosis code for idiopathic aseptic necrosis of bone, other sites, M87.08 (PPV 25.00%, 95% CI 0.6, 80.6) (data not presented). When restricted to the subset with prior use of bisphosphonates, the PPV was 11.8 (95% CI 1.5, 36.4) (data not presented). Lastly, two cases were confirmed among women over the age of 65; one in the PM cohort (PPV 8.33%, 95% CI 0.2, 38.5) and one in PMO cohort (PPV 10.00%, 95% CI 0.3, 44.5) (data not presented). Given the small number of confirmed MRONJ cases, we were not able to assess algorithm performance under comorbid conditions.
 |
Table 3 Positive Predictive Values of the Claims-Based MRONJ Algorithm, 26 May 2010 Through 31 March 2017 |
Applying the potential algorithm refinements resulted in marginal and incremental PPV improvements. The restricted algorithm that included only the four diagnosis codes that identified chart-confirmed cases of MRONJ in the main analysis (ICD-9 codes 526.4, 733.45 and ICD-10 codes M27.2 and M87.08), as well as ICD-9 code 526.5 (alveolitis of jaw), which identified true cases of MRONJ in another US-based study, increased the overall PPV to 8.96% (95% CI 3.4, 18.5). Requiring antibiotic use during the month following the MRONJ diagnosis increased the overall PPV to 7.55% (95% CI 2.1, 18.2). When the restricted algorithm was used in conjunction with the antibiotic use requirement, the overall PPV increased to 9.52% (95% CI 2.7, 22.6). Within the strata of PM and PMO cohorts, and ICD-9 and ICD-10 coding eras, no consistent pattern of higher PPVs was observed for any potential algorithm refinement (Table 4).
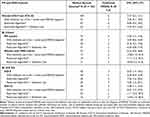 |
Table 4 Positive Predictive Values of Potential Claims-Based MRONJ Algorithm Refinements, by Coding Era and Cohort, 26 May 2010 Through 31 March 2017 |
Discussion/Conclusions
Within our study, six true cases of MRONJ were confirmed among the 104 medical records procured containing sufficient information for review, resulting in a PPV of 5.77%. Similarly, low PPVs were observed when stratifying by cohort, or coding era. In this study, we did not receive medical records containing sufficient information for review for all diagnosis codes included in the MRONJ algorithm, particularly ICD-10 M87.28 (osteonecrosis due to previous trauma, other sites), M87.38 (other secondary osteonecrosis, other sites), and M87.180 (osteonecrosis due to drugs, jaw). As such, we were unable to assess the performance of these codes in identifying true MRONJ events.
Our observed low rate of case confirmation and resulting low PPVs may be partially attributed to the rarity of MRONJ, and to the inclusion of non-MRONJ specific codes in the case algorithms, the latter of which is an approach typically taken to reduce the risk of missing true cases, but at the cost of increasing the number of false-positive cases identified. During medical record review, non-cases were most often found to have osteonecrosis at a site other than the jaw, or to have received a diagnosis unrelated to MRONJ, such as palatal abscess. Further, the presence of a diagnosis code on a medical claim may not reflect the presence of disease, as the diagnosis code may indicate a rule-out criterion or justification for procedures or services rendered rather than the presence of actual disease. The inclusion of such potential MRONJ cases (who received the MRONJ codes for services rendered rather than final diagnosis) would also result in a lower PPV due to the inclusion of false positives. The low PPV may also reflect the application of the case definition, which required the presence of specific clinical presentations in the physical record. As the information recorded in the charts may be incomplete, true cases of MRONJ may have been classified as having insufficient information to confirm the case.
When two potential algorithm refinements were assessed, we found limited improvement in PPVs, both overall and within cohort and coding era strata. Specifically, when the claims-based algorithm was restricted to include only those diagnosis codes that captured confirmed cases in the main analysis, it resulted in only a marginally improved PPV of 8.96%, suggesting that clinicians may be using a broader range of diagnosis code(s) to indicate MRONJ than expected.
The medical record procurement rate in this study was 52%, which is lower than our expected (historical) procurement rates of 70–80%.10–12 Our procurement rate may reflect the age of records being sought, as the successful retrieval of older records is often more challenging, the rarity of the outcome, and the type of providers contacted. Specifically, we preferentially contacted oral surgeons or dental providers, and these providers may be more likely to opt out of providing the requested records due to the lack of experience with this type of study request. Low procurement rates may also raise concerns about potential bias and generalizability of the study results. Concerns regarding bias often stem from scenarios where the proportion of records received is differential with respect to the exposure-outcome association (for example, those who are exposed to the drug of interest and may be more likely to have the outcome, are more likely to provide records). In this study, the decision to seek a medical record for a particular case was not based on any particular drug exposure, thereby making selection bias due to chart retrieval rate unlikely. Moreover, we found the baseline characteristics of patients with charts procured and charts not procured to be largely similar, suggesting that our study results are generalizable to the broader PM and PMO study populations.
Few studies have been conducted to develop and validate claims-based algorithms for the identification of MRONJ.6–8,13 Within the US, one study evaluated a claims-based algorithm that included ICD-9 733.45 (aseptic necrosis of the jaw), 522.7 (periapical abscess with sinus), 526.4 (inflammatory conditions of the jaw), 526.5 (alveolitis of jaw[s]), and 526.9 (unspecified disease of the jaws), among women with osteoporosis enrolled in US Medicare from 2006 to 2008. In this study, 6 of 84 potential MRONJ cases were confirmed, resulting in a PPV of 7.1% (95% CI 2.7, 14.9),6 similar to our overall PPV of 5.77%. To date, no studies have reported on the performance of ICD-10 MRONJ algorithms within the US.
Within the European Union, two studies have reported on the performance of ICD-10-based MRONJ algorithms. In a study of women with PMO identified from 2005 to 2010 in the Danish National Registry of Patients, Gammelager et al reported that an algorithm, which included ICD-10 M87.0 (idiopathic aseptic necrosis of bone), M87.1 (osteonecrosis due to drugs), M87.2 (osteonecrosis due to previous trauma), M87.3 (other secondary osteonecrosis), M87.8 (other osteonecrosis), M87.9 (osteonecrosis, unspecified), K10.2 (inflammatory conditions of the jaw), K10.3 (alveolitis of the jaws), and K04.6 (periapical abscess with sinus), confirmed 19 cases of the 60 identified, producing a PPV of 32% (95% CI 20, 45).7 Another study, conducted among women with PMO identified from the Swedish National Patient Register using the same EU ICD-10 codes as Gammelager et al, identified 87 potential cases identified, 15 of which were confirmed as true cases of MRONJ, producing a PPV of 18% (95% CI 10, 28).8
In summary, we utilized a sensitive algorithm for identifying MRONJ and confirmed a small number of true cases. While this current study contributes to the existing body of knowledge by assessing both ICD-9 and ICD-10 algorithm performance within the US, our resulting PPVs were generally low, but consistent with previously reported studies. Potential refinements to the algorithm resulted in minimal improvements, and additional research is needed to assess the performance of those diagnosis codes for which no medical records were successfully procured. To our knowledge, our study is the first to report on the identification of MRONJ using ICD-10 codes in the US.
Ethics Statement
Approval of the study protocol by the New England Independent Review Board, and a waiver of authorization for medical record procurement and review from a central Institutional Review Board (IRB) were obtained.
Acknowledgments
This work has been previously presented at the 36th International Conference on Pharmacoepidemiology and Therapeutic Risk Management (ICPE All Access); September 16-17, 2020.
Funding
This work was funded by a research contract between Optum Epidemiology (a UnitedHealth Group (UHG) company) and Amgen, Inc. The contract provides Amgen with the opportunity to provide input on the design and conduct of the study, and drafting of the manuscript. Optum and Amgen have joint publication rights.
Disclosure
L Yochum, Y Ding and FT Wang are employees of Optum and own UHG stock. L. Spangler is an employee of Amgen and owns Amgen stock. LAS Stevens is an employee of Humana Healthcare Research, Louisville, KY, USA. The authors report no other conflicts of interest in this work.
References
1. Ruggiero SL, Dodson TB, Fantasia J, et al; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956. doi:10.1016/j.joms.2014.04.031
2. American Association of Oral and Maxillofacial Surgeons (AAOMS). Position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007;5:369–376.
3. American Association of Oral and Maxillofacial Surgeons. Position paper on bisphosphonate-related osteonecrosis of the jaw 2009 update. Available from: http://www.aaoms.org/docs/position_papers/bronj_update.pdf.
4. Bamias A, Kastritis E, Bamia C, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol. 2005;23(34):8580–8587. doi:10.1200/JCO.2005.02.8670
5. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62(5):527–534. doi:10.1016/j.joms.2004.02.004
6. Wright NC, Curtis JR, Arora T, et al. The validity of claims-based algorithms to identify serious hypersensitivity reactions and osteonecrosis of the jaw. PLoS One. 2015;10(7):e0131601. doi:10.1371/journal.pone.0131601
7. Gammelager H, Sværke C, Noerholt SE, et al. Validity of an algorithm to identify osteonecrosis of the jaw in women with postmenopausal osteoporosis in the Danish National Registry of Patients. Clin Epidemiol. 2013;5:263–267. doi:10.2147/CLEP.S45226
8. Bergdahl J, Ehrenstein V, Jarnbring F, et al. Evaluation of an algorithm ascertaining cases of osteonecrosis of the jaw in the Swedish National Patient Register. Clin Epidemiol. 2013;5:1–7. doi:10.2147/CLEP.S37664
9. Menopause basics. Office on women’s health. Available from: https://www.womenshealth.gov/menopause/menopause-basics.
10. Dore DD, Bloomgren GL, Wenten M, et al. A cohort study of acute pancreatitis in relation to exenatide use. Diabetes Obes Metab. 2011;13(6):559–566. doi:10.1111/j.1463-1326.2011.01376.x
11. Eng PM, Mast TC, Loughlin J, Clifford CR, Wong J, Seeger JD. Incidence of intussusception among infants in a large commercially insured population in the United States. Ped Infec Dis J. 2012;31(3):287–291. doi:10.1097/INF.0b013e31824213b1
12. Quam L, Ellis LB, Venus P, Clouse J, Taylor CG, Leatherman S. Using claims data for epidemiologic research. The concordance of claims-based criteria with the medical record and patient survey for identifying a hypertensive population. Med Care. 1993;31(6):498–550. doi:10.1097/00005650-199306000-00003
13. Kim HY, Kim JW, Kim SJ, Lee SH, Lee HS. Uncertainty of current algorithm for bisphosphonate-related osteonecrosis of the jaw in population-based studies: a systematic review. J Bone Miner Res. 2017;32(3):584–591. doi:10.1002/jbmr.3017
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
